Abstract
Imaging is a critical component in the workup for failed anterior cruciate ligament reconstruction (ACLR). Radiographs, computed tomography (CT), and magnetic resonance (MR) can identify causes of ACLR failure, such as tunnel malposition or graft rupture, as well as facilitate preoperative planning for future tunnel placement or the need for additional procedures, such as a two-stage revision with bone grafting, collateral ligament reconstruction, meniscal transplant, sagittal or coronal plane osteotomy, or chondral restoration. Additionally, there has been an increased focus on anatomic reconstruction, and an increased recognition of associated injuries including ramp lesions and anterolateral complex injuries, that may predispose to persistent instability or a higher chance of failure. This chapter not only covers the various utilities of imaging but also reviews how to identify potential complications and preferred imaging modalities for specific purposes and presents a review of the literature on these topics.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Revision
- Anterior cruciate ligament
- Reconstruction
- Imaging
- Radiographic workup
- Graft failure
- Graft rupture
Introduction
A greater understanding of the role of imaging in the diagnosis and treatment of the failed ACLR is critical for all surgeons performing revision ACLR. Plain radiographs, computed tomography (CT), and magnetic resonance (MR) imaging all have various roles and can be helpful for identifying the etiology of a prior ACLR failure, as well as assist in preoperative planning. The focus of this chapter is on the use of imaging in the workup and treatment of the failed ACLR.
Radiographic Landmarks for Anatomic ACL Reconstruction
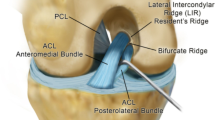
Multiple studies have shown that non-anatomic tunnel placement, specifically femoral tunnel placement, is associated with higher rates of ACLR failure [1, 2]. While anteromedial portal femoral tunnel drilling was introduced to facilitate a more anatomic and horizontal femoral tunnel position and has been shown to accomplish this goal [3], recent studies have found high rates of non-anatomic tunnel placement with both methods, which highlights the importance of careful tunnel position identification regardless of surgical technique [4].
There are several radiographic landmarks that can be used to evaluate femoral tunnel position. In the coronal plane, whether on an anteroposterior (AP) radiograph or the coronal cut of MRI or CT imaging, the clock-face method is often used to evaluate the femoral tunnel position. Using this method, the femoral tunnel is either placed at the 10 o’clock or 2 o’clock position for a right or left knee, respectively (Fig. 2.1). Of note, this method has been shown to have poor inter-rater reliability, and many, including the authors of this chapter, have moved away from this method as it is not reliable and does not accurately correspond to bony morphology [5, 6]. In the sagittal plane, the quadrant method has been described to evaluate the femoral tunnel position (Fig. 2.2). Using this method, a grid is superimposed on the femoral condyles. The ideal tunnel position is just inferior to the most superoposterior quadrant [7]. This corresponds to a point in center of the ACL footprint which leaves about 1–2 mm of the posterior cortical wall of the femur intact.
Normal radiographic appearance after anterior cruciate ligament reconstruction. Frontal and lateral radiographs of the knee demonstrate typical postoperative changes after bone-patellar tendon-bone autograft harvesting, with geographic defects along the central patella and the tibial tuberosity at the bone plug harvest site (asterisks). The femoral tunnel interference screw is in standard position, at the 10 o’clock position (femoral arrowhead, a). The tibial tunnel should lie posterior to where Blumensaat’s line intersects the tibia (dotted line, b)
Quadrant method for identifying anatomic ACL origin and correct femoral tunnel position. A grid is superimposed on the femoral condyles parallel to Blumensaat’s line. Each dimension is split into quartiles. The anatomic origin of the anteromedial bundle is about 25% anterior and deep to the posterosuperior most aspect of the femoral condyle (blue dot). The anatomic origin of the posterolateral bundle is about 33% anterior and 50% deep to the posterosuperior most aspect of the femoral condyle (yellow dot). The center of the ACL between these two points is shown by the green dot
With regard to the tibial tunnel, in the coronal plane, the tibial ACL footprint corresponds to a point between the intercondylar eminences about 2/5 of the way from the medial to lateral eminence [8]. In the sagittal plane, traditionally the tibial tunnel was recommended to be placed parallel to the slope of the intercondylar roof, i.e., Blumensaat’s line [9]. Using this model, the ideal tibial ACL footprint lies just posterior to where Blumensaat’s line intersects the surface of the tibia (Fig. 2.1). Recent studies have suggested that use of the intercondylar roof may not always be a reliable landmark, however, and have identified that the center of the tibial ACL footprint can more consistently be located at a point between 43% and 45% of the anteroposterior length of the tibia (Fig. 2.3) [10]. This is based on anatomic studies showing consistency in the location of the tibial ACL footprint relative to the length of the tibial plateau despite variation in intercondylar roof angles. Moreover the tibial tunnel angle will occasionally need to be altered depending on the length of the harvested graft to avoid graft tunnel mismatch [11]. To avoid graft impingement in the intercondylar notch during extension, the tibial tunnel angle is typically recommended to be parallel to the intercondylar roof inclination angle, which has been reported to be, on average, 36.8° in men and 35.2° in women [12].
Tibial tunnel location based on the anteroposterior length of the tibial plateau. The method of Stäubli et al. is shown for identifying the ideal tibial tunnel location. A point 44% from the anterior to the posterior edge of the tibia is noted which corresponds to the average location of the ACL insertion
It is worth noting that, while plain radiographs can provide valuable information, multiple studies have shown poor inter-rater reliability and validity with the use of plain radiographs for the evaluation of tunnel placement when compared to MR and CT imaging. Moreover, it is often difficult to even identify bony tunnels on plain radiograph. Some authors recommend routinely obtaining CT imaging for the most accurate identification of prior tunnel position whenever precise measurements are needed [13]. Three-dimensional CT reconstructions can also be extremely helpful, as they can directly examine the aperture on both the femur and the tibia, especially when the medial femoral condyle is subtracted, as this allows a direct en face view of the lateral femoral condyle wall and the tibial plafond (Fig. 2.4).
Graft Complications
Graft Integrity
MRI is the preferred diagnostic modality for evaluation of partial and complete graft tear, demonstrating an overall specificity of 86.7% and a positive predictive value of 93.5% [14]. Similar to evaluating the native anterior cruciate ligament, the anterior cruciate ligament graft should be evaluated in the axial, coronal, and sagittal planes on every knee MRI. In the authors’ experience, tear of the graft is most readily identified in the axial or coronal plane, typically in close proximity to the femoral tunnel entrance site. Graft tear may appear as frank disruption of graft fibers with an obvious defect on fluid-sensitive images (Fig. 2.5); however, graft fiber discontinuity may be difficult to appreciate in more chronic tears with scarring around the graft. Occasionally in chronic tears, the graft may become largely resorbed and poorly visualized. On sagittal images, orientation of graft fibers should be closely scrutinized. Normally the graft should remain taut and parallel to Blumensaat’s line (Fig. 2.6), with a more horizontal orientation and any fiber redundancy being important clues in subtle tears.
Complete ACL graft tear on MRI. Axial image (a) demonstrates a fluid filled full-thickness defect (arrowhead) of graft fibers adjacent to the femoral tunnel. Sagittal image (b) demonstrates redundancy of graft fibers, which are normally taut, and important secondary findings, including an impaction fracture of the lateral femoral condyle (arrowhead), contusion of the posterolateral tibial plateau (asterisk), and anterior tibial translation (c)
Additionally, it is important to distinguish partial graft tear or low-grade sprain injury from the normal process of ligamentization seen in the immature graft. This process is often described as consisting of three phases: an initial healing phase during the first 6 months after surgery, a second remodeling stage which typically continues for another 6 months, and a final maturation phase which starts around 1 year after surgery and has been shown to continue at 2 years after surgery [15]. Ligamentization during the early healing phase will manifest on MRI as focal areas of intermediate signal within the graft that should not be misinterpreted as pathologic (Fig. 2.7). This signal intensity tends to slowly decrease as the graft matures [16]. While numerous studies have found varying timelines for ligamentization, some have reported that ligamentization may persist for up to 4 years following graft reconstruction [9].
Aside from discrete graft tear, secondary findings may be useful in diagnosing a graft tear, including the presence of a large joint effusion, contusion of the lateral femoral condyle and posterior lateral tibial plateau, and anterior tibial translation, imaging findings which are commonly seen in primary ACL tears (Fig. 2.5) [9].
It is important to note, though, that MR imaging is not completely sensitive to graft rupture. One retrospective review of 50 revision ACL cases found that in 24% of cases, the graft was read on MR imaging as intact despite no intact graft on arthroscopic or clinical examination [17]. The sensitivity of MR imaging for detecting ACL graft rupture has been reported to range from 59% to 72% [14, 17, 18]. It is important that any findings on MR imaging are combined with clinical and arthroscopic findings when evaluating for graft rupture after ACLR.
Graft Impingement
Graft impingement is a significant complication of ACLR and can lead to graft rupture, anterior knee pain, knee effusions, and loss of range of motion, particularly extension [19]. Graft impingement occurs when the graft makes contact with the walls of the femoral intercondylar notch, typically during extension. This can occur due to anterior positioning of the tibial tunnel or anterior positioning of the femoral tunnel [19]. Findings of graft impingement on MR imaging include evidence of graft contact with the intercondylar roof, posterior bowing of the graft, and altered signal intensity in the graft, typically in the anterior two thirds (Fig. 2.8) [9, 20]. It is important to distinguish graft impingement from a partial graft tear with anterior tibial translation, as they can have similar findings including anterior position of the tibia relative to the femur, buckling of graft fibers, and altered graft signal intensity. Anterior positioning of the tibial tunnel and the presence of a true cyclops lesion [21] are findings that might suggest graft impingement rather than a partial graft tear. It is important to distinguish a true cyclops lesion from a “pseudocyclops” lesion which can occur in partial graft tears when the torn fibers flip into the intercondylar notch and create a mass-like appearance – these can be distinguished from true cyclops lesions as these fibers can be traced back to the femoral or tibial tunnels [22].
Roof impingement following ACL reconstruction. Sagittal MRI image shows evidence of roof impingement, with anterior graft fibers (arrowheads) mildly frayed and kinked along the undersurface of the intercondylar notch. The tibial tunnel has an anterior position relative to where Blumensaat’s line intersects the tibia, predisposing to roof impingement
A less common form of graft wall impingement is sidewall impingement, which may occur between the graft and the medial wall of the lateral femoral condyle if the tibial tunnel is placed too laterally, which appears as a medial indentation in the graft [23]. It can also occur as a result of osteophyte formation at the site of notchplasty or an interference screw protruding into the intercondylar notch [24, 25].
Hardware Complications
ACLR failure can occur as a result of failure of graft fixation. Fixation devices such as metal or bioabsorbable interference screws can rarely loosen and migrate intra-articularly (Fig. 2.9) [26, 27]. As mentioned above, if the screw is not placed entirely within the tunnel and is slightly protruding intra-articularly, it can lead to graft impingement [24]. Occasionally, the tibial interference screw will have a proud position and may irritate the overlying soft tissues, with potential for formation of an adventitial bursa.
Other Complications
Arthrofibrosis
Arthrofibrosis after ACLR is defined as the presence of scar tissue within the knee joint and is reported to occur in 1–10% of patients after ACLR. There are two main forms: focal arthrofibrosis (otherwise known as the cyclops lesion) and diffuse arthrofibrosis.
A cyclops lesion is a nodular mass of fibro-proliferative tissue and can sometimes contain osseous or cartilaginous tissue and, in such cases, are sometimes referred to as “true cyclops” lesions as opposed to cyclopoid scars, which only contain fibrous tissue [28]. True cyclops lesions are more likely to cause loss of extension since, unlike cyclopoid scars, they cannot be easily compressed. They appear on MR imaging as a well-circumscribed nodule with an average size of 10–15 mm [29] (Fig. 2.10). They are typically located in the anterior intercondylar notch and subsequently can cause impingement in extension and loss of extension. They most commonly occur at 6–12 months postoperatively after ACLR [30]. It is important to distinguish pseudocyclops lesions from cyclops lesions, as stated above [22].
Arthrofibrosis can also occur in a diffuse form and is more common in patients with poor preoperative range of motion [31]. It appears on MR imaging as hypointense fibrous tissue surrounding the graft and extending to the posterior joint capsule and possibly in the infrapatellar fat pad. This is in contrast to a distinct mass-like lesion as in the case of cyclops lesions. The differential for arthrofibrosis includes nodular synovitis (focal pigmented villonodular synovitis) and synovial chondromatosis.
Tunnel Cysts/Osteolysis
Role of CT in Cases of Suspected Tunnel Widening
It is common for small amounts of fluid to be present in the tibial and femoral graft tunnels up to 18 months after ACLR [32]. This fluid is typically reabsorbed within 18 months and does not constitute a true cyst or lead to tunnel expansion, ganglion formation, or graft failure. When tunnel cysts do form, they can occur in the pretibial space, in the tibial tunnel, and in the femoral tunnel. They can also be classified as communicating or non-communicating depending on whether they communicate with the joint space.
While their etiology is not completely understood, tunnel cysts and widening have been attributed to several causes, including excess graft motion in the tunnel, accumulation of osteolytic cytokines from synovial fluid in the tunnel secondary to incomplete graft incorporation, early accelerated rehabilitation prior to complete graft incorporation, and host response to hardware such as bioabsorbable interference screws [33, 34].
With regard to findings on imaging, plain radiographs may show tunnel widening around the fixation device [35, 36], as well as sclerotic borders identifying the geographic limits of the tunnel. MR imaging can show fluid in the tunnel, tunnel widening, or simple or loculated cysts (Fig. 2.11). These findings are most adequately visualized on STIR or fat-suppressed T2 sequences, especially since STIR images are less affected by metal artifact from certain fixation devices. These cysts extend into the pretibial space, intercondylar notch, or popliteal fossa.
CT imaging is also often used to evaluate tunnel widening and cyst formation (Fig. 2.12). One comparative study found that neither plain radiographs nor MRI was reliable in evaluating tunnel widening and found greatest intra-rater and inter-rater reliability for the evaluation of tunnel widening with CT imaging [37].
Tunnel osteolysis on CT after anterior cruciate ligament reconstruction. Sagittal (a and c) and coronal (b and d) images demonstrate examples of osteolysis of the tibial tunnel in two separate knees. Measurement of tunnels at their widest point are shown on the sagittal images (arrowheads). The first patient (a and b) was noted to have maintained cylindricity of their tunnel, whereas the second patient (c and d) was found to have a more cavitary area of bone loss
The differential for tunnel widening/osteolysis includes foreign body granulomas, which appear as a heterogenous mass that enhance with intravenous gadolinium contrast, and screw extrusion in which there will be a cyst in the tunnel but the screw will be visibly extruded from the tunnel. While there is no evidence that the development of a tunnel cyst is associated with increased rates of graft failure, it is important to note the formation of a tunnel cyst or tunnel widening on imaging for the purposes of preoperative planning for revision ACLR. In some cases, a two-stage procedure may be required with an initial bone grafting procedure followed by a second definitive ACLR once there is adequate bone stock for tunnel drilling.
Additional Factors That May Contribute to Risk of Graft Re-rupture or Recurrent Instability
Alignment
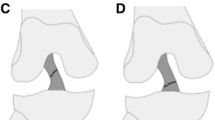
Coronal Plane
Assessment of tibiofemoral alignment in the coronal plane is a critical component of the evaluation of any patient with an ACL injury. There are several ways of assessing varus or valgus alignment. Methods include drawing the mechanical axis, which can be depicted as a line from the center of the femoral head to the center of the tibiotalar joint, and assessing whether this line passes medial or lateral to the center of the tibiofemoral joint, indicating varus or valgus alignment, respectively.
Varus alignment has been shown to increase the forces placed across both the native and reconstructed ACL, thus putting patients at risk for increased risk of ACL injury as well as ACLR failure [38]. Varus alignment combined with ACL deficiency can also lead to increased development of arthritis [39]. As a result, multiple authors have advocated for performing high tibial osteotomies (HTO), either combined or in staged fashion with revision ACLR, to address ACL deficiency, prevent or delay the progression of medial compartment osteoarthritis, and reduce the risk of revision ACLR failure. Several studies have found favorable functional and clinical outcomes with this approach [40, 41].
Tibial Sagittal Slope
Assessment of sagittal alignment is an important part of the preoperative planning process. The most commonly used parameter of sagittal alignment is posterior tibial slope (PTS), which can be measured as the angle formed by the intersection of a line parallel to the tibial shaft and another line tangential to the articular surface of the tibial plateau (Fig. 2.13).
Measurement of posterior tibial slope. A lateral radiograph (a) is shown with a measurement of the posterior tibial slope. Briefly, to identify the longitudinal axis of the tibia, a line is drawn connecting the center of the tibia at 2 points about 5 cm apart and with the distal point as distal in the tibia as possible. A second line is drawn connecting the anterior and posterior most points on the tibial plateau. The angle between a line perpendicular to the longitudinal axis of the tibia and the line tangential to the tibial plateaus is the posterior tibial slope angle, which is 9.5 degrees in this radiograph. (b) is the full-length standing film from a 24-year-old female who presented with recurrent ACL reconstruction failure after three prior ACL reconstructions. Her posterior tibial slope, which is measured in (b, c), is 16.1 degrees, and she was indicated for a closing wedge high tibial osteotomy, along with revision ACL reconstruction, to decrease her posterior tibial slope and decrease her chance of recurrent graft failure
Multiple studies have found increased rates of ACLR failure as well as primary ACL injuries with increased posterior tibial slope (PTS), with some studies identifying a particularly large increase in risk with a posterior tibial slope of 12 degrees or greater [42, 43]. Biomechanical studies have confirmed that increased forces are seen across the ACL with increased PTS [44]. As a result, several authors have suggested performing proximal tibial slope-reducing osteotomies to decrease the posterior slope in patients with excessive PTS and reduce the rate of ACLR failure [42, 45]. It remains unclear whether there is more value to measuring the PTS on the medial or lateral tibial plateau. While some authors recommended using the medial tibial plateau as it is more recognizable [46], the lateral tibial plateau PTS has also been shown to be associated with increased risk of ACL injury and ACLR failure [43, 47].
Other Sources of Persistent Instability
Meniscus Pathology
The menisci are important secondary stabilizers of the ACL-deficient knee, and meniscal injuries can increase the forces on the reconstructed ACL graft. The medial meniscus has been shown to contribute primarily to anteroposterior stability, whereas the lateral meniscus contributes more to rotatory stability by preventing anterior tibial translation during pivot-shift maneuvers involving a valgus and internal rotation load [48]. Concomitant meniscectomy with ACLR has been shown to be associated with worse clinical outcomes and increased radiographic development of osteoarthritic changes compared to ACLR alone [49]. The combination of chronic anterior tibial translation with posterior meniscus deficiency can specifically lead to increased chondral wear posteriorly. One radiographic marker of this is the “cupola” sign, or an osteophyte on the posteromedial corner of the tibia that develops in response to chronic anterior tibial translation [50]. One study of 103 patients undergoing total knee arthroplasty found that all 43 patients who had a cupola sign on preoperative radiographs were confirmed intraoperatively to have a ruptured ACL [51]. Thus, it is important to recognize meniscal pathology and perform meniscal repair when possible (Fig. 2.14), and studies have shown that lateral meniscus root repair can improve stability in the ACL-deficient knee [52].
Meniscal root injury with anterior cruciate ligament (ACL) rupture. Sagittal and coronal MRI images demonstrate an ACL tear (arrows, a) with meniscal root injury (arrowhead, a) with meniscal extrusion (arrowhead, b). Intraoperative arthroscopy confirms meniscal root injury (c, d). Meniscal root repair was performed concomitantly with ACL reconstruction (e)
There is also now increasing awareness of the importance of identifying lesions involving the peripheral attachment of the posterior medial meniscus, termed “ramp” lesions, which have been reported to be present in 9.3–17% of ACL injuries [53, 54]. These lesions can manifest as a meniscocapsular avulsion, a meniscotibial ligament avulsion, or a combination of these two. Cadaveric studies have found that ramp lesions lead to increased anterior tibial translation and external rotation in the ACL-deficient knee and that ACLR alone did not restore these parameters but ACLR with ramp repair did [55, 56]. On the other hand, one prospective randomized study of ACLR with repair of concomitant stable ramp lesions has found no difference in clinical outcomes or anterior tibial translation [57].
Although only unstable ramp lesions may require surgical intervention, it is important to identify them using MR imaging. These tend to occur in a posteromedial “blind spot,” which is difficult to view with the traditional arthroscopic portals. They can, however, easily be visualized through the Gillquist position, which will be discussed in other chapters [58]. Studies of the sensitivity of MR imaging for identifying ramp lesions report widely varying values from 0% to 84.6% [53, 59, 60], which reflects a variety of factors including that some studies only looked at the official reports in the medical record, in which ramp lesions might not have been specifically examined for. One author hypothesized that the low sensitivity of MR imaging might be related to MR imaging being performed when the knee is in extension, which can lead to the meniscocapsular separation being reduced.
Ramp lesion findings on MR imaging include the presence of a thin fluid signal between the posterior horn of the medial meniscus and adjacent posteromedial capsule, representing meniscocapsular separation [61], or may appear as a vertical longitudinal tear in the red-red zone of the medial meniscus posterior horn [62]. This can be accompanied by a high signal irregularity involving the capsular margin of the posterior horn of the medial meniscus on the fluid-sensitive images (Fig. 2.15) [63].
Arthroscopic image of ramp lesion. This image depicts a ramp lesion as seen through the Gillquist view during an arthroscopic anterior cruciate ligament reconstruction. The peripheral attachment of the posterior horn of the medial meniscus, specifically the posteromedial meniscotibial ligament, has been disrupted. MRI has varying sensitivity for detecting these lesions, and it is important to evaluate for them intraoperatively, as unstable ramp lesions may require additional surgical intervention
Anterolateral Capsular/Structural Insufficiency
There has been a large amount of interest recently in the anterolateral complex of the knee. There is increasing awareness now that traditional single-bundle ACLR may not reliably restore rotatory stability, which has been shown to have a significant effect on clinical outcomes [64, 65], and that the anterolateral complex significantly contributes to the rotatory stability of the knee [66, 67]. The anterolateral complex contains the lateral collateral ligament (LCL), the anterolateral capsule, the iliotibial band, as well as a thickening of the anterolateral capsule that has been termed the “anterolateral ligament” (ALL). While there is controversy on whether this structure constitutes a discrete ligament versus a thickening of the capsule, part of the iliotibial band, or both, evaluation of the anterolateral complex is nevertheless an important component of the preoperative planning process given its critical role in rotatory stability [68]. While there is variation in its reported appearance, the ALL has been described on MR imaging as a sheetlike structure connecting the distal femur to the proximal tibia. There is still some controversy surrounding the ALL’s origin, but most people think its origin is proximal and posterior to the LCL attachment and that it courses anteriorly and inferiorly until it inserts on the lateral meniscus and lateral tibial plateau, 6.5 mm below the articular surface [69, 70].
The reported sensitivity of MR imaging for identification of the intact ALL ranges from 11% to 100% [71, 72], and the reported incidence of concomitant ALL abnormalities with ACL injuries ranges from 33% to 90% [73,74,75]. While ultrasonography has been investigated for its utility in evaluating ALL injuries, prior studies have found contrasting results, with one study reporting 100% sensitivity for identifying ALL injuries on ultrasound [76], while others have found that ultrasound cannot even accurately identify or visualize the ALL [77].
Identification of these injuries is important because it may influence the decision to perform additional procedures during ACLR, such as extra-articular tenodesis or ALL reconstruction [78, 79]. Further work is being done to characterize the anatomy and role of the anterolateral ligament and the entire anterolateral complex, and this is an aspect of ACLR that is continuing to rapidly evolve.
Collateral Ligament Insufficiency
Evaluation of concomitant injuries to the medial collateral ligament (MCL), lateral collateral ligament (LCL), posteromedial corner, and posterolateral corner is an important component of the evaluation of the failed ACLR. Various studies have found that untreated concomitant ligamentous laxity tends to account for 3–5% of revision ACL cases [1, 80]. While these injuries can occur at the time of the initial ACL rupture, it is also important to note that concomitant ligamentous laxity can also develop over time in the ACL-deficient knee in the absence of the stabilizing effect of the ACL. The ACL has been shown to provide both valgus and varus stability, particularly in the absence of a competent medial- or lateral-sided ligamentous structures. In these chronic situations where there is ligamentous laxity without a discrete tear, especially in the setting of a history of subjective instability, stress radiography can be particularly helpful (Fig. 2.16). Prior studies have found that side-to-side differences on stress radiographs of 2.7 mm for isolated LCL, 3.2 mm for MCL, and 4 mm for PLC are suggestive of grade III ligamentous injuries [81].
Stress radiographs indicating left knee medial collateral ligament laxity. This patient was a 38-year-old male who had undergone bilateral prior anterior cruciate ligament reconstructions and presented with recurrent left knee instability and laxity to valgus stress on exam. A left knee MRI was obtained and demonstrated complete ACL graft rupture, with nonvisualization of the graft, and intact MCL (arrowhead, a). Stress radiographs were obtained and were notable for 8 mm and 12 mm of opening to valgus stress in the right (b) and left (c) knees, respectively
Conclusion
Surgeons should obtain advanced imaging as a critical component of the preoperative planning process. MR imaging is often the preferred modality for identifying various postoperative complications including graft rupture, impingement, and arthrofibrosis. CT imaging, however, is a useful adjunct and the most reliable method for assessing tunnel location and size. MR imaging can be used to both identify various causes of the failed ACLR and to diagnose additional injuries, such as ALC disruption or ramp lesions, which may require additional procedures.
References
Trojani C, Sbihi A, Djian P, Potel J-F, Hulet C, Jouve F, et al. Causes for failure of ACL reconstruction and influence of meniscectomies after revision. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):196–201.
Parkinson B, Robb C, Thomas M, Thompson P, Spalding T. Factors that predict failure in anatomic single-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(7):1529–36.
Venosa M, Delcogliano M, Padua R, Alviti F, Delcogliano A. Femoral tunnel positioning in anterior cruciate ligament reconstruction: anteromedial portal versus transtibial technique—a randomized clinical trial. Joints. 2017;5(01):034–8.
Jaecker V, Zapf T, Naendrup J-H, Pfeiffer T, Kanakamedala AC, Wafaisade A, et al. High non-anatomic tunnel position rates in ACL reconstruction failure using both transtibial and anteromedial tunnel drilling techniques. Arch Orthop Trauma Surg. 2017;137(9):1293–9.
Mehta V, Petsche T, Rawal AM. Inter-and intrarater reliability of the femoral tunnel clock-face grading system during anterior cruciate ligament reconstruction. Arthroscopy. 2017;33(2):394–7.
Rayan F, Nanjayan SK, Quah C, Ramoutar D, Konan S, Haddad FS. Review of evolution of tunnel position in anterior cruciate ligament reconstruction. World J Orthop. 2015;6(2):252.
Bernard M, Hertel P, Hornung H, Cierpinski T. Femoral insertion of the ACL. Radiographic quadrant method. Am J Knee Surg. 1997;10(1):14–21; discussion −2.
Hwang MD, Piefer JW, Lubowitz JH. Anterior cruciate ligament tibial footprint anatomy: systematic review of the 21st century literature. Arthroscopy. 2012;28(5):728–34.
Bencardino JT, Beltran J, Feldman MI, Rose DJ. MR imaging of complications of anterior cruciate ligament graft reconstruction. Radiographics. 2009;29(7):2115–26.
Scheffel PT, Henninger HB, Burks RT. Relationship of the intercondylar roof and the tibial footprint of the ACL: implications for ACL reconstruction. Am J Sports Med. 2013;41(2):396–401.
Shaffer B, Gow W, Tibone JE. Graft-tunnel mismatch in endoscopic anterior cruciate ligament reconstruction: a new technique of intraarticular measurement and modified graft harvesting. Arthroscopy. 1993;9(6):633–46.
Stäubli H-U, Rauschning W. Tibial attachment area of the anterior cruciate ligament in the extended knee position. Knee Surg Sports Traumatol Arthrosc. 1994;2(3):138–46.
Hoser C, Tecklenburg K, Kuenzel KH, Fink C. Postoperative evaluation of femoral tunnel position in ACL reconstruction: plain radiography versus computed tomography. Knee Surg Sports Traumatol Arthrosc. 2005;13(4):256–62.
Collins MS, Unruh KP, Bond JR, Mandrekar JN. Magnetic resonance imaging of surgically confirmed anterior cruciate ligament graft disruption. Skelet Radiol. 2008;37(3):233–43.
Pauzenberger L, Syré S, Schurz M. “Ligamentization” in hamstring tendon grafts after anterior cruciate ligament reconstruction: a systematic review of the literature and a glimpse into the future. Arthroscopy. 2013;29(10):1712–21.
Weiler A, Peters G, Mäurer J, Unterhauser FN, Südkamp NP. Biomechanical properties and vascularity of an anterior cruciate ligament graft can be predicted by contrast-enhanced magnetic resonance imaging: a two-year study in sheep. Am J Sports Med. 2001;29(6):751–61.
Waltz RA, Solomon DJ, Provencher MT. A radiographic assessment of failed anterior cruciate ligament reconstruction: can magnetic resonance imaging predict graft integrity? Am J Sports Med. 2014;42(7):1652–60.
Van Dyck P, Gielen JL, Vanhoenacker FM, Wouters K, Dossche L, Parizel PM. Stable or unstable tear of the anterior cruciate ligament of the knee: an MR diagnosis? Skelet Radiol. 2012;41(3):273–80.
Iriuchishima T, Shirakura K, Fu FH. Graft impingement in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):664–70.
Iriuchishima T, Shirakura K, Horaguchi T, Morimoto Y, Fu FH. Full knee extension magnetic resonance imaging for the evaluation of intercondylar roof impingement after anatomical double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(1):22–8.
Watanabe BM, Howell SM. Arthroscopic findings associated with roof impingement of an anterior cruciate ligament graft. Am J Sports Med. 1995;23(5):616–25.
Simpfendorfer C, Miniaci A, Subhas N, Winalski CS, Ilaslan H. Pseudocyclops: two cases of ACL graft partial tears mimicking cyclops lesions on MRI. Skelet Radiol. 2015;44(8):1169–73.
Papakonstantinou O, Chung CB, Chanchairujira K, Resnick DL. Complications of anterior cruciate ligament reconstruction: MR imaging. Eur Radiol. 2003;13(5):1106–17.
Bents RT, Jones RC, May DA, Snearly WS. Intercondylar notch encroachment following anterior cruciate ligament reconstruction: a prospective study. Am J Knee Surg. 1998;11(2):81–8.
May D, Snearly W, Bents R, Jones R. MR imaging findings in anterior cruciate ligament reconstruction: evaluation of notchplasty. AJR Am J Roentgenol. 1997;169(1):217–22.
Bush-Joseph CA, Bach B Jr. Migration of femoral interference screw after anterior cruciate ligament reconstruction. Am J Knee Surg. 1998;11(1):32.
Appelt A, Baier M. Recurrent locking of knee joint caused by intraarticular migration of bioabsorbable tibial interference screw after arthroscopic ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2007;15(4):378–80.
Minne C, Velleman MD, Suleman FE. MRI findings of cyclops lesions of the knee. SA Orthop J. 2012;11(2):56–60.
Zappia M, Capasso R, Berritto D, Maggialetti N, Varelli C, D’Agosto G, et al. Anterior cruciate ligament reconstruction: MR imaging findings. Musculoskelet Surg. 2017;101(1):23–35.
Gohil S, Falconer TM, Breidahl W, Annear PO. Serial MRI and clinical assessment of cyclops lesions. Knee Surg Sports Traumatol Arthrosc. 2014;22(5):1090–6.
Mayr HO, Weig TG, Plitz W. Arthrofibrosis following ACL reconstruction—reasons and outcome. Arch Orthop Trauma Surg. 2004;124(8):518–22.
Sanders TG, Tall MA, Mulloy JP, Leis HT. Fluid collections in the osseous tunnel during the first year after anterior cruciate ligament repair using an autologous hamstring graft: natural history and clinical correlation. J Comput Assist Tomogr. 2002;26(4):617–21.
Ghazikhanian V, Beltran J, Nikac V, Feldman M, Bencardino JT. Tibial tunnel and pretibial cysts following ACL graft reconstruction: MR imaging diagnosis. Skelet Radiol. 2012;41(11):1375–9.
Sprowson AP, Aldridge SE, Noakes J, Read J, Wood DG. Bio-interference screw cyst formation in anterior cruciate ligament reconstruction—10-year follow up. Knee. 2012;19(5):644–7.
Lamprakis AA, Fortis AP, Dimas A. Rejection reaction to stabilizing bolts after ACL reconstruction: a case report. Knee Surg Sports Traumatol Arthrosc. 2008;16(1):19–23.
Tsuda E, Ishibashi Y, Tazawa K, Sato H, Kusumi T, Toh S. Pretibial cyst formation after anterior cruciate ligament reconstruction with a hamstring tendon autograft. Arthroscopy. 2006;22(6):691.e1–6.
Marchant MH, Willimon SC, Vinson E, Pietrobon R, Garrett WE, Higgins LD. Comparison of plain radiography, computed tomography, and magnetic resonance imaging in the evaluation of bone tunnel widening after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18(8):1059–64.
Jan van de Pol G, Arnold MP, Verdonschot N, van Kampen A. Varus alignment leads to increased forces in the anterior cruciate ligament. Am J Sports Med. 2009;37(3):481–7.
Noyes FR, Schipplein OD, Andriacchi TP, Saddemi SR, Weise M. The anterior cruciate ligament-deficient knee with varus alignment: an analysis of gait adaptations and dynamic joint loadings. Am J Sports Med. 1992;20(6):707–16.
Zaffagnini S, Bonanzinga T, Grassi A, Muccioli GMM, Musiani C, Raggi F, et al. Combined ACL reconstruction and closing-wedge HTO for varus angulated ACL-deficient knees. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):934–41.
Noyes FR, Barber-Westin SD, Hewett TE. High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med. 2000;28(3):282–96.
Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament–reconstructed patient. Am J Sports Med. 2013;41(12):2800–4.
Christensen JJ, Krych AJ, Engasser WM, Vanhees MK, Collins MS, Dahm DL. Lateral tibial posterior slope is increased in patients with early graft failure after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(10):2510–4.
McLean SG, Oh YK, Palmer ML, Lucey SM, Lucarelli DG, Ashton-Miller JA, et al. The relationship between anterior tibial acceleration, tibial slope, and ACL strain during a simulated jump landing task. J Bone Joint Surg. 2011;93(14):1310–7.
Dejour D, Saffarini M, Demey G, Baverel L. Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2846–52.
Dejour H, Bonnin M. Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg Br. 1994;76(5):745–9.
Rahnemai-Azar AA, Yaseen Z, van Eck CF, Irrgang JJ, Fu FH, Musahl V. Increased lateral tibial plateau slope predisposes male college football players to anterior cruciate ligament injury. J Bone Joint Surg Am. 2016;98(12):1001–6.
Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2010;38(8):1591–7.
Wu WH, Hackett T, Richmond JC. Effects of meniscal and articular surface status on knee stability, function, and symptoms after anterior cruciate ligament reconstruction: a long-term prospective study. Am J Sports Med. 2002;30(6):845–50.
Brunkhorst J, Johnson DL. Radiographic evidence of anterior cruciate ligament insufficiency. Orthopedics. 2014;37(11):759–62.
Mullis BH, Karas SG, Kelley SS. Characterization of a consistent radiographic finding in chronic anterior cruciate ligament deficiency: the posteromedial osteophyte. Am J Orthop (Belle Mead NJ). 2007;36(9):494.
Forkel P, von Deimling C, Lacheta L, Imhoff FB, Foehr P, Willinger L, et al. Repair of the lateral posterior meniscal root improves stability in an ACL-deficient knee. Knee Surg Sports Traumatol Arthrosc. 2018;26(8):2302–9.
Bollen S. Posteromedial meniscocapsular injury associated with rupture of the anterior cruciate ligament: a previously unrecognised association. J Bone Joint Surg. 2010;92(2):222–3.
Liu X, Feng H, Zhang H, Hong L, Wang XS, Zhang J. Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med. 2011;39(4):832–7.
Stephen JM, Halewood C, Kittl C, Bollen SR, Williams A, Amis AA. Posteromedial meniscocapsular lesions increase tibiofemoral joint laxity with anterior cruciate ligament deficiency, and their repair reduces laxity. Am J Sports Med. 2016;44(2):400–8.
Peltier A, Lording T, Maubisson L, Ballis R, Neyret P, Lustig S. The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2967–73.
Liu X, Zhang H, Feng H, Hong L, Wang X-s, Song G-Y. Is it necessary to repair stable ramp lesions of the medial meniscus during anterior cruciate ligament reconstruction? A prospective randomized controlled trial. Am J Sports Med. 2017;45(5):1004–11.
Strobel MJ. Manual of arthroscopic surgery. Berlin: Springer Science & Business Media; 2013.
Arner JW, Herbst E, Burnham JM, Soni A, Naendrup J-H, Popchak A, et al. MRI can accurately detect meniscal ramp lesions of the knee. Knee Surg Sports Traumatol Arthrosc. 2017;25(12):3955–60.
Edgar C, Ware J, Obopilwe E, Ziegler C, Reed D, Arciero R, editors. Posteromedial meniscocapsular tear: prevalence, detection sensitivity, biomechanics, and repair technique. AAOS Annual Meeting; 2016.
Hash TW. Magnetic resonance imaging of the knee. Sports Health. 2013;5(1):78–107.
Greif DN, Baraga MG, Rizzo MG, Mohile NV, Silva FD, Fox T, et al. MRI appearance of the different meniscal ramp lesion types, with clinical and arthroscopic correlation. Skelet Radiol. 2020;49:677.
Hatayama K, Kimura M, Ogoshi A, Takagishi K, editors. Ramp lesion associated with anterior cruciate ligament rupture. International society of arthroscopy, knee surgery and orthopaedic sports medicine biennial congress, Toronto, Canada; 2013.
Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ. Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(3):629–34.
Ayeni OR, Chahal M, Tran MN, Sprague S. Pivot shift as an outcome measure for ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):767–77.
Nitri M, Rasmussen MT, Williams BT, Moulton SG, Cruz RS, Dornan GJ, et al. An in vitro robotic assessment of the anterolateral ligament, part 2: anterolateral ligament reconstruction combined with anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(3):593–601.
Musahl V, Rahnemai-Azar AA, Costello J, Arner JW, Fu FH, Hoshino Y, et al. The influence of meniscal and anterolateral capsular injury on knee laxity in patients with anterior cruciate ligament injuries. Am J Sports Med. 2016;44:3126.
Musahl V, Herbst E, Burnham JM, Fu FH. The anterolateral complex and anterolateral ligament of the knee. J Am Acad Orthop Sur. 2018;26(8):261–7.
Helito CP, Demange MK, Bonadio MB, Tírico LEP, Gobbi RG, Pécora JR, et al. Anatomy and histology of the knee anterolateral ligament. Orthop J Sports Med. 2013;1(7):2325967113513546.
Helito CP, Helito PVP, Costa HP, Bordalo-Rodrigues M, Pecora JR, Camanho GL, et al. MRI evaluation of the anterolateral ligament of the knee: assessment in routine 1.5-T scans. Skelet Radiol. 2014;43(10):1421–7.
Taneja AK, Miranda FC, Braga CA, Gill CM, Hartmann LG, Santos DC, et al. MRI features of the anterolateral ligament of the knee. Skelet Radiol. 2015;44(3):403–10.
Kosy JD, Mandalia VI, Anaspure R. Characterization of the anatomy of the anterolateral ligament of the knee using magnetic resonance imaging. Skelet Radiol. 2015;44(11):1647–53.
Van Dyck P, Clockaerts S, Vanhoenacker FM, Lambrecht V, Wouters K, De Smet E, et al. Anterolateral ligament abnormalities in patients with acute anterior cruciate ligament rupture are associated with lateral meniscal and osseous injuries. Eur Radiol. 2016;26(10):3383–91.
Claes S, Bartholomeeusen S, Bellemans J. High prevalence of anterolateral ligament abnormalities in magnetic resonance images of anterior cruciate ligament-injured knees. Acta Orthop Belg. 2014;80(1):45–9.
Helito CP, Helito PVP, Costa HP, Demange MK, Bordalo-Rodrigues M. Assessment of the anterolateral ligament of the knee by magnetic resonance imaging in acute injuries of the anterior cruciate ligament. Arthroscopy. 2017;33(1):140–6.
Cavaignac E, Wytrykowski K, Reina N, Pailhé R, Murgier J, Faruch M, et al. Ultrasonographic identification of the anterolateral ligament of the knee. Arthroscopy. 2016;32(1):120–6.
Capo J, Kaplan DJ, Fralinger DJ, Adler RS, Campbell KA, Jazrawi LM, et al. Ultrasonographic visualization and assessment of the anterolateral ligament. Knee Surg Sports Traumatol Arthrosc. 2017;25(10):3134–9.
Dodds A, Gupte C, Neyret P, Williams A, Amis A. Extra-articular techniques in anterior cruciate ligament reconstruction: a literature review. J Bone Joint Surg. 2011;93(11):1440–8.
Sonnery-Cottet B, Thaunat M, Freychet B, Pupim BH, Murphy CG, Claes S. Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am J Sports Med. 2015;43(7):1598–605.
Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med. 2012;40(7):1551–7.
James EW, Williams BT, LaPrade RF. Stress radiography for the diagnosis of knee ligament injuries: a systematic review. Clin Orthop Relat Res. 2014;472(9):2644–57.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Kanakamedala, A.C., Gipsman, A.M., Alaia, M.J., Alaia, E.F. (2022). Radiographic Workup of the Failed ACLR. In: Alaia, M.J., Jones, K.J. (eds) Revision Anterior Cruciate Ligament Reconstruction. Springer, Cham. https://doi.org/10.1007/978-3-030-96996-7_2
Download citation
DOI: https://doi.org/10.1007/978-3-030-96996-7_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-96995-0
Online ISBN: 978-3-030-96996-7
eBook Packages: MedicineMedicine (R0)