Abstract
Objective
To determine the frequency of anterolateral ligament (ALL) injury in patients with acute anterior cruciate ligament (ACL) rupture and to analyse its associated injury patterns.
Methods
Ninety patients with acute ACL rupture for which MRI was obtained within 8 weeks after the initial trauma were retrospectively identified. Two radiologists assessed the status of the ALL on MRI by consensus. The presence or absence of an ALL abnormality was compared with the existence of medial and lateral meniscal tears diagnosed during arthroscopy. Associated collateral ligament and osseous injuries were documented with MRI.
Results
Forty-one of 90 knees (46 %) demonstrated ALL abnormalities on MRI. Of 49 knees with intact ALL, 15 (31 %) had a torn lateral meniscus as compared to 25 torn lateral menisci in 41 knees (61 %) with abnormal ALL (p = 0.008). Collateral ligament (p ≤ 0.05) and osseous injuries (p = 0.0037) were more frequent and severe in ALL-injured as compared with ALL-intact knees.
Conclusion
ALL injuries are fairly common in patients with acute ACL rupture and are statistically significantly associated with lateral meniscal, collateral ligament and osseous injuries.
Key Points
• ALL injuries are fairly common in patients with acute ACL rupture.
• ALL injuries are highly associated with lateral meniscal and osseous injuries.
• MRI assessment of ACL-injured knees should include evaluation of the ALL.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Although various injury mechanisms may occur, acute anterior cruciate ligament (ACL) ruptures most often result from twisting, non-contact injuries, which have a pivot-shift-like mechanism, consisting of anterior tibial subluxation and excess internal tibial rotation [1, 2]. Once the ACL tears, the menisci can be torn by either entrapment between the tibia and femur or tension transmitted to them by the posterior capsuloligamentous structures [3]. The lateral meniscus is frequently involved since it provides a restraint to rotational forces under pivot-shift loading of the knee [4].
The recent ‘rediscovery’ of the anterolateral ligament (ALL) yields a breakthrough for diagnosing and treating problematic rotational knee instability. In brief, the ALL was recently identified as a distinct component of the anterolateral knee capsule [5–9]. Biomechanical studies demonstrated that an injury to the ALL significantly affects the pivot shift, previously attributed to injuries of the posterolateral bundle of the ACL [10, 11]. This may change the clinical approach towards ACL-injured subjects with a high-grade pivot shift [12]. Consequently, an additional anatomic reconstruction of the ALL, concomitant to the ACL, is regaining popularity [13, 14]. However, clinical [15] and arthroscopic [16] assessment of the ALL is difficult.
Few studies have used MRI to identify the ALL [17–21]. Claes et al. reported a high frequency of combined ALL and ACL abnormalities (79 %) [22]. These results, however, have not yet been confirmed by other authors. Thus the present study was performed to determine the frequency of ALL injury in patients with acute ACL rupture and to analyse its associated meniscal, collateral ligament and osseous injuries. The hypothesis was that, given the various ACL injury mechanisms, the frequency of combined ALL and ACL ruptures would probably be lower than previously reported. It was also hypothesised that, given the role of the ALL in the pivot shift, lateral meniscal and osseous injuries might be more common in ALL-injured knees as compared with knees with an intact ALL.
Materials and methods
Patient selection
This study was approved by the hospital ethics committee and patient consent was not required. The medical records of 634 patients who underwent both MRI and arthroscopy of the knee in our institution between June 2009 and November 2014 were identified retrospectively. Subjects were included in our study if they had: first, an arthroscopically proven ACL rupture for which MRI was obtained within 8 weeks after the initial trauma; second, an available medical record with relevant history and clinical assessment (anterior drawer, Lachman and/or pivot-shift test); third, no history of knee surgery; fourth, subsequent arthroscopy within 90 days after the MRI. In total, 113 of the 634 patients met these criteria. The ALL could not reliably be assessed on MRI in 23 of the 113 patients, and these were excluded from the study: (1) patients with an MRI study of suboptimal quality (n = 6), (2) patients with confounding knee pathologies affecting imaging of the knee’s lateral compartment (i.e. clinical signs of posterolateral instability, signs of degenerative osteoarthritis) (n = 9) and (3) patients without identifiable ALL in the absence of oedema (n = 8). Thus, we identified a group of 90 patients (66 male; age range 17–59 years, median age 32 years; right knee, n = 45) as the patient population of this study. The knee injury had been sustained during soccer (n = 30), skiing (n = 22), a fall (n = 14), a motor-vehicle accident (n = 10), basketball (n = 4), gymnastics (n = 4) and other (n = 6).
MRI technique
Thirty-eight patients underwent knee MRI on a 1.5-T system (Magnetom Symphony Tim, Siemens, Erlangen, Germany) and 52 patients on a 3-T system (Magnetom Trio Tim, Siemens, Erlangen, Germany).
Imaging parameters at 1.5 T included: axial and coronal fat-saturated (FS) TSE intermediate weighted (TR/TE = 3000-3590/28 ms, ST 3 mm and TF 7); coronal TSE T1 weighted (TR/TE = 500/14 ms, ST 3 mm and TF 2); sagittal TSE proton density and T2 weighted (TR/TE = 3340/21-85 ms, ST 3 mm and TF 5). All images were acquired with a matrix size 307 × 384, FOV 160 mm and 10 % gap.
Imaging parameters at 3 T included: axial and coronal FS TSE intermediate weighted (TR/TE = 3400-3670/25 ms, ST 3 mm, matrix 328/358 × 448 and TF 7); coronal TSE T1 weighted (TR/TE = 514/12 ms, ST 3 mm, matrix 279 × 448 and TF 2); sagittal TSE proton density and T2 weighted (TR/TE = 4700/21-89 ms, ST 2 mm, matrix 448 × 448 and TF 5). All images were acquired with an FOV 160 mm and 10 % gap.
Image analysis
All MRI examinations were reviewed by two radiologists [with 25 years (JLG) and 12 years (VL) of experience in musculoskeletal radiology at the time of the study] in consensus on a picture archiving and communication system (BARCO, Kortrijk, Belgium). Images were reviewed without any annotation. At the time of review, the readers were informed that the patient had an arthroscopically confirmed diagnosis of an acute ACL tear, but they were blinded to other arthroscopic findings.
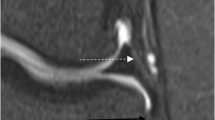
On MRI, the ALL was normal if low signal intensity fibres were seen from the lateral femoral epicondyle inserting to the anterolateral tibia [17–22]. The ALL was abnormal in the case of complete disruption of the ligament, if the contour of the ALL was irregular, if ligamentous oedema existed or if a combination of these MRI features was observed. If only peri-ligamentous oedema existed, with identifiable, continuous low signal intensity fibres, the ALL was considered intact. ALL abnormalities were classified as ‘proximal’ (above the meniscus), ‘distal’ (below the meniscus) or ‘both’. Bony ALL avulsions at the level of the tibia were categorised as ‘Segond’ fractures [9, 17, 20]. Figure 1 illustrates examples of normal and abnormal ALLs.
The anterolateral ligament (ALL) of the knee on coronal proton density-weighted images with fat saturation demonstrating its proximal meniscofemoral (arrow) and distal meniscotibial (arrowhead) components. All images were obtained at a level slightly posterior to the iliotibial tract (*) and anterior to the origin of the lateral collateral ligament. In a, a normal ALL is shown with both components attached to the lateral meniscus. In b, a proximal ALL lesion is shown with disruption and signal abnormality in the meniscofemoral component. The distal ALL is intact. In c, disruption and signal abnormality of the ALL are demonstrated in both its proximal and distal component. In d, a distal bony avulsion (curved arrow) of the ALL is seen (Segond fracture)
Widely accepted MRI criteria for the diagnosis of meniscal tear were used [23, 24]. If a meniscal tear was diagnosed on MRI, the readers localised tears in the anterior horn, body or posterior horn. No attempt was made to classify meniscal tear patterns as this is frequently difficult on MRI [25].
The medial and lateral collateral ligaments were graded (0–3) according to Schweitzer et al. [26], and only grade 2 and 3 injuries were considered tears for the purpose of this study.
Osseous injuries including bone contusions and (cortical depression and trabecular) fractures were located on the lateral and medial femoral condyle as well as the lateral and medial tibial plateau. Injuries were classified as anterior, central and posterior and were counted separately. The size of traumatic bone contusions was graded according to the classification system proposed by Brittberg and Winalski [27].
False-negative and false-positive MR diagnoses for lateral meniscal tear were evaluated in consensus again with knowledge of the arthroscopic findings and the original MRI diagnoses.
To determine the reliability of the ALL assessments, two independent radiologists [(FMV) and (PVD) with 25 years and 13 years of experience in musculoskeletal radiology at the time of the study, respectively], who were not readers in the study, reviewed MR images twice, with a 3-weeks interval, for 40 patients who were randomly selected from the study group by the sample ( ) function in R.
Arthroscopic surgery technique
All patients in the study group underwent knee arthroscopy, confirming ACL tear. If present, a meniscal tear was located in the anterior horn, body or posterior horn and classified as vertical (longitudinal, oblique, radial, bucket handle), horizontal or complex tears.
Statistical analysis
All patients were classified according to ALL status, and lesion locations were tabulated. All injuries were summarised using frequencies and were then correlated with the status of the ALL. Evaluation of the relationship between categorical variables was performed by the chi-square test, and Fisher’s exact test was used in cases of a small sample size. Bonferroni-Holm correction was used for multiple testing. Pairwise Wilcoxon test was used to compare the size of the bone contusions. Injuries of the menisci were confirmed with arthroscopy, and collateral ligament and osseous injuries were diagnosed with MRI. Kappa (κ)-values were measured to assess inter- and intra-reader agreement for determining the presence or absence of an ALL abnormality on MRI. The κ-values were interpreted according to the recommendations by Landis and Koch [28]. Statistical analysis was performed by a statistician (KW) with the use of R software (version 3.1.1.; R Foundation for Statistical Computing, Vienna, Austria). A difference was considered statistically significant if p was less than 0.05.
Results
Frequency and location of ALL abnormalities
Forty-one of the 90 knees (46 %; 95 % CI 35-56 %) demonstrated ALL abnormalities on MRI. In 29 of the 41 lesions (71 %), the distal component of the ALL was involved. Fifteen of 41 ALL lesions (37 %) were bony avulsions or Segond fractures (17 % of ACL injuries) (Table 1).
ALL abnormalities and meniscal injuries
Thirty-nine medial meniscal tears (all posterior horn) and 40 lateral meniscal tears (anterior horn n = 3, body n = 3, posterior horn n = 34) were diagnosed by arthroscopy. Tear patterns for the medial meniscus were peripheral vertical (n = 17), oblique (n = 8), bucket handle (n = 4), horizontal (n = 3) and complex (n = 7) and for the lateral meniscus were peripheral vertical (n = 15), oblique (n = 14), bucket handle (n = 1), radial (n = 7), horizontal (n = 2) and complex (n = 1). Of 49 knees with an intact ALL, 15 (31 %) had a torn lateral meniscus, as compared to 25 torn lateral menisci in 41 knees (61 %) with an abnormal ALL (Figs. 2 and 3). There was a significant association between ALL injury and a tear of the lateral meniscus (p = 0.008). No statistically significant association was found between ALL abnormalities and tears of the medial meniscus (p = 0.75) (Table 2). After retrospective re-review, seven lateral meniscal tears (body n = 1, posterior horn n = 6) were missed on MRI, three of which had an associated ALL abnormality (Fig. 4). Five of the seven missed lateral meniscal tears could be seen in retrospect (interpretation errors), including two with associated Segond fracture. Two lateral meniscal tears were unavoidably missed. There were two false-positive MR diagnoses for lateral meniscal tear. Both of these had an associated ALL abnormality and showed definite MRI signs of meniscal tear on retrospective re-review.
A 31-year-old male with an acute knee injury while playing basketball. a Coronal proton density-weighted image with fat saturation shows abnormal ALL (arrow). Note associated tear of the lateral meniscus (arrowhead). Bone contusions in the lateral and medial knee compartment (*) and medial collateral ligament (MCL) injury (curved arrow) are also seen. b Sagittal proton density-weighted image shows complete tear of the anterior cruciate ligament (ACL) and large synovial effusion. Peripheral longitudinal tears in the posterior horn of the medial (c) and lateral meniscus (d) (arrows) are clearly visible and were confirmed during arthroscopy. Bone contusion and cortical depression fracture at the lateral femoral condyle are also seen (arrowhead)
A 24-year-old male who tore his ACL while playing football. Coronal proton density-weighted image with fat saturation shows normal appearance of the ALL (arrow). ACL tear (arrowhead) and mild MCL sprain (curved arrow) are also seen. Note normal meniscal appearance, which was confirmed on arthroscopy
A 32-year-old male with an acute knee injury while playing football. a Coronal T1-weighted image shows abnormal ALL with Segond avulsion fracture (arrow). Note the intact anterior arm of the biceps femoris inferior to it (arrowhead). Bone contusion in the lateral tibia (*), ACL tear (curved arrow) and MCL injury (double arrow) are also seen. b Sagittal proton density-weighted image shows questionable signal change in the posterior horn of the lateral meniscus (arrow). Also note bone contusion at the posterolateral tibia (arrowhead) and marked joint effusion (*). A peripheral longitudinal tear in the posterior horn of the lateral meniscus was confirmed during arthroscopy
ALL abnormalities and collateral ligament injuries
A significant association was found between ALL and lateral collateral ligament (LCL) injuries (p = 0.0037). The association between ALL and medial collateral ligament (MCL) injuries was of borderline significance (p = 0.054) (Table 3).
ALL abnormalities and osseous injuries
The overall frequencies of bone contusions were higher in the ALL-injured as compared with ALL-intact knees, reaching significance at the anterior aspect of the lateral femoral condyle (p = 0.014), central and posterior aspects of the lateral tibia (p ≤ 0.013) and posterior aspect of the medial tibia (p = 0.0001) (Table 4). The size of the bone contusions was significantly larger in ALL-injured as compared with ALL-intact knees at the lateral femoral condyle (p ≤ 0.0024) and the lateral and medial aspects of the tibia (p = 0.0001). Forty-two of the 90 patients had an associated fracture (central aspect of the lateral femoral condyle, n = 22; posterior aspect of the lateral tibia, n = 16; posterior aspect of the medial tibia, n = 4). Of these, 30 (71 %) had concomitant ALL injury (p < 0.0001).
Inter- and intra-reader reliability of ALL assessment
There was good inter-reader agreement for determining the presence of an ALL abnormality on MRI (κ = 0.79). Intra-reader agreement was good for both readers (κ = 0.79 and 0.74).
Discussion
Our study shows that patients diagnosed with an acute ACL injury often demonstrate associated abnormalities of the ALL on MRI. It also shows that ALL injuries are significantly associated with lateral meniscal and osseous injuries.
The enigma surrounding the ALL is reflected in confusing names such as 'mid-third lateral capsular ligament' [29], ‘anterior oblique band of the LCL’ [30] or ‘capsulo-osseous layer of the iliotibial band’ [31]. However, as recently described by Porrino et al. [17], all of these names refer to different components of the same structure, the ALL.
The mechanism of injury is the most important factor to predict the structural abnormalities that can be expected [3]. Although pivot-shift injuries are common, other ACL mechanisms have been proposed, including flexion valgus and external rotation and pure valgus, typically not affecting the lateral supporting structures [1, 2]. In our study, 46 % of our patients had combined ALL and ACL injury, suggesting that these injuries often share a common mechanism of injury, characterised by excessive internal tibial torque. This was evidenced by the specific location of contusions, most frequently occurring at the anterior and central portion of the lateral femoral condyle, at the central portion of the medial femoral condyle and at the posterior portions of the lateral (and medial) tibia. However, we found MCL injuries to be more common than ALL injuries (61 % and 46 %, respectively). This finding suggests that valgus with external rotation and pure valgus injuries were also common mechanisms of ACL rupture.
The 46 % of combined ALL and ACL injuries in our study is much lower than the 79 % found by Claes et al. [22]. Aside from the injury mechanisms that may have been different, other factors may account for these different results. First, MRIs for our patients were obtained within 8 weeks after trauma. Claes et al. possibly used a longer time interval for their patients and thus patients with an unstable knee owing to an ACL tear might have sustained new ALL lesions before the MRI was performed. Second, whereas Claes et al. also included MR grade 1 (‘peri-ligamentous oedema’) as positive for ALL tear, we only considered grades 2 and 3 as positive for a tear as these can be assessed more reliably on MRI. Third, images in our study were interpreted by two radiologists, whereas MR interpretations in their study were performed by orthopaedic surgeons.
In our study, the distal component of the ALL was involved in most lesions (71 %). This result is not surprising. With the ALL originating at the lateral femoral epicondyle and the transepicondylar axis being the best representation of the knee’s optimal flexion-extension axis, the ALL’s lever arm becomes larger with increasing distance from the lateral femoral epicondyle [32]. Thus, damage to the ALL is likely to occur distally.
Fifteen of 90 of our patients were diagnosed with Segond fractures. Recently, a direct link between the ALL tibial attachment and Segond fracture was found, and in fact, the latter should be seen as ‘the tip of the iceberg’ for lesions of the ALL [33]. These findings suggest that, similar to the clinical significance of the Segond fracture [34], any ALL lesion should be seen as an important indicator of internal derangement of the knee joint.
We could identify the ALL with MRI in 80 % of our study patients. This value compares well with previously reported detection rates on MRI in the uninjured knee, ranging between 72 % and 93 % [11, 17, 19, 21]. Taneja et al. [18] reported lower visibility of the ALL on MRI (51 %). However, these authors included postoperative and chronically injured knees in their study, probably making it more difficult to visualise the ALL. Our experience suggests that, in the acutely injured knee, the ALL is readily apparent on MRI because of the articular distension associated with the acute ACL rupture. We agree with Porrino et al. [17] and others [18, 19, 21] that the femoral portion of the ALL is less easily seen on MRI because of its close association with the femoral origin of the LCL. In contrast, the distal ALL can be visualised with relative ease.
Our study found a significant association between ALL injury and tears of the lateral meniscus. However, we can only hypothesise about the causal relationship between the two. Vincent et al. [7] theorised that, following avulsion of the ALL from the proximal tibia, further anterolateral tibial displacement could result in tension on the meniscus from the ALL’s remaining femoral attachment. This force may contribute to tearing of the lateral meniscus, still anchored at its roots. Alternatively, lateral meniscal injury may further destabilise the ACL-deficient knee [4], thus leading to ALL injury. Further research in this regard is needed.
The results of our study disagree with the findings of De Maeseneer et al. [20]. These authors only found medial meniscal tears to be associated with Segond fractures. However, that study was limited by its small sample size and lack of arthroscopic correlation.
In the setting of acute ACL injury, MRI has lower sensitivity for the detection of lateral meniscal tears compared with medial meniscal tears [24, 35]. To increase the radiologist’s diagnostic confidence about the presence of a lateral meniscal tear, several secondary or indirect MRI signs of a lateral meniscal tear have been reported (e.g. abnormal superior meniscopopliteal fascicle) [36]. In our study, seven lateral meniscal tears were missed, three of which had an associated ALL abnormality (Segond fracture). The results of our study suggest that, if ALL injury is present in a patient with an ACL tear, radiologists should carefully search for a lateral meniscal tear. However, one should not diagnose a tear only on the basis of an abnormal ALL because this sign is not specific for a tear. There were two false-positive MRI diagnoses of lateral meniscal tear in our study. We cannot determine with certainty whether these two were healed tears or were tears missed during arthroscopy.
Our study found more frequent osseous injuries in knees with an abnormal ALL as compared with ALL-intact knees. Interestingly, a highly significant association was found between ALL injuries and osseous contusions of the posteromedial tibia. These medial contusions suggest a higher-energy injury than those involving only the lateral compartment [2]. A contrecoup impact after the initial injury on the lateral compartment via a pivot-shift mechanism has been proposed to explain these medial contusions [2, 3]. The significant association of ALL and collateral ligament injuries found in our study further supports this theory. The higher frequency of osseous fractures in patients with combined ALL and ACL injury in our study is of clinical importance, as fractures are considered a more important risk factor for a suboptimal clinical outcome than the presence or degree of osseous contusion [37].
It is clear that the rapid increase in knowledge of the ALL has stimulated further research to improve ACL surgical results. The poor results of previous extra-articular lateral tenodesis (LET) are now explained by an empirical, non-anatomic LET [12–14]. Although anatomic ALL reconstruction techniques are in clinical use, long-term and comparative follow-up studies are further required to determine whether treatment of the ALL improves surgical ACL outcomes [13, 14].
There were several limitations to this retrospective study. First, we acknowledge the limitations of MRI as a reference standard for ALL assessment. However, clinical testing of rotatory laxity is subjective [15], and arthroscopy only provides indirect evidence of ALL injury [16]. Direct arthroscopic assessment of the ALL was recently described anecdotally [38], but visualisation was limited to its proximal part. Second, we did not compare 1.5- and 3-T images to assess ALL visibility. In a previous study [18], comparable ALL detection rates were found at both field strengths. Third, it may be that acute meniscal tears could not be differentiated from chronic meniscal tears. Given the short time interval between the MRI and initial trauma as well as the arthroscopic tear patterns, the injuries found in our study were likely to be related to the acute trauma. Fourth, only a minority of our patients (12 %) had concomitant LCL injury. Patients with clinical signs of posterolateral corner injury were excluded because this may affect imaging of the knee’s lateral compartment. Moreover, posterolateral knee instability is far less frequent than ALRI [3, 5]. Fifth, we used an imperfect reference standard in arthroscopy to assess the menisci [23].
In conclusion, ALL injuries are fairly common in patients with acute ACL rupture and are statistically significantly associated with lateral meniscal, collateral ligament and osseous injuries. Given the importance of the ALL to ACL injuries, radiologists should not overlook the pathology of the ALL when reviewing MR images of the ACL-deficient knee.
Abbreviations
- ALL:
-
Anterolateral ligament
- ACL:
-
Anterior cruciate ligament
- ALRI:
-
Anterolateral rotatory instability
- LCL:
-
Lateral collateral ligament
- LET:
-
Lateral extra-articular tenodesis
References
Oh YK, Lipps DB, Ashton-Miller JA, Wojtys EM (2012) What strains the anterior cruciate ligament during a pivot landing? Am J Sports Med 40:574–83
Yoon KH, Yoo JH, Kim KI (2011) Bone contusion and associated meniscal and medial collateral ligament injury in patients with anterior cruciate ligament rupture. J Bone Joint Surg Am 93:1510–8
MacMahon PJ, Palmer WE (2011) A biomechanical approach to MRI of acute knee injuries. AJR Am J Roentgenol 197:568–77
Shybut TB, Vega CE, Haddad J et al (2015) Effect of lateral meniscal root tear on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 43:905–11
Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J (2013) Anatomy of the anterolateral ligament of the knee. J Anat 223:321–8
Stijak L, Bumbaširević M, Radonjić V et al (2014) Anatomic description of the anterolateral ligament of the knee. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3422-6
Vincent JP, Magnussen RA, Gezmez F et al (2012) The anterolateral ligament of the human knee: an anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc 20:147–52
Caterine S, Litchfield R, Johnson M, Chronik B, Getgood A (2014) A cadaveric study of the anterolateral ligament: re-introducing the lateral capsular ligament. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3117-z
Dodds AL, Halewood C, Gupte CM, Williams A, Amis AA (2014) The anterolateral ligament: anatomy, length changes and association with the Segond fractures. Bone Joint J 96-B:325–31
Parsons EM, Gee AO, Spiekerman C, Cavanagh PR (2015) The biomechanical function of the anterolateral ligament of the knee. Am J Sports Med 43:669–74
Van der Watt L, Khan M, Rothrauff BB et al (2015) The structure and function of the anterolateral ligament of the knee: a systematic review. Arthroscopy 31:569–582.e3
Dodds AL, Gupte CM, Neyret P, Williams AM, Amis AA (2011) Extra-articular techniques in anterior cruciate ligament reconstruction: a literature review. J Bone Joint Surg (Br) 93:1440–8
Sonnery-Cottet B, Thaunat M, Freychet B, Pupim BHB, Murphy CG, Claes S (2015) Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am J Sports Med 43:1598–605
Mackay GM, Blyth MJ, Anthony I, Hopper GP, Ribbans WJ (2015) A review of ligament augmentation with the InternalBrace™: the surgical principle is described for the lateral ankle ligament and ACL repair in particular, and a comprehensive review of other surgical applications and techniques is presented. Surg Technol Int 26:239–55
Lopomo N, Zaffagnini S, Amis AA (2013) Quantifying the pivot shift test: a systematic review. Knee Surg Sports Traumatol Arthrosc 21:767–83
LaPrade RF, Gilbert TJ, Bollom TS, Wentorf F, Chaljub G (2000) The magnetic resonance imaging appearance of individual structures of the posterolateral knee. A prospective study of normal knees and knees with surgically verified grade III injuries. Am J Sports Med 28:191–9
Porrino J Jr, Maloney E, Richardson M, Mulcahy H, Ha A, Chew FS (2015) The anterolateral ligament of the knee: MRI appearance, association with the Segond fracture, and historical perspective. AJR Am J Roentgenol 204:367–73
Taneja AK, Miranda FC, Braga CA et al (2015) MRI features of the anterolateral ligament of the knee. Skelet Radiol 44:403–10
Helito CP, Helito PV, Costa HP et al (2014) MRI evaluation of the anterolateral ligament of the knee: assessment in routine 1.5-T scans. Skelet Radiol 43:1421–7
De Maeseneer M, Boulet C, Willekens I et al (2015) Segond fracture: involvement of the iliotibial band, anterolateral ligament, and anterior arm of the biceps femoris in knee trauma. Skelet Radiol 44:413–21
Kosy JD, Mandalia VI, Anaspure R (2015) Characterization of the anatomy of the anterolateral ligament of the knee using magnetic resonance imaging. Skelet Radiol 44:1647–53
Claes S, Bartholomeeusen S, Bellemans J (2014) High prevalence of anterolateral ligament abnormalities in magnetic resonance images of anterior cruciate ligament-injured knees. Acta Orthop Belg 80:45–9
Sanders TG, Miller MD (2005) A systematic approach to magnetic resonance imaging interpretation of sports medicine injuries of the knee. Am J Sports Med 33:131–48
Oei EH, Nikken JJ, Verstijnen AC, Ginai AZ, Hunink MG (2003) MR imaging of the menisci and cruciate ligaments: a systematic review. Radiology 226:837–48
Jee WH, McCauley TR, Kim JM, Jun DJ, Lee YJ, Choi BG et al (2003) Meniscal tear configurations: categorization with MR imaging. AJR Am J Roentgenol 180:93–7
Schweitzer ME, Tran D, Deely DM, Hume EL (1995) Medial collateral ligament injuries: evaluation of multiple signs, prevalence and location of associated bone bruises, and assessment with MR imaging. Radiology 194:825–9
Brittberg M, Winalski CS (2003) Evaluation of cartilage injuries and repair. J Bone Joint Surg Am 85-A:58–69
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–74
Hughston JC, Andrews JR, Cross MJ, Moschi A (1976) Classification of knee ligament instabilities. Part II. The lateral compartment. J Bone Joint Surg Am 58:173–9
Campos JC, Chung CB, Lektrakul N, Pedowitz R, Trudell D, Yu J et al (2001) Pathogenesis of the Segond fracture: anatomic and MR imaging evidence of an iliotibial tract or anterior oblique band avulsion. Radiology 219:381–6
Terry GC, Hughston JC, Norwood LA (1986) The anatomy of the iliopatellar band and iliotibial tract. Am J Sports Med 14:39–45
Churchill DL, Incavo SJ, Johnson CC, Beynnon BD (1998) The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res 356:111–8
Claes S, Luyckx T, Vereecke E, Bellemans J (2014) The Segond fracture: a bony injury of the anterolateral ligament of the knee. Arthroscopy 30:1475–82
Hess T, Rupp S, Hopf T, Gleitz M, Liebler J (1994) Lateral tibial avulsion fractures and disruptions to the anterior cruciate ligament: a clinical study of their incidence and correlation. Clin Orthop Relat Res 303:193–7
Savoye PY, Ravey JN, Dubois C et al (2011) Magnetic resonance diagnosis of posterior horn tears of the lateral meniscus using a thin axial plane: the zip sign – a preliminary study. Eur Radiol 21:151–9
Blankenbaker DG, De Smet AA, Smith JD (2002) Usefulness of two indirect MR imaging signs to diagnose lateral meniscal tears. AJR Am J Roentgenol 178:579–782
Kijowski R, Sanogo ML, Lee KS et al (2012) Short-term clinical importance of osseous injuries diagnosed at MR imaging in patients with anterior cruciate ligament tear. Radiology 264:531–41
Sonnery-Cottet B, Archbold P, Rezende FC, Neto AM, Fayard JM, Thaunat M (2014) Arthroscopic identification of the anterolateral ligament of the knee. Arthrosc Tech 3:e389–92
Acknowledgments
The scientific guarantor of this publication is Pieter Van Dyck. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. One of the authors has significant statistical expertise. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board. Methodology: retrospective, cross-sectional study/diagnostic or prognostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Van Dyck, P., Clockaerts, S., Vanhoenacker, F.M. et al. Anterolateral ligament abnormalities in patients with acute anterior cruciate ligament rupture are associated with lateral meniscal and osseous injuries. Eur Radiol 26, 3383–3391 (2016). https://doi.org/10.1007/s00330-015-4171-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-4171-8