Abstract
Purpose
Posterior horn meniscal tears are commonly found in conjunction with anterior cruciate ligament (ACL) injury. Some believe tears in the posterior meniscocapsular zone, coined ramp lesions, are important to knee stability. The purpose of this study was to determine whether pre-operative MRI evaluation was able to accurately and reproducibly identify ramp lesions.
Methods
Three blinded reviewers assessed MRIs twice for the presence of ramp lesions in patients undergoing ACL reconstruction. Sensitivity, specificity, negative predictive value, and positive predictive value for MRI were calculated based on arthroscopic diagnosis of a ramp lesion. Intra-class correlation coefficient was calculated to assess intra- and interobserver reliability of the MRI assessment between the three examiners. Significance was set at p < 0.05.
Results
Ninety patients met inclusion criteria (45 males, 45 females, mean age 28.0 years). Thirteen of these patients had arthroscopy-confirmed ramp lesions, while the other 77 had other meniscal pathology. Sensitivity of detecting a ramp lesion on MRI ranged from 53.9 to 84.6%, while specificity was 92.3–98.7%. Negative predictive value was 91.1–97.4%, while positive predictive value was 50.0–90.0%. Inter-rater reliability between three reviewers was moderate at 0.56. The observers had excellent intra-rater reliability ranging from 0.75 to 0.81.
Conclusions
This study demonstrates high sensitivity and excellent specificity in detecting meniscal ramp lesions on MRI. Ramp lesions are likely more common and may have greater clinical implications than previously appreciated; the outcomes of untreated lesions must be investigated. Pre-operative identification of ramp lesions may aid clinicians in surgical planning and patient education to improve outcomes by addressing pathology which may have otherwise been missed.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Meniscal tears are common in conjunction with anterior cruciate ligament (ACL) injury [17]. A lesion of the peripheral attachment of the posterior medial meniscus, coined ramp lesion, has been described as being common with ACL rupture, ranging in prevalence from 9.3 to 17% [3, 11]. Due to its location, visualization may be difficult during standard knee arthroscopy using only anteromedial and anterolateral portals [16, 19]. These lesions therefore may commonly be overlooked and if not appropriately addressed may impart pain, abnormal knee kinematics, instability, and increased ACL strain [5, 14, 16, 20].
The medial meniscus, particularly the posterior horn, has been found to confer an important amount of stability in regard to anterior tibial translation [1, 9, 13, 17]. The integrity of the meniscus is important in ACL-deficient knees as forces are increased in the posterior horn of the medial meniscus [14]. Due to the importance of the posterior horn of the medial meniscus in ACL-deficient knees and difficulty in visualization of ramp lesions with standard knee arthroscopy, identification of ramp lesions pre-operatively may allow surgeons to more consistently address these lesions intra-operatively. Unfortunately, many times these injuries may be overlooked on MRI, and the authors are not aware of published studies evaluating the sensitivity and specificity in identifying ramp lesions on MRI [4].
Due to the proposed importance of the posterior horn of the medial meniscus in ACL-deficient knees, identification of a ramp lesion pre-operatively may allow the surgeon to appropriately intervene and therefore improve outcomes, particularly during concomitant ACL reconstruction. This may lead to improved knee stability, more normal kinematics, and less graft strain compared to knees with unaddressed ramp lesions [19].
The purpose of this study was to determine whether pre-operative MRI evaluation is able to accurately and reproducibly identify ramp lesions. It was hypothesized that identification of ramp lesions on MRI is possible with high sensitivity and specificity. Current literature is sparse regarding accuracy of MRI evaluation of ramp lesions. If these lesions are able to be identified reliably on MRI, this may aid the surgeon in surgical planning; if MRI identification is poor, direct visualization of the region may be paramount.
Materials and methods
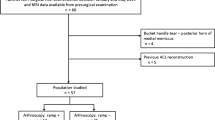
Inclusion criteria were (1) acute ACL injury treated with ACL reconstruction consecutively from 2013 to 2015, (2) age 14–45, (3) had a supine 1.5-Tesla MRI with 3 mm slice thickness (GE signal, GE Healthcare, USA) with the knee near full extension performed pre-operatively, and patients with intra-operative findings of posterior medial meniscocapsular separation (ramp lesion). A control group was also collected with inclusion criteria being acute ACL injury, age 14–45 years old who underwent ACL reconstruction surgery during that same time period, and had a pre-operative MRI. Subjects were excluded if they had a partial ACL disruption, two or more ligamentous injuries, previous surgery on the involved knee, or high-grade articular cartilage defects.
Intra-operatively, in each patient with concern for posterior medial meniscus or ramp lesion pathology based on MRI (Fig. 1) or initial diagnostic arthroscopy, a standard posteromedial portal was established, and the posterior medial meniscus and meniscocapsular junction were evaluated for injury using a 70° arthroscope. If a meniscocapsular separation was identified (Fig. 2), the injury was abraded (Fig. 3a) and a curved suture passer was inserted through the posteromedial portal. The curved suture passer was then used to penetrate both the capsule and meniscus (Fig. 3b), and a non-braided suture was passed through the lesion. This suture was then tied arthroscopically (Fig. 3c), reducing and securing the meniscocapsular injury as previously described [15]. The repair was then evaluated with a probe via standard anteromedial and anterolateral portals with a 70° scope using the Gilchrist view.
a Sagittal T2 MRI showing high signal irregularity with complete fluid filling between the posterior horn of the medial meniscus and capsular margin indicating a ramp lesion (arrow); b sagittal T2 MRI demonstrating a meniscocapsular separation (ramp lesion) as well as a commonly seen increased signal in the posteromedial tibial plateau consistent with a bone bruise (arrow)
Gilchrist view using a 70° scope with the medial condyle labelled with an arrowhead, posteromedial meniscus with a star, and the posterior medial capsule with an arrow; a, a rasp abrading the meniscocapsular junction through the posteromedial portal using a cannula; b, a suture hook capturing the posteromedial capsule before being passed through the meniscus to fix this meniscocapsular separation; c, final fixation of the meniscocapsular separation
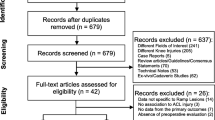
After surgical procedures were complete, images were randomized and blinded to intra-operative findings. The number of control patients included in this study was determined to replicate the assumed 9–17% incidence of these injuries in ACL-injured patients as reported in the literature [3, 10]. Images were independently reviewed twice by three reviewers, with 2 months between the three physician’s evaluations. The presence of either a fluid signal, which previously have been shown as the most specific sign on MRI [6], or an obvious separation between the posterior capsule and the posterior medial meniscus on MRI was documented (Figs. 1, 2) by each reviewer on sagittal MRI.
Institutional review board approval was obtained by the University of Pittsburgh before initiation of this study (PRO12020619).
Statistical analysis
Data analysis was performed using SPSS 24 for Mac (IBM, Armonk New York, USA). Intra-class correlation coefficient was calculated to assess intra- and interobserver reliability of the MRI assessment (ICC (3,1)). Further, sensitivity, specificity, negative, and positive predictive values in diagnosis of ramp lesions were calculated. The significance level was set to a p value of less than 0.05.
Results
A total of 90 patients met inclusion criteria (45 males, 45 females, mean age 28.0 years (SD = 10.0)) and were included for the final analysis. All patients had complete acute ACL disruptions intra-operatively and on MRI evaluation. Thirteen of these patients had arthroscopy-confirmed ramp lesions, while the other 77 had pathology involving the body of the meniscus. The average time interval between MRI and surgical intervention was 57.3 days (SD = 44.1).
Sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV) are displayed in Table 1. The three observers had excellent intra-rater reliability ranging from 0.75 to 0.81 (Table 1) and inter-rater reliability was moderate between the three reviewers at 0.56.
Discussion
The most important finding of this study was that there was moderate to high sensitivity (53.9–84.6%) and excellent specificity (92.3–98.7%) in detecting meniscal ramp lesions on MRI. The negative predictive value was high (91.1–97.4%) and the positive predictive value was slightly lower (50.0–90.0%), with greater variation, in identifying these lesions on MRI. These results indicate that MRI is an excellent test to rule out ramp lesions but slightly less accurate in capturing all ramp injuries. Likely slice thickness, MRI resolution, and other posterior medial meniscal injuries can affect the detection of these injuries on MRI. Therefore, MRI is effective in evaluation and identification of posterior medial meniscocapsular (ramp) injuries; however, arthroscopic evaluation remains the gold standard. Importantly, these lesions may be missed if evaluated solely with pre-operative imaging, and the implications of a missed injury are not currently known. Therefore, it is recommended to routinely use a 70° arthroscope using the Gilchrist view to evaluate the posteromedial corner during ACL reconstruction.
Studies evaluating ramp lesions on MRI are limited and have not reported specific statistical parameters or methods of evaluation of ramp lesions on MRI. Those studies that do exist report ranges in sensitivity from 0 to 77% [3, 5, 11]. One abstract presented at the 2015 American Academy of Orthopaedic Surgery (AAOS) Annual Meeting evaluated 337 patients and found 44 ramp lesions (13.1% incidence) intra-operatively, 33 of which were identified on MRI (77% sensitivity). However, this study only reviewed MRI reports, and many times these meniscocapsular injuries are not closely evaluated on routine MRI [5]. An ePoster at the 2013 ISAKOS Biennial Congress evaluated ramp lesions intra-operatively in 92 knees with a posteromedial portal and found 23 knees (25%) with ramp lesions. Fourteen of these 23 knees (61%) were found to have meniscocapsular separation on MRI, and this group stated that the T2*-weighted gradient-echo sagittal image was best in identifying this pathology. The study also reported that younger patients more commonly had ramp lesions and they recommend routine evaluation with a posteromedial viewing portal, as implications in missing a ramp lesion may be quite significant [7]. In both studies, the methods of evaluation on MRI were not presented and no other parameters or statistics (i.e. specificity, positive predictive value, or negative predictive value) were reported. On the contrary, the current study indicates that MRI is a good tool for pre-operative evaluation of meniscocapsular separation as the negative predictive value is high, indicating that >90% who do not show evidence of a ramp lesion on MRI will not have one on arthroscopy.
The prevalence of ramp lesions intra-operatively also varies greatly in the literature with no clear agreement, ranging from 9.3 to 16.6% with younger patients being affected more in some studies, but all occurrences of ramp lesions being associated with ACL injury or ACL graft failure [3, 11, 19]. One study reported an incidence of 9.3% intra-operatively in 183 ACL reconstruction patients and no ramp lesions found intra-operatively were identified pre-operatively on MRI. They cited mild anteromedial rotatory subluxation as the pre-operative finding with this condition; however, this was subjective. The author states this injury may be difficult to visualize on MRI because with the knee near full extension, the meniscocapsular separation is reduced [3].
Risk factors for development of meniscocapsular separations are unknown. One recent study recognized the importance of ramp lesions and investigated medial meniscal slope as a contributor, as this has been shown to be an independent risk factor for noncontact ACL injury. This group reviewed MRIs of 53 ramp lesions found on arthroscopy during ACL reconstruction and determined the medial meniscal slope to be 1.5° greater in patients with ramp lesions when compared to those with ACL injury only, particularly in patients who waited greater than 6 months for surgery [18]. This study further stressed the importance in diagnosis and treatment of these injuries in a timely manner.
Studies evaluating the best arthroscopic technique to identify ramp lesions are limited. One study of 302 ACL reconstructions more closely investigated the use of a posteromedial portal to identify otherwise unrecognized pathology. They found the prevalence of ramp lesions to be 40% of all medial meniscal injuries and found a high rate (16.8%) of missed meniscocapsular injury before addition of the posteromedial portal. They also therefore recommend the addition of a posteromedial portal for viewing as well as debridement of the region as lesions can also be “hidden” under a membrane-like structure [19]. Another study of 39 patients undergoing ACL reconstruction evaluated the posteromedial meniscus sequentially with the anterolateral portal, intercondylar view, and a posteromedial portal and found that addition of the intercondylar view identified four more lesions, while the posteromedial portal found two more lesions not seen on either previous view. The authors submit that an intercondylar view as well as a posteromedial portal should be routine in ACL reconstruction, particularly in delayed surgery [16].
The consequences of a missed ramp lesion are not well defined. One cadaveric study of nine knees found increased anterior tibial translation and external rotation after sectioning the posteromedial meniscocapsular junction in cadavers with ACL deficiency, and this was not restored after ACL reconstruction alone, but was after the ramp lesion was repaired [20]. Further, numerous repair techniques exist; however, many have not been well defined. One study of 132 patients undergoing ACL reconstruction who were found to have ramp lesions underwent repair using a posteromedial portal technique, similar to the current study. These authors found an increase in subjective and objective clinical data at an average of 27 months, indicating that this technique is safe and effective [21]. Another recent prospective study treated 40 ACL reconstruction patients with repair and 33 ACL reconstruction patients with abrasion and trephination and found no difference in outcomes scores, clinical measures, or MRI evaluation at 2-year minimum follow-up [12]. Although both beyond the scope of this study, the use of a posteromedial portal should be considered, particularly in patients with a high degree of laxity, and further research is needed to define the best treatment modalities [2, 8, 10, 12, 15].
Limitations of this study include the possibility that patients developed meniscocapsular separations after MRI and therefore would only be found on arthroscopy. Further, a higher-resolution MRI (3T) may provide better evaluation for ramp lesions; however, 1.5 T as used in this study is more common and therefore more generally applicable. Although not determined in this study, ramp lesions are more common and may have greater clinical implications than previously appreciated, including continued instability after ACL reconstruction if medial meniscocapsular ramp lesions are not appropriately repaired at the time of surgery [14]. Pre-operative identification of ramp lesions using MRI may aid clinicians in surgical planning and patient education. By addressing pathology appropriately, which may have otherwise been missed, outcomes and patient satisfaction may be improved.
Conclusions
This study found moderate to high sensitivity and excellent specificity in detecting meniscal ramp lesions on MRI. While MRI is good in identifying posterior medial meniscocapsular injuries, arthroscopic evaluation remains the gold standard, as the implications of untreated meniscocapsular injuries are unknown.
References
Ahn JH, Bae TS, Kang KS, Kang SY, Lee SH (2011) Longitudinal tear of the medial meniscus posterior horn in the anterior cruciate ligament-deficient knee significantly influences anterior stability. Am J Sports Med 39:2187–2193
Ahn JH, Wang JH, Yoo JC (2004) Arthroscopic all-inside suture repair of medial meniscus lesion in anterior cruciate ligament–deficient knees: results of second-look arthroscopies in 39 cases. Arthroscopy 20:936–945
Bollen SR (2010) Posteromedial meniscocapsular injury associated with rupture of the anterior cruciate ligament: a previously unrecognised association. J Bone Joint Surg Br 92:222–223
Chahla J, Dean CS, Moatshe G, Mitchell JJ, Cram TR, Yacuzzi C, LaPrade RF (2016) Meniscal ramp lesions: anatomy, incidence, diagnosis, and treatment. Orthop J Sports Med 4:2325967116657815
Edgar CWJ, Obopilwe E, Ziegler C, Reed D, Arciero RA (2015) Posteromedial meniscocapsular tear: prevalence, detection sensitivity, biomechanics, and repair technique. Paper presented at the American academy of orthopaedic surgeons annual meeting, Las Vegas, NV, 24–28 March 2015
Hash T (2013) Magnetic resonance imaging of the knee. Sports Health 5:78–107
Hatayama KKM, Ogoshi A, Takagishi K (2013) Ramp lesion associated with anterior cruciate ligament rupture. Paper presented at the international society of arthroscopy, knee surgery and orthopaedic sports medicine biennial congress, Toronto, Canada
Keyhani S, Ahn JH, Verdonk R, Soleymanha M, Abbasian M (2016) Arthroscopic all-inside ramp lesion repair using the posterolateral transseptal portal view. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-016-4410-9
Levy IM, Torzilli PA, Warren RF (1982) The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am 64:883–888
Li WP, Chen Z, Song B, Yang R, Tan W (2015) The FasT-Fix repair technique for ramp lesion of the medial meniscus. Knee Surg Relat Res 27:56–60
Liu X, Feng H, Zhang H, Hong L, Wang XS, Zhang J (2011) Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med 39:832–837
Liu X, Zhang H, Feng H, Hong L, Wang XS, Song GY (2016) Is it necessary to repair stable ramp lesions of the medial meniscus during anterior cruciate ligament reconstruction? Am J Sports Med. doi:10.1177/0363546516682493
Lorbach O, Kieb M, Herbort M, Weyers I, Raschke M, Engelhardt M (2015) The influence of the medial meniscus in different conditions on anterior tibial translation in the anterior cruciate deficient knee. Int Orthop 39:681–687
Mariani PP (2011) Posterior horn instability of the medial meniscus a sign of posterior meniscotibial ligament insufficiency. Knee Surg Sports Traumatol Arthrosc 19:1148–1153
Park IS, Kim SJ (2006) New meniscus repair technique for peripheral tears near the posterior tibial attachment of the posterior horn of the medial meniscus. Arthroscopy 22:908-e901–908-e904
Peltier A, Lording TD, Lustig S, Servien E, Maubisson L, Neyret P (2015) Posteromedial meniscal tears may be missed during anterior cruciate ligament reconstruction. Arthroscopy 31:691–698
Smith JP 3rd, Barrett GR (2001) Medial and lateral meniscal tear patterns in anterior cruciate ligament-deficient knees. A prospective analysis of 575 tears. Am J Sports Med 29:415–419
Song GY, Liu X, Zhang H, Wang QQ, Zhang J, Li Y, Feng H (2016) Increased medial meniscal slope is associated with greater risk of ramp lesion in noncontact anterior cruciate ligament injury. Am J Sports Med 44:2039–2046
Sonnery-Cottet B, Conteduca J, Thaunat M, Gunepin FX, Seil R (2014) Hidden lesions of the posterior horn of the medial meniscus: a systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med 42:921–926
Stephen JM, Halewood C, Kittl C, Bollen SR, Williams A, Amis AA (2016) Posteromedial meniscocapsular lesions increase tibiofemoral joint laxity with anterior cruciate ligament deficiency, and their repair reduces laxity. Am J Sports Med 44:400–408
Thaunat M, Jan N, Fayard JM, Kajetanek C, Murphy CG, Pupim B, Gardon R, Sonnery-Cottet B (2016) Repair of meniscal ramp lesions through a posteromedial portal during anterior cruciate ligament reconstruction: outcome study with a minimum 2-year follow-up. Arthroscopy 32:2269–2277
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All co-authors declare they have no conflict of interest.
Funding
No funding was used for this study.
Ethical approval
This study was performed with the ethical standards of the institution and with the 1964 Helsinki declaration and its later amendments.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Arner, J.W., Herbst, E., Burnham, J.M. et al. MRI can accurately detect meniscal ramp lesions of the knee. Knee Surg Sports Traumatol Arthrosc 25, 3955–3960 (2017). https://doi.org/10.1007/s00167-017-4523-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4523-9