Abstract
Purpose
Tears of the posterior horn of the medial meniscus (PHMM) are very common in the ACL-deficient knee. Specific lesions of the PHMM have been described in the setting of ACL rupture: ramp lesions and injuries to the meniscotibial ligament. There are little data available regarding the role these lesions play in knee instability. The aim of this study is to analyse the biomechanical consequences of ramp and meniscotibial ligament lesions on knee stability. Our hypothesis was that these lesions would cause increased instability in the setting of ACL rupture.
Methods
A cadaveric study was undertaken: ten knees were included for analysis. The biomechanical repercussions of different meniscoligamentous injuries were studied in four stages: stage 1 involved testing the intact knee, stage 2 after transection of the ACL, stage 3 following creation of a ramp lesion, and stage 4 after detachment of the meniscotibial ligament. Four parameters were measured during the experiment: anterior tibial translation under a force of 134 N, internal and external tibial rotation under a torque of 5 Nm, and valgus angulation under a torque of 10 Nm. Measurements were taken in four knee flexion positions: 0° or full extension, 30°, 70°, and 90° of flexion.
Results
There was a statistically significant increase in anterior tibial translation for stage 2 (6.8 ± 1.3 mm, p ≤ 0.001), stage 3 (9.4 ± 1.3 mm, p ≤ 0.001), and stage 4 (9.3 ± 1.3 mm, p ≤ 0.001) compared to stage 1. There was no significant difference between stage 2 and stage 3 (2.6 mm, n.s.) or stage 4 (2.5 mm, n.s.). We did, however, demonstrate an increase in anterior tibial translation of 2.6 mm after the creation on a lesion of the PHMM compared to isolated division of the ACL, for all flexion angles combined. There was an increase in internal tibial rotation between stage 1 and stage 4 (3.2° ± 0.7°, p ≤ 0.001) and between stage 2 and stage 4 (2.0° ± 0.7°, p = 0.023). A significant difference was demonstrated for external rotation under 5 Nm torque between stages 4 and 1 (2.2° ± 0.5°, p ≤ 0.001) and between stages 4 and 2 (1.7° ± 0.5°, p = 0.007) for all knee flexion angles combined. No created lesion had a significant effect on medial laxity under a 10-Nm valgus torque at any degree of knee flexion.
Conclusion
Lesions of the posterior horn of the medial meniscus are frequent in cases of anterior cruciate ligament rupture. These lesions appear to play a significant role in knee stability. Ramp lesions increase the forces in the ACL, and the PHMM is a secondary restraint to anterior tibial translation. Lesions of the meniscotibial ligament may increase rotatory instability of the knee.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meniscal lesions occur in association with rupture of the anterior cruciate ligament (ACL) in over 60 % of cases [8], with tears of the posterior horn of the medial meniscus (PHMM), the most commonly observed lesion (40 % of lesions) [14]. From a biomechanical perspective, there is interdependence between the ACL and the PHMM. A lesion of the PHMM increases forces in the ACL by 50 %, and conversely, a rupture of the ACL increases forces in the PHMM by 100 % [11]. Tears of the PHMM are frequently secondary to ACL rupture, occurring with further episodes of instability. The longer the delay between ACL injury and surgical intervention, the higher the incidence of PHMM tears [4].
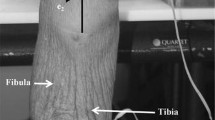
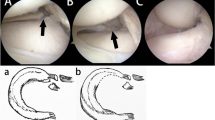
Specific lesions of the PHMM have been described in the setting of ACL rupture: ramp lesions and lesions of the meniscotibial ligament. Ramp lesions were first described by Strobel in his 1980 Manual of Arthroscopic Surgery [16]. The term refers to a complete, longitudinal lesion of the PHMM occurring in the very periphery of the meniscus (Fig. 1). In a series of 868 ACL ruptures, Liu et al. [7] documented the presence of such lesions in over 16 % of patients. Lesions of the meniscotibial ligament may occur either as a rupture in its mid-substance or as an avulsion from its tibial insertion (Fig. 2). The sensitivity of magnetic resonance imaging (MRI) for the detection of these lesions is reduced in the setting of ACL injury [10, 13], and thus, they may be missed on radiological investigations. These lesions of the PHMM are also frequently underestimated during ACL reconstruction surgery. Accurate diagnosis requires the use of supplemental arthroscopic views, such as the intercondylar view and viewing via a posteromedial portal [12]. Use of a shaver may also be required to debride scar tissue that may mask very peripheral lesions [15].
Despite a number of publications describing these injuries and their diagnosis, there are little data available regarding the role these lesions play in knee instability. Ahn et al. [1] demonstrated an increase in anteroposterior instability in the ACL-deficient knee with the creation of a very peripheral, longitudinal PHMM lesion.
The aim of this study is to analyse the biomechanical consequences of ramp and meniscotibial ligament lesions on knee stability, more precisely on anterior tibial translation, valgus angulation, and internal and external rotation. Our hypothesis was that these lesions would cause increased instability in the setting of ACL rupture.
Materials and methods
A cadaveric study was undertaken. The cadaveric specimens were preserved with bromopol (safe balm®) following the technique used at the Rockefeller anatomy laboratory, Grange Blanche, Lyon, France. This preservation technique should not affect the biomechanical properties of soft tissues when tested at ambient temperature. Full-body cadaveric specimens were used. Exclusion criteria were previous surgery or dissection of the knee, clinical anterior or medial laxity, and lesions of the ACL or medial meniscus at initial arthroscopic assessment.
Ten knees were included for analysis. Six knees were excluded: two due to the presence of surgical scars about the knee, and four after arthroscopic assessment revealed a degenerative medial meniscal tear (three cases) or ACL rupture (one case).
The biomechanical repercussions of different meniscoligamentous injuries were studied in four stages, with each stage corresponding to a type or combination of lesions. Stage 1 was a reference stage, testing the knee untouched besides arthroscopic examination. Stage 2 involved testing after the transection of the ACL, and stage 3 following creation of a ramp lesion using the intercondylar view for visualisation and a posteromedial portal for instrumentation. In stage 4, the knee was tested after detachment of the meniscotibial ligament of the PHMM. The stages were performed sequentially, such that each stage involved the addition of a new lesion to those already created.
Four parameters were measured during the experiment: anterior tibial translation under a force of 134 N, internal and external tibial rotation under a torque of 5 Nm, and valgus angulation under a torque of 10 Nm. Each parameter was measured at each stage of the investigation in four knee flexion positions: 0° or full extension, 30°, 70°, and 90° of flexion.
Testing was performed by two orthopaedic surgeons (AP, SL) in the presence of a qualified engineer (D.Goy). The specimens were placed in a supine position on a dissection table. A strap was used to secure the pelvis, to allow accurate determination of the hip centre. A leg-holding device was used to control and stabilise knee flexion. Arthroscopy was performed using a standard 30° arthroscope, tower, and fluid pump. Rigid bodies for the navigation system and traction hooks were placed precisely to allow accurate measurement and reproducibility between subjects. For tibial translation and rotation, a 100-mm metal rod was fixed to the centre of the tibial tuberosity using two 4.5-mm cancellous screws 50 mm in length. The rod was placed in the sagittal plane, perpendicular to the axis of the tibia. For valgus force, a traction hook was fixed to the medial border of the tibia, 30 cm from the joint line of the knee, and fixed using two 4.5-mm bicortical screws.
Measurements were taken using a Tornier® navigation system with a Polaris® infrared camera. The accuracy of the system is <1 mm for length measurement. For each cadaveric body, the system was recalibrated to obtain the highest precision measurements possible. After calibration of the system, rigid bodies were fixed to the femoral and tibial diaphysis. Twenty reference points were palpated and recorded. A KERN CH50 K50® dynamometer was used for dynamic measures and recalibrated for each specimen. Each dynamic measurement was captured by a single acquisition of the navigation system, totalling 64 acquisitions per specimen and 640 acquisitions in total. The navigation system was programmed in engineering mode specifically for the purpose of this study. This allowed a blinded interpretation of the data, such that the data analysis was performed only after the completion of the laboratory work.
All collected data were analysed by an independent engineer. From the palpated reference points and raw data, a reference tibia and femur were defined. Anterior tibial translation was referenced from the resting position of the untouched knee and given as an absolute value in mm. Rotation of the tibia in reference to the femur was calculated following the recommendations for interpretation of movement at the knee described by Grood and Suntay [5]. IRB approval was obtained before starting this study.
Statistical analysis
The same method of analysis was applied to all data. A univariate analysis was performed with fixed factors. The fixed factor was the test stage 1 through 4. The tested variable varied as a function of the testing stage. As the data followed a normal distribution, parametric tests were performed. Statistical analysis was performed using SSPS software (IBM®). Significance was set at p < 0.05.
Results
Analysis of anterior tibial translation under 134 N (Table 1)
Initially, we analysed the combined measurements for all knee flexion angles combined (0°, 30°, 70°, and 90°).
Stage 1 was defined as the reference for anterior tibial translation with an arbitrary value of 0 mm. The values for anterior translation for all other stages were thus the difference between that stage and stage 1, in mm. There was a statistically significant difference for anterior tibial translation for stage 2 (6.8 ± 1.3 mm, p ≤ 0.001), stage 3 (9.4 ± 1.3 mm, p ≤ 0.001), and stage 4 (9.3 ± 1.3 mm, p ≤ 0.001). There was no significant difference between stage 2 and stage 3 (2.6 mm, n.s.) or stage 4 (2.5 mm, n.s.). We did, however, demonstrate an increase in anterior tibial translation of 2.6 mm after the creation on a lesion of the PHMM compared to isolated division of the ACL, for all flexion angles combined.
Next we analysed the data as a function of knee flexion angle. In extension (0°), there was a significant difference between stage 1 and stage 3 (10.0 mm, p = 0.039) and stage 1 and stage 4 (13.5 mm, p = 0.003).
At 30° of knee flexion, there was a significant difference demonstrated between stage 1 and stage 2 (p = 0.006), stage 3 (p ≤ 0.001), and stage 4 (p = 0.002). No significant difference was demonstrated between stages 2, 3, and 4. Creation of a lesion of the PHMM resulted in an increase in anterior tibial translation of 4.9 mm compared to isolated sectioning of the ACL. This result was not statistically significant (p = 0.27) despite the large quantitative difference.
At 70° of knee flexion, there was a significant difference demonstrated between stage 1 and stage 2 (p = 0.033), stage 3 (p ≤ 0.001), and stage 4 (p ≤ 0.001). Again, no significant difference was found between stages 2, 3, and 4. Creation of a PHMM lesion at stage 3 resulted in an increase in anterior tibial translation of 4.3 mm compared to stage 2, but again this did not reach statistical significance (p = 0.062).
At 90° of knee flexion, a significant difference was found between stage 1 and stage 2 (p = 0.008), stage 3 (p = 0.002), and stage 4 (p ≤ 0.001). No difference was demonstrated between stages 2, 3, and 4.
Analysis of internal tibial rotation under 5 Nm torque (Table 1)
Global analysis of all knee flexion angles combined (0°, 30°, 70°, and 90° of flexion) demonstrated an increase in internal tibial rotation between stage 1 and stage 4 (3.2° ± 0.7°, p ≤ 0.001) and between stage 2 and stage 4 (2.0° ± 0.7°, p = 0.023).
Sectioning of the ACL had no effect on internal tibial rotation (comparison of stages 1 and 2, p = n.s.). Analysis as a function of knee flexion angle demonstrated no difference between any stages at knee flexion angles 70° and 90. At 30° of flexion, a significant difference was found between stages 1 and 4 only (+4.5°, p = 0.030). In full extension, internal rotation at stage 4 was significantly increased compared to all other stages (comparison with stage 1: +7.3°, p ≤ 0.001; with stage 2: +4.8°, p ≤ 0.001; with stage 3: +2.8°, p = 0.024).
Analysis of external tibial rotation under 5 Nm torque
A significant difference was demonstrated for external rotation between stages 4 and 1 (2.2° ± 0.5°, p ≤ 0.001) and between stages 4 and 2 (1.7° ± 0.5°, p = 0.007), for all knee flexion angles combined. Subgroup analysis by knee flexion angle did not yield any additional information.
Analysis of valgus under 10 Nm torque
No created lesion had a significant effect on medial laxity at any degree of knee flexion.
Discussion
The most important finding of this study is evidence of a role for the meniscotibial ligament in rotatory knee stability. In the extended knee, the additional division of the meniscotibial ligament (Fig. 3) resulted in an increase in internal tibial rotation of 4.8° (p ≤ 0.001) when compared to isolated ACL sectioning, and of 7.3° (p ≤ 0.001) compared to the untouched knee. Furthermore, division of the meniscotibial ligament resulted in an increase in external tibial rotation compared to the untouched knee (+2.2°, p ≤ 0.001) and to isolated sectioning of the ACL (+1.7°, p = 0.007). To our knowledge, this is the first study to present a potential role for the meniscotibial ligament in rotatory knee stability.
We were unable to demonstrate a statistically significant role for the PHMM in limiting anterior tibial translation in the ACL-deficient knee. We did, however, measure important differences in this translation after the creation of a lesion of the PHMM (Fig. 4), varying from 4.3 mm at 70° to 4.9 mm at 30° of knee flexion. This trended towards, but did not reach, statistical significance (p = 0.062 at 70°). With a greater sample size, it is likely that this would have reached significance. Levy et al. [6] found that tibial translation was greater in the ACL-deficient knee after total medial meniscectomy. Our results are consistent with the data available in the literature [1, 11]. The PHMM seems to play an important role in limiting anterior tibial translation in the ACL-deficient knee [3].
The meniscotibial ligament solidly anchors the PHMM. Detachment of the ligament probably allows abnormal mobility of the entire PHMM, with a notable reduction in rotational stability. The posterior root insertions of the menisci vary considerably between the medial and lateral sides (Fig. 5). The PHMM is stabilised posteriorly by the meniscotibial ligament, which in turn inserts onto the posterior aspect of the proximal tibia. The capsule of the knee joint inserts more distally on this posterior surface. There is no insertion of the posterior capsule onto the posterior aspect of the PHMM. Conversely, the posterior horn of the lateral meniscus is fixed posteriorly by the meniscofemoral ligament and by the joint capsule. These two structures fuse and share a common insertion onto the posterior aspect of the tibia. We have observed that lesions of the mensiscotibial ligament occur either in the mid-substance (which may be repairable) or as a bony avulsion (which is irreparable). In cases of ramp lesions or meniscotibial ligament lesions, the posterior part of the lesion tends to sag posteriorly. This is in part what makes their diagnosis difficult. Repair requires the use of supplemental arthroscopic views and portals, such as an intercondylar view and a posteromedial portal, to lift this sagging peripheral tissue to the more central part. These lesions are not amenable to repair using all inside devices and standard anterolateral and anteromedial portals.
We did not analyse the role of lateral meniscus in this study. Musahl et al. [9] demonstrated that the lateral meniscus is an important restraint on anterior tibial translation during combined valgus and rotary loads.
The strengths of this study include the use of a reliable and precise measurement system, capable of interpreting the range of movements at the knee under various loads. The use of a calibrated measurement system during dynamic testing allows perfect reproducibility between test specimens. This study is subject to some weaknesses. Firstly, knee testing was performed in an unloaded state, which may yield different results than would be seen in the weight-bearing knee. Secondly, lesions were created sequentially. A lesion of the meniscotibial ligament in the absence of a ramp lesion may have a different biomechanical effect. Furthermore, sectioning of the ACL and the creation of different PHMM lesions in an experimental setting may not produce the same effects as those seen in cases of chronic anterior laxity. As lesions of the PHMM and meniscotibial ligament occur secondary to ACL rupture, they are in effect the result of chronic anterior laxity.
Lesions of the PHMM as well as lesions of the meniscotibial ligament should be sought during ACL reconstructive procedures. Where possible, they should be repaired, to avoid compromising knee stability and causing increased forces in the graft in the post-operative period. Ramp lesions increase anterior knee laxity, while lesions of the meniscotibial ligament appear to increase rotatory instability. Allaire et al. [2] demonstrated significant changes in contact pressure and knee joint kinematics due to a posterior root tear of the medial meniscus. Furthermore, they also demonstrated that root repair was successful in restoring joint biomechanics to within normal conditions.
Conclusion
Lesions of the posterior horn of the medial meniscus are frequent in cases of anterior cruciate ligament rupture. Diagnosis of these lesions may be difficult, with MRI having reduced sensitivity in the pre-operative period. During arthroscopic ACL reconstruction, diagnosis and repair of these lesions may require supplemental arthroscopic views or portals. These lesions appear to play a significant role in knee stability. Ramp lesions increase the forces in the ACL, and the PHMM is a secondary restraint to anterior tibial translation. Lesions of the meniscotibial ligament may increase rotatory instability of the knee. Their precise biomechanical role will undoubtedly be more accurately determined in the coming years. We believe these lesions should be systematically sought and treated during ACL reconstruction.
References
Ahn JH, Bae TS, Kang K-S, Kang SY, Lee SH (2011) Longitudinal tear of the medial meniscus posterior horn in the anterior cruciate ligament-deficient knee significantly influences anterior stability. Am J Sports Med 39:2187–2193
Allaire R, Muriuki M, Gilbertson L, Harner CD (2008) Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am 90:1922–1931
Allen CR, Wong EK, Livesay GA, Sakane M, Fu FH, Woo SL (2000) Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. J Orthop Res 18:109–115
Chen G, Tang X, Li Q, Zheng G, Yang T, Li J (2013) The evaluation of patient-specific factors associated with meniscal and chondral injuries accompanying ACL rupture in young adult patients. Knee Surg Sports Traumatol Arthrosc 23:792–798
Grood ES, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech 105:136–144
Levy IM, Torzilli PA, Warren RF (1982) The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am 64:883–888
Liu X, Feng H, Zhang H, Hong L, Wang XS, Zhang J (2011) Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med 39:832–837
Michalitsis S, Vlychou M, Malizos KN, Thriskos P, Hantes ME (2015) Meniscal and articular cartilage lesions in the anterior cruciate ligament-deficient knee: correlation between time from injury and knee scores. Knee Surg Sports Traumatol Arthrosc 23:232–239
Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD (2010) The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 38:1591–1597
Nam T-S, Kim MK, Ahn JH (2014) Efficacy of magnetic resonance imaging evaluation for meniscal tear in acute anterior cruciate ligament injuries. Arthroscopy 30:475–482
Papageorgiou CD, Gil JE, Kanamori A, Fenwick JA, Woo SL, Fu FH (2001) The biomechanical interdependence between the anterior cruciate ligament replacement graft and the medial meniscus. Am J Sports Med 29:226–231
Peltier A, Lording TD, Lustig S, Servien E, Maubisson L, Neyret P (2015) Posteromedial meniscal tears may be missed during anterior cruciate ligament reconstruction. Arthroscopy 31:691–698
Sharifah MIA, Lee CL, Suraya A, Johan A, Syed AFSK, Tan SP (2013) Accuracy of MRI in the diagnosis of meniscal tears in patients with chronic ACL tears. Knee Surg Sports Traumatol Arthrosc 23:826–830
Smith JP, Barrett GR (2001) Medial and lateral meniscal tear patterns in anterior cruciate ligament-deficient knees. A prospective analysis of 575 tears. Am J Sports Med 29:415–419
Sonnery-Cottet B, Conteduca J, Thaunat M, Gunepin FX, Seil R (2014) Hidden lesions of the posterior horn of the medial meniscus: a systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med 42:921–926
Strobel M (2002) Manual of arthroscopic surgery. Michael Strobel—Springer, New York, pp 171–177
Acknowledgments
Mr Damien Goy (Bioengineering) for his advice, assistance, and investment in this study, Mr Rodolphe Testa for his aide in the interpretation of the results, the anatomy laboratory, and the staff at the Rockefeller Faculty of Medicine, Lyon Grange Blanche.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Peltier, A., Lording, T., Maubisson, L. et al. The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surg Sports Traumatol Arthrosc 23, 2967–2973 (2015). https://doi.org/10.1007/s00167-015-3751-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3751-0