Abstract
To investigate the functional role of fasudil in optic nerve crush (ONC), and further explore its possible molecular mechanism. After ONC injury, the rats were injected intraperitoneally either with fasudil or normal saline once a day until euthanized. RGCs survival was assessed by retrograde labeling with FluoroGold. Retinal glial cells activation and population changes (GFAP, iba-1) were measured by immunofluorescence. The expressions of cleaved caspase 3 and 9, p-ERK1/2 and p-AKT were detected by western blot. The levels of the pro-inflammatory cytokines were determined using real-time polymerase chain reaction. Fasudil treatment inhibited RGCs apoptosis and reduced RGCs loss demonstrated by the decreased apoptosis-associated proteins expression and the increased fluorogold labeling of RGCs after ONC, respectively. In addition, the ONC + fasudil group compared had a significantly lower expression of GFAP and iba1 compared with the ONC group. The levels of pro-inflammatory cytokines were significantly reduced in the ONC + fasudil group than in the ONC group. Furthermore, the phosphorylation levels of ERK1/2 and AKT (p-ERK1/2 and p-AKT) were obviously elevated by the fasudil treatment. Our study demonstrated that fasudil attenuated glial cell-mediated neuroinflammation by up-regulating the ERK1/2 and AKT signaling pathways in rats ONC models. We conclude that fasudil may be a novel treatment for traumatic optic neuropathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traumatic optic neuropathy (TON), characterized by significant visual impairment and even blindness, is an irreversible injury of the optic nerve caused bytrauma [1,2,3,4,5,6,7]. The main mechanism of TON is retinal ganglion cells (RGCs) apoptosis [7] and axon degeneration, which may be mediated by glial cells dysfunction and optic nerve inflammation. Optic nerve crush (ONC) have been reported and share similar features, indicating that ONC is an excellent working animal model of TON. However, the underlying pathophysiologic and molecular mechanisms remain far from clear.
Inflammation is the basic response to optic nerve injury [8]. Growing evidence shows that ONC triggers inflammatory response produced by activated retinal glial cells, further aggravates the loss of RGCs [9,10,11,12]. Indeed, neuroinflammation involves the activation of glial cells and the release of proinflammatory cytokines [13]. Retinal glial cells, including microglia, astrocytes, Müller cells and so on, play crucial roles in maintaining retinal homeostasis and protecting retinal neurons [14]. Under pathological conditions, glial cells become activated and produce pro-inflammatory cytokines [15,16,17] such as IL-1β, IL-6, COX-2, and TNF-α [18]. These pro-inflammatory cytokines can convey neurotoxicity to RGCs [16,17,18,19]. In view of this, agents aimed at modulating the neuroinflammatory responses have attracted the attention of researchers. Although many agents have been tested in animal models where they have been effective in attenuating glial cell-mediated neuroinflammation [8, 20, 21]. To date, however, there is no effective clinical treatment for TON. Thus, searching for novel agents that can attenuate glial cell-mediated neuroinflammation may be particularly beneficial [7, 22].
Recently, some studies provided evidence that the ERK1/2 and Akt pathways mediated neuroprotection after injury [23,24,25,26]. Pernet et al. have shown that the activation of ERK1/2 by ciliary neurotrophic factor attenuated glial cells-mediated neuroinflammation and increased RGCs survival after optic nerve injured [27]. Besides, the ERK1/2 pathways was known to participate in LPA1-driven microglial activation [28]. Furthermore, compound C (CC) inhibited neuroinflammation and protected nerve through the activation of the ERK1/2 and AKT pathways [29, 30]. Moreover, G-CSF may play a neuroprotective role by activating AKT phosphorylation after ONC [31, 32]. In addition, Brimonidine fueled optic nerve regeneration after injury by activating ERK1/2 [23]. Therefore, the activation of ERK1/2 and AKT signaling pathways may inhibit the activation of glial cells and attenuate glial cells-mediated neuroinflammation.
Fasudil, a selective Rho-Associated Protein Kinase (ROCK) inhibitor [4, 5, 7, 33,34,35], is primarily used to treat subarachnoid hemorrhage (SAH) [34, 36], pulmonary hypertension [37, 38], cardiovascular diseases [39] and cerebral vasospasms after subarachnoid hemorrhage [40]. Most studies to date showed beneficial treatment effects of fasudil in treating central nervous system disease in animal models, such as stroke [41], cerebral infarct [42], cerebral vasospasm [33, 42, 43], Parkinson [11, 44], and traumatic spinal cord injury [33, 36]. Mounting amount of evidence have shown that the neuroprotective and cardioprotective effects of fasudil was via the AKT and ERK1/2 pathways [45,46,47,48,49,50]. Furthermore, fasudil attenuates the inflammatory response by shifting of microglial M1 polarization toward the M2 phenotype [51, 52]. Also, fasudil has been found to attenuate glial cells-mediated neuroinflammation in a New Zealand rabbit optic nerve injury model [7]. However, the mechanism by which fasudil attenuates glial cells-mediated neuroinflammation in the rats ONC model remain unclear.
The purpose of this research, therefore, is to verify the hypothesis that fasudil attenuates glial cells-mediated neuroinflammation via activating the ERK1/2 and AKT signaling pathways in the rats ONC model.
Materials and methods
Animals
Adult male Sprague Dawley rats (10 weeks, weight 250 ± 30 g) were cared for by the Medical Laboratory Animal Center of Guangxi Medical University (Nanning, China). All experiments were approved by the Ethics Committee of the People’s Hospital of Guangxi Zhuang Autonomous Region and performed in accordance with the Association for Research in Vision and Ophthalmology (ARVO) Statement for the Use of Animals in Ophthalmic and Vision Research.
ONC model
The ONC model was constructed on 10-week-old rats as described previously with slight modification [50, 53,54,55,56]. 1% Pentobarbital Sodium (50 mg/kg) was injected intraperitoneally to anesthesia rats. After anesthesia, the eye was routinely disinfected. The left optic nerve was surgically exposed and squeezed 2 mm behind the eyeball for 10 s. After the operation, funduscopic examination revealed that the retinal blood supply remained intact, and then ofloxacin ointment was applied topically. The right optic nerve was exposed but without crushed. The study of Berkelaar et al. suggests that axotomy causes a loss of RGCs in a delayed pattern, and the number of RGCs was significantly reduced at days 14 [57]. Besides, there are studies also have shown that ONC caused a significant decrease of RGCs and a increase of retinal glial cells, which peaks on day 14 [58,59,60,61]. Therefore, the 14-day time point was chosen for the subsequent experiments. All rats were euthanized by CO2 pneumoperitoneum 14 days after ONC.
Fasudil administration
The rats were randomly assigned to four groups: control group (sham surgery control), fasudil group, ONC group, and ONC + fasudil group). Animals were given an intraperitoneal injection of normal saline or fasudil (10 mg/kg/day, 30 rats) (Sigma Chemical Co., St. Louis, MO) once daily for 14 consecutive days following model building. The choice of concentrations of fasudil for this study were based on previous research [33, 62, 63]. None of the rats were lost or died during the specified survival time.
Retrograde labeling of RGCs with FluoroGold
The retrograde labeling of FluoroGold (FG) has been used for morphometry analysis of RGCs after injury as described in previous studies [64, 65]. To distinguish RGCs from glial cells, RGCs were retrogradely labeled with FG (4%, Colorado). Briefly, 7 days before the establishment of rats ONC model [59, 66,67,68], midline incisions of approximately 1.2 cm in length were made on the rat head, exposing the sagittal and lambda suture. Holes (1 mm diameter) were then drilled into the skull 2.5 mm rostral to lambda and 1.2 mm lateral to the sagittal sutures based on rat brain stereotaxic coordinates. 4 μl FG was injected 3 mm deep into the superior colliculi using a 10 μl microsyringe. Following euthanasia of the rats, eye balls were enucleated immediately and fixed with 4% paraformaldehyde (PFA). Retinas dissected and flat mounted. Labeled RGCs were counted in three areas (62,500 μm2 each) per retinal quadrant (n > 6 in each group) and the average was calculated under fluorescence microscope (Leica Microsystems; Mannheim, Germany). RGC survival percentage was defined as RGCs density ratios between left eyes with an right eyes multiplied by 100 [69, 70].
Western blot analysis
Western blot were performed as described previously [50, 55, 71]. Retinal tissues of 5 rats each group were collected and stored at − 80 °C. Retinal proteins were extracted using RIPA buffer (Beyotime) and quantified using the BCA assay (Thermo). After SDS-PAGE, PVDF membranes were blocked with 5% non fat milk, followed by overnight incubation with primary antibodies for mouse monoclonal anti-caspase-3, mouse monoclonal anti-caspase-9, rabbit polyclonal anti-cleaved-caspase-3, rabbit polyclonal anti-cleaved-caspase-9, mouse monoclonal anti-p44/42 (ERK1/2), rabbit monoclonal anti-Phospho-p44/42 MAPK (p-ERK1/2), mouse monoclonal anti-AKT, mouse monoclonal anti-Phospho-AKT, or rabbit polyclonal anti-β-actin at 4℃. All labeled antibodies were purchased from Cell Signaling Technology, except antibody against β-actin (Abcam). After three 5-min PBST washes, the membranes were incubated with secondary antibodies (SouthernBiotech) for additional 1 h at room temperature. Finally, the bands were visualized by ECL Plus(Amersham), and quantified by ImageJ software (NIH, Bethesda, MD).
Immunofluorescence and cell counting of microglial and macroglia
Eyes from euthanized rats were removed, fixed overnight in 4% PFA, cryoprotected with 30% sucrose afterwards. Tissues were embedded in optimum cutting temperature compound (OCT, Leica Biosystems, Shanghai, China) overnight and 7 μm thick frozen sections were prepared for immunofluorescence staining. After being washed with PBS, nonspecific sites were blocked by incubation with 5% bovine serum albumin (BSA) for 2 h Subsequently, the sections were incubated overnight with either rabbit polyclonal anti-iba1 (a microglial cells marker; #019-19741, Wako) or rabbit monoclonal anti-GFAP (an astrocyte marker; #MAB3402, Millipore) primary antibody in a humidified box, followed by Alexa Fluor 488 or 555 (Invitrogen) secondary antibodies 2 h at room temperature and finally DAPI (Sigma-Aldrich). Finally, imaging of the stained sections were photographed using confocal microscopy (Germany). The number of microglia or macroglia was calculated and then average was worked out. Finally, the numbers of iba1-positive cells and GFAP-positive cells were quantified using the cellcounter tool in ImageJ.
Quantitative real-time PCR (qPCR)
Sample collection, RNA isolations and qPCR were carried out as previously described [53, 72]. Total RNA of retinal cells was extracted by Trizol (Invitrogen) and reversed-transcribed into cDNA by using a cDNA first-strand synthesis kit (Fermentas). The Primers were designed to amplify within a 200-bp length according to the NCBI Primer-Blast (Table 1). PCR steps was as follows: 50 °C for 2 min, 95 °C for 10 min, followed by 40 cycles of 95 °C for 15 s and 60 °C for 1 min. Fluorescence signals were detected during the extended phase. Each sample was detected three times with the 6-point standard curve. qPCR was performed with SYBR Green (Biotool, Houston). The results were expressed as percentages. The expression of target genes calculated as normalized ratio and normalized to β-actin using the 2−∆∆Cq method.
Statistical analysis
All of the values were presented as mean ± standard deviation (SD) and analyzed using one-way analysis of variance (ANOVA) followed by Turkey’s posthoc multiple comparison tests. All statistical analysis were done using GraphPad Prism 6.0 (GraphPad Software). A p-value < 0.05 was considered statistically significant. Each experiment involved at least three repetitions.
Results
Fasudil reduced the loss of RGCs after ONC
To investigate the protective effects of fasudil on optic nerve injury induced by ONC, FG retrograde labeling was performed in all groups, and the surviving RGCs were visible as a round shape (Fig. 1a–d). FG-positive RGCs were remained viable 14 days post-ONC, but in significantly decreased number(1043 ± 52 cells/mm2, Fig. 1b, e, #p < 0.001). Notably, fasudil dramatically inhibited the loss of RGCs and improved survival after ONC (1890 ± 83 cells/mm2, **p < 0.001). After 14 days of treatment, no notable differences in the number of RGCs were found between the control (2642 ± 182 cells/mm2) and control + fasudil (2530 ± 231 cells/mm2) groups, indicating that fasudil had no cytotoxicity to RGCs. These results suggested that fasudil played a neuroprotective role in the ONC animal model.
The protective effects of fasudil in RGCs after ONC. The photos of retina in each group were captured using a fluorescence microscope. Scale bar = 100 μm. a Con group; b fasudil group; c ONC group; d ONC + fasudil group. e The number of FG-positive RGCs in each group was counted (mean ± SEM, n = 6). (#p < 0.001 vs. the control group; **p < 0.001 vs. the ONC group). Con control, ONC optic nerve crush, RGCs retinal ganglion cells
Fasudil attenuated apoptosis of RGCs after ONC
ONC is an acute axonal damage model that leads to cell apoptotic in RGCs. Caspase-3 and caspase-9 are the principal effector caspases in the execution of apoptotic cell death [25, 73, 74]. To further explore the impact of fasudil on RGCs apoptosis, we used western blot to assess the expression of apoptosis-related proteins as mentioned above (Fig. 2a). The relative amount of cleavage of caspases 3 or 9, normalized to respective total protein as a loading control, was calculated as a ratio. The results showed that there was no significant difference in the protein expression level of total caspases 9 and 3 between all groups. Of note, the ONC group showed statistically increased levels of cleavage of caspases 3 and 9 (#p < 0.001). However, after treatment with fasudil, these expression levels were significantly reduced (**p < 0.001). In general, these results indicate that fasudil may upregulate the phosphorylation levels of caspase 3 and 9, which is further favorable to the anti-apoptotic effect on RGCs (Fig. 2b, c).
Fasudil inhibited ONC-induced caspase-3/9 activation in the retina after ONC. a Western blot analysis assessed the protein level of total caspases 9/3 and cleavage of caspases 9/3. β-actin was used as a loading control. Gel bands were subjected to densitometric analysis, and the relative cleaved-caspase-3/9 level was calculated as cleaved-caspase-3/9 level divided by totalcaspase3/9 level (mean ± SEM, n = 10). (#p < 0.001 vs. the control group, **p < 0.001 vs. the ONC group). ONC optic nerve crush
Fasudil restrained the activation of retinal glial cells after ONC
The retinal glial cells undergo significantly morphological and behavioral changes and switch from a quiescent state to a highly active state after ONC injury [22, 75]. Then, to determine whether the effect of fasudil on retinal glial cells was correlated with its neuroprotective function, the expressions of the GFAP and iba-1 were detected and the number of microglia or macroglia cells was counted by immunofluorescence (Fig. 3). As showed in Fig. 3a, the expression of GFAP and iba-1 was dramatically elevated in the ONC group compared with the control group (#p < 0.001), and was markedly reduced after fasudil treatment (**p < 0.001). In addition, ONC resulted in the increases in the number of microglia and macroglia cells (#p < 0.001). However, these expansion in cell numbers were inhibited by fasudil treatment (**p < 0.001). Overall, our results suggested that fasudil inhibited the activation of retinal glial cells after ONC.
Fasudil exerted its rewarding effect through inhibition of ONC-induced glial cells activation. a Retinal sections were stained with the GFAP (green), Iba1 (red) and DAPI (blue), and viewed on a confocal microscope. Scale bar = 100 μm. The stained cells were dropped onto slides and imaged by confocal microscopy. Densitometric analysis was used to quantify the number of macroglia (b) and macroglia (c). Values are expressed as mean ± s.e.m. *p < 0.05; Data were means ± SEM of multiple experiments (n = 8; #p < 0.001 vs. the control group; **p < 0.001 vs. the ONC group). GFAP glial fibrillary acidic protein, Iba1 ionized calcium binding adapter molecule 1, ONC optic nerve crush. (Color figure online)
Fasudil inhibited optic nerve inflammation after ONC
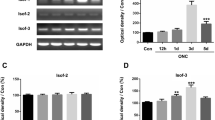
Then, to further investigate the anti-inflammatory effects of fasudil, we determined the mRNA level of IL-6, IL-1β, COX-2, and TNF-α in the retina by qPCR. As expected, the mRNA expression levels of these proinflammatory cytokines were significantly increased after ONC (#p < 0.001), while were decreased after treatment with fasudil (**p < 0.001) (Fig. 4a–d). Our results indicated that fasudil inhibited the mRNA expression of proinflammatory cytokines after ONC. Namely, fasudil played a key anti-inflammatory role during optic nerve provoked by ONC.
Fasudil played an anti-inflammatory role in ONC, as reflected by transcriptional inhibition of proinflammatory cytokines. The mRNA levels of proinflammatory cytokines genes were assayed via qPCR (mean ± SEM, n = 6). a IL-6, b IL-1β, c COX-2, and d TNF-α (#p < 0.001 vs. the control group; **p < 0.001 vs. the ONC group). IL-6, interleukin 6; IL-1β, interleukin 1β; COX-2, cyclooxygenase-2; TNF-α, tumor necrosis factor-α; ONC, optic nerve crush
Fasudil up-regulated ERK1/2 and AKT pathway after ONC
Previous studies demonstrated that fasudil administration leads to ERK1/2 and AKT phosphorylation [27, 76]. To explore whether fasudil protect RGCs from apoptosis via ERK1/2 and AKT pathways, the total and phosphorylated levels of ERK1/2 and AKT were detected by western blot (Fig. 5a). The relative amount of phosphoprotein levels, normalized to total level of the corresponding protein as a loading control respectively was calculated as a ratio. As expected, there was no significant difference between the total levels of ERK1/2 or AKT for each group. Moreover, the phosphorylation levels of ERK1/2 and AKT increased slightly after ONC, but the change was not statistically (#p > 0.05). And we considered this change was triggered by ONC stress. Following treatment with fasudil, the levels of the above phosphorylated protein significantly increased (Fig. 5, **p < 0.001). The above results further implicate that fasudil can activate the ERK1/2 and AKT pathway, and the activation of these signalings can inhibited the activation of retinal glial cells and the apoptosis of RGCs after ONC.
Fasudil induce activation of ERK1/2 and AKT pathways after ONC. a Western blot analysis assessed the phosphorylated and total levels of ERK1/2 and AKT. β-actin served as an internal loading control. Densitometric analysis of bands was performed, and relative p-ERK1/2 (b) or p-AKT (c) level was calculated as phosphorylated proteins level divided by the corresponding values of total proteins level, respectively (mean ± SEM, n = 10). (**p < 0.001 vs. the ONC group). ONC optic nerve crush, ERK1/2 extracellular regulated protein kinases ½, AKT protein kinase B, p phosphorylated, t total
Discussion
TON is a serious vision threatening condition. However, there is no proven-effective therapy and interventions that can reverse the optic nerve degeneration and recover the vision. In this present study, our results demonstrated that fasudil directly attenuated RGCs apoptosis and increased the survival rate of RGCs via inhibiting caspase3 and caspase9 cleavage in retina after ONC. In addition, fasudil administration specifically attenuates glial cells-mediated neuroinflammation, played a neuroprotective and anti-inflammatory role by up-regulating the phosphorylation of ERK1/2 and AKT in rats ONC model. In general, these findings provided convincing evidence that fasudil exerts neuroprotective effects through attenuating glial cells-mediated neuroinflammation.
Fasudil, a widely used compound for many preclinical studies, may offer a novel therapeutic option for TON due to its potential neuroprotective and anti-inflammatory properties [4]. Yamamoto et al. revealed that fasudil had a concentration-dependent neuroprotective effect against ROCK activation in retina after ONC by inhibiting RGC apoptosis [67]. Moreover, fasudil could ameliorates damage of the optic nerve through Rho/ROCK signaling pathway, suggesting that fasudil is efficacious for the treatment of ONC injury [7, 35, 36]. Our results displayed that the fasudil treated group had significantly more viable RGCs after ONC as compared to the untreated group, suggesting that fasudil could resist the apoptosis of RGCs after ONC.
The effector caspases become activated through cleavage by initiator caspases, and lead to RGCs apoptosis after ONC [5, 25]. Fasudil suppressed inflammation-induced caspase activation that ultimately inhibited apoptosis [77]. Increasing evidence suggested that the activations of caspase-3 and caspase-9 pathways were up-regulated after RGCs injury [5, 78,79,80,81], while the inhibition of cleaved caspase of 3 and 9 significantly enhances RGCs survival rate [5, 82, 83]. Furthermore, fasudil was able to inhibit caspase-3 activation and protect optic nerve [7]. Our findings are in line with prior studies that fasudil treatment significantly inhibited RGCs apoptosis related proteins expression after ONC.
Retinal glial cells were verified as the critical cells in the neuroinflammatory processes of TON, which were cause optic nerve inflammation and contributed to RGCs apoptosis when they were activated [53, 84, 85]. Therefore, inhibiting the activation of retinal glial cells that further reduce optic nerve inflammation may provide a suitable and effective treatment for ONC. Activated retinal glial cells may upregulate the expression of GFAP and iba-1 and promotes the release of proinflammatory cytokines, thus resulting in neuroinflammation. Prior research have documented that fasudil can inhibit the conversion of retinal glial cells from M2 to M1 [51, 52, 86, 87]). In the hippocampus of the cigarette smoke-exposed mice model, chronic fasudil administration suppressed the overproduction of cytokines (IL-1β, IL-6 and TNF-α) and lessened the inflammatory impairments [88]. Our study detected that fasudil significantly inhibited the activation of retinal glial cells, which were manifested by decreased the expression of GFAP and iba-1. Moreover, fasudil inhibited the mRNA expression of proinflammatory factors after ONC. Thus, we speculate that the anti-apoptosis mechanism of fasudil might be associated with the inhibition of glial cell-mediated neuroinflammation.
Recently, ERK1/2 and AKT pathways have been demonstrated to protect against cell apoptosis, and some agents exert neuroprotective effects by activating ERK1/2 signaling pathways in the retina [89, 90]. Moreover, overexpression of MEK1 mutants resulted in a conspicuous increase in p-ERK1/2 levels further attenuated neuroinflammation and improve RGCs survival after optic nerve injury [91]. The activation of AKT and ERK1/2 can lead to phosphorylation of pro-apoptotic BAD (thus inactivation) and activation of anti-apoptotic Bcl-2 protein, which may work together to improve RGCs survival [44, 92]. Notably, fasudil attenuate neuroinflammation and prevent the nerve from damage via ERK1/2 and AKT pathways. All the results above were consistent with our founding.
In summary, we reveal that the number of RGCs were significantly decreased, retinal glial cells were activated, which was accompanied by slight elevation (no statistical significance) in the phosphorylation of AKT and ERK1/2 in the retina after ONC. However, fasudil treatment significantly attenuated glial cell-mediated neuroinflammation and further enhanced RGCs survival by a concomitant increase in p-ERK1/2 expression along with p-AKT expression in the rats ONC model. Hence, these findings may promote the useful application of fasudil in the treatment of TON.
References
Chen M, Jiang Y, Zhang J, Li N (2018) Clinical treatment of traumatic optic neuropathy in children: summary of 29 cases. Exp Ther Med 16:3562–3566. https://doi.org/10.3892/etm.2018.6637
Kashkouli MB, Yousefi S, Nojomi M, Sanjari MS, Pakdel F, Entezari M, Etezad-Razavi M, Razeghinejad MR, Esmaeli M, Shafiee M, Bagheri M (2018) Traumatic optic neuropathy treatment trial (TONTT): open label, phase 3, multicenter, semi-experimental trial. Graefes Arch Clin Exp Ophthalmol 256:209–218. https://doi.org/10.1007/s00417-017-3816-5
Lee WJ, Hong EH, Park HM, Lim HW (2019) Traumatic optic neuropathy-associated progressive thinning of the retinal nerve fiber layer and ganglion cell complex: two case reports. BMC Ophthalmol 19:216. https://doi.org/10.1186/s12886-019-1232-9
Yu J, Lan S, Wang R, Maier A (2015) Fasudil alleviates traumatic optic neuropathy by inhibiting Rho signaling pathway. Int J Clin Exp Med 8:13377–13382
Yu J, Lin L, Luan X, Jing X et al (2015) Impacts of Rho kinase inhibitor Fasudil on Rho/ROCK signaling pathway in rabbits with optic nerve injury. Int J Clin Exp Pathol 8:14717–14724
Yu J, Lan S, Wang R, Maier A, Luan X (2015) Fasudil alleviates traumatic optic neuropathy by inhibiting Rho signaling pathway. Int J Clin Exp Med 8:13377–13382
Yu J, Luan X, Lan S, Yan B, Maier A (2016) Fasudil, a rho-associated protein kinase inhibitor, attenuates traumatic retinal nerve injury in rabbits. J Mol Neurosci 58:74–82. https://doi.org/10.1007/s12031-015-0691-6
Rovere G, Nadal-Nicolas FM, Sobrado-Calvo P, Garcia-Bernal D, Villegas-Perez MP, Vidal-Sanz M, Agudo-Barriuso M (2016) Topical treatment with bromfenac reduces retinal gliosis and inflammation after optic nerve crush. Invest Ophthalmol Vis Sci 57:6098–6106. https://doi.org/10.1167/iovs.16-20425
Bond WS, Rex TS (2014) Evidence that erythropoietin modulates neuroinflammation through differential action on neurons, astrocytes, and microglia. Front Immunol 5:523. https://doi.org/10.3389/fimmu.2014.00523
Cueva Vargas JL, Belforte N, Di Polo A (2016) The glial cell modulator ibudilast attenuates neuroinflammation and enhances retinal ganglion cell viability in glaucoma through protein kinase A signaling. Neurobiol Dis 93:156–171. https://doi.org/10.1016/j.nbd.2016.05.002
Jia Y, Jiang S, Chen C, Lu G, Xie Y, Sun X, Huang L (2019) Caffeic acid phenethyl ester attenuates nuclear factor kappaB mediated inflammatory responses in Muller cells and protects against retinal ganglion cell death. Mol Med Rep 19:4863–4871. https://doi.org/10.3892/mmr.2019.10151
Mac Nair CE, Schlamp CL, Montgomery AD, Shestopalov VI, Nickells RW (2016) Retinal glial responses to optic nerve crush are attenuated in Bax-deficient mice and modulated by purinergic signaling pathways. J Neuroinflamm 13:93. https://doi.org/10.1186/s12974-016-0558-y
Adornetto A, Russo R, Parisi V (2019) Neuroinflammation as a target for glaucoma therapy. Neural Regen Res 14:391–394. https://doi.org/10.4103/1673-5374.245465
Welser-Alves JV, Milner R (2013) Microglia are the major source of TNF-alpha and TGF-beta1 in postnatal glial cultures; regulation by cytokines, lipopolysaccharide, and vitronectin. Neurochem Int 63:47–53. https://doi.org/10.1016/j.neuint.2013.04.007
He D, Huang B, Fu S, Li Y, Ran X, Liu Y, Chen G, Liu J, Liu D (2018) Tubeimoside I protects dopaminergic neurons against inflammation-mediated damage in lipopolysaccharide (LPS)-evoked model of Parkinson’s disease in rats. Int J Mol Sci 19:2242. https://doi.org/10.3390/ijms19082242
Lakhan SE, Kirchgessner A, Hofer M (2009) Inflammatory mechanisms in ischemic stroke: therapeutic approaches. J Transl Med 7:97. https://doi.org/10.1186/1479-5876-7-97
Wu N, Yu J, Chen S, Xu J, Ying X, Ye M, Li Y, Wang Y (2014) αCrystallin protects RGC survivaland inhibits microglial activation after optic nerve crush. Life Sci 94:17–23. https://doi.org/10.1016/j.lfs.2013.10.034
McGeer PL, McGeer EG (1995) The inflammatory response system of brain: implications for therapy of Alzheimer and other neurodegenerative diseases. Brain Res Brain Res Rev 21:195–218. https://doi.org/10.1016/0165-0173(95)00011-9
Tsai RK, Chang CH, Wang HZ (2008) Neuroprotective effects of recombinant human granulocyte colony-stimulating factor (G-CSF) in neurodegeneration after optic nerve crush in rats. Exp Eye Res 87:242–250. https://doi.org/10.1016/j.exer.2008.06.004
Levkovitch-Verbin H, Waserzoog Y, Vander S, Makarovsky D, Piven I (2014) Minocycline upregulates pro-survival genes and downregulates pro-apoptotic genes in experimental glaucoma. Graefes Arch Clin Exp Ophthalmol 252:761–772. https://doi.org/10.1007/s00417-014-2588-4
Yang X, Hondur G, Tezel G (2016) Antioxidant treatment limits neuroinflammation in experimental glaucoma. Investig Opthalmol Vis Sci. https://doi.org/10.1167/iovs.16-19153
Xu P, Huang MW, Xiao CX, Long F, Wang Y, Liu SY, Jia WW, Wu WJ, Yang D, Hu JF, Liu XH, Zhu YZ (2017) Matairesinol suppresses neuroinflammation and migration associated with Src and ERK1/2-NF-kappaB pathway in activating BV2 microglia. Neurochem Res 42:2850–2860. https://doi.org/10.1007/s11064-017-2301-1
Fujita Y, Sato A, Yamashita T (2013) Brimonidine promotes axon growth after optic nerve injury through Erk phosphorylation. Cell Death Dis 4:e763. https://doi.org/10.1038/cddis.2013.298
Kaplan DR, Miller FD (2000) Neurotrophin signal transduction in the nervous system. Curr Opin Neurobiol 10:381–391. https://doi.org/10.1016/s0959-4388(00)00092-1
Kermer P, Klöcker N, Labes M, Bähr M (2000) Insulin-like growth factor-I protects axotomized rat retinal ganglion cells from secondary death via PI3-K-dependent Akt phosphorylation and inhibition of caspase-3 In vivo. J Neurosci 20:2–8
Li DJ, Li YH, Yuan HB, Qu LF, Wang P (2017) The novel exercise-induced hormone irisin protects against neuronal injury via activation of the Akt and ERK1/2 signaling pathways and contributes to the neuroprotection of physical exercise in cerebral ischemia. Metabolism 68:31–42. https://doi.org/10.1016/j.metabol.2016.12.003
Pernet V, Joly S, Jordi N, Dalkara D, Guzik-Kornacka A, Flannery JG, Schwab ME (2013) Misguidance and modulation of axonal regeneration by Stat3 and Rho/ROCK signaling in the transparent optic nerve. Cell Death Dis 4:e734. https://doi.org/10.1038/cddis.2013.266
Kwon JH, Gaire BP, Park SJ, Shin DY, Choi JW (2018) Identifying lysophosphatidic acid receptor subtype 1 (LPA1) as a novel factor to modulate microglial activation and their TNF-alpha production by activating ERK1/2. Biochim Biophys Acta Mol Cell Biol Lipids 1863:1237–1245. https://doi.org/10.1016/j.bbalip.2018.07.015
Gaire BP, Song MR, Choi JW (2018) Sphingosine 1-phosphate receptor subtype 3 (S1P3) contributes to brain injury after transient focal cerebral ischemia via modulating microglial activation and their M1 polarization. J Neuroinflamm 15:284. https://doi.org/10.1186/s12974-018-1323-1
Huang C, Lu X, Wang JL, Tong LJ, Ling Y, Jiang B, Yang RR, Zhang W (2016) Compound C induces the ramification of murine microglia in an AMPK-independent and small rhogtpase-dependent manner. Neuroscience 331:24–39. https://doi.org/10.1016/j.neuroscience.2016.06.018
Chang YC, Lin CY, Hsu CM, Lin HC, Chen YH, Lee-Chen GJ, Su MT, Ro LS, Chen CM, Hsieh-Li HM (2011) Neuroprotective effects of granulocyte-colony stimulating factor in a novel transgenic mouse model of SCA17. J Neurochem 118:288–303. https://doi.org/10.1111/j.1471-4159.2011.07304
Tsai RK, Chang CH, Sheu MM, Huang ZL (2010) Anti-apoptotic effects of human granulocyte colony-stimulating factor (G-CSF) on retinal ganglion cells after optic nerve crush are PI3K/AKT-dependent. Exp Eye Res 90:537–545. https://doi.org/10.1016/j.exer.2010.01.004
Hara M, Takayasu M, Watanabe K, Noda A, Takagi T, Suzuki Y, Yoshida J (2000) Protein kinase inhibition by fasudil hydrochloride promotes neurological recovery after spinal cord injury in rats. J Neurosurg 93:94–101
Shintani N, Ishiyama T, Kotoda M, Asano N, Sessler DI, Matsukawa T (2017) The effects of Y-27632 on pial microvessels during global brain ischemia and reperfusion in rabbits. BMC Anesthesiol 17:38. https://doi.org/10.1186/s12871-017-0331-5
Wu J, Li J, Hu H, Liu P, Fang Y, Wu D (2012) Rho-kinase inhibitor, fasudil, prevents neuronal apoptosis via the Akt activation and PTEN inactivation in the ischemic penumbra of rat brain. Cell Mol Neurobiol 32:1187–1197. https://doi.org/10.1007/s10571-012-9845-z
Chen M, Liu A, Ouyang Y, Huang Y, Chao X, Pi R (2013) Fasudil and its analogs: a new powerful weapon in the long war against central nervous system disorders? Expert Opin Investig Drugs 22:537–550. https://doi.org/10.1517/13543784.2013.778242
Ruan H, Zhang Y, Liu R, Yang X (2019) The acute effects of 30 mg vs 60 mg of intravenous Fasudil on patients with congenital heart defects and severe pulmonary arterial hypertension. Congenit Heart Dis 14:645–650. https://doi.org/10.1111/chd.12764
Zhang Y, Wu S (2017) Effects of fasudil on pulmonary hypertension in clinical practice. Pulm Pharmacol Ther 46:54–63. https://doi.org/10.1016/j.pupt.2017.08.002
Masumoto A, Mohri M, Shimokawa H, Urakami L, Usui M, Takeshita A (2002) Suppression of coronary artery spasm by the rho-kinase inhibitor fasudil in patients with V asospastic angina. Circulation 105:1545–1547. https://doi.org/10.1161/hc1302.105938
Zhao J, Zhou D, Guo J, Ren Z, Zhou L, Wang S, Xu B, Wang R (2006) Effect of fasudil hydrochloride, a protein kinase inhibitor, on cerebral vasospasm and delayed cerebral ischemic symptoms after aneurysmal subarachnoid hemorrhage. Neurol Med Chir (Tokyo) 46:421–428
Sugiyama T, Shibata M, Kajiura S, Okuno T, Tonari M, Oku H, Ikeda T (2011) Effects of fasudil, a Rho-associated protein kinase inhibitor, on optic nerve head blood flow in rabbits. Invest Ophthalmol Vis Sci 52:64–69. https://doi.org/10.1167/iovs.10-5265
Li Q, Huang XJ, He W, Ding J, Jia JT, Fu G, Wang HX, Guo LJ (2009) Neuroprotective potential of fasudil mesylate in brain ischemia-reperfusion injury of rats. Cell Mol Neurobiol 29:169–180. https://doi.org/10.1007/s10571-008-9308-8
Ichikawa M, Yoshida J, Saito K, Sagawa H, Tokita Y, Watanabe M (2008) Differential effects of two ROCK inhibitors, Fasudil and Y-27632, on optic nerve regeneration in adult cats. Brain Res 1201:23–33. https://doi.org/10.1016/j.brainres.2008.01.063
Brunet A, Datta SR, Greenberg ME (2011) Transcription-dependent and -independent control of neuronal survival by the PI3K-Akt signaling pathway. Curr Opin Neurobiol 11:297–305
Ahmed LA, Darwish HA, Abdelsalam RM, Amin HA (2016) Role of rho kinase inhibition in the protective effect of fasudil and simvastatin against 3-nitropropionic acid-induced striatal neurodegeneration and mitochondrial dysfunction in rats. Mol Neurobiol 53:3927–3938. https://doi.org/10.1007/s12035-015-9303-2
Fu PC, Tang RH, Yu ZY, Xie MJ, Wang W, Luo X (2018) The Rho-associated kinase inhibitors Y27632 and fasudil promote microglial migration in the spinal cord via the ERK signaling pathway. Neural Regen Res 13:677–683. https://doi.org/10.4103/1673-5374.230294
Takata M, Tanaka H, Kimura M, Nagahara Y, Tanaka K, Kawasaki K, Seto M, Tsuruma K, Shimazawa M, Hara H (2013) Fasudil, a rho kinase inhibitor, limits motor neuron loss in experimental models of amyotrophic lateral sclerosis. Br J Pharmacol 170:341–351. https://doi.org/10.1111/bph.12277
Tönges L, Frank T, Tatenhorst L, Saal KA, Koch JC, Szego EM, Bahr M, Weishaupt JH, Lingor P (2012) Inhibition of rho kinase enhances survival of dopaminergic neurons and attenuates axonal loss in a mouse model of Parkinson’s disease. Brain 135:3355–3370. https://doi.org/10.1093/brain/aws254
Wu N, Li W, Shu W, Lv Y, Jia D (2014) Inhibition of Rho-kinase by fasudil restores the cardioprotection of ischemic postconditioninng in hypercholesterolemic rat heart. Mol Med Rep 10:2517–2524. https://doi.org/10.3892/mmr.2014.2566
Wu Y, Xu F, Huang H, Chen L, Wen M, Jiang L, Lu L, Li L, Song D, Zeng S, Li L, Li M (2014) Up-regulation of SKIP relates to retinal ganglion cells apoptosis after optic nerve crush in vivo. J Mol Histol 45:715–721. https://doi.org/10.1007/s10735-014-9589-9
He Q, Li YH, Guo SS, Wang Y, Lin W, Zhang Q, Wang J, Ma CG, Xiao BG (2016) Inhibition of Rho-kinase by Fasudil protects dopamine neurons and attenuates inflammatory response in an intranasal lipopolysaccharide-mediated Parkinson’s model. Eur J Neurosci 43:41–52
Zhang H, Li Y, Yu J, Guo M, Meng J, Liu C, Xie Y, Feng L, Xiao B, Ma C (2013) Rho kinase inhibitor fasudil regulates microglia polarization and function. Neuroimmunomodulation 20:313–322. https://doi.org/10.1159/000351221
Huang R, Lan Q, Chen L, Zhong H, Cui L, Jiang L, Huang H, Li L, Zeng S, Li M, Zhao X, Xu F (2018) CD200Fc attenuates retinal glial responses and RGCs apoptosis after optic nerve crush by modulating CD200/CD200R1 interaction. J Mol Neurosci 64:200–210. https://doi.org/10.1007/s12031-017-1020-z
Tang Z, Zhang S, Lee C, Kumar A, Arjunan P, Li Y, Zhang F, Li X (2011) An optic nerve crush injury murine model to study retinal ganglion cell survival. J Vis Exp. https://doi.org/10.3791/2685
Xu F, Huang H, Wu Y, Lu L, Jiang L, Chen L, Zeng S, Li L, Li M (2014) Upregulation of Gem relates to retinal ganglion cells apoptosis after optic nerve crush in adult rats. J Mol Histol 45:565–571. https://doi.org/10.1007/s10735-014-9579-y
Xu Y, Yang B, Hu Y, Lu L, Lu X, Wang J, Xu F, Yu S, Huang J (2016) Wogonin prevents TLR4-NF-κB-medicated neuro-inflammation and improves retinal ganglion cells survival in retina after optic nerve crush. Oncotarget 7:72503–72517
Berkelaar M, Clarke DB, Wang YC, Bray GM, Aguayo AJ (1994) Axotomy results in delayed death and apoptosis of retinal ganglion cells in adult rats. J Neurosci 14:4368–4374
Wang J, Chen S, Zhang X, Huang W, Jonas JB (2016) Intravitreal triamcinolone acetonide, retinal microglia and retinal ganglion cell apoptosis in the optic nerve crush model. Acta Ophthalmol 94:e305-311. https://doi.org/10.1111/aos.12698
Wang R, Sun Q, Xia F, Chen Z, Wu J, Zhang Y, Xu J, Liu L (2017) Methane rescues retinal ganglion cells and limits retinal mitochondrial dysfunction following optic nerve crush. Exp Eye Res 159:49–57. https://doi.org/10.1016/j.exer.2017.03.008
Wang R, Xu J, Xie J, Kang Z, Sun X, Chen N, Liu L, Xu J (2010) Hyperbaric oxygen preconditioning promotes survival of retinal ganglion cells in a rat model of optic nerve crush. J Neurotrauma 27:763–770
Zhong H, Cui L, Xu F, Chen L, Jiang L, Huang H, Xu J, Zhao X, Li L, Zeng S, Li M (2016) Up-regulation of Wip1 involves in neuroinflammation of retinal astrocytes after optic nerve crush via NF-kappaB signaling pathway. Inflamm Res 65:709–715. https://doi.org/10.1007/s00011-016-0952-z
Brockmann C, Corkhill C, Jaroslawska E, Dege S, Brockmann T, Kociok N, Joussen AM (2019) Systemic Rho-kinase inhibition using fasudil in mice with oxygen-induced retinopathy. Graefes Arch Clin Exp Ophthalmol 257:1699–1708. https://doi.org/10.1007/s00417-019-04365-4
Zhu WW, Ma XL, Guo AL, Zhao HY, Luo HH (2011) Neuroprotective effects of NEP1-40 and fasudil on Nogo-A expression in neonatal rats with hypoxic-ischemic brain damage. Genet Mol Res 10:2987–2995. https://doi.org/10.4238/2011.November.29.9
Huang TL, Huang SP, Chang CH, Lin KH, Sheu MM, Tsai RK (2014) Factors influencing the retrograde labeling of retinal ganglion cells with fluorogold in an animal optic nerve crush model. Ophthalmic Res 51:173–178. https://doi.org/10.1159/000357736
Koeberle PD, Ball AK (2002) Neurturin enhances the survival of axotomized retinal ganglion cells in vivo: combined effects with glial cell line-derived neurotrophic factor and brain-derived neurotrophic factor. Neuroscience 110:555–567
Tsuda S, Tanaka Y, Kunikata H, Yokoyama Y, Yasuda M, Ito A, Nakazawa T (2016) Real-time imaging of RGC death with a cell-impermeable nucleic acid dyeing compound after optic nerve crush in a murine model. Exp Eye Res 146:179–188. https://doi.org/10.1016/j.exer.2016.03.017
Yamamoto K, Maruyama K, Himori N, Omodaka K, Yokoyama Y, Shiga Y, Morin R, Nakazawa T (2014) The novel Rho kinase (ROCK) inhibitor K-115: a new candidate drug for neuroprotective treatment in glaucoma. Invest Ophthalmol Vis Sci 55:7126–7136. https://doi.org/10.1167/iovs.13-13842
Zhang ZZ, Gong YY, Shi YH, Zhang W, Qin XH, Wu XW (2012) V alproate promotes survival of retinal ganglion cells in a rat model of optic nerve crush. Neuroscience 224:282–293. https://doi.org/10.1016/j.neuroscience.2012.07.056
Ma K, Xu L, Zhang H, Zhang S, Pu M, Jonas JB (2009) Effect of brimonidine on retinal ganglion cell survival in an optic nerve crush model. Am J Ophthalmol 147:326–331. https://doi.org/10.1016/j.ajo.2008.08.005
Zhang R, Zhang H, Xu L, Ma K, Wallrapp C, Jonas JB (2011) Neuroprotective effect of intravitreal cell-based glucagon-like peptide-1 production in the optic nerve crush model. Acta Ophthalmol 89:e320–e326. https://doi.org/10.1111/j.1755-3768.2010.02044
Cui L, He WJ, Xu F, Jiang L, Lv ML, Huang H, Xu JP, Wu Y, Zhong HB, Zhang SY, Chen LF, Shen CL, Yao G, Li L, Li M, Zeng SM (2016) Alterations in the expression of Hs1-associated protein X-1 in the rat retina after optic nerve crush. Mol Med Rep 14:4761–4766. https://doi.org/10.3892/mmr.2016.5824
Jiang L, Xu F, He W, Chen L, Zhong H, Wu Y, Zeng S, Li L, Li M (2016) CD200Fc reduces TLR4-mediated inflammatory responses in LPS-induced rat primary microglial cells via inhibition of the NF-kappaB pathway. Inflamm Res 65:521–532. https://doi.org/10.1007/s00011-016-0932-3
Elmore S (2007) Apoptosis: a review of programmed cell death. Toxicol Pathol 35:495–516. https://doi.org/10.1080/01926230701320337
Song H, Gao D (2011) Fasudil, a Rho-associated protein kinase inhibitor, attenuates retinal ischemia and reperfusion injury in rats. Int J Mol Med 28:193–198
Lu XC, Shear DA, Graham PB, Bridson GW, Uttamsingh V, Chen Z, Leung LY, Tortella FC (2015) Dual therapeutic effects of C-10068, a dextromethorphan derivative, against post-traumatic nonconvulsive seizures and neuroinflammation in a rat model of penetrating ballistic-like brain injury. J Neurotrauma 32:1621–1632. https://doi.org/10.1089/neu.2014.3766
Luo JM, Cen LP, Zhang XM, Chiang SW, Huang Y, Lin D, Fan YM, van Rooijen N, Lam DS, Pang CP, Cui Q (2007) PI3K/akt, JAK/STA T and MEK/ERK pathway inhibition protects retinal ganglion cells via different mechanisms after optic nerve injury. Eur J Neurosci 26:828–842. https://doi.org/10.1111/j.1460-9568.2007.05718.x
Hannan JL, Matsui H, Sopko NA, Liu X, Weyne E, Albersen M, Watson JW, Hoke A, Burnett AL, Bivalacqua TJ (2016) Caspase-3 dependent nitrergic neuronal apoptosis following cavernous nerve injury is mediated via RhoA and ROCK activation in major pelvic ganglion. Sci Rep 6:29416. https://doi.org/10.1038/srep29416
Cheung ZH, Chan YM, Siu FK, Yip HK, Wu W, Leung MC, So KF (2004) Regulation of caspase activation in axotomized retinal ganglion cells. Mol Cell Neurosci 25:383–393. https://doi.org/10.1016/j.mcn.2003.11.001
Kermer P, Ankerhold R, Klöcker N, Krajewski S, Reed JC, Bähr M (2000) Caspase-9: involvement in secondary death of axotomized rat retinal ganglion cells in vivo. Brain Res Mol Brain Res 85:144–150
Kermer P, Klöcker N, Labes M, Thomsen S, Srinivasan A, Bähr M (1999) Activation of caspase-3 in axotomized rat retinal ganglion cells in vivo. FEBS Lett 453:361–364
Ye D, Shi Y, Xu Y, Huang J (2019) PACAP attenuates optic nerve crush-induced retinal ganglion cell apoptosis via activation of the CREB-Bcl-2 pathway. J Mol Neurosci 68:475–484. https://doi.org/10.1007/s12031-019-01309-9
Kermer P, Klöcker N, Labes M, Bähr M (1998) Inhibition of CPP32-like proteases rescues axotomized retinal ganglion cells from secondary cell death in vivo. J Neurosci 18:4656–4662
Liu Y, Yan H, Chen S, Sabel BA (2015) Caspase-3 inhibitor Z-DEVD-FMK enhances retinal ganglion cell survival and vision restoration after rabbit traumatic optic nerve injury. Restor Neurol Neurosci 33:205–220. https://doi.org/10.3233/RNN-159001
Lu YB, Pannicke T, Wei EQ, Bringmann A, Wiedemann P, Habermann G, Buse E, Käs JA, Reichenbach A (2013) Biomechanical properties of retinal glial cells: comparative and developmental data. Exp Eye Res 113:60–65. https://doi.org/10.1016/j.exer.2013.05.012
Rosen AM, Stevens B (2010) The role of the classical complement cascade in synapse loss during development and glaucoma. Adv Exp Med Biol 703:75–93. https://doi.org/10.1007/978-1-4419-5635-4_6
Geissmann F, Auffray C, Palframan R, Wirrig C, Ciocca A, Campisi L, Narni-Mancinelli E, Lauvau G (2008) Blood monocytes: distinct subsets, how they relate to dendritic cells, and their possible roles in the regulation of T-cell responses. Immunol Cell Biol 86:398–408. https://doi.org/10.1038/icb.2008.19
Zhao Y, Zhang Q, Xi J, Xiao B, Li Y, Ma C (2015) Neuroprotective effect of fasudil on inflammation through PI3K/Akt and Wnt/beta-catenin dependent pathways in a mice model of Parkinson’s disease. Int J Clin Exp Pathol 8:2354–2364
Xueyang D, Zhanqiang M, Chunhua M, Kun H (2016) Fasudil, an inhibitor of Rho-associated coiled-coil kinase, improves cognitive impairments induced by smoke exposure. Oncotarget 7:78764–78772
Johnson K, D’Mello SR (2005) p21-Activated kinase-1 is necessary for depolarization-mediated neuronal survival. J Neurosci Res 79:809–815. https://doi.org/10.1002/jnr.20415
Marra C, Gomes Moret D, de Souza CA, Chagas da Silva F, Moraes P, Linden R, Sholl-Franco A (2011) Protein kinases JAK and ERK mediate protective effect of interleukin-2 upon ganglion cells of the developing rat retina. J Neuroimmunol 233:120–126. https://doi.org/10.1016/j.jneuroim.2010.12.008
Pernet V, Hauswirth WW, Di Polo A (2005) Extracellular signal-regulated kinase 1/2 mediates survival, but not axon regeneration, of adult injured central nervous system neurons in vivo. J Neurochem 93:72–83. https://doi.org/10.1111/j.1471-4159.2005.03002.x
Alonzi T, Middleton G, Wyatt S, Buchman V, Betz UAK, Müller W, Musiani P, Poli V, Davies AM (2001) Role of STA T3 and PI 3-kinase/Akt in mediating the survival actions of cytokines on sensory neurons. Mol Cell Neurosci 18:270–282. https://doi.org/10.1006/mcne.2001.1018
Acknowledgements
Chinese government provided financial support in the form of the National Natural Science Foundation of China (Grant Nos. 81560166, 81460087, 81660168, 81660161, 8176040227 and 81760172) and the Natural Science Foundation of Guangxi Zhuang Autonomous Region (Grant Nos. 2018GXNSFAA281128 and 2018GXNSFBA281066).
Funding
This study was supported by the National Natural Science Foundation of China (No. 81660161, 81560166, 81460087, 81660168, 8176040227 and 81760172), and the Natural Science Foundation of Guangxi Zhuang Autonomous Region (No. 2018GXNSFAA281128 and No. 2018GXNSFBA281066) and Guangxi clinical ophthalmic research center (No. AD19245193).
Author information
Authors and Affiliations
Contributions
QL, LJ and FX conceived and designed the experiments. ZM, BH, NL and MZ performed the establishment of model and the intraperitoneal injection. The retrograde labeling of RGCs with FluoroGold was performed by WH, HH and JL. WH, LJ and WY performed the western blot analysis and immunofluorescence staining experiments. FT, CS and JL performed the qPCR. WH, QL, LJ, FT analyzed and interpreted the data. WH, QL, LJ, and LC edited the paper. HZ, SZ, ML, LC and FX read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, W., Lan, Q., Jiang, L. et al. Fasudil attenuates glial cell-mediated neuroinflammation via ERK1/2 and AKT signaling pathways after optic nerve crush. Mol Biol Rep 47, 8963–8973 (2020). https://doi.org/10.1007/s11033-020-05953-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-020-05953-y