Abstract
The existence of several oxalate specific binding proteins have been demonstrated in human and rat kidney. These occur in both cortical and medullary cells and are distributed mostly in the subcellular organelles. About 1/3 of the total cellular oxalate binding was localised in the inner mitochondrial membrane while the rest was in the nucleus. The purified mitochondrial oxalate binding protein (62 kDa) was composed, with a higher molar proportion, of basic amino acids, and could accumulate oxalate on incorporation into liposomes. In the nucleus, histone H1B (27.5 kDa), nuclear membrane protein (68 kDa) and nuclear pore complex protein (205 kDa) were present with oxalate binding activities. In addition, a 45 kDa calcium oxalate binding protein was identified in most of the subcellular organelles. Both mitochondrial and nuclear oxalate binding proteins and calcium oxalate binding protein have shown the kinetic properties of specificity, saturability, pH and temperature dependency, energy of activation and inhibition by substrate analogues. All oxalate binding proteins were sensitive to the transport inhibitor 4′-4′ diisothiocyano stilbene-2–2 disulphonic acid (DIDS), which is known to interact with the lysine moiety of the proteins. Calcium oxalate monohydrate (COM) crystals adsorbed oxalate binding proteins from human and rat kidney, and oxalate binding proteins isolated from human kidney stone matrix also exhibited the above kinetic properties. In experimental hyperoxaluria, all of the renal oxalate binding proteins showed enhanced oxalate binding activity with increased protein concentration. This enhanced oxalate binding activity was also attributed to increased lipid peroxidation, which correlated positively, and to decreased thiol status, which correlated negatively. A positive correlation was observed between the lipid peroxidation and both the oxalate binding activity of the in vitro peroxidised subcellular organelles and the purified protein. Similarly, in an in vivo hyperoxaluric condition, a negative correlation was observed between thiol content and both the oxalate binding activity of the peroxidised subcellular organelles and the purified protein. In the calcium oxalate crystal growth system, the oxalate binding proteins behaved either as promoters or inhibitors of the nucleation and aggregation of crystals. Following the peroxidation of the proteins, the degree of effect of the promoter protein was further stimulated while the degree of inhibition caused by the inhibitor protein further declined. Similar observations were duplicated with the proteins derived from hyperoxaluric rat kidney or kidney homogenate subjected to in vitro lipid peroxidation. The oxalate binding proteins were thought to modulate the crystallisation process in an hyperoxaluric condition similar to calcium specific binding protein modulators.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Urinary stone disease, which has plagued and intrigued human beings, existed at least 7,000 years ago, as it has been found in the pelvis, presumably in the bladder, of a mummified Egyptian [112]. Renal stone disease is estimated to occur in 2–5% of the population, and the rate of recurrence increases with age if untreated [14]. The formation of a stone within the urinary tract is not a specific disease but a culmination of the potential complications of many different metabolic disorders such as hypercalciuria, hyperoxaluria, hypocitraturia, abnormal crystallization inhibition, hyperabsorption in the intestine, excess secretion in tubular fluid, hormone imbalance and inborn errors in oxalate metabolism [40, 72, 114, 133]. Despite the development of novel means of treatment, such as dietary modifications, supplementation of citrate, magnesium oxide, antioxidants like vitamin E, lipoic acid, indigenous medicines and by surgical methods [9, 90, 93], the basic mechanism of stone formation, the identity of predictors of recurrence, and the factors involved in retention are still largely shrouded in uncertainty.
Abnormality in oxalate metabolism has been suggested for the pathogenesis of stone disease. The urinary excretion of oxalate depends on various factors such as dietary intake, endogenous synthesis, intestinal absorption, and intestinal elimination by secretion, intestinal elimination by Oxalobacter formigenes and renal secretion [45, 81, 113]. Excessive excretion of oxalate leads to calcium oxalate (CaOx) crystalluria. Oxalate can be voided freely in the urine of healthy subjects who also pass crystals with normal oxalate excretion. The question of stone formation arises only when these crystals are retained in the tubules due to their size as well as their association with the epithelium, as proposed by Finlayson and Reid in the fixed particle hypothesis [28]. The factors which facilitate the retention and further growth of the crystals may play an important role in the development of nephrolithiasis. The specific molecular processes that mediate the attachment of crystal to kidney epithelium are yet to be identified. The attachment of crystals to cells may be dependent on the specific composition and arrangement of cell surface proteins, glycoproteins, glycolipids and lipids, as well as to cell damage mediated by lipid and protein peroxidation [15, 67, 96, 124]. Membranes are the prime sites involved in the transport, uptake and binding of oxalate during the absorption process in the intestine, as well as the secretion process in renal tubules. Many of the oxalate uptake studies have been performed using membrane vesicles [78], microperfused renal tubules [121], stripped intestinal tissue as a two compartment system [37], and cultured epithelial cells [84]. All of these systems have inherent defects, as membrane vesicles and culture do not provide the same information as the intact and functional epithelia under hormonal coordination. Most of the oxalate uptake studies present data on its ion-exchange system, such as chloride, bicarbonate, proton and formate [130]. But these studies do not throw light onto the mechanism of oxalate retention. Excellent reviews are available on calculi formation mechanisms, both with the involvement of altered papillary epithelium and also in the cavities without any attachment [35], as well as the interaction of macromolecules with stone forming calcific crystals [56, 123]. All of the macromolecules implicated in the crystallization processes so far have some form of calculi binding activity, either through specific domains or anionic sites [56]. This review presents evidence for the presence of oxalate/CaOx binding proteins and CaOx crystal adsorbing proteins with oxalate binding activity in the renal cells which are thought to be involved in the retention of crystals under altered physiological conditions.
Intestinal oxalate binding protein
The hyperabsorption of dietary oxalate has been attributed to idiopathic CaOx nephrolithiasis [46]. In the rabbit, oxalate is transported through the intestine by a diffusion mechanism that is not energy but concentration dependent [27]. Oxalate absorption from the gut takes place by simple passive diffusion in humans and experimental animals [38]. In rat colon mucosa, oxalate and chloride share a common transport pathway in which chloride exchanges with bicarbonate [49]. The energy dependent net absorption of oxalate is found to be 4′,4′-diisothio-cyano stilbene 2-2 disulfonic acid (DIDS) sensitive and carrier mediated. Studies by Pinto and Paternain showed, for the first time, the presence of an oxalate transport system mediated by a carrier protein having the characteristics of a transport protein with a molecular weight of 73 kDa [83]. They speculated that two different oxalate transport systems exist, one operating at low oxalate concentration mediated by the transport protein and the other at high oxalate concentration by passive diffusion.
Pyridoxine deficiency causes hyperoxaluria in humans and animals [31]. In pyridoxine deficiency, oxalate absorption takes place with biphasic carrier mediated characteristics in which a carrier-mediated saturable component facilitates oxalate uptake from the lumen into enterocytes at low mucosal oxalate concentrations [27]. Koul et al. identified an oxalate binding protein in the brush border membrane having the kinetic properties of reversibility, saturability, temperature sensitivity and inhibition by substrate analogues [63]. The protein was induced under pyridoxine deficiency with two distinct classes of receptor sites for oxalate, one with high affinity and the other with low affinity (Table 1). The protein had a molecular weight of 79 kDa and may be involved in oxalate binding and transport in the rat intestinal brush border membrane during pyridoxine deficiency.
Red blood cell band 3 protein
The anion transporter band 3 protein is ubiquitous, not only being present in cell membranes, but also in nuclei, Golgi's complex and mitochondrial membranes [55]. It is involved in respiration, acid-base balance and is the major structural protein linking the plasma membrane to the cytoskeleton. The transport of chloride and bicarbonate, physiologically important anions, is rapid in human red blood cells (RBC) from adults and late fetuses [22], and also from adult chickens [21]. Band 3 protein has been cloned in many species [70], and the gene is located on chromosome 17. It is a 911 amino acid protein having a hydrophilic cytoplasmic domain, a hydrophobic transmembrane domain and an acidic C-terminal domain. The amino acids involved in anion exchange include lysine, arginine, histidine and glutamic acid [85]. Band 3 protein is involved in the transport of oxalate across the human RBC membrane [11]. It behaves as an oxalate exchanger in a phosphorylation dependent manner [12]. Increased arachidonic acid content of the RBC membrane of stone formers was attributed to enhanced oxalate exchange through the phosphorylation reaction. Diet induced reduction of arachidonic acid content of RBC membranes resulted in the modification of RBC oxalate transport and urinary oxalate excretion by human subjects and animals [30], suggesting that membrane phospholipid arachidonic acid content can control cellular oxalate transport by modulating protein kinases involved in the band 3 phosphorylation process [13].
Band 3 like proteins are present along the gastrointestinal tract as well as the renal tubules [4]. Immunological studies using highly purified antibodies raised against the intra-membranous domain of band 3 protein have shown specific fluorescence along the basolateral membrane's alpha intercalated cells of the collecting duct [126]. A link between RBC abnormality and renal stone formation has been suggested [19]. Patients with primary CaOx nephrolithiasis have a significantly elevated RBC oxalate exchange [10, 74]
Renal oxalate uptake and oxalate binding proteins
Renal oxalate uptake
The transcellular movement of substrates from the peritubular capillaries to the tubular fluid requires the crossing of two barriers: the basolateral plasma membrane, which is in contact with the internal milieu facing the blood supply, and the apical plasma membrane, which is in contact with the external milieu and faces the tubular fluid. The transport of oxalate across these membranes is mediated by anion exchange mechanisms.
Renal oxalate secretion is mediated by the cellular entry of oxalate in exchange for sulfate and/or bicarbonate at the basolateral membrane, followed by the cellular exit of oxalate in exchange for sulfate, bicarbonate or hydroxyl ions at the apical membrane [122]. To create a driving force for the exit of sulfate via the central luminal membrane, sulfate must first accumulate in the cell. This happens by virtue of sodium coupled sulfate transport in the luminal membrane. Using LLC-PK1 cell lines, as well as rabbit renal microvillus membrane, transport studies have suggested that chloride/oxalate exchange plays a major role in the cellular exit of oxalate at the apical membrane [54, 131]. The presence of distinct oxalate transporters in the mammalian proximal tubule has been demonstrated [33]. In addition, a sulfate/bicarbonate anion exchanger having affinity for oxalate in the rat renal cortex basolateral membrane vesicles [61], oxalate exchange for bicarbonate and sulfate in rabbit renal cortex apical membranes [53], and an oxalate/OH– exchanger [134] in rat renal proximal brush border vesicles have been demonstrated. All of these anion exchangers, including subtypes of organic anion transporters are thought to be involved in the transport of organic anions [121]. Several oxalate specific binding proteins had been identified in renal tissues in our laboratory and their kinetic properties and influence on crystal growth have been studied.
Oxalate binding proteins
Mitochondria
The presence of an oxalate binding protein had been identified in tissues such as the human kidney, where it is found in mitochondria, and rat kidney and liver [65]. Other rat tissues like heart, lung, skeletal muscle, spleen, stomach, and small and large intestinal homogenate showed no binding with oxalate. About a third of the total oxalate binding was found to be localized in the inner mitochondrial membrane. The binding of oxalate was specific and the other substrate analogues compete with it less efficiently. The binding of oxalate was rapid, reversible, dependent on oxalate concentration, and temperature sensitive. Scatchard plot analysis has shown the maximum binding capacity (Bmax) to be 49 pmol/mg protein with a dissociation (Kd) of 43 nM. Calcium had no effect on oxalate binding [65], suggesting that the binding was oxalate specific. The purified proteins from human as well as rat mitochondria showed molecular weights of 62 and 58 kDa, respectively. Both proteins had higher percentages of both basic and acidic amino acids [98]. Antibody raised to the rat protein inhibited oxalate binding and also cross-reacted with the human protein. The characteristic properties are listed in Table 1. Proteoliposomes prepared with the proteins showed an accumulation of oxalate, confirming a transport function for the protein. The uptake of oxalate in mitochondria was mediated through the dicarboxylate transport carrier [115].
Nucleus
About 2/3 of the total cellular oxalate binding activity was distributed in the kidney and liver nuclei [73]. Most of the radioactive oxalate binding was present in the histone-H1 fraction, and in particular the H1B fraction [103]. Purified protein showed oxalate binding with the characteristics of rapidity, reversibility, saturability and pH dependency. Trypsin treatment abolished oxalate binding. Scatchard plot analysis showed the characteristics of protein ligand binding (Table 1). Two distinct binding sites were found, one with high affinity and the other with low affinity for oxalate. The oxalate binding activity was inhibited by the transport inhibitors DIDS and phenyl succinate. Similarly, liver H1B was found to have a maximal oxalate binding activity with similar characteristics to renal protein [104]. This binding was not associated with calcium binding. Different tissues histone H1 fractions also exhibited oxalate binding, showing its ubiquitous nature.
About 40% of the total nuclear oxalate binding was localized in nuclear membrane. Two oxalate binding proteins were identified on the nuclear membrane, one having a molecular weight of 68 kDa [110] and the other in the nuclear pore complex having a molecular weight of 205 kDa [128]. Both oxalate binding proteins had maximal binding at pH 7.4 for both rats and humans.
All nucleated cells had oxalate uptake mechanisms. Oxalate binding and uptake were studied using, for example, intact, nucleated chicken RBC, nuclear membranes and nuclear histones. The rate of oxalate anion exchange by nucleated erythrocytes was found to be higher (K=1.24/min) than that of human RBC (K=0.5/min), but less than that of nuclei (K=1.55/min) [106]. The flux rate was pH and temperature dependent. Oxalate exchange was reduced by 35% for chicken RBCs and nuclei in the presence of sulfate, bicarbonate, phosphate and succinate, suggesting their common transport nature. Both plasma membrane and nuclear membrane showed maximal oxalate binding at pH 7.4, while for the nuclear basic protein fraction this occurred at pH 4.5, similar to renal and hepatic histones. DIDS inhibited both exchange as well as oxalate binding, suggesting that oxalate specific binding proteins are involved in the transport systems.
Calcium oxalate binding proteins
Renal calcium binding proteins have been identified in several biological systems [41]. Resnik et al. [90] reported excess excretion of calcium binding proteins in kidney stone formers. Calcium binding proteins as well as molecules like sialic acid, γ carboxy glutamic acid and phosphatidic acid allow high local concentrations of calcium inside the cell in hyperoxaluric conditions [5, 87, 88].
Using calcium-14C oxalate, the existence of CaOx binding protein has been demonstrated in several rat tissues [2]. Kidney showed the maximum binding activity among the various tissues studied. Renal medulla exhibited higher CaOx binding activity than papilla or cortex. Subcellular studies revealed the enrichment of this protein in nuclei. The purified protein has a molecular weight of 45 kDa and the kinetic properties of concentration and time dependency, optimum temperature, substrate saturability with a single affinity site with a Kd of 41 nM and Bmax of 6.5 nmol/mg protein (Table 1). This binding was inhibited by DIDS, while EGTA and ruthenium red had no effect on the binding, suggesting that the protein-oxalate binding was oxalate specific and not calcium site specific. Further lysine group might be involved in oxalate binding since DIDS is known to react with lysine-amine residues.
All of the above listed oxalate specific binding proteins, located in the different membranes of renal cells, may serve the function of carrier proteins for the transport systems since all of the transport systems exhibit energy of activation as well as transition point during temperature effect studies and inhibition by transport inhibitors. Carrier proteins of the transport system are generally constituted with lipids and they undergo phase transition at a temperature which is a function of the fatty acid composition of the lipid components [20, 91].
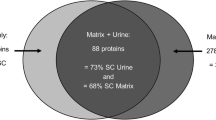
Calcium oxalate monohydrate adsorbing proteins
All urinary stones contain an organic matrix which comprises approximately 2–5% of the total stone weight. Organic matrix has been considered to be essential for the genesis and mineralization in the growth of urinary calculi during stone formation [76]. As the matrix proteins are thought to be present due to inclusion by tissue trauma or by coprecipitation along with crystals, the actual proteins in the active involvement of the crystallization process are still unknown. Thus, studies have been attempted with the proteins which were adsorbed with calcium oxalate monohydrate (COM) crystals in urine. Several proteins have been identified by this method which resemble those identified in stone matrix. [8, 26, 44, 48]. All of these proteins, such as nephrocalcin, Tomm-Horsfall glycoprotein, crystal matrix protein or prothrombin fragment F1 and bikunin, have the characteristic properties of calcium binding and inhibition of crystal growth. None have been tested for oxalate binding activity. Several oxalate-binding proteins have been identified in COM crystal adsorbed proteins as well as stone matrix proteins in our laboratory.
Human kidney
The proteins were adsorbed on CaOx crystals by allowing them to interact with triton-extracted human kidney homogenate. They were then subjected to DEAE-cellulose column chromatography and three protein peak fractions were eluted (designated as fraction I–III) according to their order of elution with increasing concentration of NaCl [100]. Among the three eluted protein peaks, the protein eluted with 0.3 M NaCl (fraction III) had the maximum oxalate binding activity of 270 pmol/mg protein at pH 4.5. The protein had no oxalate binding at pH 7.4. The purified protein had a molecular weight of 23 kDa. Amino acid analysis showed that 18% of the total molar proportion was made up of basic amino acids (lysine and arginine) while acidic amino acids accounted for only 11%. Modification of the lysine group abolished oxalate-binding activity.
In contrast to fraction III, fraction I had oxalate binding activity at pH 7.4.The purified protein had a molecular weight of 45 kDa with an activity of 280 pmol oxalate/mg protein. The protein had the kinetic properties of saturability, with a Kd of 1.96 nmol and Bmax of 200 pmol/mg protein [99].
Rat kidney
Among the different tissues, the COM adsorption of proteins derived from kidney was found to be maximum. DEAE-cellulose chromatographic fractionation yielded three proteins with oxalate binding activities, fractions I–III according to their order of elution. The molecular weight of these fractions were determined to be 74, 20 and 23 kDa, respectively. Subcellular distribution studies of these proteins revealed that the 20 kDa one was largely distributed in microsomes, that of 74 kDa in mitochondria and the 23 kDa protein in nuclei [101]. The 74 kDa protein exhibited maximum oxalate binding activity at pH 7.4, while for the 23 kDa protein this was at pH 4.5 with no activity at pH 7.4.
Human kidney stone matrix
When EDTA-extractable proteins from human kidney stone matrix were subjected to DEAE-cellulose chromatography, three protein peaks were identified with oxalate binding activity in the order of elution, fractions 1–3. Fraction 1 on further passage through a Sephadex G-200 column, separated into 48 kDa and 29 kDa proteins. The 48 kDa protein had maximum oxalate binding activity compared to the other. Both proteins exhibited the binding characteristics of renal proteins [34] (Table 2).
Effect of lipid and protein peroxidation on oxalate/CaOx binding proteins in hyperoxaluria
Mitochondrial oxalate binding
Oxalate binding was increased by 150–180% of control values in kidney and liver after subjecting them to lipid peroxidation (LPO) [107]. Renal mitochondrial oxalate binding was stimulated by promoters in the order of Fe2+>tBH>ascorbic acid>Fe3+>H2O2. The iron induced oxalate binding was inhibited by reduced glutathione, ß-mercaptoethanol, alpha tocopherol, and the hydroxyl radical scavengers histidine and mannitol. Catalase also inhibited both Fe2+and H2O2 induced enhanced oxalate binding and LPO reaction suggesting that the oxalate binding was mediated through a hydroxyl radical reaction. Increased oxalate binding had a positive correlation (r=+0.98) with LPO and a negative correlation with reduced GSH content (r=−0.80), observed during lipid peroxidation in rat kidney mitochondria [108] (Table 2). In the presence of oxidized glutathione (GSSG), peroxidized mitochondria lost 48% of their protein-SH with a concomitant threefold increase in oxalate binding activity, while control mitochondria lost only 20% of their protein-SH content with only a 0.8%-fold increase in oxalate binding activity [108]. The affinity of oxalate (Km) to GSSG treated mitochondria increased from 1×10-8 M to 0.6×10-8 M. Reduced GSH inhibited oxalate binding activity competitively (Ki=1.4×10-31 M). Urolithic kidney mitochondria showed a 30–50% increase in oxalate binding activity along with a depletion in total GSH and protein-SH as observed in vitro [79]. Similarly, feeding dehydroascorbic acid to rats also increased renal oxalate binding activity [102]. This increased activity was associated with increased LPO and decreased activities of the antioxidant enzymes superoxide dismutase (SOD), glutathione peroxidase (GPX), catalase, glutathione-S-transferase (GST) and the scavengers, reduced glutathione (GSH) ascorbic acid and vitamin E. These studies suggest that oxalate binding is regulated by the thiol status of the mitochondria. This is further supported by the following studies: (1) feeding a vitamin B6 deficient diet or calculi producing diet such as sodium glycolate or ethylene glycol in drinking water increased oxalate binding activity in mitochondria with the depletion of thiol content [79, 108]; (2) the depletion of GSH by buthionine sulfoximine in the presence of ethylene glycol feeding [80] increased oxalate binding activity. Further, oxalate binding activity was correlated negatively with the thiol status of mitochondria and calcium accumulation was also negatively correlated with thiol content; (3) ischemia reperfused kidney also showed stimulated mitochondrial oxalate binding with the depletion of thiol content [109]. A well pronounced effect was seen when ischemia reperfusion was combined with hyperoxaluria. (4) In addition, oxalate administration to rats also increased mitochondrial oxalate binding activity, and peak activity was correlated with the deposition of crystals [119].
Nuclear oxalate binding proteins
An increase in oxalate binding activity was observed when nuclear fractions were subjected to lipid peroxidation. The increased oxalate binding was associated with the depletion of -SH content. The binding activity was correlated positively with LPO and negatively with thiol content in the nuclear as well as residual membrane fractions [52]. In contrast, histone oxalate binding activity was correlated negatively with LPO (Table 2). Increased nuclear oxalate binding was also associated with experimental urolithiasis. The hyperoxaluric rat kidney nucleus exhibited a 50% increase in oxalate binding in both the residual fractions containing nuclear envelope and the histone fraction, with a concomitant increase in basal lipid peroxidation and a decrease in thiol content [53]. Hyperoxaluric rat kidney showed an increased H1 content and oxalate binding activity. The distribution of H1B was higher than in the control, showing that hyperoxaluria increased the expression of H1B. Similarly, the expression of nuclear pore complex protein was found to be dependent on the cell cycle and oxalate concentration. Maximum expression was associated with telophase [129].
Calcium oxalate binding protein
Renal CaOx binding activity was increased in rats treated only with cyclosporin A, a condition which increases lipid peroxidation leading to nephropathy [3]. A further increase was observed when combined with hyperoxaluria. This increased CaOx binding was associated with LPO as well as with a concomitant decrease in total thiol in both rat and human kidney [3]. The increase in CaOx binding activity observed in hyperoxaluria was associated with increased availability of the protein, suggesting an enhanced expression of this protein.
COM binding proteins
Proteins derived from different rat tissues show that all organs have the capacity for COM adsorption. Maximum adsorption occurred in rat kidneys and pancreas. Microsomes showed maximum adsorption in the kidney. Hyperoxaluric rat tissues showed a greater percentage of adsorption to crystals suggesting an enhanced affinity. Among COM binding proteins derived from hyperoxaluric rat kidney, both the 74 kDa and 23 kDa proteins showed an increased concentration with increased oxalate binding activity [51].
Stone matrix proteins
Similar to mitochondrial, nuclear and COM adsorbed proteins, stone matrix fractions obtained from DEAE-cellulose chromatography showed increased oxalate binding by 22%,11% and 14%, respectively, for fractions 1–3. During peroxidation, there was no loss of protein content but thiol content was drastically decreased [33] (Table 2).
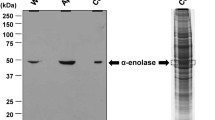
Effect of oxalate binding proteins on cCaOx crystal growth: the role of peroxidation
Differences in the effect of oxalate binding proteins on CaOx crystal growth have been noted (Table 2). Purified mitochondrial oxalate binding proteins derived from rat and human kidney showed a promoter effect on CaOx crystallization [98]. Among them, rat protein showed higher promoter activity and the antibody of this protein inhibited both oxalate binding activity and crystal growth in vitro, suggesting that the oxalate binding site plays an important role in crystal growth.
Histone oxalate binding protein also exhibited CaOx crystal growth promoter activity [103]. Histone may be involved in the initiation of crystal formation in nuclei, since calcium and calcium binding protein concentrations are also higher in the nucleus [32]. In contrast to histone oxalate binding protein, nuclear pore complex oxalate binding protein (205 kDa) showed an 87% inhibition of CaOx crystal growth in vitro [128].
Among the COM adsorbed human kidney proteins, the basic protein (23 kDa) was found to inhibit crystal growth by 82% at 0.8 µmol/l. It inhibited the nucleation and aggregation of the crystals by 6% and 28%, respectively, at 49 nmol/l. The inhibition of both nucleation and aggregation was higher at pH 5.7 than at pH 7.4. Significantly, the protein induced the formation of intertwined CaOx dihydrate crystals in a medium known to induce the formation of individual dihydrate crystals [78]. In contrast, the 45 kDa protein was found to promote crystal growth with −38.61 inhibitory units at 125 µg/l protein concentration. The protein promoted crystallization to a greater extent when modified with oxidized glutathione by promoting both nucleation and aggregation [100]. It transformed the structure of crystals from COD to COM even in the presence of citrate. The COD crystals were of 5–7 µm in size while the COM crystals were of 3–5 μm [51]. These studies suggest that the 45 kDa protein seems to be a strong candidate for promoting crystal formation, since the antibody to this protein cross reacted with the matrix stone proteins as well as urinary proteins (unpublished data).
Among the COM adsorbed rat renal proteins, the 74 kDa protein was found to be a promoter while the other protein fractions inhibited crystallization. In hyperoxaluria, the crystal growth promoting activity of the 74 kDa protein was further increased while the degree of inhibition by the 20 and 23 kDa proteins was decreased. The 74 kDa protein derived from control rats formed single COM crystals in crystal growth while the hyperoxaluric rat fraction induced the aggregation of COM crystals [51].
In order to determine whether LPO of membranes alters the binding properties of COM crystals, the kidney homogenate was subjected to lipid peroxidation and COM adsorbing proteins were isolated and studied in relation to their effect on CaOx crystal growth. A positive correlation between LPO and COM adsorption and a negative correlation between reduced glutathione and COM adsorption were observed [51]. However the peroxidized proteins did not show any alterations in the elution profile on the DEAE-cellulose column. The -SH content of the peroxidized fractions was lower than that of the control fractions, but their oxalate binding activities were increased. Peroxidized fraction I (74 kDa) promoted crystal growth to a greater extent than control fraction I (74 kDa). Peroxidized fractions II and III were found to be less inhibitory in nature compared to their control fractions. Light microscopic examination of the crystals formed in the presence of peroxidized fractions showed the formation of large aggregates of COM (Table 2). These results suggest that peroxidation may be one of the mechanisms altering the crystal growth modulatory activity of the proteins in hyperoxaluria [101].
Kidney stone matrix protein fractions eluted from the DEAE-cellulose column showed increased oxalate binding activity and correlated negatively with reduced thiol content. Fraction 1 (eluted in Tris-HCl, pH 7.4) and fraction 3 (0.3 M NaCl in buffer) showed an inhibitory effect in an in vitro crystallization system [33]. On peroxidation, fractions 1 and 3 showed a further increase in the promoting effect whereas fraction 2 showed a reduction in the inhibitory effect of nucleation and aggregation of CaOx crystals. Protein peroxidation was negatively correlated with the inhibitory activity of the protein in CaOx nucleation and aggregation. A similar promoting effect of nucleation and aggregation was seen with mitochondria and nuclei after peroxidation. These studies suggest that the peroxidation of proteins or tissue has a substantial influence on nucleation and aggregation in CaOx crystal growth.
In all of the above studies, it is very interesting to note that in the oxalate binding protein fraction eluted in buffer from DEAE-cellulose columns from human or rat kidney, COM adsorbed proteins and human stone matrix proteins behaved as strong promoters of CaOx crystal growth. The other fractions eluted in salt buffer eluate behaved as strong inhibitors. Peroxidation of the protein fractions either increased the promoting effect of the promoter proteins or decreased the inhibitory effect of the inhibitor proteins. These functional alterations are attributed directly to the thiol status of the cell. This is also reflected by urinary protein in crystal growth behaviour.
Similar to tissue proteins, hyperoxaluric rat urinary proteins also showed a different behaviour in crystal growth studies. The protein eluted in 0.3 M NaCl on DEAE-cellulose columns having a molecular weight of 45 kDa had maximaum nucleation as well as aggregation inhibitory effect. In hyperoxaluria, the excretion of this protein was increased significantly. In the crystal growth assay, the control 45 kDa protein inhibited nucleation by 75% and aggregation by 100%[111]. In contrast, it is very interesting to note that the protein derived from 28th day hyperoxaluric urine, behaved as a promoter of nucleation (−113%) and a weak inhibitor of aggregation (28%). A highly significantly negative correlation (r=−0.97) between oxalate excretion and the inhibitory effect of the 45 kDa protein was observed suggesting a modification of the protein by oxalate.
Apart from the peroxidation of proteins, the carboxylation of proteins was also found to facilitate COM crystal adsorption. Microsomal proteins were adsorbed maximally with COM crystals. On carboxylation of the renal microsomal proteins, a significant increase in the COM crystal adsorption by 2.5-fold was observed in the hyperoxaluric condition [6]. Further, carboxylated microsomes of ethylene glycol fed rats showed significant binding with CaOx. The enhanced carboxylation reaction was associated with enhanced carboxylase activity due to stimulation of the enzyme oxalate/CaOx, and lipid peroxidation [5]. The microsomal γ-glutamyl carboxylation system has been shown to be an integral membrane protein in the renal tubule [29], and enhanced γ-carboxy glutamic acid and carboxylated protein excretion has been observed in calcium nephrolithiasis [25, 77]. Both γ-carboxy glutamic acid and carboxylated proteins exert a marked enhancing effect on the nucleation rate of CaOx.
Physiological significance of oxalate binding proteins in relation to other proteins in CaOx stone formation
The interaction between CaOx crystals and tubular epithelial membrane is considered to be an essential event for the development of renal stones. Several mechanisms have been proposed for the aetiology of stone formation and crystal retention [62, 120]. The principal causative factors for the formation of calcium salt stones are attributed to the supersaturation of precipitating salts and decreased excretion of inhibitory substances such as citrate, pyrophosphate or glycosaminoglycans and inhibitory proteins which form complexes with calcium or elements such as magnesium and sodium which bind oxalate [24, 72]. The events leading to the attachment of crystals followed by retention of crystals by renal cells are still not well understood. In order for the renal cell to retain CaOx crystal, the crystal should bind to the cell surface or, primarily, to the subcellular organelles. The retention of crystals in the tubular luminal side may occur due to the size of the crystals exceeding the diameter of the nephron or increased passage time due to an abnormal nephron morphology [23, 35].
The adherence of crystals is considered to be the first event in the final phase of retention. Khan et al. identified renal cell injury as a high risk factor for CaOx nephrolithiasis [58]. Cell injury can be induced during mild hyperoxaluria, as evidenced by enzymuria and membranuria [59], in the absence of crystalluria and crystal deposition, implying that hyperoxaluria plays a significant role in membrane physiology. Our studies have established a positive correlation between free radical induced lipid peroxidation of the membrane and oxalate binding. This increased oxalate binding is negatively correlated with decreased thiol content of the membrane/protein [2, 93,79, 98, 103, 106, 108] in stone forming condition. That the involvement of free radical mediated lipid peroxidation is the major cause of tissue injury is further confirmed by our studies with the supplementation of antioxidants to urolithic rats, in which not only the LPO reaction but also CaOx deposition was prevented in the renal cells [1, 79, 93, 94, 97, 105, 116]. The role of lipid peroxidation and free radical mediated changes in renal stone formation have been further confirmed by Schied et al. [92] and Thamilselvan et al. [117, 119]. Oxalate and not CaOx is found to be more effective in inducing lipid peroxidation [95], and this effect is also substantiated by studies on the exposure of cells to a metastable concentration of oxalate along with CaOx [118]. Similarly, Koul et al. [64] have also shown a specific interaction of oxalate and not CaOx crystals in altering the cell reaction for the promotion of retention of COM crystals. In addition, oxalate is known to interact with the cellular machinery to induce the expression of several gene products such as early growth response-1, Nur 77, C-Jun, C-myc, zinc finger transcription factor, fast acting plasminogen activator inhibitor, osteopontin and platelet derived growth factor [117].
Several crystal-adhering molecules have been proposed (Table 3). The urinary epithelial cell can bind a crystal only after injury to the cell that results in the exposure of membrane phosphatidyl serine on its luminal surface. This is correlated with a corresponding increase in COM crystal attachment. The apical membrane lipid asymmetry due to the loss of cell polarity occurs by the exposure of crystals [132]. Specific sialic acid containing glycoproteins and glycolipids have been suggested as the critical determinants of the face-specific nucleation of COD crystals on the apical renal cell surface [69]. Crystal retention is attributed to alterations in the number or composition of these cell surface molecules on genetic modification by genetic alterations, cell injury or drugs in the tubular fluid [125]. Evidence has been provided for the interaction of CaOx crystals with sialic acid [47, 135], hyalouranan, chondroiton sulphate and heparan sulfate molecules, which are thought to play a major role in the attachment of crystals [127]. It has been suggested that in the absence of structural injury, sub-lethal injury mediated by ischmeia or oxalate induced lipid peroxidation reaction can expose previously concealed sialic acid residues so that they protrude into the tubular lumen in a different orientation which enable them to interact with the crystals, resulting in crystal adhesion. Moreover, the increased expression of sialic acids in the distal tubule glycoprotein as well as glycolipids with altered sialic acid linkages has been suggested for the increased nucleation and attachment of crystals [49].
Several crystal adhesion inhibitor molecules have been identified and their expression is found to increase during crystal formation [50, 60]. These molecules such as osteopontin, nephrocalcin, Tomm-Horsfall glycoprotein and bikunin inhibit crystal nucleation as well as aggregation [56, 60] (Table 3). Mild hyperoxaluria promotes the increased production of crystallisation modulators/inhibitors [49]. It has been suggested that these molecules control not only crystal nucleation, growth and aggregation but also crystal interaction with the tubular epithelium and their retention in the cell [56].
All the crystal binding molecules or adherence molecules facilitating crystal adherence to the epithelium or molecules which inhibit or modulate crystal growth behaviour are specific calcium binding molecules. They form a molecular contact with the calcium atoms on the surface of CaOx crystals [56]. All of the crystal binding molecules possess anionic sites such as carboxylate contributed by either sialic acid (glycoprotein, glycolipids) or serine, glutamate/aspartate (Tamm-Horsfall glycoprotein, bikunin, prothrombin F1); carboxylate and phosphate contributed by the membrane phospholipids of phosphatidyl serine and phosphatidyl inositol, and sulfate contributed by surface carbohydrates (glycosaminoglycans, heparan sulphate and chondroiton sulphate).
Apart from calcium binding sites, we now have evidence of oxalate specific binding molecules with similar crystal growth modulating activity. Both crystal promoting and crystal growth inhibitor proteins are known [51, 98, 100, 101, 103, 111]. They occur in the renal medulla and cortex and are differentially abundant in the subcellular organelles. All of the proteins possess lysine in the active binding site with oxalate. Lysine modification abolishes oxalate-binding activity. Oxalate binding activity is influenced by the thiol status of the cell. Oxalate itself is known to deplete the thiol status of the protein by means of inducing lipid peroxidation [1, 94, 97, 105], and peroxidised proteins modulate the crystal growth behaviour differently. Following peroxidation, the promoter activity is increased for the promoter protein while the degree of crystal growth inhibition is decreased for the inhibitor proteins, with a net result of promoting crystal growth. This situation is also reproducible in CaOx nephrolithiasis (Table 3) and these proteins are at higher concentration under this condition.
All of the oxalate specific binding proteins are distributed in the subcellular organelles. Their functions, although not defined at present, may be implicated in the movement of oxalate/CaOx from the basolateral side to the luminal side for secretion and/or from the luminal side to the lateral side for possible detoxification through macrophage mediated destruction [56]. Adhesion followed by internalisation of CaOx crystal by endocytosis has been suggested to promote crystal retention in the nephron by a positive feedback loop that favours the adhesion of additional crystals [66]. In addition to the endocytic process, the cellular depletion of thiol could contribute further for the accumulation of both calcium and oxalate [80, 93]. The increased concentration of calcium and oxalate in the cells may turn on the expression and cell proliferation by the presence of calcium and oxalate binding proteins in the nucleus and mitochondria. The oxalate binding nature of histone H1B, and the involvement of nuclear membrane pore complex oxalate binding proteins in the cell cycle reaction suggest that oxalate is not like a simple dicarboxylate molecule alone but has a specific genomic interaction to modulate its activity.
In conclusion, oxalate specific binding proteins could be involved in the initiation of renal stone formation under altered physiological conditions. In hyperoxaluria, these membrane proteins undergo lipid/protein peroxidation with the loss of sulfhydryl groups, resulting in enhanced binding with the oxalate. The peroxidised membranes/proteins have a net promoting effect of CaOx crystallisation by way of enhancing the promoter effect and decreasing the efficiency of the inhibitory effect (Fig. 1). The crystal promoting activities could be increased further by increased availability of these proteins in hyperoxaluria. The lipid peroxidation reaction could lead to fragmentation of the membrane and peroxidised membrane/protein could act as a nidus by facilitating increased binding with oxalate on the crystal, culminating in more and more deposition of crystals. This reaction might further lead to crystal incorporation into stones or/and pass along with the flow of urine.
Editorial comment (C.F. Verkoelen)
Since the mid-1980s investigators at the Department of Medical Biochemistry of the University of Madras have regularly reported on renal oxalate binding proteins in subcellular organelles such as mitochondria and nuclei. Although the proteins were purified and partially characterized, they were not identified. Oxalate has been reported to recycle across the apical membrane of renal tubular cells via anion-exchange proteins to promote the transcellular transport of chloride, But it is doubtful whether dicarboxylic acids, like oxalate, are capable of accumulating inside renal tubular cells. Renal cell oxalate handling has been engaging nephrolithiasis research for many years. The possibility cannot be excluded that oxalate binding proteins are somehow involved in the etiology of this disease. Progress can only be expected, however, after the identity and function of these proteins has been revealed.
C.F. Verkoelen
Head Stone Research Group, Department of Urology, Erasmus MC, Rotterdam, The Netherlands, and
Josephine Nefkens Institute, Room BE330, P.O.B. 1738, 3000 DR Rotterdam
References
Adhirai M, Selvam R (1997) Protection of cyclosporin A induced biochemical changes by vitamin E pretreatment in hyperoxaluric rat kidney. J Nutr Biochem 8: 32
Adhirai M, Selvam R (1998) Renal calcium oxalate binding protein: studies on its properties. Kidney Int 53: 125
Adhirai M, Sakthivel R, Selvam R (2002) Effect of cyclosporin A treatment on renal calcium oxalate binding in experimental hyperoxaluria. Mol Cell Biochem 236: 1
Alper SL, Kopito RR, Lodish HF (1987) A molecular biological approach to the study of anion transport. Kidney Int 32: 117
Angayarkanni N, Selvam R (1998) Enchanced renal vitamin-K dependent γ-glutamyl carboxylase activity in experimental urolithiasis. Eur Urol 33:116
Angayarkanni N, Selvam R(1999) Effect of γ-glutamyl carboxylation of renal microsomes on calcium oxalate monohydrate crystal binding in hyperoxaluria. Nephron 81: 342
Aronson PS(1989) The renal proximal tubules a model for diversity of anion exchangers and stilbene sensitive anion transporters. Annu Rev Physiol 51: 419
Atmani F, Opalko FJ, Khan SR (1996) Association of urinary macromolecules with calcium oxalate crystals induced in vitro in normal human urine and rat urine. Urol Res 24: 45
Backman U, Danvelson BG, Ljunghall S (1984) Renal stones—etiology, management and treatment. Almquist and Wiksell, Stockholm
Baggio B, Gambaro G, Marchini F, Cicerello E, Borsatti A (1984) Raised transmembrane oxalate flux in red blood cell in idiopathic calcium oxalate nephrolithiasis. Lancet 2: 12
Baggio B, Gambaro G, Marchini F, Cicerello F, Tenconi R, Clementi M, Borsatti A (1986) An inheritable anomaly of red cell oxalate transport in primary calcium nephrolithiasis correctable with diuretics. N Engl J Med 314: 599
Baggio B, Bordin L, Clari G(1993) Functional correlation between the Ser/Thr-phosphorylation of band 3 and band3-mediated membrane anion transport in human erythrocytes. Biochem Biophys Acta 1148: 157
Baggio B, Priante G, Brunati AM, Clari G, Bordin L(1999) Specific modulatory effect of arachidonic acid on human red blood cell oxalate transport: clinical implications in calcium oxalate nephrolithiasis. J Am Soc Nephrol 10: S381
Balaji KC, Menon M (1997) Mechanism of stone formation. Urol Clin North Am 24: 1
Bigelow MW, Wiessner JH, Kleinman JG, Mandel NS(1996) Calcium oxalate-crystal membrane interactions: dependence on membrane lipid composition. J Urol 155: 1094
Bigelow MW, Wiessner JH, Klienman JG, Mandell NS (1997)Surface exposure of phosphatidyl serine increases calcium oxalate crystals attachment. Am J Physiol 272: F55
Binder HJ (1974) Intestinal oxalate absorption. Gasteroenterology 67: 441
Bjerum PJ (1983) Identification and location of amino acid residues essential for anion transport in red cell membrane. In: Quagliarello E, Palmieri F (eds) Structure and function of membrane proteins. Elsevier, Amsterdam, p 107
Borsatti A (1991) Calcium oxalate nephrolithiasis: defective oxalate transport. Kidney Int 39: 1283
Boyce WH (1968) Organic matrix of human urinary concretions. Am J Med 45: 673
Brahm J, Wieth JO (1977) Separate pathways for urea and water and for chloride in chicken erythrocytes. J Physiol 266: 727
Brahm J, Wimberley PD (1989) Chloride and bicarbonate transport in fetal red cells. J Physiol 419: 141
Carr RJ (1953) A new theory in the formation of renal calculi. Br J Urol 26: 105
Coe FL, Parks JH, Nakagawa Y (1992) Inhibitors and promoters of calcium oxalate crystallisation : their relationship to the pathogenesis and treatment of nephrolithiasis. In: Coe FL, Favus MJ (eds) Disorders of bone and mineral metabolism. Raven Press, New York, p 757
Collette C, Bennbarrack A, Boniface H, Astre C, Herbute NP, Monnier L, Guilter J (1991) Determination of protein-bound urinary γ-carboxy glutamic acid in calcium nephrolithiasis. Clin Chim Acta 204: 43
Doyle R, Ryall Rl, Marshall VR (1991) Inclusion of proteins into calcium oxalate crystals precipitated from human urine: a highly selective phenomenon. Clin Chem 37: 1589
Farooqui S, Mahmood A, Nath R, Thind SK (1981) Nutrition and urolithiasis: Part I. Intestinal absorption of oxalate in vitamin B6 deficient rats. Indian J Expt Biol 19: 551
Finlayson B, Reid S (1978) The expectation of free and fixed particles in urinary stone disease. Invest Urol 15: 442
Friedman PA, Mitch EW, Silva P (1982) Localisation of renal vitamin K dependent γ glutamyl carboxylase to tubule cells. J Biol Chem 257: 11037
Gambaro G, Bordoni A, Nardelotto S (1996) Membrane lipid composition modulates erythrocytes and renal transport of calcium and oxalate. Nephrol Dial Transplant 11: A50
Gershoff SN (1970) Production of urinary calculi in vitamin B6 deficient male, female and castrated male rats. J Nutr 100: 117
Gilchrist JSC, Czubryt MP, Pierce GN (1994) Calcium and calcium binding proteins in the nucleus. Mol Cell Biochem 135: 79
Govindaraj A, Selvam R (2001) Increased calcium oxalate crystal nucleation and aggregation by peroxidized protein of human kidney stone matrix and renal cells. Urol Res 29: 194
Govindaraj A, Selvam R (2002) An oxalate binding protein with crystal growth promoter activity from human kidney stone matrix. Br J Urol Int 90: 336
Grases F, Costa Bauza A, Garcia Ferragut L (1998) Biopathological crystallisation: a general view about the mechanism of renal stone formation. Adv Colloid Interface Sci 74: 169
Grover PK, Stapleton AMF, Ryall RL (1999) Prothrombin gene expression in rat kidneys provide an opportunity to examine its role in urinary stone pathogenesis. J Am Soc Nephrol 10: S404
Hatch M, Vazin ND (1991) Segmental differences in intestinal oxalate transport. FASEB J 5: A1138
Hatch M, Free RW (1996) Oxalate transport across intestinal and renal epithelial. In: Khan S (ed) Calcium oxalate in biological systems. CRC Press, Boca Raton, p217
Hatch M, Free RW, Goldner AM, Earnest DL(1984) Oxalate and chloride absorption by the rabbit colon: sensitivity to metabolic and anion transport inhibitors. Gut 25: 232
Hatch M, Freel RW, Vaziril ND (1999) Regulatory aspects of oxalate secretion in enteric oxalate elimination. J Am Soc Nephrol 10: S324
Hermsdorf CL, Bronner F (1975) Vitamin D-dependent calcium binding protein from rat kidney. Biochem Biophys Acta 379: 553
Hess B (1991) The role of Tamm-Horsfall glycoprotein and nephrocalcin in calcium oxalate monohydrate crystallisation processes. Scanning Microsc 5: 689
Hess B (1994) Tamm-Horsfall glycoprotein and calcium nephrolithiasis. Miner Electrolyte Metab 20: 393
Hess B, Nakagawa Y, Coe FL (1989) Inhibition of calcium oxalate monohydrate crystal aggregation by urine proteins. Am J Physiol 257: F99
Hesse A, Schneeberger W, Engfeld S, Von Unruh GE, Sauerbruch T (1999) Intestinal hyperabsorption of oxalate in calcium oxalate stone formers: applications of a new test with (13C2)-oxalate. Am J Soc Nephrol 10: S329
Hodgkinson HJ (1977) In: Oxalic acid in biology and medicine. Academic Press, London
Hofbauer J, Fang-Kircher S, Steiner G et al. (1998) N-acetyl neuraminic acids (nana): a potential key in calculogenesis. Urol Res 26: 49
Hoyer JR (1994) Uropontin in urinary calcium stone formation. Miner Electrolyte Metab 20: 385
Iida S, Peck AB, Johnson-Tardiew J, Moriyama M, Glenton PA, Byer KJ, Khan SR (1999) Temporal changes in mRNA expression for bikunin in the kidneys of rats during calcium oxalate nephrolithiasis. J Am Soc Nephrol 10: S986
Jonassen JA, Cooney R, Kennigton L, Gravel K, Honeyman T, Scheid CR (1999) Oxalate induced changes in the viability and growth of human renal epithelial cells. J Am Soc Nephrol 10: S446
Kalaiselvi P, Selvam R (2001) Effect of experimental hyperoxaluria on renal calcium oxalate monohydrate binding proteins in the rat. Br J Urol Int 87: 110
Kannabiran K, Selvam R (1995) Induction of renal nuclear oxalate binding activity by lipid peroxidation. Med Sci Res 23: 689
Kannabiran K, Selvam R (1997) Induction of renal nuclear oxalate binding activity in experimental hyperoxaluric rats. Nephron 75: 219
Karniski LP, Aronson (1987) Anion exchage pathway for the Cl- transport in rabbit renal microvilli membranes. Am J Physiol 253: F 513
Kay MM, Bosman G, Johnson RC, Poulin J, Lawrence C, Goodman J (1994) Molecular basis of human band 3 mutation associated with increased anion transport. Exp Clin Immunogenet 11: 209
Khan SR (1997) Interactions between stone-forming calcific crystals and macromolecules. Urol Int 59: 59
Khan SR (1997) Interactions between stone-forming calclific crystals and macromolecules. Urol Int 59: 59
Khan SR, Hackett RL (1994) Renal epithelial injury: a risk factor in urolithiasis. In: Ryall R, Bais R, Marshall VR, Rofe AM, Smith LH, Walker VR (eds) Urolithiasis 2. Plenum, New York, p 29
Khan SR, Shevock PN, Hackett RL (1989) Urinary enzymes and calcium oxalate nephrolithiasis. J Urol 142: 846
Khan SR, Byer KJ,Thamilselvan S, Hackett RL, McCormack WT, Beuson NA, Vaughn KL, Erdos GW (1999) Crystal-cell interaction and apoptosis in oxalate associated injury of renal epithelial cells. J AM SocNephrol 10: S457
Knickelbein RG, Dobbins JW (1990) Sulfate and oxalate exchange for bicarbonate across the basolateral membrane of rabbit ileum. Am J Physiol 259: G807
Kok DJ, Schell-Feith EA (1999) Risk factors for crystallisation in the nephron: the role of renal development. J Am Soc Nephrol 10: S364
Koul HK, Thind SK, Nath R (1991) Oxalate binding to rat intestinal brush border membrane in pyridoxine deficiency: a kinetic study. Biochem Biophys Acta 1064: 184
Koul HK, Koul S, Sherry Fu, Santosham V, Seikhon A, Menon M (1999) Oxalate: from crystal formation to crystal retention. J Am Soc Nephrol 10: S417
Laxmanan S, Selvam R, Mahle CJ, Menon M (1986) Binding of oxalate to mitochondrial inner membranes of rat and human kidney. J Urol 135: 862
Lieske JC, Derganello S (1999) Nucleation, adhesion and internalisation of calcium containing urinary crystals by renal cells. J Am Soc Nephrol 10: S422
Lieske JC, Leonard R, Swift H, Toback FG (1996) Adhesion of calcium oxalate monohydrate crystals to anionic sites on the surface of epithelial cells. Am J Physiol 270: F192
Lieske JC, Norris R, Toback FG (1997) Adhesion of hydroxyapatite crystals to anionic sites on the surface of renal epithelial cells. Am J Physiol 273: F224
Lieske JC, Toback FG, Deganello S (2001) Sialic acid containing glycoproteins on renal cells determine nucleation of calcium oxalate dihydrate crystals. Kidney Int 60: 1784
Lux SE, Joh KM, Kopito RR, Lodish HF (1989) Cloning and characterisation of band-3, the human erythrocyte anion exchange protein (AE1). Proc Natl Acad Sci U S A 86: 9089
Matsuyama H, Kawano Y, Homasaki N (1986) Involvement of histidine residue in inorganic phosphate and phosphoenol pyruvate transport across the human erythrocyte membrane. J Biochem 99: 495
Menon M, Koul H (1992) Calcium oxalate nephrolithiasis.J Clin endocrinol Metab 74: 703
Menon M, Selvam R, Mahle CJ (1984) Binding of oxalate to inner mitochondrial membranes of rat and human kidney. In: Ryall RL, Brockis JG, Marshal VR, Finlayson B (eds) Urinary stone. Churchill Livingstone, p 258
Motola JA, Univetsky M, Molia L, Smith AD (1992) Transmembrane oxalate exchange: its relationship to idiopathic calcium oxalate nephrolithiasis. J Urol 147: 549
Moriyama MT, Glenton PA, Khan SR (2001) Expression of inter-alpha inhibitor related proteins in kidneys and urine of hyperoxaluric rats. J Urol 165: 1687
Morse RM, Resnick MI (1988) A new approach to the study of urinary macromolecules as participants in calcium oxalate crystallisation. J Urol 139: 869
Motomiya Y, Sasaki K, Mahuyama Y, Arai K, Ozono S, Hiro Y, Okajima E, Uji Y, Okabe H (1992) A study of urinary free γ-carboxy glutamic acid in patients with idiopathic urinary calcium stone. Nippon Hingokika Gakkai Zasshi 83: 2085
Murer IL, Kinne R (1980) The use of isolated membrane vesicles to study epithelial transport processes. J Membr Biol 55: 81
Muthukumar A, Selvam R (1997) Effect of depletion of reduced glutathione and its supplementation by glutathione monoester on renal oxalate retention in hyperoxaluria. Nutr Biochem 8: 445
Muthukumar A, Selvam R (1998) Role of glutathione on renal mitochondrial status in hyperoxaluria. Mol Biochem 185: 77
Ogawa Y, Miyazato T, Hatano T (1999) Importance of oxalate precursors for oxalate metabolism in rats. J Am Soc Nephrol 10: S341
Pak CYC, Resnick MI, Preminger GM (1996) Cell density-dependent calcium oxalate crystals binding to sulphated proteins at the surface of MDCK cells. In: Pak CYC, Resnick MI, Preminger GM (eds) Urolithiasis. Miller, Dallas, p 208
Pinto B, Paternain AL (1978) Oxalate transport by the human small intestine. Invest Urol 15: 502
Rabito CA (1986) Sodium co-transport processes in renal epithelial cell lines. Miner Electrolyte Metab 12: 32
Ramjee Singh M, Gaers A, Rothstein A (1980) The location of a disulphonic stilbene binding site in band 3, the anion transport protein of the red blood cell membrane. Biochem Biophys Acta 599: 127
Ramjee Singh M, Gaers A, Rothstein A (1980) The location of a disulphonic stilbene in band 3, the anion transport protein of the red blood cell membrane. Biochem Biophys Acta 599: 127
Rengarajan M, Selvam R(1987) Increased protein bound sialic acid in rat tissue in experimental urolithiasis. Med Sci Res 15: 1119
Rengarajan M, Selvam R (1989) Lipid changes in tissues in experimental urolithiasis. Indian J Biochem Biophys 27: 795
Resnick MI, Pak CYC (1990) Urolithiasis, a medical and surgical reference. WB Saunders, Philadelphia
Resnick MI, Gammon CW, Sorrell MB, Boyce WH (1980) Calcium binding proteins and renal lithiasis. Surgery 88: 239
Ryall RL, Stapleton AMF (1995) Urinary macromolecules in calcium oxalate stone and crystal matrix: good, bad or indifferent? In: Khan SR (ed) Calcium oxalate in biological systems. CRC Press, Boca Raton, p 265
Scheid C, Koul H, Adam Hill W, Luber Narod L, Kennington L, Honeyman T, Jonassen J, Menon M (1996) Oxalate toxicity in LLC-PK1 cells. Role of free radicals. Kidney Int 49: 413
Selvam R (2002) Calcium oxalate stone disease: role of lipid peroxidation and antioxidants. Urol Res 30: 35
Selvam R, Adhirai M (1997) Vitamin E pretreatment prevents cyclosporin A induced crystal deposition in hyperoxaluric rats. Nephron 75: 77
Selvam R, Bijikurien T (1987) Induction of lipid peroxidation by oxalate in experimental rat urolithiasis. J Bio Sci 12: 367
Selvam R, Bijikurien T (1991) Methionine feeding prevents kidney stone deposition by restoration of free radical mediated changes in experimental urolithiasis. J Nutr Biochem 2: 644
Selvam R, Bijikurien T (1992) Effect of citrate feeding on the free radical induced changes in experimental urolithiasis. Indian J Exp Biol 30: 705
Selvam R, Devaraj S (1997) Oxalate binding protein from the kidneys of rat and human mitochondria: studies on its properties. Indian J Biochem Biophys 34: 470
Selvam R, Kalaiselvi P (1999) Studies on calcium oxalate binding proteins Eighth European Symposium on Urolithiasis, Parma, Italy, p 339
Selvam R, Kalaiselvi P (2000) A novel basic protein from human kidney which inhibits calcium oxalate crystal growth. Br J Urol 86: 7
Selvam R, Kalaiselvi P (2001) Studies on calcium oxalate binding proteins: effect of lipid peroxidation. Nephron 88: 163
Selvam R, Kannabiran K (1993) Induction of oxalate binding by dehydroascorbic acid feeding in rat kidney. Nutr Res 13: 667
Selvam R, Kannabiran K (1996) Characterisation of nuclear oxalate binding protein of rat and human kidney. J Urol 156: 237
Selvam R, Prasannalakshmi V(1996) Occurrence of histone-related oxalate binding in rat liver nucleus. Mol Cell Biochem 156: 93
Selvam R, Ravichandran V(1993) Restoration of tissue antioxidants and prevention of renal stone deposition in vitamin B6 deficient rats fed with vitamin E or methionine. Indian J Exp Biol 31: 882
Selvam R, Saradha Devi V(1998) Enhanced oxalate transport in nucleated red blood cells. Eur Urol 33: 124
Selvam R, Sridevi D (1991) Induction of oxalate binding by lipid peroxidation in rat kidney mitochondria. Biochem Int 24: 857
Selvam R, Sridevi D (1996) Oxalate binding to rat kidney mitochondria: induction by oxidised glutathione. Indian J Biochem Biophys 33: 62
Selvam R, Vijaya A (2000) Effect of renal ischemia reperfusion on calcium oxalate retention. Indian J Med Res 111: 62
Selvam R, Angayarkanni N, Vijaya R (1996) Nuclear oxalate binding proteins of rat liver nuclei—a preliminary report. Med Sci Res 24: 267
Selvam R, Balakrishnan S, Kalaiselvi P (2002) Effect of hyperoxaluria on the inhibitory activity of a 45 kDa urinary protein. Nephron 90: 206
Shattock SG (1905) A prehistoric or predynastic Egyptian calculus.Trans Pathol Soc London 56: 279
Sidhu H, Schmidt ME, Cornelius JG, Thamilselvan S, Khan SR, Hesse A, Peck AB (1999) Direct correlation between hyperoxaluria/oxalate stone disease and the absence of the gastrointestinal tract dwelling bacterium Oxalobacter formigens: possible prevention by gut recolonisation or enzyme replacement therapy. J Am Soc Nephrol 10: S334
Smith LH (1990) The pathophysiology and medical treatment of urolithiasis.Semin Nephrol 10: 31
Strzelecki T, Menon M (1986) The uptake of oxalate by rat liver and kidney mitochondria. J Bio Chem 261: 12197
Thamilselvan S, Selvam R (1997) Effect of vitamin E and mannitol on renal calcium oxalate retention in experimental nephrolithiasis. Indian J Biochem Biophys 34: 319
Thamilselvan S, Hackett RL, Khan SR (1997) Lipid peroxidation in ethylene glycol induced hyperoxaluria and calcium oxalate nephrolithiasis. J Urol 157: 1059
Thamilselvan S, Hackett RL, Khan SR (1999) Cells of proximal and distal tubular origin respond differently to challenges of oxalate and calcium oxalate crytals. J Am Soc Nephrol 10: S452
Thamilselvan S, Byer KJ, Hackett RL, Khan SR (2000) Free radicals scavengers catalase, superoxide dismutase provide protection and MDCK cells. J Urol 164: 224
Tiselius HG, Hojgaard I (1999) Some aspects of the intratubular precipitation of calcium salts. J Am Soc Nephrol 10: S371
Ullrich KJ (1994) Specificity of transporters for 'organic anions' and 'organic cations' in the kidney. Biochem Biophys Acta 1197: 45
Verkoelen CF, Romijn JC (1996) Oxalate transport and calcium oxalate renal stone disease. Urol Res 24: 183
Verkoelen CF, Schepers MSJ (2000) Changing aspects with aetiology of renal stones. Curr Opin Urol 10: 539
Verkoelen CF, Nauder Boom BG, Houts Muller AB, Schroder FH, Remijn JC (1998) Increased calcium oxalate monohydrate crystals binding to injured renal tubular epithelial cells in culture. Am J Physiol 274: F958
Verkoelen CF, Van Der Boom BG, Kok DJ, Schroder FH, Romijn JC (1999) Attachment sites for particles in the urinary tract. J Am Soc Nephrol 10: S430
Verkoelen CF, Van Der Boom BG, Kok DJ, Romijn JC (2000) Sialic acid and crystal binding. Kidney Int 57:1072
Verlander JW, Madson KM, Low PS, Allen DP, Tisher CC (1988) Immunocytochemical localisation of band 3 protein in the rat collecting duct. Am J Physiol 255: 115
Vijaya R, Selvam R (1999) Characterisation of nuclear pore complex oxalate binding protein gp210. Eighth European Symposium on Urolithiasis, Parma, Italy, p 213
Vijaya R, Kannabiran K, Selvam R (1999) Oxalate induced and cell cycle dependent expression of nuclear pore complex oxalate binding protein gp210. Biochem Biophys Res Comm 266: 72
Wandzilak TR, Calo L, Borsalti A, William HE (1992) Oxalate transport in cultures porcine renal epithelial cells. Urol Res 20: 341
Wareing M, Green R (1994) Effects of formate and oxalate on fluid reabsorption from the proximal convoluted tubules of the anaesthetised rat. J Physiol 447: 347
Weissner JH, Hasegawa AT, Hung LY, Mandel GS, Mandel NS (2001) Mechanisms of calcium oxalate crystal attachment to injured renal collecting duct cells. Kidney Int 59: 637
Williams HE, Smith LH (1968) Disorders of oxalate metabolism.Am J Med 45: 715
Yamakawa K, Kawamma J(1990) Oxalate: OH exchanger across rat renal cortical brush border membrane. Kidney Int 37: 1105
Yoshimura K, Yoshioka T, Miyako O, Honda M, Koide T, Okuyama A (1998) Investigation of the possible role of sialic acid in calcium oxalate urolithiasis. Eur Urol 33: 111
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Selvam, R., Kalaiselvi, P. Oxalate binding proteins in calcium oxalate nephrolithiasis. Urol Res 31, 242–256 (2003). https://doi.org/10.1007/s00240-003-0316-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-003-0316-3