Abstract
Inaccurate femoral tunnel placement has been identified as one of the most frequent errors in failed anterior cruciate ligament reconstructions. Most surgeons evaluate the femoral tunnel position on plain radiographs but in a lot of cases it is difficult to detect the femoral tunnel. The goal of this study was to compare plain digital radiographs and multiplanar computed tomography (CT) scans for the evaluation of femoral tunnel position. We examined 50 patients 24–60 months postoperatively, following an arthroscopically-assisted anterior cruciate ligament reconstruction with central third bone–patellar tendon–bone graft. Endobutton fixation was used on the femoral side and titanium interference screws on the tibial side. Standard antero-posterior and lateral X-rays and a CT scan were obtained from each patient. Sagittal and frontal reconstructions of the CT scan were used for the evaluation. We measured the height of the center of the tunnel in the notch in the frontal plane, and the position of the tunnel along Blumensaat’s line (BL) in the lateral plane. Measurements are reported as percentages of total notch height and of the length of BL. On plain X-rays the tunnel was invisible in 46 cases in the anterior–posterior plane and in eight cases on the lateral plane. The average position in the frontal plane was 89.8%, and in the lateral plane 38.6%. In the CT scans, measurements were able to be done in 48 patients. The frontal-plane position averaged 90.5% and the lateral-plane position 34.1%. Pearson’s correlation coefficient for the values in the lateral plane for CT and X-rays was low at 0.22, with p>0.05. In our group of 50 patients we were able to detect the femoral tunnel on both plains of standard X-rays in only four patients, whereas it was possible to take accurate measurements in 48 patients on reconstructed CT scans. We advocate the use of CT technology for the evaluation of femoral position whenever precise measurements are needed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The postoperative radiographic evaluation of bone tunnel position in intraarticular anterior cruciate ligament (ACL) reconstruction has received increasing attention. Plain radiographs in the early postoperative period serve as a standard quality control tool regarding tunnel position. Inaccurate tunnel placement has been identified as one of the most frequent errors in failed ACL reconstructions.
There is still considerable debate about the optimal position of the femoral tunnel. Recommendations include the over the top position [4, 9, 12], the central part [13, 14] and the postero-superior part [5–7, 15] of the insertion area. Furthermore, the superiority of an outside-in or an inside-out drilling technique is still subject to discussion regarding femoral tunnel accuracy [2].
When planning revision surgery, the surgeon has to know about both position and morphology of the tunnels drilled in previous surgery. Both parameters influence the surgical procedure, so that knowledge about position and morphology is the key to a successful revision ACL reconstruction. Therefore, any method used to evaluate the bone tunnels has to meet high standards.
Most previous studies on tunnel position have used plain radiographs. Some authors mention difficulties in locating the bone tunnels in a considerable percentage of cases. This parallels our own experience [10, 11, 17–19].
As computed tomography (CT) allows for excellent visualization of bony anatomy, it has been mandatory in the preoperative evaluation of a patient undergoing revision ACL reconstruction at our institution for several years. Based on that experience, we designed this study.
The goal of this study was to determine the ability of CT scan and plain X-ray to detect the femoral tunnel after ACL reconstruction and to measure femoral tunnel position.
Materials and methods
Cadaver knee
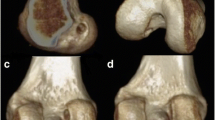
A male cadaver knee (age 35 years) with no evidence of degenerative changes was used for this study. The menisci, the collateral ligaments and the posterior cruciate ligament were intact. The ACL was resected and a standard reconstruction procedure was performed. A K-wire was introduced into the knee with inside-out technique by using an Acufex femoral aimer, and subsequently overreamed with an 8 mm cannulated reamer.
Standard anterior–posterior (AP) and lateral-plane X-rays were taken and a CT scan was performed. The specimen was then cut in the sagittal plane in the highest area of the notch, which gave a view onto the medial side of the lateral femoral condyle. The measurements were then taken directly from the specimen. The length of Blumensaat’s line (BL) and the distance from the posterior end of BL to the anterior femoral tunnel wall were measured (Zanat).
Patients
Fifty-one patients (seven female, 44 male) who had undergone ACL reconstruction with autologous bone–patellar tendon–bone graft taken from the middle third of the patellar tendon were included in this study.
The procedures were performed between June 1996 and September 1999 by two surgeons (C.F. and C.H.).
The operative procedure was done arthroscopically. The femoral bone tunnel was drilled inside-out through the tibial tunnel using an Acufex femoral aimer (5 mm offset) at the 11 o’clock position (right knee). The graft was fixed by endobutton fixation with a mersilene tape in the femur and a 7×20 mm interference screw on the tibial side. If the length of the graft was appropriate, the femoral bone block was positioned flush with the intraarticular opening of the femoral tunnel. In case of a long patellar tendon, the proximal bone block was positioned further proximally in order to place the distal bone block completely in the tibial tunnel. The cancellous side of the femoral bone block was rotated to face the arthroscope, which positioned the tendon deep and inferior in the intraarticular femoral tunnel opening.
The follow-up was done 24–60 months postoperatively, and the protocol consisted of a clinical and radiographic evaluation based on the IKDC form.
Lateral and AP radiographs (digital X-ray equipment, AGFA-Gevaert, Belgium) of all operated knees were performed in 15° flexion. The pictures were stored digitally on a hospital network [picture archiving and communication system (PACS)].
Computed tomography scans, with the knee positioned close to extension, were obtained in 50 cases. One patient refused the CT and was excluded from the study.
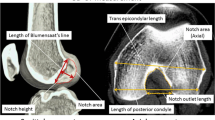
Nomenclature for orientation and position of the femoral tunnel was used according to Amis et al. [1]. Anterior and posterior positions along the roof of the notch (BL) on a lateral radiograph are called superficial and deep, respectively. Positions along a line perpendicular to the roof of the notch are defined as superior and inferior.
Radiographic evaluation
Digital X-ray technology allows for adjustments of contrast and brightness to optimize the localization of the relevant structures. X-rays were judged to be adequate if the overlap of the posterior condyles was more than 90%. The examiner (KT) was blinded for the findings in both CT scans and X-rays.
At first femoral tunnels were rated as visible or invisible on each radiograph. We adopted and slightly modified the three-dimensional coordinate system to measure radiographic femoral tunnel position as published by Khalfayan et al.[10].
The measurement ZX-ray describes the position of the anterior tunnel wall on a lateral radiograph (Khalfayan et al. [10] originally used the center of the tunnel for their measurements). We used the anterior tunnel wall as the measurement point to take into account any possible tunnel widening; low values represent a deep position. ZX-ray is expressed as a percentage of the total length of BL (Fig. 1).
In the AP view the measurement YX-ray is taken from a line drawn in a tangent to the femoral condyles to the center of the femoral tunnel opening. It is expressed as a percentage of the total height of the notch (FNH) measured from the mentioned tangential line (Fig. 2).
Computed tomography evaluation
Multislice CT technology (LightSpeed QX/I; GE Medical Systems, Milwaukee, WI, USA) with helical acquisition in 1.25-mm sections and pitch 3 (highQ mode) and spacing of 0.6 mm was used (120 kV, 80 mA, rotation time 0.8 s). Data were transferred to a postprocessing machine (Advantage Windows 4.0; GE Medical Systems). Secondary sagittal and frontal reconstructions were obtained.
The same examiner (KT) evaluated the scans 2 weeks after the plain radiographs, and was blinded for those measurement results.
All measurements on CT scans were performed in analogy to those on the plain radiographs.
On the sagittal reconstructions the roof of the notch was taken as the representation of BL. The most lateral slice that showed the roof and the tunnel was taken for the measurement of the Z value. If roof and tunnel were not seen on the same slice, the measurement was rated as impossible. ZCT is expressed as a percentage of the total length of BL (Fig. 3).
A frontal reconstruction through the intraarticular femoral tunnel entry was used for the measurement of the Y value. YCT is expressed as a percentage of the FNH (Fig. 4).
Statistical analysis
Data analysis was performed using Systat software (Systat Software Inc., Richmond, CA, USA). Pearson’s correlation coefficient was calculated for the data of plain radiographic and CT measurements.
Results
Cadaver knee
The measurements of the femoral tunnel position in the cadaver knee are shown in Table 1. Only marginal differences were seen between the three measurement modalities (Fig. 5).
Routine sagittal and coronal CT reconstructions were found to be adequate for the intended purpose.
Radiographic evaluation of patient knees
Lateral view
Three radiographs (5.8%) were judged inadequate because of less than 90% posterior condyle overlap. In eight cases (15.6%) the tunnel was invisible.
The remaining 40 cases showed a ZX-ray value ranging from 5 to 100%, average 38.6±12.7%. The outlier with the value of 100% will be discussed as case 1.
AP view
We were able to detect the tunnel in only four cases (7.8%). YX-ray was 89.8% on average. In the remaining 46 cases the measurement was not possible due to invisible tunnels.
Computed tomography evaluation of patient knees
Fifty CT scans were evaluated. The tunnel and the ingrown bone plug were identified in all cases. In two cases a ZCT measurement could not be performed, because notch roof and tunnel were not identified in the same picture. For the remaining 48 cases the average ZCT was 34.1±6.8%, with a range from 23.7% to 59.4%.
The YCT was <70% in no case, 70–79.9% in two cases, 80–89.9% in 19 cases, and 90–100% in 26 cases. On two CT scans this ratio was not measurable. The average ratio was 90.5±4.6%, ranging from 75% to 100%.
Comparison of X-ray and CT values
Statistical analysis was done for cases, where both X-ray and CT measurements were obtainable (39 cases) for the Z value.
ZX-ray and ZCT were not significantly different. The CT measurements showed the position as a trend deeper (p=0.09, paired Student’s t-test).The Pearson correlation coefficient was 0.22 at p>0.05. The regression analysis showed two outliers (Fig. 6).
In one case (ZX-ray 100%, ZCT 32.9%) radiographic structures were incorrectly taken as the representation of the tunnel. This only became obvious after the CT scans were evaluated and compared to the plain films (Fig. 7).
The second case (Fig. 8) showed a ZX-ray value of 46.6% and a ZCT 59.4%. Both values indicate an incorrectly-placed graft, too anterior on the femoral side.
Discussion
The importance of correctly-placed tunnels in ACL reconstruction is well accepted. However, inaccurate radiographic technique and poor visibility of the tunnels can make it impossible to determine femoral tunnel position on plain films.
Summarizing our results, we were not able to measure femoral tunnel position in 92.2% of all cases on AP and in 21.6% on lateral radiographs. Even more disturbing is the fact that in two cases we identified the wrong anatomic radiographic structure as the femoral tunnel. This was only obvious after having evaluated the CT scan.
Khalfayan et al. [10] mentioned that inadequate radiographic data were one of the exclusion criteria in their study, but they do not specify the percentage of patients they had to exclude.
Sommer et al. [19] found problems concerning tunnel visibility on the tunnel view and stressed the importance of an accurate projection on the lateral view. Their patient collective consisted of failed ACL reconstructions, in which tunnel-wall sclerosis due to prolonged effusions may make it even easier to read the X-ray.
Lintner et al. [11] stated that it was difficult to see the intraarticular mouth of the tunnel on the lateral view in cadavers with stripped soft tissues.
In our study it was always possible to visualize the tunnel and the ingrown bone block in the sagittal reconstructions of the CT scan; however, in two cases a measurement was impossible. For those cases it would have been necessary to recalculate the sagittal CT reconstruction at a different angle, in order to see the notch roof and the tunnel on one single slice.
Recently there has been increasing interest in the femoral tunnel position in the frontal plane [2, 8]. We found that tunnel visibility on the AP view was only 7.8% in our patient group. This big discrepancy compared to studies previously published can be explained by several facts.
On immediate postoperative radiographs tunnel visibility may be better than after several years. This could especially apply to a bone–tendon–bone graft, as the bone block shows complete ingrowth after a few weeks. Soft-tissue grafts may therefore present with a better tunnel visibility even months after ACL reconstruction.
Furthermore, metallic implants can help in the detection of the tunnel. Particularly in cases where the position of the implant is close to the joint, the evaluation of tunnel placement is facilitated. However, with the introduction of bioabsorbable implants, which are invisible on radiographs, metallic implants no longer indicate tunnel position. This fact may increase the need for additional imaging beyond plain films.
It is also important to mention that different drilling techniques have an influence on the visibility of the femoral tunnel. Tunnel visibility on a lateral projection becomes better as the longitudinal axis of the femoral tunnel approaches the transverse plane. Therefore, a tunnel drilled from outside-in is better visible than a tunnel drilled with single-incision technique.
Bagnolesi et al. [3] compared the value of CT and magnetic resonance imaging (MRI) for the postoperative evaluation of ACL reconstruction. They did not use reconstructed CT planes and found better measurement results in MRI. Modern CT-scanning software allows for the reconstruction of any desired plane. With regard to bony morphology, CT proved to be superior in their study.
Metal implants create artifacts on MRI, which reduce picture quality [16]. Tomczak et al. [20] even considered it necessary to remove titanium interference screws to avoid image distortion.
Computed tomography exposes the patient to radiation, although appropriate protection is certainly used. In our opinion this disadvantage is outweighed by the amount of information gained by a CT investigation. This information is crucial for the success of revision reconstructions.
We do not think that MRI is an option for avoiding radiation. Bony anatomy is markedly better visualized on CT scans, and metallic implants do not deteriorate the imaging quality.
The results of our study indicate that in a lot of cases plain radiographs are not sufficient for the evaluation of femoral tunnel placement, because of both poor tunnel visibility and inaccurate tunnel projection.
However, plain films remain standard in general postoperative documentation after ACL reconstruction.
We recommend CT imaging for the following situations:
-
1.
Failed ACL reconstructions that need revision, as exact evaluation of primary tunnel placement is crucial for the revision procedure.
-
2.
Studies on tunnel positioning comparing different surgical techniques.
-
3.
Second opinions in patients after ACL reconstruction.
References
Amis AA, Beynnon B, Blankevoort L et al (1994) Proceedings of the ESSKA scientific workshop on reconstruction of the anterior and posterior cruciate ligaments. Knee Surg Sports Traumatol Arthrosc 2:124–132
Arnold MP, Kooloos J, van Kampen A (2001) Single-incision technique misses the anatomical femoral anterior cruciate ligament insertion: a cadaver study. Knee Surg Sports Traumatol Arthrosc 9:194–199
Bagnolesi P, Russo R, Battolla L et al (1994) Reconstruction of the anterior cruciate ligament with patellar tendon. Comparison between magnetic resonance and computerized tomography. Radiol Med (Torino) 88:378–387
Feagin JA Jr (1979) The syndrome of the torn anterior cruciate ligament. Orthop Clin North Am 10:81–90
Girgis FG, Marshall JL, Monajem A (1975) The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop 106: 216–231
Hefzy MS, Grood ES, Noyes FR (1989) Factors affecting the region of most isometric femoral attachments. Part II: the anterior cruciate ligament. Am J Sports Med 17:208–216
Hoogland T, Hillen B (1984) Intra-articular reconstruction of the anterior cruciate ligament. An experimental study of length changes in different ligament reconstructions. Clin Orthop 185:197–202
Howell SM, Gittins ME, Gottlieb JE, Traina SM, Zoellner TM (2001) The relationship between the angle of the tibial tunnel in the coronal plane and loss of flexion and anterior laxity after anterior cruciate ligament reconstruction. Am J Sports Med 29:567–574
Insall J, Joseph DM, Aglietti P, Campbell RD Jr (1981) Bone-block iliotibial-band transfer for anterior cruciate insufficiency. J Bone Joint Surg Am 63:560–569
Khalfayan EE, Sharkey PF, Alexander AH, Bruckner JD, Bynum EB (1996) The relationship between tunnel placement and clinical results after anterior cruciate ligament reconstruction. Am J Sports Med 24:335–341
Lintner DM, Dewitt SE, Moseley JB (1996) Radiographic evaluation of native anterior cruciate ligament attachments and graft placement for reconstruction. A cadaveric study. Am J Sports Med 24:72–78
Melhorn JM, Henning CE (1987) The relationship of the femoral attachment site to the isometric tracking of the anterior cruciate ligament graft. Am J Sports Med 15:539–542
Muneta T, Yamamoto H, Sakai H, Ishibashi T, Furuya K (1993) Relationship between changes in length and force in in vitro reconstructed anterior cruciate ligament. Am J Sports Med 21:299–304
Odensten M, Gillquist J (1985) Functional anatomy of the anterior cruciate ligament and a rationale for reconstruction. J Bone Joint Surg Am 67:257–262
Shelbourne KD, Whitaker HJ, McCarroll JR, Rettig AC, Hirschman LD (1990) Anterior cruciate ligament injury: evaluation of intraarticular reconstruction of acute tears without repair. Two to seven year followup of 155 athletes. Am J Sports Med 18:484–488
Shellock FG, Mink JH, Curtin S, Friedman MJ (1992) MR imaging and metallic implants for anterior cruciate ligament reconstruction: assessment of ferromagnetism and artifact. J Magn Reson Imaging 2:225–228
Sim E (1993) Choice of femoral reinsertion sites after rupture of the anterior cruciate ligament—a roentgenologic evaluation model. Aktuelle Traumatol 23:330–331
Sim E (1994) Transcondylar reinsertion of femoral avulsions of the anterior cruciate ligament: evaluation of the position in 20 cases using three-dimensional computed tomographic reconstruction. J Trauma 37:525–531
Sommer C, Friederich NF, Muller W (2000) Improperly placed anterior cruciate ligament grafts: correlation between radiological parameters and clinical results. Knee Surg Sports Traumatol Arthrosc 8:207–213
Tomczak RJ, Hehl G, Mergo PJ, Merkle E, Rieber A, Brambs HJ (1997) Tunnel placement in anterior cruciate ligament reconstruction: MRI analysis as an important factor in the radiological report. Skeletal Radiol 26:409–413
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hoser, C., Tecklenburg, K., Kuenzel, K.H. et al. Postoperative evaluation of femoral tunnel position in ACL reconstruction: plain radiography versus computed tomography. Knee Surg Sports Traumatol Arthrosc 13, 256–262 (2005). https://doi.org/10.1007/s00167-004-0548-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-004-0548-y