Abstract
Autism spectrum disorder (ASD) is a mosaic of neurodevelopmental conditions composed of early-onset social interaction and communication deficits, along with repetitive and/or restricted patterns of activities, behavior, and interests. ASD affects around 1% of children worldwide, with a male predominance. Energy, porphyrin, and neurotransmitter homeostasis are the key metabolic pathways affected by heavy metal exposure, potentially implicated in the pathogenesis of ASD. Exposure to heavy metals can lead to an altered porphyrin metabolism due to enzyme inhibition by heavy metals. Heavy metal exposure, inborn genetic susceptibility, and abnormal thiol and selenol metabolism may play a significant role in the urinary porphyrin profile anomalies observed in ASD. Altered porphyrin metabolism in ASD may also be associated with, vitamin B6 deficiency, hyperoxalemia, hyperhomocysteinemia, and hypomagnesemia. The present review considers the abnormal porphyrin metabolism in ASD in relation to the potential pathogenic mechanism and discusses the possible metabolic therapies such as vitamins, minerals, cofactors, and antioxidants that need to be explored in future research. Such targeted therapeutic therapies would bring about favorable outcomes such as improvements in core and co-occurring symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autism spectrum disorder (ASD) is a mosaic of neurodevelopmental disorder composed of early-onset deficits of social interaction and communication, as well as repetitive and/or restricted patterns of activities, behavior, and interests associated with a number of genetic and environmental risk factors [1]. It is a spectrum disorder with significant heterogeneity in nature, severity, and progression of core symptoms, cognitive development, language abilities, and other co-occurring problems [2]. According to recent consensus, ASD affects around 1% of children worldwide, with males having a higher prevalence [3,4,5]. Furthermore, as stated by Zeidan et al., ASD prevalence has expanded over time, varying substantially across different socio-demographics [3]. According to the latest estimates in 2020 from Autism and Developmental Disabilities Monitoring (ADDM) Network, about 1 in 36 children in the USA are identified with ASD, which is a significant increase compared to the estimates of 1 in 150 chidren in 2000.
With no reliable molecular biomarkers to guide the diagnosis, ASD is diagnosed based on clinical criteria defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [6]. The DSM-5 recognizes that ASD can coexist with other disorders [6], including sleep disorders [7,8,9]; epilepsy [10]; other neurodevelopmental, mental, or behavioral disorders [1]; inherited metabolic disorders [11]; and other genetic syndromes [12, 13]. Accordingly, the etiology of ASD is multifactorial and involves a spectrum of genetic, epigenetic, and environmental factors [14]. Moreover, a plethora of research on molecular biomarker studies exploring genetics, metabolic biomarkers, autoantibodies, and cytokine profile in ASD has shown that the symptoms are associated with several dysfunctions including intestinal dysbiosis [15], immune and metabolic abnormalities, mitochondrial dysfunction, environmental toxicant exposures, and oxidative stress [16]. Interplay in these dysfunctions may lead toabnormalties in early brain development with altered brain connectivity, exaggerated synaptic pruning, imbalance of excitatory and inhibitory neurotransmitters, and other neuronal-level abnormalities leading to ASD [17].
The key metabolic pathways potentially implicated in the pathogenesis of ASD include energy [18, 19], amino acid [20, 21], serotonin [22], dopamine [23], one-carbon [24,25,26], purine [27], and porphyrin metabolism [28,29,30,31]. Porphyrins are a group of naturally occurring compounds with great importance in the metabolic processes of many organisms including humans. Various porphyrin derivatives are biosynthesized from δ-aminolevulinic acid and glycine during human haem biosynthesis. The core structure of porphyrin is called porphine, and different substitutions on the porphine ring result in porphyrin derivatives such as uroporphyrin, coproporphyrin, and protoporphyrin [32]. Defects in the haem biosynthetic pathway due to genetic and/or environmental factors lead to the accumulation of metabolic intermediates and abnormal porphyrin excretion (porphyrinuria) [33].
Porphyrinuria in ASD has often been attributed to heavy metal toxicity [34,35,36,37,38,39,40]. However, the heterogeneity of the underlying factors involved in ASD has prompted researchers to reconsider their attempts to comprehend the neurochemical changes underlying ASD, including porphyrin metabolism. Therefore, it may be anecdotal to attribute abnormal porphyrin excretion profile to heavy metal toxicity alone. The novel research findings concerning neurochemical abnormalities in autism etiology propose possible other pathogenic mechanisms with implications on alternative diagnostic and therapeutic approaches that could enhance the quality of ASD interventions. The present review considers the abnormal porphyrin metabolism in ASD in relation to plausible alternative biochemical mechanisms and discusses the possible therapeutic implications.
Porphyrin Metabolites in ASD Subjects
Urinary porphyrin levels in ASD have been explored by several study groups. However, most of them were conducted by a few research teams in the USA [28, 29, 31, 36,37,38, 41, 42], while the rest were conducted in Australia [43, 44], France [41], South Korea [45], Egypt [34] Slovenia [35], and Armenia [46].
Evaluation of any urinary metabolite requires normalization to a ubiquitous urinary metabolite such as creatinine. Although it was once hypothesized a possible correlation between ASD and depressed urinary creatinine levels by Whiteley et al., 2 years later, Nataf et al. concluded their study on porphyrinuria in childhood ASD, refuting the former finding further stating that urinary porphyrin levels were elevated in ASD individuals when normalized to creatinine [30].
When normalized to creatinine, copropophyrin levels [29, 31, 34, 36, 41], precoproporphyrin [31, 34, 36, 41, 45], pentacarboxyporphyrin [29, 31, 34, 41, 45], and hexacarboxyporphyrin [31, 34, 41] levels have been found to be higher in ASD group compaired to controls, while heptacarboxyporphyrin and uroporphyrin have been reported to be higher in ASD group only in a single study [34]. It is important to note that even when the reported differences of specific porphyrins are not statistically significant, the trend was towards higher levels in ASD compared to controls.
Uroporphyrin levels have not been reported to be significantly different from the controls except in a single study [34] and considered a marker independent of environmental toxicity [41]. Therefore, several study groups have used specific porphyrin to uroporphyrin ratios to eliminate the effects of variations in urinary volume. Coproporphyrin/uroporphyrin ratio and precoproporphyrin/uroporphyrin ratio have been reported to be higher in ASD group [37, 41]. Studies reporting specific porphyrin levels normalized to creatinine and uroporphyrin levels are summarized in Table 1.
Geier et al. and Khaled et al. also compared porphyrin levels between subjects with ASD and controls without normalizing to creatinine in several publications [28, 34, 37, 38]. However, there findings also showed increased pentacarboxyporphyrin and coproporphyrin levels in children with ASD.
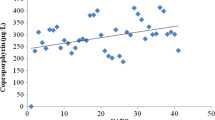
Woods et al. reported that higher porphyrin concentrations were found in young children, particularly uro-, hepta-, and coproporphyrins, although their concentrations were observed to decline with age, possibly due to age-related differences in haem biosynthesis [31]. This indicates that in analyzing the differences of porphyrin levels between cases and controls, the moderating effects of age should be controlled by using such statistical models as ANCOVA.
Urinary Porphyrin as a Potential Biomarker of Heavy Metal Exposure
Many researchers have investigated the correlation between ASD, abnormal urinary porphyrin profile, and the possible causal impact of heavy metals on the correlation [41, 47, 48]. For instance, Nataf et al. demostrated that average elevation of coproporphyrin levels in autistic disorder was comparable to the elevation observed in subjects with significant arsenic (As) and mercury (Hg) exposure [41]. This speculation is further strengthened by demonstrating a reduction in urinary porphyrins following the treatment of ASD children or rats exposed to methylmercury hydroxide, with dimercaptosuccinic acid (DMSA/succimer), a heavy metal chelator [30, 37, 39, 49, 50].
Many study groups proposed that the abnormally high porphyrin levels in subjects with ASD could be due to Hg toxicity. For instance, precoproporphyrin, an atypical porphyrin, previously described primarily in animals and humans exposed to Hg or Hg compounds, was found in higher concentrations in the urine of children with ASD [31, 41]. Additionally, the differences in Hg toxicity-associated porphyrin levels from different geographical areas suggest the interplay of variations in the environmental factors and genetic predispositions in detoxification capacity [51].
The biosynthesis of haem begins with delta-aminolevulinic acid (ALA) formation and ends with the insertion of iron into the protoporphyrin IX ring [52]. Exposure to heavy metals such as Pb and Hg can lead to several metabolic disturbances, with heavy metals being known direct or indirect inhibitors of several metabolic pathways in the human body.
The meta-analysis by Zhang et al. revealed higher levels of Hg and Pb in children with ASD compared to controls [53]. Another study demonstrated that following chelation therapy with DMSA, urinary Hg concentrations increased from three to approximately five folds higher in ASD subjects compared to healthy controls, while Pb and cadmium (Cd) levels in urine showed only statistically non-significant increase [54]. Windham et al. suggested a possible association between ASD and estimated environmental exposure of potential neuro- and developmental toxicants near the birth region in their 2006 case-control study, and seven more ecological studies revealed a correlation between environmental Hg and ASD, while another study uncovered a similar association to Pb [55,56,57,58,59,60,61,62,63]. Some studies, however, observed no statistically significant difference in urinary Hg levels or previous Hg exposure as measured by fish consumption, vaccines received, or the number of dental amalgam fillings in subjects with ASD compared to the controls [31]. Furthermore, Adams et al. demonstrated a significantly strong correlation between toxic metal excretion and behavioral measures of ASD [48].
In contrast to Pb and Hg, meta-analysis of zinc (Zn) levels in blood showed significantly lower levels in subjects with ASD compared to neurotypical controls [53, 64]. Atypical porphyrin levels might be a consequence of the imbalance between the level of heavy metal exposure and protective factors such as detoxification capacity and sufficiancy of Zn at least in a subset of ASD individuals. For instance, a young ASD subject with low-level Hg exposure might have relatively higher urine atypical porphyrins in the presence of low detoxification capacity. Furthermore, Zn deficiency may potentiate the toxic effects of heavy metals even at relatively normal levels [65].
The main target in Pb poisoning is delta-aminolevulinic acid dehydratase (ALAD), also known as porphobilinogen synthase (PBGS). The main mechanism of inhibition is the oxidation of sulfhydryl groups located at the active site of ALAD [66]. The lone electron pair on Pb(II) could also sterically interfere with the substrate or product binding to ALAD enzyme [67]. The inhibition of ALAD causes the accumulation of ALA. As cited by Akshatha et al., ALA which is implicated in symptoms of porphyria alters neurotransmitter metabolism, induces mitochondrial dysfunction, inhibits melatonin release, and increases production of reactive oxygen species, which are also relevant in pathogenesis of ASD [68]. Interestingly, there are case reports describing patients with Pb toxicity presenting with clinical features of porphyria and ASD [69].
Coproporphyrinogen III oxidase (CPOX) seems to be the second vulnerable enzyme, catalyzing the two-step decarboxylation of coproporphyrinogen III into protoporphyrinogen IX [52]. Impaired CPOX activity leads to increased coproporphyrin levels in urine. Pb does not exert any direct inhibitory effect by its binding to the active site of the enzyme. As the enzyme is located in the mitochondrial intermembrane space, Pb-induced mitochondrial membrane distortion has been discussed as a potential culprit [70]. However, Hg binding to thiol groups of the CPOX enzyme (e.g., C319 cysteine moiety) could interfere with the structure and directly inhibit the conversion of harderoporphyrinogen to protoporphyrinogen [71].
Uroporphyrin decarboxylase (UROD) is also inhibited by Hg binding to thiol groups. Accordingly, the inhibition can be prevented by the thiols [72]. While Hg and Cd may inhibit ferrochelatase directly, Pb is thought to reduce iron availability for Fe2+ ferrochelatase activity in the cell, leading to Zn protoporphyrin accumulation owing to Zn2+ ferrochelatase activity unopposed by Fe2+ [70].
ALAD gene exhibits polymorphisms due to transversion of the base at position 177, producing two codominant alleles, namely ALAD1 and ALAD2. Consequently, three genotypes are formed by pairs of alleles: ALAD1-1, ALAD1-2, and ALAD2-2. ALAD2 protein binds Pb more tightly to the enzyme than ALAD1 protein due to the substitution of asparagine for lysine at the 59th position, resulting in more effective inactivation of ALAD and elevated Pb concentration in the body [73]. Therefore, it has been hypothesized that ALAD-2 may reduce harmful effects by conferring a protective effect by sequestering circulating Pb, thus preventing toxic effects [74]. However, recent evidence suggests that the ALAD1-2 genotype may be associated with a higher risk of long-term Pb toxicity than the ALAD1-1 genotype. The ALAD1-2 heterozygosity was significantly more common in autistic children than in controls, indicating that children with the ALAD2 variant were approximately 1.67 times more likely to be autistic [75]. Intriguingly, the maternal ALAD2 variant was associated with higher placental Pb levels [76]. The effects of higher placental Pb levels related to the ALAD2 variant on the fetus are yet to be explored.
In human subjects with low-level Hg exposure, a specific variant (A814C) in exon 4 of the human CPOX gene (CPOX4) encoding an N272H substitution is linked with anomalous urinary porphyrin efflux and increased neuro-behavioral deficits. Studies suggest that this variant encodes an enzyme with a lower affinity for coproporphyrinogen-III [71]. This gene product preferentially converts the upstream penta-carboxylporphyrin to ketoisocoproporphyrin. Hg-exposed subjects carrying the CPOX4 variant exhibit increased levels of penta-carboxylporphyrin due to inhibition of the penta- to the tetra-decarboxylation step of UROD, with elevated excretion of tetra-carboxyl porphyrins and atypical ketoisocoproporphyrin [77].
Taken together, characteristic changes in urine porphyrin levels of Hg toxicity include elevated levels of tetra- and penta-carboxylporphyrin and the appearance of an atypical metabolite pre-coproporphyrin [78]. Additionally, in subjects harboring CPOX4, atypical porphyrin ketoisocoproporphyrin is also increased [77]. Pb toxicity can lead to the elevation of urine coproporphyrin [70, 79], erythrocyte Zn protoporphyrin, and urinary ALA without any increase in urine porphobilinogen [80, 81]. Interestingly, blood lead levels have been shown to negatively corelate with low serum Zn levels in school chidren [82].
Can Heavy Metal-Induced Toxicity Explain Sex Differences in Autism Spectrum Disorder?
Meta-analysis of prevalence studies demonstrated a male-to-female ratio close to 3:1 in ASD [83]. A perfect pathogenic model proposed for ASD should be able to explain this male preponderance. This could be explained by the presence of sexual dimorphism in terms of higher body burdens of heavy metals or increased susceptibility to the effects of exposure. In addition, influences of gonadal hormones, epigenetic modifications, and sex chromosome activation may be involved in gender differences in exposure outcomes [84].
Heavy metals appear to exhibit gender-specific effects that could be explained by lesser glutathione availability, lesser sulfate-based detoxification capacity, potentiating effects of testosterone, and greater neuroinflammatory response in males [85]. According to large-scale epidemiological studies, males have greater mean blood Pb levels than females. However, the differences in blood Pb levels are not significant at birth or early in life. Surprisingly, the differences intensified around the age of 12 years, correlating with puberty. Furthermore, males appear to be more susceptible to the impact of prenatal and postnatal Pb exposure. Postnatal and early childhood exposure was associated with attention span and cognitive development with males being more adversely affected with lower cognitive function scores [84, 86].
Evidence supporting potential sexual dimorphism associated with prenatal and early postnatal exposure to Hg is sparse. The results show that sex differences in Hg metabolism are only noticeable at high Hg concentrations. Males seem more prone to deficits in motor functions and cognitive and neurobehavioral performance when exposed to Hg. Unlike Pb, however, most of these studies have been carried out in people exposed to relatively greater levels of Hg. Therefore, it is uncertain if the dimorphism in neurotoxicity persists at lower exposure levels [86]. Furthermore, Hg exposure at the age of nine years was linked to poorer mental agility and worse neurobehavioral development, short-term memory, visual memory processes, and sequential organization in Spanish children. This association has been altered by gender and specific genetic variants in BDNF, APOE, and GSTP1 [87].
Some studies reported evidence supporting the presence of sexual dimorphism in the glutathione system, although most studies indicated the lack of sex-specific differences [88]. A Jamaican study found that ASD patients with GSTP1 Ile105Val genotype Ile/Ile correspond to higher blood Hg concentrations compared to genotype Ile/Val. GSTP1 encodes a glutathione S-transferase enzyme that catalyzes the formation of glutathione conjugates. This finding suggests that defects in GSTP1-mediated detoxification of Hg play a potential role in the pathogenesis of autism [89]. Sexual dimorphism in the glutathione system appears to be affected by several confounding variables, including age and brain region [88].
The Usefulness of Porphyrins as Biomarkers in ASD
Certain porphyrin metabolites appear as candidate biomarkers with relatively low sensitivity but nearly 100% specificity [29]. Moreover, the urine porphyrin levels positively correlated with the severity of autism [28, 42, 44]. For instance, pentacarboxyporphyrin, precoproporphyrin, and coproporphyrin levels are higher in severe cases with ASD compared to mild cases [28, 42]. Correspondingly, subjects with Asperger syndrome, who are usually mildly affected, with better language and cognitive skills did not show significant differences in urine porphyrin levels compared to the control group. Moreover, abnormal porphyrin levels were reported to be significantly higher in chidren with autistic disorder associated with epilepsy [41].
As the name implies, ASD is a spectrum disorder with significant heterogeneity of clinical features and underlying pathogenic mechanisms. This explains why the biomarkers yield less sensitivity and higher specificity. For instance, ASD subjects with a pathogenic mechanism apart from heavy metal toxicity or reduced capacity to detoxify heavy metals may yield negative test results for urine porphyrin assessment. The primary goal of such a test is to accurately identify a subset of individuals with shared pathogenicity, predict prognosis, and attempt metal-type-targeted therapy. Prospective follow-up studies are needed to evaluate the use of urine porphyrin biomarkers to predict prognosis.
Urine porphyrin levels appear to be a good biomarker to monitor response to therapy. The differences in urine porphyrin biomarkers between chelated ASD subjects and non-chelated ASD subjects were statistically significant [37, 38]. Importantly, the test can be performed on an untimed spot urine sample, a convenient, non-invasive sampling strategy. This is particularly beneficial as children with ASD can be hypersensitive to venipuncture procedures. On the other hand, the test is relatively inexpensive.
Shared Pathogenic Mechanisms in Porphyria and ASD
Despite the presence of porphyria in ASD as reported consistently by many study groups, genetic porphyrias co-occurring with ASD have not been common with only a single case report of an ASD patient with acute intermittent porphyria (AIP) reported in the online literature [90]. However, porphyria is a commonly underdiagnosed entity due to non-specific symptoms [68].
There are striking similarities between the symptomatology of porphyria and ASD such as abdominal pain [91, 92], vomiting [91, 92], constipation [91, 92], seizures [10, 91, 93], and behavioral changes [91, 94, 95]. Even more striking are the biochemical similarities; porphyrinuria [31, 33, 34, 44, 45], increased oxidative stress [96, 97], mitochondrial dysfunction [96, 98], hyperhomocysteinemia [99,100,101], functional vitamin B6 deficiency [102,103,104], hyperoxalemia and hyperoxaluria [104, 105], and hypomagnesemia [64, 106]. Both porphyria and ASD exhibit enhanced pyridoxal 5′-phosphate-dependent tryptophan-kynurenine metabolism, probably mediated by substrate availability, at the expense of the tryptophan-serotonin-melatonin pathway [103, 107]. Increased oxidative stress in porphyria is evident by increased malondialdehyde [108] and may be partly produced by increased δ-aminolevulinic acid levels [109]. The presence of mitochondrial dysfunction in porphyria is supported by reduced total cellular ATP levels [110], reduced oxygen consumption rate [96], and reduced expression of mitochondrial respiratory chain proteins [108, 110].
Alanine-glyoxylate aminotransferase (AGT) is a pyridoxal-5′-phosphate-dependent enzyme involved in the metabolism of glyoxylate [111]. Depletion of pyridoxal-5′-phosphate may cause hyperoxalemia and hyperoxaluria due to reduced activity of AGT. Defects in porphyrin metabolism can affect the transsulfuration pathway of sulfur amino acid metabolism leading to hyperhomocysteinemia [99]. This interrelationship could be partly explained by the knowledge of cofactors and regulation of cystathionine beta-synthase (CBS), catalyzing the first committed step. Haem, the synthetic product of porphyrin metabolism, is also a cofactor for the cystathionine beta-synthase enzyme [112]. Vitamin B6 is a cofactor for delta-aminolevulinic acid synthase 1 (ALAS1), the rate-limiting step of haem biosynthesis, and CBS and cystathionine-gamma lyase (CGL) in the transsulfuration pathway. CBS has a lower affinity for pyridoxal 5′-phosphate compared to ALAS1 and other pyridoxal 5′-phosphate-dependent enzymes in the tryptophan-kynurenine pathway and therefore is at a disadvantage when pyridoxal 5′-phosphate is decreased [112]. The plausible metabolic consequences of abnormal porphyrin metabolism in ASD are illustrated in Fig. 1.
Hypothesized mechanism for abnormal porphyrin metabolism and its metabolic consequences in ASD. Heavy metals may block several steps in haem biosynthesis resulting in porphyrinuria. Overconsumption of pyridoxal 5'-phosphate (PLP) by induced ALAS1 and PLP-dependent enzymes in the tryptophan-kynurenine pathway leads to reduced activity of other PLP-dependent enzymes, hence abnormal homocysteine, oxalate, and melatonin levels. (ALAS1; delta-aminolevulinic acid synthase 1, ALAD; delta-aminolevulinic acid dehydratase, PBGD; porphobilinogen deaminase, UROS; Uroporphyrinogen-III synthase, UROD; Uroporphyrinogen decarboxylase, CPOX; Oxygen-dependent coproporphyrinogen-III oxidase, PPOX; Protoporphyrinogen oxidase. FECH; Ferrochelatase)
CBS activity can be also reduced in haem deficiency, interfering with pyridoxal 5′-phosphate binding and promoting CBS degradation [112]. Therefore, hyperhomocysteinemia in porphyria patients is most likely to occur from decreased hepatic CBS and CGL activity due to low haem availability, as well as possible relative/absolute vitamin B6 deficiency caused by ALAS1 induction [99]. Considering the evidence at hand, deciding whether atypical porphyrin excretion in ASD is a cause or consequence is premature. The link between sulfur amino acid metabolism and porphyrin metabolism is further corroborated by a study demonstrating that compared to unaffected controls, compound heterozygotes for ALAD 177CG and RFC1 80AG variants were nearly four times more likely to be autistic. RFC1 encodes a reduced folate carrier involved in the folate transport, which is linked to the remethylation pathway of the methionine cycle [75]. Moreover, the same research group demonstrated that a significant lowering of plasma reduced glutathione and glutathione redox ratio in ASD children with ALAD2 allele compared to controls [75]. Despite adult acute porphyrias predominantly affecting females, pediatric-onset acute hepatic porphyria shows a male predominance [91], corresponding with the male predominance well-established in ASD [4].
Significance of Abnormal Thiol and Selenol Metabolism
Even though the underlying pathogenic mechanism of abnormal porphyrin metabolism is yet to be uncovered, the present understanding of metabolic interrelationships provides intriguing clues to a possible connection between abnormal thiol and selenol metabolism. Altered sulfur metabolism has received much attention due to consistently reported abnormalities corroborated by meta-analyses. Subjects with ASD have lower levels of methionine, cysteine, vitamin B12, folate, and S-adenosylmethionine to S-adenosylhomocysteine ratio [101]. In addition, the total thiol concentrations, median reduced thiol ratios, and mean native thiol were significantly lower. In contrast, median oxidized thiol ratios, redox potential, and median disulfide concentrations were considerably higher in children with ASD than in healthy controls [113].
Interestingly thiol groups in free cysteine, cysteine residues of proteins, selenol groups of seleno-cysteine, and seleno-cysteine residues of selenoenzymes and other selenoproteins are critical targets of Hg toxicity. The binding of Hg compounds to thiol and selenol groups depletes these substances and inhibits antioxidant enzymes, which are essential to mitigate oxidative damage [114]. Moreover, the effects of heavy metals on enzymes involved in thiol and selenol metabolism are brain region-specific especially affecting the hypothalamus and brainstem structures [115]. The sulfur-containing ligands exhibit protective and reactivation effects toward the enzyme inhibition [116].
Hg is a well-known toxic heavy metal that occurs in several forms, i.e., metallic Hg, Hg vapor, mercurous ions, mercuric ions, and organo-Hg compounds (e.g., methyl-Hg). Food contaminated with Hg, dental amalgams, Hg-containing cosmetics, and Hg-containing paints are some of the common sources of Hg exposure in humans [117]. The most toxic form, methyl-Hg, is readily absorbed via biological membranes such as gut and placenta due to its lipophilic nature [118]. It is easily complexed with cysteine to produce an abnormal amino acid analogous to methionine. Methyl-Hg competes with amino acids for transport via specialized amino acid transporters at the placenta and blood-brain barrier and accumulates in the brain [86]. These harmful actions of Hg are mitigated by glutathione, a naturally occurring chelator, that serves as the major detoxification mechanism of heavy metals (e.g., Hg and Pb) [75].
Interestingly pre-coproporphyrin and penta-carboxylporphyrin levels have shown a positive correlation with plasma-oxidized glutathione levels in subjects with ASD [42]. Depletion of thiols such as glutathione may predispose to increased susceptibility to heavy metal toxicity and resultant atypical urine porphyrin profile in subjects with ASD. The deficiency of thiols may reduce biliary and renal excretion of heavy metals, increasing their toxicity. Whole blood Hg levels were significantly higher in ASD patients compared to healthy subjects. The Hg level in hair was significantly lower in healthy subjects, whereas there was no difference in the urinary Hg level. This could be attributed to the evidence of an impairment in the detoxification and excretory mechanisms in ASD [119].
Cellular accumulation of oxalate (which is associated with abnormal haem metabolism, as discussed above) [96, 105] may also contribute to mitochondrial dysfunction and oxidative stress [120]. A significant proportion of cellular oxalate binding appears to occur in the mitochondria and the oxalate binding increases with thiol depletion [121]. Additionally, oxalate-induced mitochondrial dysfunction in circulating monocytes appears to alter plasma cytokine and chemokine levels [122]. In light of these findings, oxalate appears to connect many dots in the intricate pathogenic mechanism of ASD.
A metabolic Approach to the Treatment of ASD Associated with Porphyrinuria
Several chelating agents are used in clinical practice to manage heavy metal poisoning; dimercaprol, penicillamine, sodium calcium edetate, ethylenediaminetetraacetic acid (EDTA), succimer, etc. These agents bind to heavy metals (Pb, Hg, As) and facilitate renal excretion. Sulfhydryl moiety is responsible for the chelation of the metal ion forming a metal-sulfur linkage (Fig. 2) [123,124,125,126,127]. However, based on a Cochrane systematic review, there is no evidence that multiple rounds of oral DMSA would have an impact on ASD symptoms. On the other hand, chelation therapy is associated with serious adverse effects such as hypocalcemia, renal impairment, and even death. Therefore, the risks of using chelation for ASD treatment currently outweigh the proven benefits [128].
Several other supplements that can enhance natural chelation detoxification pathways, such as taurine, methionine, cysteine, alpha-lipoic acid and dihydrolipoic acid (DHLA), glutathione, and N-acetylcysteine (a precursor of glutathione), have received attention in addressing metal toxicities [116, 129]. Some of these agents, such as oral N-acetyl cysteine and oral alpha-lipoic acid are proposed as potential metabolic therapies that can be used in ASD associated with mitochondrial dysfunction [130]. Liposomal (absorbed better) and transdermal glutathione have shown benefits in improving plasma cysteine and reduced glutathione levels in subjects with ASD [131]. Evidencing metal chelation property, these compounds contain sulfhydryl moiety (Fig. 3), which can effectively chelate heavy metal ions of Hg and Pb. Notably, both reduced and oxidized forms of alpha-lipoic acid are known to chelate metal ions. At the same time, DHLA is a potent antioxidant in the body that can recycle other antioxidants like glutathione and ascorbic acid [132, 133]. Glutathione, N-acetylcysteine, and alpha-lipoic acid chelate heavy metals by forming a metal-sulfur linkage [134, 135] (Fig. 4). Additionally, alpha-lipoic acid can ameliorate mitochondrial dysfunction and increase ATP synthesis in cells with defective porphyrin metabolism [110]. The naturally occurring compounds with chelation properties are generally associated with minimal side effects and hence appear to be a good alternative to chelating agents associated with severe adverse effects such as DMSA. Moreover, calcium and iron supplementation attenuate Pb accumulation, while dietary deficiencies are reported to enhance Pb absorption. This forms the basis for using calcium and iron supplementation to manage Pb poisoning [136].
Nevertheless, the action of glutathione on brain Hg levels depends on the form of Hg. For instance, glutathione plays a crucial role in methylmercury transport into the brain. Watanabe et al. demonstrated that the transport of methylmercury into the brain is accelerated by glutathione, but retarded by the surplus glutathione. It was further suggested that methylmercury is transported into the brain after being converted to methylmercury-cysteine by gamma-glutamyl transpeptidase [137]. Conversely, elemental mercury uptake by the brain is increased by depletion of glutathione in rats [138]. DMSA, 2,3-dimercaptopropane-1-sulfonic acid (DMPS), glutathione, vitamin C, lipoic acid alone, or in combination were able to reduce kidney Hg levels but unable to reduce elementary Hg content of the brains of rats exposed to Hg [139, 140]. On the other hand, sulfhydryl compounds appear to have non-chelation functions such as free radical scavenging ability and protective effects against uroporphyrinogen-decarboxylase inhibition [141] that may be more relevant in the subset of ASD with abnormal porphyrinuria.
A study revealed that thiamin and thiamin monophosphate (TMP) concentrations are not significantly different from healthy subjects, while thiamin pyrophosphate (TPP) levels were decreased by 24% in children with ASD [142]. Moreover, dysautonomia associated with abnormal erythrocyte transketolase has been observed in two ASD individuals, indicating abnormal thiamin homeostasis. [143]. The use of thiamin in the treatment of ASD has mainly been due to its function as a cofactor in the citric acid cycle enzymes [130]. In one pilot study, two months of thiamine tetrahydrofurfuryl disulfide (TTFD) supplementation has shown clinical improvement in eight out of the ten children with ASD as measured by Autism Treatment Evaluation Checklist (ATEC), with an increase in urinary Cd and Pb observed in two children and one child, respectively [144]. Concomitant thiamine administration with chelators such as EDTA enhanced the efficacy by potentiating urinary Pb excretion, reducing tissue Pb including brain Pb, and restoring Pb-induced biochemical alterations, suggesting a promising role of thiamine as a complementary agent to heavy metal chelators [145]. Thiamin interacts with the pyrimidine ring, forming a readily excretable metal Pb-thiamine complex [146]. Facilitation of cellular penetration by EDTA and increasing effective chelation of intracellular bound Pb is another proposed mechanism [145]. Interestingly, thiamin is also a sulfur-containing molecule similar to most metal chelators. Importantly thiamin is a safe nutritional supplement with no adverse effects [130] but many beneficial metabolic effects in ASD.
Sulforaphane is a sulfur-containing compound found in cruciferous vegetables such as cauliflower, broccoli, and cabbage. It is a dietary supplement with minimal side effects. It has multiple biological effects pertinent to ASD, including antioxidant, anti-inflammatory, and neuroprotective effects. A systematic review of five clinical trials demonstrated a significant positive correlation between sulforaphane use and improvement in ASD behavior and cognitive function [147]. Metallothionein, a primary antioxidant enzyme involved in the metabolism and detoxification of heavy metals, is induced by sulforaphane through modulation of the MT gene expression [148]. Corroborating these findings, the administration of sulforaphane has been found to increase the brain glutathione levels [149].
The presence of hyperhomocysteinemia, hyperoxalemia/hyperoxaluria, vitamin B6 deficiency, and magnesium (Mg) implies that a vitamin B6, Mg, and low oxalate diet might be effective. Vitamin B6 will enhance the activity of vitamin B6-dependent enzymes such as CBS and thereby correct hyperhomocysteinemia. As many B6-dependent enzymes use Mg also as a co-factor, vitamin B6-Mg co-therapy appears to be a good combination [102]. On the other hand, vitamin B6 also has non-cofactor functions as a metal chelator and potent antioxidant, pertinent in ASD [150].
Additionally, lower blood Zn levels [53, 64] and elevated blood Cu/Zn ratios [35] were also found in ASD individuals. Therefore, it has been hypothesized that Hg toxicity-associated metallothionein dysfunction may be one of the contributory factors of Zn deficiency in children with ASD [151]. Therefore, Zn deficiency might potentiate the toxic effects of heavy metals even at a low level of exposure [65]. Zinc supplementation may be used as a possible preventative and therapeutic approach to lessen the core/co-occurring symptoms associated with ASD [102].
Another promising therapeutic approach in porphyrinuria-associated ASD is melatonin which has received attention in ASD [152] as well as in porphyria [153] and may be mediated by scavenging reactive oxygen species and suppression of the key enzyme ALAS1 [153]. Additionally, melatonin has been shown to reverse Pb-induced neurotoxicity in animal models by eliciting its properties via antioxidants and other mechanisms [154].
Multiple levels of evidence suggest a possible role of heavy metals, impaired detoxification pathways in the pathogenesis of autism, impaired porphyrin metabolites as potential biomarkers, and chelating agents, thiols, thiamin, and sulforaphane as potential therapeutic agents. The abnormal porphyrin metabolites appear to be candidate biomarkers useful in precision medicine in ASD. However, despite all that attention given to the heterogeneity of ASD, many studies compared the effectiveness of the heavy metal-targeted interventions between chelated-ASD subjects vs. non-chelated-ASD subjects. Future research should focus on comparing the efficacy of less invasive nutritional approaches in reducing co-symptoms and co-occurring symptoms in the subgroup of patients with increased porphyrin excretion.
Concluding Remarks
Porphyrin metabolites are potential biomarkers for ASD, having relatively low sensitivity but very high specificity. Their levels were positively correlated with the severity of autism. The low sensitivity is attributed to the high heterogeneity of this group of disorders with a broad spectrum of underlying pathogenic mechanisms. Heavy metal poisoning was proposed as one of the causative factors, as heavy metals are known inhibitors of several metabolic pathways. An abnormal urinary porphyrin profile was reported to correlate with ASD, and exposure to heavy metals may play a role. Several chelating agents have been used in clinical practice to manage heavy metal poisoning, but the risks of their use outweigh the proven benefits. Many supplements with therapeutic benefits in ASD, such as N-acetyl cysteine, alpha-lipoic acid, thiamin, sulforaphane, melatonin, and zinc appear to have potential benefits in the subgroup of ASD with abnormal porphyrin metabolism. However, more research into the role of abnormal porphyrin metabolism in ASD is needed to translate scientific evidence into clinical practice.
Data Availability
Not applicable
Abbreviations
- AGT:
-
Alanine-glyoxylate aminotransferase
- AIP:
-
Acute intermittent porphyria
- ALA:
-
Delta-aminolevulinic acid
- ALAD:
-
Delta-aminolevulinic acid dehydratase
- ALAS1:
-
Delta-aminolevulinic acid synthase 1
- AS:
-
Asperger’s syndrome
- ASD:
-
Autism spectrum disorder
- ATEC:
-
Autism Treatment Evaluation Checklist
- CBS:
-
Cystathionine beta-synthase
- Cd:
-
Cadmium
- CGL:
-
Cystathionine-gamma lyase
- CPOX:
-
Coproporphyrinogen III oxidase
- DHLA:
-
Dihydrolipoic acid
- DMPS:
-
Dimercaptopropane-1-sulfonic acid
- DMSA:
-
Dimercaptosuccinic acid
- DSM-5:
-
Diagnostic and Statistical Manual of Mental Disorders
- EDTA:
-
Ethylenediaminetetraacetic acid
- Hg:
-
Mercury
- Mg:
-
Magnesium
- PBGS:
-
Porphobilinogen synthase
- Pb:
-
Lead
- TMP:
-
Thiamine monophosphate
- TPP:
-
Thiamine pyrophosphate
- TTFD:
-
Thiamine tetrahydrofurfuryl disulfide
- UROD:
-
Uroporphyrin decarboxylase
- Zn:
-
Zinc
References
American Psychiatric Association (2022) Diagnostic and statistical manual of mental disorders, fifth edition, text revision. American psychiatric association Washington, DC
Lord C, Elsabbagh M, Baird G, Veenstra-Vanderweele J (2018) Autism spectrum disorder. The Lancet 392(10146):508–520. https://doi.org/10.1016/S0140-6736(18)31129-2
Zeidan J, Fombonne E, Scorah J, Ibrahim A, Durkin MS, Saxena S, Yusuf A, Shih A et al (2022) Global prevalence of autism: a systematic review update. Autism Res 15(5):778–790. https://doi.org/10.1002/aur.2696
Maenner MJ, Shaw KA, Baio J, Washington A, Patrick M, DiRienzo M, Christensen DL, Wiggins LD et al (2020) Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2016. MMWR Surveill Summ 69(4):1–12. https://doi.org/10.15585/mmwr.ss6904a1
Elsabbagh M, Divan G, Koh YJ, Kim YS, Kauchali S, Marcín C, Montiel-Nava C, Patel V et al (2012) Global prevalence of autism and other pervasive developmental disorders. Autism Res 5(3):160–179. https://doi.org/10.1002/aur.239
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub
Morgan B, Nageye F, Masi G, Cortese S (2020) Sleep in adults with autism spectrum disorder: a systematic review and meta-analysis of subjective and objective studies. Sleep Med 65:113–120. https://doi.org/10.1016/j.sleep.2019.07.019
Díaz-Román A, Zhang J, Delorme R, Beggiato A, Cortese S (2018) Sleep in youth with autism spectrum disorders: systematic review and meta-analysis of subjective and objective studies. Evid Based Ment Health 21(4):146–154. https://doi.org/10.1136/ebmental-2018-300037
Cortese S, Wang F, Angriman M, Masi G, Bruni O (2020) Sleep disorders in children and adolescents with autism spectrum disorder: diagnosis, epidemiology, and management. CNS Drugs 34(4):415–423. https://doi.org/10.1007/s40263-020-00710-y
Lukmanji S, Manji SA, Kadhim S, Sauro KM, Wirrell EC, Kwon CS, Jetté N (2019) The co-occurrence of epilepsy and autism: a systematic review. Epilepsy Behav 98(Pt A):238–248. https://doi.org/10.1016/j.yebeh.2019.07.037
Senarathne UD, Indika N-LR, Jezela-Stanek A, Ciara E, Frye RE, Chen C, Stepien KM (2023) Biochemical, genetic and clinical diagnostic approaches to autism-associated inherited metabolic disorders. Genes 14(4):803
Genovese A, Butler MG (2020) Clinical assessment, genetics, and treatment approaches in autism spectrum disorder (ASD). Int J Mol Sci 21(13). https://doi.org/10.3390/ijms21134726
Munnich A, Demily C, Frugère L, Duwime C, Malan V, Barcia G, Vidal C, Throo E et al (2019) Impact of on-site clinical genetics consultations on diagnostic rate in children and young adults with autism spectrum disorder. Mol Autism 10:33. https://doi.org/10.1186/s13229-019-0284-2
Bhandari R, Paliwal JK, Kuhad A (2020) Neuropsychopathology of autism spectrum disorder: complex interplay of genetic, epigenetic, and environmental factors. Adv Neurobiol 24:97–141. https://doi.org/10.1007/978-3-030-30402-7_4
Srikantha P, Mohajeri MH (2019) The possible role of the microbiota-gut-brain-axis in autism spectrum disorder. Int J Mol Sci 20(9). https://doi.org/10.3390/ijms20092115
Rossignol DA, Frye RE (2012) A review of research trends in physiological abnormalities in autism spectrum disorders: immune dysregulation, inflammation, oxidative stress, mitochondrial dysfunction and environmental toxicant exposures. Mol Psychiatry 17(4):389–401. https://doi.org/10.1038/mp.2011.165
Rafiee F, Rezvani Habibabadi R, Motaghi M, Yousem DM, Yousem IJ (2022) Brain MRI in autism spectrum disorder: narrative review and recent advances. J Magn Reson Imaging 55(6):1613–1624. https://doi.org/10.1002/jmri.27949
El-Ansary A, Bjørklund G, Chirumbolo S, Alnakhli OM (2017) Predictive value of selected biomarkers related to metabolism and oxidative stress in children with autism spectrum disorder. Metab Brain Dis 32(4):1209–1221. https://doi.org/10.1007/s11011-017-0029-x
Rossignol DA, Frye RE (2012) Mitochondrial dysfunction in autism spectrum disorders: a systematic review and meta-analysis. Mol Psychiatry 17(3):290–314. https://doi.org/10.1038/mp.2010.136
Indika NR, Deutz NEP, Engelen M, Peiris H, Wijetunge S, Perera R (2021) Sulfur amino acid metabolism and related metabotypes of autism spectrum disorder: a review of biochemical evidence for a hypothesis. Biochimie 184:143–157. https://doi.org/10.1016/j.biochi.2021.02.018
Zheng Z, Zhu T, Qu Y, Mu D (2016) Blood glutamate levels in autism spectrum disorder: a systematic review and meta-analysis. PLoS One 11(7):e0158688. https://doi.org/10.1371/journal.pone.0158688
Gabriele S, Sacco R, Persico AM (2014) Blood serotonin levels in autism spectrum disorder: a systematic review and meta-analysis. Eur Neuropsychopharmacol 24(6):919–929. https://doi.org/10.1016/j.euroneuro.2014.02.004
Pavăl D, Micluția IV (2021) The dopamine hypothesis of autism spectrum disorder revisited: current status and future prospects. Dev Neurosci 43(2):73–83. https://doi.org/10.1159/000515751
Tisato V, Silva JA, Longo G, Gallo I, Singh AV, Milani D, Gemmati D (2021) Genetics and epigenetics of one-carbon metabolism pathway in autism spectrum disorder: a sex-specific brain epigenome? Genes (Basel) 12(5). https://doi.org/10.3390/genes12050782
James SJ, Melnyk S, Jernigan S, Pavliv O, Trusty T, Lehman S, Seidel L, Gaylor DW et al (2010) A functional polymorphism in the reduced folate carrier gene and DNA hypomethylation in mothers of children with autism. Am J Med Genet B Neuropsychiatr Genet 153b(6):1209–1220. https://doi.org/10.1002/ajmg.b.31094
Pasca SP, Dronca E, Ts K, Craciun EC, Ek E, Ferencz BK, Iftene F, Benga I et al (2009) One carbon metabolism disturbances and the C677T MTHFR gene polymorphism in children with autism spectrum disorders. J Cell Mol Med 13(10):4229–4238. https://doi.org/10.1111/j.1582-4934.2008.00463.x
Dai S, Lin J, Hou Y, Luo X, Shen Y, Ou J (2023) Purine signaling pathway dysfunction in autism spectrum disorders: evidence from multiple omics data. Front Mol Neurosci 16:1089871. https://doi.org/10.3389/fnmol.2023.1089871
Geier DA, Kern JK, Geier MR (2009) A prospective blinded evaluation of urinary porphyrins verses the clinical severity of autism spectrum disorders. J Toxicol Environ Health A 72(24):1585–1591. https://doi.org/10.1080/15287390903232475
Heyer NJ, Echeverria D, Woods JS (2012) Disordered porphyrin metabolism: a potential biological marker for autism risk assessment. Autism Res 5(2):84–92. https://doi.org/10.1002/aur.236
Nataf R, Skorupka C, Lam A, Springbett A, Lathe R (2008) Porphyrinuria in childhood autistic disorder is not associated with urinary creatinine deficiency. Pediatr Int 50(4):528–532. https://doi.org/10.1111/j.1442-200X.2008.02621.x
Woods JS, Armel SE, Fulton DI, Allen J, Wessels K, Simmonds PL, Granpeesheh D, Mumper E et al (2010) Urinary porphyrin excretion in neurotypical and autistic children. Environ Health Perspect 118(10):1450–1457. https://doi.org/10.1289/ehp.0901713
Kaneko JJ (1980) 4 - Porphyrin, heme, and erythrocyte metabolism: the porphyrias. In: Kaneko JJ (ed) Clinical biochemistry of domestic animals, third edn. Academic Press, pp. 119–174. https://doi.org/10.1016/B978-0-12-396350-5.50009-7
Phillips JD (2019) Heme biosynthesis and the porphyrias. Mol Genet Metab 128(3):164–177. https://doi.org/10.1016/j.ymgme.2019.04.008
Khaled EM, Meguid NA, Bjørklund G, Gouda A, Bahary MH, Hashish A, Sallam NM, Chirumbolo S et al (2016) Altered urinary porphyrins and mercury exposure as biomarkers for autism severity in Egyptian children with autism spectrum disorder. Metab Brain Dis 31(6):1419. https://doi.org/10.1007/s11011-016-9870-6
Macedoni-Lukšič M, Gosar D, Bjørklund G, Oražem J, Kodrič J, Lešnik-Musek P, Zupančič M, France-Štiglic A et al (2015) Levels of metals in the blood and specific porphyrins in the urine in children with autism spectrum disorders. Biol Trace Elem Res 163(1-2):2–10. https://doi.org/10.1007/s12011-014-0121-6
Kern JK, Geier DA, Adams JB, Mehta JA, Grannemann BD, Geier MR (2011) Toxicity biomarkers in autism spectrum disorder: a blinded study of urinary porphyrins. Pediatr Int 53(2):147–153. https://doi.org/10.1111/j.1442-200X.2010.03196.x
Geier DA, Geier MR (2007) A prospective study of mercury toxicity biomarkers in autistic spectrum disorders. J Toxicol Environ Health A 70(20):1723–1730. https://doi.org/10.1080/15287390701457712
Geier DA, Geier MR (2006) A prospective assessment of porphyrins in autistic disorders: a potential marker for heavy metal exposure. Neurotox Res 10(1):57–63. https://doi.org/10.1007/BF03033334
Woods J (1995) Porphyrin metabolism as indicator of metal exposure and toxicity. In: Toxicology of metals. Springer, pp. 19–52
Kern JK, Geier DA, Sykes LK, Haley BE, Geier MR (2016) The relationship between mercury and autism: a comprehensive review and discussion. J Trace Elem Med Biol 37:8–24. https://doi.org/10.1016/j.jtemb.2016.06.002
Nataf R, Skorupka C, Amet L, Lam A, Springbett A, Lathe R (2006) Porphyrinuria in childhood autistic disorder: implications for environmental toxicity. Toxicol Appl Pharmacol 214(2):99–108. https://doi.org/10.1016/j.taap.2006.04.008
Geier DA, Kern JK, Garver CR, Adams JB, Audhya T, Nataf R, Geier MR (2009) Biomarkers of environmental toxicity and susceptibility in autism. J Neurol Sci 280(1-2):101–108. https://doi.org/10.1016/j.jns.2008.08.021
Austin DW, Shandley K (2008) An investigation of porphyrinuria in Australian children with autism. J Toxicol Environ Health, A 71(20):1349–1351. https://doi.org/10.1080/15287390802271723
Shandley K, Austin DW, Bhowmik JL (2014) Are urinary porphyrins a valid diagnostic biomarker of autism spectrum disorder? Autism Res 7(5):535–542. https://doi.org/10.1002/aur.1385
Youn S-I, Jin S-H, Kim S-H, Lim S (2010) Porphyrinuria in Korean children with autism: correlation with oxidative stress. J Toxicol Environ Health, A 73(10):701–710. https://doi.org/10.1080/15287391003614000
Harutyunyan AA, Harutyunyan HA, Yenkoyan KB (2021) Novel probable glance at inflammatory scenario development in autistic pathology. Front Psychiatry 12:788779. https://doi.org/10.3389/fpsyt.2021.788779
Rossignol DA, Genuis SJ, Frye RE (2014) Environmental toxicants and autism spectrum disorders: a systematic review. Transl Psychiatry 4(2):e360. https://doi.org/10.1038/tp.2014.4
Adams J, Howsmon DP, Kruger U, Geis E, Gehn E, Fimbres V, Pollard E, Mitchell J et al (2017) Significant association of urinary toxic metals and autism-related symptoms-a nonlinear statistical analysis with cross validation. PLoS One 12(1):e0169526. https://doi.org/10.1371/journal.pone.0169526
Heyer NJ, Bittner AC Jr, Echeverria D, Woods JS (2006) A cascade analysis of the interaction of mercury and coproporphyrinogen oxidase (CPOX) polymorphism on the heme biosynthetic pathway and porphyrin production. Toxicol Lett 161(2):159–166. https://doi.org/10.1016/j.toxlet.2005.09.005
Pingree SD, Simmonds PL, Rummel KT, Woods JS (2001) Quantitative evaluation of urinary porphyrins as a measure of kidney mercury content and mercury body burden during prolonged methylmercury exposure in rats. Toxicol Sci 61(2):234–240. https://doi.org/10.1093/toxsci/61.2.234
Kern JK, Geier DA, Ayzac F, Adams JB, Mehta JA, Geier MR (2011) Toxicity biomarkers among US children compared to a similar cohort in France: a blinded study measuring urinary porphyrins. Toxicol Environ Chem 93(1-2):396–405. https://doi.org/10.1080/02772248.2010.508609
Layer G, Reichelt J, Jahn D, Heinz DW (2010) Structure and function of enzymes in heme biosynthesis. Protein Sci 19(6):1137–1161. https://doi.org/10.1002/pro.405
Zhang J, Li X, Shen L, Khan NU, Zhang X, Chen L, Zhao H, Luo P (2021) Trace elements in children with autism spectrum disorder: a meta-analysis based on case-control studies. J Trace Elem Med Biol 67:126782. https://doi.org/10.1016/j.jtemb.2021.126782
Bradstreet J, Geier DA, Kartzinel JJ, Adams JB, Geier MR (2003) A case-control study of mercury burden in children with autistic spectrum disorders. J Am Phys Surg 8(3):76–79
Windham GC, Zhang L, Gunier R, Croen LA, Grether JK (2006) Autism spectrum disorders in relation to distribution of hazardous air pollutants in the san francisco bay area. Environ Health Perspect 114(9):1438–1444. https://doi.org/10.1289/ehp.9120
Bartell SM, Lewandowski TA (2011) Administrative censoring in ecological analyses of autism and a Bayesian solution. J Environ Public Health 2011:202783. https://doi.org/10.1155/2011/202783
Blanchard KS, Palmer RF, Stein Z (2011) The value of ecologic studies: mercury concentration in ambient air and the risk of autism. Rev Environ Health 26(2):111–118. https://doi.org/10.1515/reveh.2011.015
DeSoto MC, Hitlan RT (2012) Fish consumption advisories and the surprising relationship to prevalence rate of developmental disability as reported by public schools. J Environ Prot (Irvine, Calif) 03(11):11. https://doi.org/10.4236/jep.2012.311174
Lewandowski TA, Bartell SM, Yager JW, Levin L (2009) An evaluation of surrogate chemical exposure measures and autism prevalence in Texas. J Toxicol Environ Health A 72(24):1592–1603. https://doi.org/10.1080/15287390903232483
Palmer RF, Blanchard S, Stein Z, Mandell D, Miller C (2006) Environmental mercury release, special education rates, and autism disorder: an ecological study of Texas. Health Place 12(2):203–209. https://doi.org/10.1016/j.healthplace.2004.11.005
Palmer RF, Blanchard S, Wood R (2009) Proximity to point sources of environmental mercury release as a predictor of autism prevalence. Health Place 15(1):18–24. https://doi.org/10.1016/j.healthplace.2008.02.001
Rury J (2006) Links between environmental mercury, special education, and autism in Louisiana. Louisiana State University
Schweikert C, Li Y, Dayya D, Yens D, Torrents M, Hsu DF (2009) Analysis of autism prevalence and neurotoxins using combinatorial fusion and association rule mining. In: In: 2009 Ninth IEEE International Conference on Bioinformatics and BioEngineering. IEEE, pp. 400–404
Saghazadeh A, Ahangari N, Hendi K, Saleh F, Rezaei N (2017) Status of essential elements in autism spectrum disorder: systematic review and meta-analysis. Rev Neurosci 28(7):783–809. https://doi.org/10.1515/revneuro-2017-0015
Błażewicz A, Grabrucker AM (2022) Metal profiles in autism spectrum disorders: a crosstalk between toxic and essential metals. Int J Mol Sci 24(1). https://doi.org/10.3390/ijms24010308
Farina M, Brandão R, Lara FS, Soares FA, Souza DO, Rocha JB (2003) Mechanisms of the inhibitory effects of selenium and mercury on the activity of delta-aminolevulinate dehydratase from mouse liver, kidney and brain. Toxicol Lett 139(1):55–66. https://doi.org/10.1016/s0378-4274(02)00454-x
Jaffe EK, Martins J, Li J, Kervinen J, Dunbrack RL Jr (2001) The molecular mechanism of lead inhibition of human porphobilinogen synthase. J Biol Chem 276(2):1531–1537. https://doi.org/10.1074/jbc.M007663200
de Souza PVS, Badia BML, Farias IB, Pinto W, Oliveira ASB (2021) Acute hepatic porphyria: pathophysiological basis of neuromuscular manifestations. Front Neurosci 15:715523. https://doi.org/10.3389/fnins.2021.715523
Akshatha L, Rukmini M, Mamatha TS, Sadashiva Rao P, Prashanth B (2014) Lead poisoning mimicking acute porphyria! J Clin Diagn Res 8(12):CD01–CD02
Rossi E, Taketani S, Garcia-Webb P (1993) Lead and the terminal mitochondrial enzymes of haem biosynthesis. Biomed Chromatogr 7(1):1–6. https://doi.org/10.1002/bmc.1130070102
Li T, Woods JS (2009) Cloning, expression, and biochemical properties of CPOX4, a genetic variant of coproporphyrinogen oxidase that affects susceptibility to mercury toxicity in humans. Toxicol Sci 109(2):228–236. https://doi.org/10.1093/toxsci/kfp066
Woods JS, Kardish R, Fowler BA (1981) Studies on the action of porphyrinogenic trace metals on the activity of hepatic uroporphyrinogen decarboxylase. Biochem Biophys Res Commun 103(1):264–271. https://doi.org/10.1016/0006-291x(81)91688-0
Qader A, Rehman K, Akash MSH (2021) Genetic susceptibility of δ-ALAD associated with lead (Pb) intoxication: sources of exposure, preventive measures, and treatment interventions. Environ Sci Pollut Res Int 28(33):44818–44832. https://doi.org/10.1007/s11356-021-15323-1
Schwartz BS, Lee BK, Stewart W, Ahn KD, Springer K, Kelsey K (1995) Associations of delta-aminolevulinic acid dehydratase genotype with plant, exposure duration, and blood lead and zinc protoporphyrin levels in Korean lead workers. Am J Epidemiol 142(7):738–745. https://doi.org/10.1093/oxfordjournals.aje.a117705
Rose S, Melnyk S, Savenka A, Hubanks A, Jernigan S, Cleves M, James SJ (2008) The frequency of polymorphisms affecting lead and mercury toxicity among children with autism. Am J Biochem Biotech 4(2):85–94
Kayaaltı Z, Sert S, Kaya-Akyüzlü D, Söylemez E, Söylemezoğlu T (2016) Association between delta-aminolevulinic acid dehydratase polymorphism and placental lead levels. Environ Toxicol Pharmacol 41:147–151. https://doi.org/10.1016/j.etap.2015.11.017
Woods JS, Echeverria D, Heyer NJ, Simmonds PL, Wilkerson J, Farin FM (2005) The association between genetic polymorphisms of coproporphyrinogen oxidase and an atypical porphyrinogenic response to mercury exposure in humans. Toxicol Appl Pharmacol 206(2):113–120. https://doi.org/10.1016/j.taap.2004.12.016
Nuttall KL (2004) Interpreting mercury in blood and urine of individual patients. Ann Clin Lab Sci 34(3):235–250
Lo YH, Shen CM, Chang WK (2020) Intractable abdominal pain with purple colored urine. Am J Med Sci 360(4):e5–e6. https://doi.org/10.1016/j.amjms.2020.05.010
Kaneko M, Kazatani T, Shikata H (2020) Occupational lead poisoning in a patient with acute abdomen and normocytic anemia. Intern Med 59(12):1565–1570. https://doi.org/10.2169/internalmedicine.4176-19
Tsai MT, Huang SY, Cheng SY (2017) Lead poisoning can be easily misdiagnosed as acute porphyria and nonspecific abdominal pain. Case Rep Emerg Med 2017:9050713. https://doi.org/10.1155/2017/9050713
Pramono A, Panunggal B, Rahfiludin MZ, Swastawati F (2017) Low zinc serum levels and high blood lead levels among school-age children in coastal area. IOP Conf Ser: Earth Environ Sci 55(1):012058. https://doi.org/10.1088/1755-1315/55/1/012058
Loomes R, Hull L, Mandy WPL (2017) What is the male-to-female ratio in autism spectrum disorder? a systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry 56(6):466–474. https://doi.org/10.1016/j.jaac.2017.03.013
Singh G, Singh V, Sobolewski M, Cory-Slechta DA, Schneider JS (2018) Sex-dependent effects of developmental lead exposure on the brain. Front Genet 9:89. https://doi.org/10.3389/fgene.2018.00089
Kern JK, Geier DA, Homme KG, King PG, Bjørklund G, Chirumbolo S, Geier MR (2017) Developmental neurotoxicants and the vulnerable male brain: a systematic review of suspected neurotoxicants that disproportionally affect males. Acta Neurobiol Exp (Wars) 77(4):269–296
Gade M, Comfort N, Re DB (2021) Sex-specific neurotoxic effects of heavy metal pollutants: epidemiological, experimental evidence and candidate mechanisms. Environ Res 201:111558. https://doi.org/10.1016/j.envres.2021.111558
Lozano M, Murcia M, Soler-Blasco R, González L, Iriarte G, Rebagliato M, Lopez-Espinosa MJ, Esplugues A et al (2021) Exposure to mercury among 9-year-old children and neurobehavioural function. Environ Int 146:106173. https://doi.org/10.1016/j.envint.2020.106173
Ruszkiewicz JA, Miranda-Vizuete A, Tinkov AA, Skalnaya MG, Skalny AV, Tsatsakis A, Aschner M (2019) Sex-specific differences in redox homeostasis in brain norm and disease. J Mol Neurosci 67(2):312–342. https://doi.org/10.1007/s12031-018-1241-9
Rahbar MH, Samms-Vaughan M, Saroukhani S, Bressler J, Hessabi M, Grove ML, Shakspeare-Pellington S, Loveland KA et al (2021) Associations of metabolic genes (GSTT1, GSTP1, GSTM1) and blood mercury concentrations differ in Jamaican children with and without autism spectrum disorder. Int J Environ Res Public Health 18(4). https://doi.org/10.3390/ijerph18041377
Luder AS, Mamet R, Farbstein I, Schoenfeld N (2009) Awareness is the name of the game: clinical and biochemical evaluation of a case of a girl diagnosed with acute intermittent porphyria associated with autism. Cell Mol Biol (Noisy-le-grand) 55(1):19–22
Jaramillo-Calle DA, Martinez YA, Balwani M, Fernandez C, Toro M (2021) Porphyria attacks in prepubertal children and adolescents. Mol Genet Metab 133(3):242–249. https://doi.org/10.1016/j.ymgme.2021.04.008
Bjørklund G, Pivina L, Dadar M, Meguid NA, Semenova Y, Anwar M, Chirumbolo S (2020) Gastrointestinal alterations in autism spectrum disorder: what do we know? Neurosci Biobehav Rev 118:111–120. https://doi.org/10.1016/j.neubiorev.2020.06.033
Besag FMC, Vasey MJ (2021) Seizures and epilepsy in autism spectrum disorder. Psychiatr Clin North Am 44(1):51–68. https://doi.org/10.1016/j.psc.2020.11.005
Howes OD, Rogdaki M, Findon JL, Wichers RH, Charman T, King BH, Loth E, McAlonan GM et al (2018) Autism spectrum disorder: consensus guidelines on assessment, treatment and research from the British Association for Psychopharmacology. J Psychopharm 32(1):3–29. https://doi.org/10.1177/0269881117741766
Fung LK, Mahajan R, Nozzolillo A, Bernal P, Krasner A, Jo B, Coury D, Whitaker A et al (2016) Pharmacologic treatment of severe irritability and problem behaviors in autism: a systematic review and meta-analysis. Pediatrics 137(Suppl 2):S124–S135. https://doi.org/10.1542/peds.2015-2851K
Chacko B, Culp ML, Bloomer J, Phillips J, Kuo YF, Darley-Usmar V, Singal AK (2019) Feasibility of cellular bioenergetics as a biomarker in porphyria patients. Mol Genet Metab Rep 19:100451. https://doi.org/10.1016/j.ymgmr.2019.100451
Liu X, Lin J, Zhang H, Khan NU, Zhang J, Tang X, Cao X, Shen L (2022) Oxidative stress in autism spectrum disorder-current progress of mechanisms and biomarkers. Front Psychiatry 13:813304–813304. https://doi.org/10.3389/fpsyt.2022.813304
Pecorelli A, Ferrara F, Messano N, Cordone V, Schiavone ML, Cervellati F, Woodby B, Cervellati C et al (2020) Alterations of mitochondrial bioenergetics, dynamics, and morphology support the theory of oxidative damage involvement in autism spectrum disorder. FASEB J 34(5):6521–6538. https://doi.org/10.1096/fj.201902677R
Ventura P, Corradini E, Di Pierro E, Marchini S, Marcacci M, Cuoghi C, Buzzetti E, Pietrangelo A (2020) Hyperhomocysteinemia in patients with acute porphyrias: a potentially dangerous metabolic crossroad? Eur J Intern Med 79:101–107. https://doi.org/10.1016/j.ejim.2020.04.002
Ali A, Waly MI, Al-Farsi YM, Essa MM, Al-Sharbati MM, Deth RC (2011) Hyperhomocysteinemia among Omani autistic children: a case-control study. Acta Biochim Pol 58(4)
Chen L, Shi XJ, Liu H, Mao X, Gui LN, Wang H, Cheng Y (2021) Oxidative stress marker aberrations in children with autism spectrum disorder: a systematic review and meta-analysis of 87 studies (N = 9109). Transl Psychiatry 11(1):15. https://doi.org/10.1038/s41398-020-01135-3
Indika NR, Frye RE, Rossignol DA, Owens SC, Senarathne UD, Grabrucker AM, Perera R, Engelen M et al (2023) The rationale for vitamin, mineral, and cofactor treatment in the precision medical care of autism spectrum disorder. J Pers Med 13(2). https://doi.org/10.3390/jpm13020252
Ricci A, Di Pierro E, Marcacci M, Ventura P (2021) Mechanisms of neuronal damage in acute hepatic porphyrias. Diagnostics (Basel) 11(12). https://doi.org/10.3390/diagnostics11122205
Mydlík M, Derzsiová K (2010) Vitamin B6 and oxalic acid in clinical nephrology. J Ren Nutr 20(5 Suppl):S95–S102. https://doi.org/10.1053/j.jrn.2010.06.009
Konstantynowicz J, Porowski T, Zoch-Zwierz W, Wasilewska J, Kadziela-Olech H, Kulak W, Owens SC, Piotrowska-Jastrzebska J et al (2012) A potential pathogenic role of oxalate in autism. Eur J Paediatr Neurol 16(5):485–491. https://doi.org/10.1016/j.ejpn.2011.08.004
Wang B, Rudnick S, Cengia B, Bonkovsky HL (2019) Acute hepatic porphyrias: review and recent progress. Hepatol Commun 3(2):193–206. https://doi.org/10.1002/hep4.1297
Gevi F, Zolla L, Gabriele S, Persico AM (2016) Urinary metabolomics of young Italian autistic children supports abnormal tryptophan and purine metabolism. Mol Autism 7(1):47. https://doi.org/10.1186/s13229-016-0109-5
Felitsyn N, McLeod C, Shroads AL, Stacpoole PW, Notterpek L (2008) The heme precursor delta-aminolevulinate blocks peripheral myelin formation. J Neurochem 106(5):2068–2079. https://doi.org/10.1111/j.1471-4159.2008.05552.x
Solares I, Jericó D, Córdoba KM, Morales-Conejo M, Ena J, Enríquez de Salamanca R, Fontanellas A (2022) Understanding carbohydrate metabolism and insulin resistance in acute intermittent porphyria. Int J Mol Sci 24(1). https://doi.org/10.3390/ijms24010051
Longo M, Paolini E, Meroni M, Duca L, Motta I, Fracanzani AL, Di Pierro E, Dongiovanni P (2021) α-Lipoic acid improves hepatic metabolic dysfunctions in acute intermittent porphyria: a proof-of-concept study. Diagnostics (Basel) 11(9). https://doi.org/10.3390/diagnostics11091628
Fargue S, Acquaviva Bourdain C (2022) Primary hyperoxaluria type 1: pathophysiology and genetics. Clin Kidney J 15(Suppl 1):i4–i8. https://doi.org/10.1093/ckj/sfab217
Badawy AA (2021) Multiple roles of haem in cystathionine β-synthase activity: implications for hemin and other therapies of acute hepatic porphyria. Biosci Rep 41(7). https://doi.org/10.1042/bsr20210935
Ayaydın H, Kılıçaslan F, Koyuncu İ, Çelik H, Çalık M, Güzelçiçek A, Kirmit A (2021) Impaired thiol/disulfide homeostasis in children diagnosed with autism: a case-control study. J Mol Neurosci 71(7):1394–1402. https://doi.org/10.1007/s12031-021-01790-1
Carocci A, Rovito N, Sinicropi MS, Genchi G (2014) Mercury toxicity and neurodegenerative effects. Rev Environ Contam Toxicol 229:1–18. https://doi.org/10.1007/978-3-319-03777-6_1
Malqui H, Anarghou H, Ouardi FZ, Ouasmi N, Najimi M, Chigr F (2018) Continuous exposure to inorganic mercury affects neurobehavioral and physiological parameters in mice. J Mol Neurosci 66(2):291–305. https://doi.org/10.1007/s12031-018-1176-1
Colovic MB, Vasic VM, Djuric DM, Krstic DZ (2018) Sulphur-containing amino acids: protective role against free radicals and heavy metals. Curr Med Chem 25(3):324–335. https://doi.org/10.2174/0929867324666170609075434
Clarkson TW (1997) The toxicology of mercury. Crit Rev Clin Lab Sci 34(4):369–403. https://doi.org/10.3109/10408369708998098
Gad SC (2014) Methylmercury. In: Wexler P (ed) Encyclopedia of toxicology, third edn. Academic Press, Oxford, pp. 318–320. https://doi.org/10.1016/B978-0-12-386454-3.00881-2
Jafari T, Rostampour N, Fallah AA, Hesami A (2017) The association between mercury levels and autism spectrum disorders: a systematic review and meta-analysis. J Trace Elem Med Biol 44:289–297. https://doi.org/10.1016/j.jtemb.2017.09.002
Patel M, Yarlagadda V, Adedoyin O, Saini V, Assimos DG, Holmes RP, Mitchell T (2018) Oxalate induces mitochondrial dysfunction and disrupts redox homeostasis in a human monocyte derived cell line. Redox Biol 15:207–215. https://doi.org/10.1016/j.redox.2017.12.003
Selvam R, Kalaiselvi P (2003) Oxalate binding proteins in calcium oxalate nephrolithiasis. Urol Res 31(4):242–256. https://doi.org/10.1007/s00240-003-0316-3
Kumar P, Patel M, Oster RA, Yarlagadda V, Ambrosetti A, Assimos DG, Mitchell T (2021) Dietary oxalate loading impacts monocyte metabolism and inflammatory signaling in humans. Front Immunol 12:617508. https://doi.org/10.3389/fimmu.2021.617508
Sisombath NS, Jalilehvand F, Schell AC, Wu Q (2014) Lead(II) binding to the chelating agent d-penicillamine in aqueous solution. Inorg Chem 53(23):12459–12468. https://doi.org/10.1021/ic5018714
Leung BO, Jalilehvand F, Mah V (2007) Mercury(ii) penicillamine complex formation in alkaline aqueous solution. Dalton Transactions 41:4666–4674. https://doi.org/10.1039/B711436B
Sakthithasan K, Lévy P, Poupon J, Garnier R (2018) A comparative study of edetate calcium disodium and dimercaptosuccinic acid in the treatment of lead poisoning in adults. Clin Toxicol (Phila) 56(11):1143–1149. https://doi.org/10.1080/15563650.2018.1478424
Markowitz ME, Rosen JF (1991) Need for the lead mobilization test in children with lead poisoning. J Pediatr 119(2):305–310. https://doi.org/10.1016/s0022-3476(05)80750-4
Flora SJ, Pachauri V (2010) Chelation in metal intoxication. Int J Environ Res Public Health 7(7):2745–2788. https://doi.org/10.3390/ijerph7072745
James S, Stevenson SW, Silove N, Williams K (2015) Chelation for autism spectrum disorder (ASD). Cochrane Database Syst Rev 5:Cd010766. https://doi.org/10.1002/14651858.Cd010766
Sears ME (2013) Chelation: harnessing and enhancing heavy metal detoxification--a review. Sci World J 2013:219840. https://doi.org/10.1155/2013/219840
Frye RE (2020) Mitochondrial dysfunction in autism spectrum disorder: unique abnormalities and targeted treatments. Semin Pediatr Neurol 35:100829. https://doi.org/10.1016/j.spen.2020.100829
Kern JK, Geier DA, Adams JB, Garver CR, Audhya T, Geier MR (2011) A clinical trial of glutathione supplementation in autism spectrum disorders. Med Sci Monit 17(12):Cr677–Cr682. https://doi.org/10.12659/msm.882125
Bjørklund G, Aaseth J, Crisponi G, Rahman MM, Chirumbolo S (2019) Insights on alpha lipoic and dihydrolipoic acids as promising scavengers of oxidative stress and possible chelators in mercury toxicology. J Inorg Biochem 195:111–119. https://doi.org/10.1016/j.jinorgbio.2019.03.019
Flora SJ (2009) Structural, chemical and biological aspects of antioxidants for strategies against metal and metalloid exposure. Oxid Med Cell Longev 2(4):191–206. https://doi.org/10.4161/oxim.2.4.9112
Mah V, Jalilehvand F (2012) Lead(II) complex formation with glutathione. Inorg Chem 51(11):6285–6298. https://doi.org/10.1021/ic300496t
Jalilehvand F, Parmar K, Zielke S (2013) Mercury(ii) complex formation with N-acetylcysteine. Metallomics 5(10):1368–1376. https://doi.org/10.1039/C3MT00173C
WHO (2021) WHO guideline for clinical management of exposure to lead. World Health Organization
Watanabe H, Shimojo N, Sano K, Yamaguchi S (1988) The distribution of total mercury in the brain after the lateral ventricular single injection of methylmercury and glutathione. Res Commun Chem Pathol Pharmacol 60(1):57–69
Eide I, Syversen TL (1983) Uptake of elemental mercury by brain in relation to concentration of glutathione and activity of glutathione peroxidase. Toxicol Lett 17(3-4):209–213. https://doi.org/10.1016/0378-4274(83)90228-x
Aposhian HV, Morgan DL, Queen HL, Maiorino RM, Aposhian MM (2003) Vitamin C, glutathione, or lipoic acid did not decrease brain or kidney mercury in rats exposed to mercury vapor. J Toxicol Clin Toxicol 41(4):339–347. https://doi.org/10.1081/clt-120022000
Gao ZZ, Pan YJ, Ma J, Li HL, Mei X, Song YG (2022) Study on the difference of curative effect of conventional mercury displacement treatment on mercury in brain and kidney. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 40(4):255–259. https://doi.org/10.3760/cma.j.cn121094-20210202-00073
Vilas GL, Aldonatti C, Martín S, de Viale LC, Ríos de Molina MC (1999) Effect of alpha lipoic acid amide on hexachlorobenzene porphyria. Biochem Mol Biol Int 47(5):815–823. https://doi.org/10.1080/15216549900201903
Anwar A, Marini M, Abruzzo PM, Bolotta A, Ghezzo A, Visconti P, Thornalley PJ, Rabbani N (2016) Quantitation of plasma thiamine, related metabolites and plasma protein oxidative damage markers in children with autism spectrum disorder and healthy controls. Free Radic Res 50(sup1):S85–s90. https://doi.org/10.1080/10715762.2016.1239821
Lonsdale D (2018) Thiamin. Adv Food Nutr Res 83:1–56. https://doi.org/10.1016/bs.afnr.2017.11.001
Lonsdale D, Shamberger RJ, Audhya T (2002) Treatment of autism spectrum children with thiamine tetrahydrofurfuryl disulfide: a pilot study. Neuro Endocrinol Lett 23(4):303–308
Flora SJS (2002) Nutritional components modify metal absorption, toxic response and chelation therapy. J Nutr Environ Med 12(1):53–67. https://doi.org/10.1080/13590840220123361
Reddy SY, Pullakhandam R, Dinesh Kumar B (2010) Thiamine reduces tissue lead levels in rats: mechanism of interaction. Biometals 23(2):247–253. https://doi.org/10.1007/s10534-009-9282-8
McGuinness G, Kim Y (2020) Sulforaphane treatment for autism spectrum disorder: a systematic review. Excli J 19:892–903. https://doi.org/10.17179/excli2020-2487
Yeh C-T, Yen G-C (2009) Chemopreventive functions of sulforaphane: a potent inducer of antioxidant enzymes and apoptosis. J Funct Foods 1(1):23–32. https://doi.org/10.1016/j.jff.2008.09.002
Klomparens EA, Ding Y (2019) The neuroprotective mechanisms and effects of sulforaphane. Brain Circ 5(2):74–83. https://doi.org/10.4103/bc.bc_7_19
Wondrak GT, Jacobson EL (2012) Vitamin B6: beyond coenzyme functions. Subcell Biochem 56:291–300. https://doi.org/10.1007/978-94-007-2199-9_15
Bjorklund G (2013) The role of zinc and copper in autism spectrum disorders. Acta Neurobiol Exp (Wars) 73(2):225–236
Abdelgadir IS, Gordon MA, Akobeng AK (2018) Melatonin for the management of sleep problems in children with neurodevelopmental disorders: a systematic review and meta-analysis. Arch Dis Child 103(12):1155–1162. https://doi.org/10.1136/archdischild-2017-314181
Lelli SM, Mazzetti MB, Martín S, de Viale LC (2016) Melatonin modulates drug-induced acute porphyria. Toxicol Rep 3:141–147. https://doi.org/10.1016/j.toxrep.2015.12.010
Omeiza NA, Abdulrahim HA, Alagbonsi AI, Ezurike PU, Soluoku TK, Isiabor H, Alli-Oluwafuyi AA (2021) Melatonin salvages lead-induced neuro-cognitive shutdown, anxiety, and depressive-like symptoms via oxido-inflammatory and cholinergic mechanisms. Brain Behav 11(8):e2227. https://doi.org/10.1002/brb3.2227
Author information
Authors and Affiliations
Contributions
All authors confirmed that they contributed to the intellectual content of this paper and have met the following three requirements: (a) significant contributions to the conception and design, acquisition of data, or analysis and interpretation of data; (b) drafting or revising the article for intellectual content; and (c) final approval of the published article.
Corresponding authors
Ethics declarations
Ethics Approval
Not applicable
Consent to Participate
Not applicable
Consent for Publication
Not applicable
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Indika, NL.R., Senarathne, U.D., Malvaso, A. et al. Abnormal Porphyrin Metabolism in Autism Spectrum Disorder and Therapeutic Implications. Mol Neurobiol 61, 3851–3866 (2024). https://doi.org/10.1007/s12035-023-03722-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-023-03722-z