Abstract
Purpose
To report the medium-term clinical and radiographic outcomes of a group of patients who underwent anterior cruciate ligament (ACL) surgery combined with high tibial osteotomy (HTO) for varus-related early medial osteoarthritis (OA) and ACL deficiency knee.
Methods
Thirty-two patients underwent single-bundle over-the-top ACL reconstruction or revision surgery and a concomitant closing-wedge lateral HTO. The mean age at surgery was 40.1 ± 8.1 years. Evaluation at a mean of 6.5 ± 2.7 years of follow-up consisted of subjective and objective IKDC, Tegner Activity Level, EQ-5D, VAS for pain and AP laxity assessment with KT-1000 arthrometer. Limb alignment and OA changes were evaluated on radiographs.
Results
All scores significantly improved from pre-operative status to final follow-up. KT-1000 evaluation showed a mean side-to-side difference of 2.2 ± 1.0 mm. Two patients were considered as failures. The mean correction of the limb alignment was 5.6° ± 2.8°. Posterior tibial slope decreased at a mean of 1.2° ± 0.9°. At final follow-up, the mechanical axes crossed the medial–lateral length of tibial plateau at a mean of 56 ± 23 %, with only 1 patient (3 %) presenting severe varus alignment. OA progression was recorded only on the medial compartment (p = 0.0230), with severe medial OA in 22 % of the patients. No patients underwent osteotomy revision, ACL revision, UKA or TKA.
Conclusions
The described technique allowed patients with medial OA, varus alignment and chronic ACL deficiency to restore knee laxity, correct alignment and resume a recreational level of activity at 6.5 years of follow-up.
Level of evidence
Case series with no comparison group, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High tibial osteotomy (HTO) is a widely accepted treatment for symptomatic medial osteoarthritis with lower extremity varus alignment. In young active patients, this pattern could be caused by chronic anterior cruciate ligament (ACL) lesion [16, 26] ACL deficiency is also responsible for the high frequency of medial meniscal lesion requiring meniscectomy, which is already known as a factor worsening medial osteoarthritis and varus alignment. [15].
On the other hand, severe varus alignment itself is demonstrated to increase the load on the native or reconstructed ACL, potentially compromising the ACL function or increasing the risk of failure of the reconstruction [25]. Moreover, an ACL-deficient knee combined with a varus alignment can even risk to precipitate the progression of the arthritis [22]. Therefore, combined ACL reconstruction and HTO represents a feasible salvage procedure in such complex patients, who are usually young and willing to improve their function to keep participating at work or recreational sport activities. This combined treatment has been described by several authors as staged or concomitant procedure, using a variety of ACL grafts or osteotomy technique [2, 3, 5, 13, 14, 21].
The purpose of this study was to report the medium-term clinical and radiographic outcomes of a group of patients who underwent one-stage combined hamstrings ACL surgery, either reconstruction or revision, and closing-wedge HTO for varus-related early medial osteoarthritis and ACL deficiency. The original step of this procedure is the addition of a lateral plasty to ACL reconstruction in order to reduce the rotational laxity in these patients.
Methods
Between 2002 and 2007, 32 patients underwent ACL surgery, either primary reconstruction or revision, plus closing-wedge lateral high tibial osteotomy and were prospectively followed. Exclusion criteria were age >60 years, PCL lesion, MCL III° lesion, inflammatory synovitis and grade D osteoarthritis according to IKDC radiographic score. Patients who underwent an ACL revision with an allograft were excluded as well.
Pre-operatively, the history of each patient was collected, and they all underwent a clinical and radiological evaluation (Table 1). Thirteen patients (40 %) underwent a previous patellar tendon ACL reconstruction; therefore, they were managed with a hamstring ACL revision. In these patients, the mean time between first ACL reconstruction and revision was 9.8 ± 3.6 years. The other 19 patients (60 %) were managed with primary hamstring ACL reconstruction due to chronic ACL insufficiency.
Regarding meniscal lesions, 17 patients (53 %) underwent a partial or subtotal meniscectomy at a mean of 10.4 ± 8.1 years before the combined procedure.
The study design was approved by the Institutional Review Board of the Institute, and all the patients provided their informed consent.
Every patient completed a self-administrated questionnaire including subjective IKDC, Tegner activity level (pre-symptoms, pre-operatively, post-operatively), EQ-5D and 100-points Visual Analogue Scale (VAS) for pain. A clinical evaluation was performed as an independent examiner according to the International Knee Documentation Committee (IKDC) knee ligament standard evaluation form [10].
AP laxity was assessed using the KT-1000 arthrometer (KT 1000; MEDmetric Corporation, San Diego, CA, USA) by means of the manual maximum test (MMT), which has been demonstrated to be the most discriminating and reliable test to evaluate the side-to-side differences in AP laxity between knees [23].
A radiological evaluation was also performed in order to asses the osteoarthritis changes and the alignment of the indexed knee. Osteoarthritis of medial and lateral and patellofemoral compartment joint was graded on AP and lateral radiographs according to the IKDC radiographic score [10]. Grade A corresponds to a normal joint, grade B to a joint affected by remodelling changes without narrowing, while grade C and D to joint with remodelling changes and narrowing of less or more than 50 % of the space.
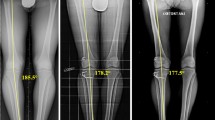
The alignment angles were measured on plain film or lateral radiographs using PACS system (DirectView, Kodak, Rochester, New York). The femorotibial angle (FTA) was the angle obtained by the intersection of tibial and femoral anatomical axis (Fig. 1a). The hip–knee–ankle angle (HKA) was the angle obtained by the intersection of the line connecting the centre of femoral head and the knee centre and the line connecting the knee centre and the centre of talar dome (Fig. 1b). For both angles, values <180° were referred to the valgus knees, while >180° were referred to the varus ones. The tibial plateau percentage (TP%) was the percentage of mediolateral width of knee joint where the lower limb mechanical axis (the line connecting femoral head and talar dome centres) crossed the joint line (Fig. 1c) [9]. Values <50 % were considered varus alignment, while >50 % were considered valgus alignment.
Parameters measured on radiographies to evaluate varus alignment and posterior tibial slope. a FTA: angle between the intersection of tibial (b) and femoral anatomical axis (a). b HKA: angle between the intersection of the line connecting the centre of femoral head (a) and the knee centre and the line connecting the knee centre to the centre of talar dome (b). c The tibial plateau percentage (TP%): percentage of mediolateral width of knee joint (a) where the lower limb mechanical axis (the line connecting femoral head and talar dome centres) (b) crossed the joint line. d Posterior tibial slope angle (PST): angle between the perpendicular line (a) to the proximal tibia axes (c) and the tangent line to medial tibial plateau (b) measured on lateral radiographs
The posterior tibial slope angle (PST) was the angle obtained between the perpendicular line to the proximal tibia axes and the tangent line to medial tibial plateau measured on lateral radiographs (Fig. 1d) [8]. Positive values are referred to a tibial plateau directed backward and inferiorly.
Between December 2010 and October 2011, all the patients (100 %) were available at a mean of 6.5 ± 2.7 (range 4–10) years follow-up and were evaluated with the same protocol.
Further, all complications and revision surgeries during the whole follow-up period were also recorded.
All the patients requiring revision HTO, revision ACL, UKA or TKA, or presenting a side-to-side difference at KT-1000 >5 mm were considered as failures.
Surgical procedure
The ACL reconstruction or revision was performed with an over-the-top procedure with lateral extraarticular augmentation involving a hamstring graft harvested preserving its distal insertion [18]. After graft harvesting, a 7-mm tibial tunnel was drilled to the posteromedial portion of ACL tibial insertion. Then, a proximal tibial closing-wedge osteotomy was performed under an intraoperative image intensifier. Internal plate fixation was accomplished with a Kracow staple [17]. Disruption of the proximal tibiofibular joint was avoided to prevent proximal migration and laxity in the posterolateral structures. An osteotomy of the fibula was performed at the fibular neck, with bone removal to allow for compression of the osteotomy site. Finally, the hamstring graft was passed through tibial tunnel and fixed at “over-the-top” site with two metal staples. The distal portion of the graft was passed below the fascia and fixed on Gerdy’s tubercle with a metal staple (Fig. 2).
Rehabilitative protocol
Post-operatively, patients were instructed to wear a long-leg brace for the first 4 weeks after surgery. Rehabilitation protocol started the first post-operative day with quadriceps muscle isometric exercises, straight leg raises, patellar mobilization and electric muscle stimulation. Passive range of motion exercises (0°–90°) with motorized hardware was allowed after 2 weeks. Complete range of motion was achieved at week 6. Patients were allowed to toe-touch weightbearing for the first 4 weeks to prevent excessive forces of the osteotomy site, and then, progressive weightbearing was allowed. Swimming pool exercises and stationary bike were started at week 5, running was allowed 4 months after surgery and return to sport activity after 8 months.
Statistical analysis
The statistical analysis was performed using Analyse-it-2.00 (Analyse-it Software Ltd, Leeds, UK).
Statistical comparison between the pre-operative and follow-up parametric scores was performed using a Student’s t test. We tested the population study for normal distribution before t test was applied. For differences between time points in Tegner level, we used the nonparametric Wilcoxon test. For difference in objective and radiographic IKDC score, we used the Pearson’s chi-square test. Correlation between BMI, clinical outcomes and the angles measured on rx was analyzed by Spearman’s rho test. The comparison of subgroups was performed using independent Student’s t test. The level of significance was set at p < 0.05.
Results are expressed using mean values ± standard deviation (SD) for parametric values and median ± interquartile range (IQR) for nonparametric ones.
Results
At pre-operative evaluation, 1 patient was graded as B (3 %), 13 as C (41 %) and 18 as D (56 %) according to IKDC form, while at final follow-up, 12 patients were graded as A (38 %), 17 as B (53 %), 1 as C (3 %) and 2 as D (6 %), showing a significant improvement (p < 0.0001). Subjective evaluation showed a significant improvement of all the scores between pre-operative status and final follow-up (Table 2). The Tegner activity level significantly improved from 3 (IQR 2–4) at pre-operative status to 5 (IQR 4–5) at final follow-up (p = 0.0012). Although reduced when compared with the pre-symptoms one (6, IQR 5–6), it resulted higher or equal to 5 (basketball, skiing and tennis at recreational level) in 20 patients (62 %). Moreover, six patients (18 %) at the final follow-up were still able to perform the same activity level as prior to the onset of symptoms.
KT-1000 evaluation showed a reduction in tibial anterior displacement with a mean side-to-side difference of 2.2 ± 1.0 mm. In 22 patients (69 %), it was <3 mm, while in 9 patients (28 %), it was among 3 and 5 mm. In one patient, it was higher than 5 mm, and therefore, it was considered as a failure. Another patient with a recent contralateral ACL lesion documented by Lachman test and MRI showed a side-to-side difference of 0 mm, but a manual maximum displacement test of 12 mm for each side and a clinical evidence of abnormal AP laxity; therefore, it was considered as a failure as well.
Regarding radiological evaluation, all the parameters at final follow-up improved significantly when compared to the pre-operative findings (Table 3).
The mean correction of FTA was 5.6° ± 2.8°, while the mean correction of HKA was 6.6° ± 3.0° (Fig. 3). The PTS decreased at a mean of 1.2° ± 0.9°. The mechanical axes crossed the medial–lateral length of tibial plateau at a mean of 56 ± 23 %, shifting laterally of 29 ± 11 % compared to pre-operative status. At final follow-up, 28 patients (88 %) presented value >50 % and only 1 (3 %) with severe varus alignment.
The radiological evaluation of degenerative changes according to IKDC radiographic scale demonstrated significant changes only in the medial compartment (p = 0.0230) (Table 4).
Signs of severe medial osteoarthritis (grade D) occurred in 22 % patients at final follow-up. No differences in clinical and radiological scores were found between primary or revision ACL surgery nor between patients with or without previous meniscectomy.
Regarding correlation analysis, a significant (p = 0.0441) positive (r = 0.64) correlation was found between PTS and KT-1000 manual maximum displacement test of the indexed knee at final follow-up. No further significant correlation was found between clinical, subjective and radiographic findings both pre-operatively and at final follow-up.
The analysis of subgroups showed the tendency of patients with medial compartment severe osteoarthritis (grade D) at final follow-up, to present with higher pre-operative grade of degenerative changes on lateral compartment as well (p = 0.0239). There was no significant difference in terms of demographic characteristics, level of activity and AP laxity between this subgroup and the rest of patients. Complications related to the procedure during the follow-up period were reported in 4 patients (12 %). One patient experienced hardware intolerance and underwent an intervention to remove the tibial and femoral staples of ACL reconstruction. Two patients (6 %) presented lack of knee flexion during the rehabilitative programme and underwent arthroscopic arthrolysis, restoring full knee motion. One patient showed delayed union of the osteotomy was successfully treated with external fixator. At final follow-up, no significant difference was noticed between these patients who experienced complications and the rest of the sample.
No patients underwent osteotomy revision, ACL revision, UKA or TKA during the considered follow-up period. According to failure criteria, two patients presented pathological AP laxity, and therefore, failure rate of the combined procedure at a mean of 6.5 years of follow-up has been 6 %.
Discussion
The most important finding of this study is that ACL reconstruction or revision combined with closing-wedge HTO reduced pain and improved knee function and laxity in complex patients presenting with chronic ACL deficiency, varus alignment and initial medial osteoarthritis.
These kinds of patients have been described by Noyes [21] as “some of the most difficult diagnostic and treatment dilemmas that clinician may require to manage”. Therefore, when facing with this issue, it is hard to achieve a complete resumption to the pre-symptoms-1 appearance level of activity or function. Few authors have reported about similar samples of patients achieving comparable clinical results [5, 13, 21]. Bonin et al. [2] with ACL reconstruction using patellar tendon and closing-wedge upper tibial osteotomy achieved a lower number of knee rated as normal or almost normal according to the IKDC scale; however, this difference could be imputable to the longer follow-up, 6.5 years compared with 12 years of follow-up. Moreover, we achieved satisfactory results in terms of pain reduction and knee function even if slightly inferior to other reports [2, 21], but probably this is due to the higher age (46 years) of the patients at final follow-up. Moreover, despite of a certain grade of pain and dysfunction, most of these patients were still able to perform regular intense sports (62 %). Further, none of the patients reported severe inability due to knee problems. Such beneficial effect of this combined procedure on the activity has been reported by Bonin et al.’s longer follow-up, suggesting a potential long-lasting positive result of this combined procedure.
The instrumented AP laxity assessment showed a significant restoration to normal values in 22 patients (69 %) and only two (6 %) failures [2, 3, 14, 21]. Boss et al. [3], 6 years after patellar tendon ACL reconstruction combined with closing-wedge HTO, showed 66 % of patients with <3 mm value and 4 % with >6 mm value measured with KT-1000, while Noyes et al. [21] showed a mean of 2.8 mm side-to-side difference. The latter authors reported a 10 % ACL-failure rate 4.5 years after reconstruction that does not substantially deviate from the 6 % rates of the present study.
Radiographic outcomes play a crucial role in the evaluation of HTO. Generally, the procedure is aimed to move the low limb mechanical axes laterally toward the so-called Fujisawa point [9], which correspond to the 62 % of medial–lateral width of the knee joint away from medial edge. A different algorithm has been suggested by Marti et al. [19] which relates the amount of overcorrection to be achieved to the grade of degeneration of the medial compartment. However, there is no clear evidence supporting one approach over another. On the other hand, solid evidence is available on the risk of excessively overcorrecting the alignment. Hernigou et al. [11] showed a significant progression of lateral compartment degeneration in patient with more than 6° valgus after alignment correction. Agneskirchner et al. [1] proved that neutral mechanical axis slightly loads the lateral more than the medial compartment, and overcorrecting produces an increase in the contact pressure on the lateral compartment.
The mean mechanical axes of the patients analyzed in this study resulted slightly medial to the Fujisawa point (56 %), differently from Noyes et al. [21] that described about 80 % of patients with a mechanical axes around the Fujisawa point. Nevertheless, in this study, 88 % of cases maintained a neutral or valgus alignment and a overall mean valgus of 0.4° with no significant progression of the degenerative changes occurring to the lateral compartment in any patient. This finding shows that limiting the overcorrection is effective in protecting the lateral compartment still not compromising the survivorship of the osteotomy result. Other authors showed similar or even higher post-operative mean valgus angulation (1.2°–3°) [2, 6] and correction values, reported to range from 6° to 8.7° [2, 6, 12].
For what concerns radiographic evaluation of the medial side, controversial findings are reported [2, 3, 14]. In the present study, it is reported a significant progression osteoarthritis in 22 % of patients. This is a predictable degeneration rate at 6.5 years of follow-up when facing with certain patients with a pre-operative mean age older than 40 and a significant number of failures of previous ACL reconstruction and meniscectomies. Interestingly, the patients who suffered a higher degeneration process on the medial side are pre-operatively presented with a higher degree of osteoarthritis on the lateral side. Bonin et al. [2] showed less degenerative changes at 12 years after the procedure, but in 10-year younger population undergoing just primary ACL reconstruction.
A controversial topic concerning HTO is the role of posterior tibial slope and its effect on ACL-deficient knee. It is well known that HTO can alter the slope on purpose or inadvertently [8]. A multicentric study of the French Society of Orthopaedic Surgery and Traumatology performed on 321 HTO highlighted how open-wedge HTO increases the slope of a mean of 0.6°, while closing-wedge HTO decreases slope of a mean of 0.7° [7]. The present study confirms this finding, as it reported a significant reduction in the tibial slope of 1.2° with closing-wedge HTO. The role of tibial slope is particularly interesting because it has been demonstrated that a steeper slope could be a risk factor for non-contact ACL lesions [4], caused by increased strain in the anteromedial bundle [20] due to the mechanism of anterior tibial translation when a compressive axial load is applied to knee joint [24]. However, a HTO aimed to decrease tibial slope has not been established as therapeutic option for ACL insufficiency [8]. The present study highlights the importance of tibial slope, due to the positive correlation reported between PTS and manual maximum displacement test measured with KT-1000 Arthrometer.
Considering the relatively low rate of complications, it can be stated that combined one-stage hamstrings ACL reconstruction and closing-wedge HTO represents a safe procedure. Various authors reported complication rates up to 37 % [13], presenting the knee stiffness as one of the most common (15 %). Furthermore, no patients required revision procedures and unicompartmental or total resurfacing during the follow-up period.
In day by day clinical work, this combined procedure should be used more frequently to improve the quality of life of these patients and delay the degenerative changes related to stress concentration and increased laxity.
This study has some limitations. First, the non-homogeneity of the patients makes it difficult to generalize and standardize the findings, but such complex cases hardly offer themselves to standardization given their variety in terms of osteoarthritis changes, medial meniscus status and previous surgeries. Second, the relatively small number of patients does not allow statistical analysis between small subgroups, though it is not extremely frequent to see these complex cases in the clinical practice. Third, the mid-term follow-up may be short to evaluate the outcome of a salvage procedure as combined ACL reconstruction/revision and closing-wedge osteotomy with chronic ACL deficiency, varus alignment and initial medial osteoarthritis. Finally, fourth, since we had no control group of patients treated in another way, we compared our results to the available literature, and owing to variability in patient selection and methods, such a comparison was only an approximation.
Conclusions
The combined ACL reconstruction or revision and closing-wedge HTO procedure described in this study allowed patients with medial osteoarthritis, varus alignment and chronic ACL deficiency to restore knee laxity, correct alignment and resume a recreational level of activity at 6.5 years of follow-up. This one-stage procedure in such complex cases has to be considered a salvage procedure aiming to improve the function, reduce the pain and avoid early prosthetic resurfacing.
References
Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P (2007) The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy 23(8):852–861
Bonin N, Ait Si Selmi T, Donell ST, Dejour H, Neyret P (2004) Anterior cruciate reconstruction combined with valgus upper tibial osteotomy: 12 years follow-up. Knee 11(6):431–437
Boss A, Stutz G, Oursin C, Gächter A (1995) Anterior cruciate ligament reconstruction combined with valgus tibial osteotomy (combined procedure). Knee Surg Sports Traumatol Arthrosc 3(3):187–191
Brandon ML, Haynes PT, Bonamo JR, Flynn MI, Barrett GR, Sherman MF (2006) The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy 22(8):894–899
Dejour H, Neyret P, Boileau P, Donell ST (1994) Anterior cruciate reconstruction combined with valgus tibial osteotomy. Clin Orthop Relat Res 299:220–228
Demange MK, Camanho GL, Pécora JR, Gobbi RG, Tirico LE, da Mota e Albuquerque RF (2011) Simultaneous anterior cruciate ligament reconstruction and computer-assisted open-wedge high tibial osteotomy: a report of eight cases. Knee 18(6):387–391
Ducat A, Sariali E, Lebel B, Mertl P, Hernigou P, Flecher X, Zayni R, Bonnin M, Jalil R, Amzallag J, Rosset P, Servien E, Gaudot F, Judet T, Catonné Y (2012) Posterior tibial slope changes after opening- and closing-wedge high tibial osteotomy: a comparative prospective multicenter study. Orthop Traumatol Surg Res 98(1):68–74
Feucht MJ, Mauro CS, Brucker PU, Imhoff AB, Hinterwimmer S (2012) The role of the tibial slope in sustaining and treating anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-012-1941-6
Fujisawa Y, Masuhara K, Shiomi S (1979) The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin N Am 10(3):585–608
Hefti F, Muller W, Jakob RP, Staubli HU (1993) Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc 1(3–4):226–234
Hernigou P, Medevielle D, Debeyre J, Goutallier D (1987) Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Joint Surg Am 69(3):332–354
Imhoff AB, Linke RD, Agneskirchner J (2004) Corrective osteotomy in primary varus, double varus and triple varus knee instability with cruciate ligament replacement. Orthopade 33(2):201–207
Lattermann C, Jakob RP (1996) High tibial osteotomy alone or combined with ligament reconstruction in anterior cruciate ligament-deficient knees. Knee Surg Sports Traumatol Arthrosc 4(1):32–38
Lerat JL, Moyen B, Garin C, Mandrino A, Besse JL, Brunet-Guedj E (1993) Anterior laxity and internal arthritis of the knee. Results of the reconstruction of the anterior cruciate ligament associated with tibial osteotomy. Rev Chir Orthop Reparatrice Appar Mot 79(5):365–374
Levy AS, Meier SW (2003) Approach to cartilage injury in the anterior cruciate ligament-deficient knee. Orthop Clin N Am 34(1):149–167
Li G, Papannagari R, DeFrate LE, Yoo JD, Park SE, Gill TJ (2007) The effects of ACL deficiency on mediolateral translation and varus-valgus rotation. Acta Orthop 78(3):355–360
Marcacci M, Zaffagnini S, Giordano G, Muccioli GMM, Bruni D, Halvadjian R (2007) High tibial osteotomy: the Italian experience. Oper Tech Orthop 17(1):22–28
Marcacci M, Zaffagnini S, Iacono F, Neri MP, Loreti I, Petitto A (1998) Arthroscopic intra- and extra-articular anterior cruciate ligament reconstruction with gracilis and semitendinosus tendons. Knee Surg Sports Traumatol Arthrosc 6(2):68–75
Marti CB, Gautier E, Wachtl SW, Jakob RP (2004) Accuracy of frontal and sagittal plane correction in open-wedge high tibial osteotomy. Arthroscopy 20(4):366–372
McLean SG, Oh YK, Palmer ML, Lucey SM, Lucarelli DG, Ashton-Miller JA, Wojtys EM (2011) The relationship between anterior tibial acceleration, tibial slope, and ACL strain during a simulated jump landing task. J Bone Joint Surg Am 93(14):1310–1317
Noyes FR, Barber-Westin SD, Hewett TE (2000) High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med 28(3):282–296
Noyes FR, Schipplein OD, Andriacchi TP, Saddemi SR, Weise M (1992) The anterior cruciate ligament-deficient knee with varus alignment. An analysis of gait adaptations and dynamic joint loadings. Am J Sports Med 20(6):707–716
Pugh L, Mascarenhas R, Arneja S, Chin PY, Leith JM (2009) Current concepts in instrumented knee-laxity testing. Am J Sports Med 37(1):199–210
Torzilli PA, Deng X, Warren RF (1994) The effect of joint-compressive load and quadriceps muscle force on knee motion in the intact and anterior cruciate ligament-sectioned knee. Am J Sports Med 22(1):105–112
van de Pol GJ, Arnold MP, Verdonschot N, van Kampen A (2009) Varus alignment leads to increased forces in the anterior cruciate ligament. Am J Sports Med 37(3):481–487
Yoshimura I, Naito M, Hara M, Zhang J (2000) Analysis of the significance of the measurement of acceleration with respect to lateral laxity of the anterior cruciate ligament insufficient knee. Int Orthop 24(5):276–278
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zaffagnini, S., Bonanzinga, T., Grassi, A. et al. Combined ACL reconstruction and closing-wedge HTO for varus angulated ACL-deficient knees. Knee Surg Sports Traumatol Arthrosc 21, 934–941 (2013). https://doi.org/10.1007/s00167-013-2400-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2400-8