Abstract
Missense mutations of the V600E type constitute the vast majority of tumor-associated somatic alterations in the v-RAF murine sarcoma viral oncogene homolog B1 (BRAF) gene. Initially described in melanoma, colon and papillary thyroid carcinoma, these alterations have also been observed in primary nervous system tumors albeit at a low frequency. We analyzed exon 15 of BRAF spanning the V600 locus by direct sequencing in 1,320 adult and pediatric tumors of the nervous system including various types of glial, embryonal, neuronal and glioneuronal, meningeal, adenohypophyseal/sellar, and peripheral nervous system tumors. A total of 96 BRAF mutations were detected; 93 of the V600E type and 3 cases with a three base pair insertion between codons 599 and 600. The highest frequencies of BRAF V600E mutations were found in WHO grade II pleomorphic xanthoastrocytomas (42/64; 66%) and pleomorphic xanthoastrocytomas with anaplasia (15/23; 65%), as well as WHO grade I gangliogliomas (14/77; 18%), WHO grade III anaplastic gangliogliomas (3/6) and pilocytic astrocytomas (9/97; 9%). In pilocytic astrocytomas BRAF V600E mutation was strongly associated with extra-cerebellar location (p = 0.009) and was most frequent in diencephalic tumors (4/12; 33%). Glioblastomas and other gliomas were characterized by a low frequency or absence of mutations. No mutations were detected in non-glial tumors, including embryonal tumors, meningiomas, nerve sheath tumors and pituitary adenomas. The high mutation frequencies in pleomorphic xanthoastrocytomas, gangliogliomas and extra-cerebellar pilocytic astrocytomas implicate BRAF V600E mutation as a valuable diagnostic marker for these rare tumor entities. Future clinical trials should address whether BRAF V600E mutant brain tumor patients will benefit from BRAF V600E-directed targeted therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
BRAF mutations have been detected in a high proportion of melanoma and papillary thyroid carcinoma and are also frequent in various other cancers, in particular colorectal carcinoma, carcinoma of the biliary tract and ovarian cancer [5, 27, 36]. A comprehensive overview of BRAF mutations can be found in the Catalogue of Somatic Mutations in Cancer (http://www.sanger.ac.uk/cosmic) [11]. The vast majority of mutations affects a mutational hot spot at amino acid position 600 and is characterized by the exchange of valine by glutamate (referred to as BRAFV600E). Earlier studies of human brain tumors revealed absence of BRAFV600E or only single instances of BRAFV600E mutations in glioblastoma (GBM) [2, 8, 14, 18, 21] and in astrocytic, oligodendroglial and ependymal tumors of WHO grades II and III [8, 18]. Recent findings, however, suggest that certain types of mostly low grade and pediatric brain tumors may have higher rates of BRAF alterations. In particular, pilocytic astrocytomas often carry BRAF aberrations, though more commonly in the form of oncogenic fusion genes like KIAA1549:BRAF rather than BRAFV600E missense mutations [19, 23, 32]. Recently, BRAFV600E mutations have been detected in small series of pediatric gangliogliomas, pleomorphic xanthoastrocytomas, desmoplastic infantile gangliogliomas and atypical teratoid/rhabdoid tumors as well as pediatric GBM, anaplastic astrocytomas and diffuse astrocytomas [6, 12, 17, 34].
BRAF is a member of the RAS/RAF/MEK/ERK kinase pathway. The BRAF V600E mutation is thought to mimic phosphorylation of the activating amino acids T599 and S602, thereby leading to constitutive activation of the protein [5]. Such activation affects cell proliferation, differentiation and survival. Several inhibitors targeting the RAS/RAF/MEK/ERK signaling cascade are currently in clinical trials for various malignancies [29]. Furthermore, several small molecules specifically inhibiting the function of BRAF V600E have been developed and are currently under investigation. The small molecule inhibitor of BRAF V600E PLX4032 (RG7204) has been shown to prolong survival of mice bearing BRAF V600E melanoma xenografts [39] and currently is in phase III clinical testing. Similarly, the small molecule inhibitor GDC-0879 has been demonstrated to inhibit tumor growth of melanoma xenografts carrying BRAF V600E [15]. Thus, it is of major clinical interest to determine the frequency and distribution of BRAF V600E mutations across various types of central and peripheral nervous system tumors to identify those tumor entities that might potentially benefit from BRAF V600E targeted therapy. We therefore analyzed a comprehensive series of 1,320 primary pediatric and adult nervous system tumors for the presence of the BRAF V600E mutation.
Materials and methods
Tumor specimens
DNA samples from archival human nervous system tumor tissue specimens diagnosed at the Departments of Pathology/Neuropathology at the Universities of Heidelberg, Muenster, Magdeburg, Duesseldorf, the Burdenko Neurosurgical Institute in Moscow, the Radboud University Nijmegen Medical Centre, Nijmegen, and Massachusetts General Hospital, Boston, were analyzed. All tumors were diagnosed according to the revised WHO 2000 and 2007 classifications [26]. In total, 1,384 DNA samples were investigated. Of these, BRAF mutation analysis was successful in 1,320 samples (95%); the remaining 64 DNA samples were either not amplifiable by PCR or did not yield evaluable sequences. All samples were analyzed in an anonymous manner as approved by the local ethics committees at the participating institutions.
The series included 97 pilocytic astrocytomas WHO grade I (PA I), 64 pleomorphic xanthoastrocytomas WHO grade II (PXA II), 23 pleomorphic xanthoastrocytomas with anaplasia (aPXA), 57 diffuse astrocytomas WHO grade II, 58 anaplastic astrocytomas WHO grade III (A III), 115 primary glioblastomas WHO grade IV (GBM), 18 secondary glioblastomas WHO grade IV (secGBM, based on clinical information of previously resected lower grade lesion), 15 giant cell glioblastomas WHO grade IV (gcGBM), 16 gliosarcomas WHO grade IV (GS), 64 oligodendrogliomas WHO grade II (O II), 70 anaplastic oligodendrogliomas WHO grade III, 41 oligoastrocytomas WHO grade II, 51 anaplastic oligoastrocytomas WHO grade III, 5 gliomatosis cerebri, 3 subependymal giant cell astrocytomas WHO grade I (SEGA), 94 ependymomas WHO grade II, 52 anaplastic ependymomas WHO grade III, 4 myxopapillary ependymomas WHO grade I, 2 subependymomas WHO grade I, 141 medulloblastomas WHO grade IV, 29 supratentorial primitive neuroectodermal tumors WHO grade IV, 14 atypical teratoid/rhabdoid tumors WHO grade IV (AT/RT), 77 gangliogliomas WHO grade I (GG I), 6 anaplastic gangliogliomas WHO grade III (GG III), 8 gangliocytomas, 9 central neurocytomas WHO grade II, 4 desmoplastic infantile gangliogliomas or astrocytomas WHO grade I, 4 dysembryoplastic neuroepithelial tumors WHO grade I, 14 schwannomas WHO grade I, 42 meningiomas WHO grade I including the meningothelial and transitional variants, 16 atypical meningiomas WHO grade II, 11 anaplastic meningiomas WHO grade III, 2 hemangiopericytomas WHO grade II, 18 malignant peripheral nerve sheath tumors, 9 neurofibromas, 5 craniopharyngiomas, 4 capillary hemangioblastomas WHO grade I and 58 pituitary adenomas.
The BRAF mutation status of 64 PA I has been reported in a previous study [7]. Six of the PXA II samples in this study are also included in a separate study by D. Dias-Santagata et al. (manuscript in preparation). Pediatric tumors were defined as lesions operated in patients younger than 18 years. Diagnoses of the 1,320 tumors are summarized in Table 1. Available data on tumor location of PA I, PXA (both PXA II and aPXA) and GG (both GG I and GG III) is summarized in Table 2.
In 16 tumors (6 GG I, 1 GG III, 3 PXA II, 1 aPXA, 1 O II, 1 PA I, 1 secGBM, 1 gcGBM and 1 GS) with BRAFV600E mutation, peripheral blood samples were available for the investigation of constitutive (germline) or somatic (tumor-associated) origin of the BRAF alterations.
DNA from the melanoma cell line A375 with a previously described BRAF V600E mutation served as positive control [39]; HEK293T cells served as wild-type control.
PCR amplification and direct sequencing
Older publications often referred to codon 600 mutations as codon 599 mutations. In 2003, the BRAF sequence was updated with the insertion of 3 bp in the coding sequence resulting in a new number of the hot-spot codon (600 instead of 599). In the following, we refer to RefSeq DNA: NM_004333. A fragment of 173 bp length including codon 600 of BRAF was amplified using 60 ng each of the sense primer BRAFf TGCTTGCTCTGATAGGAAAATG and the antisense primer BRAFr CCACAAAATGGATCCAGACA. PCR using standard buffer conditions, 100 ng of DNA and GoTaq DNA Polymerase (Promega, Madison, USA) employed 35 cycles with denaturing at 95°C for 30 s, annealing at 56°C for 30 s and extension at 72°C for 40 s in a total volume of 25 μl. Two microliters of the PCR amplification product were submitted to the sequencing reaction using the BigDye Terminator v3.1 Sequencing Kit (Applied Biosystems, Foster City, USA). 25 cycles were performed employing 12 ng of the sense primer BRAFf, with denaturing at 95°C for 30 s, annealing at 56°C for 15 s and extension at 60°C for 240 s. For selected cases, a second round of sequencing analysis was performed using the antisense primer BRAFr and the sequencing reaction conditions as described above. Sequences were determined using a semiautomated sequencer (ABI 3100 Genetic Analyzer, Applied Biosystems, Foster City) and the Sequence Pilot version 3.1 software (JSI-Medisys, Kippenheim, Germany). For analysis confirmation, 30 BRAF-mutated and 30 wild-type cases were re-analyzed with a second set of primers (sense primer BRAFf_confirm TCATAATGCTTGCTCTGATAGGA and antisense primer BRAFr_confirm GGCCAAAAATTTAATCAGTGGA) generating a 224-bp fragment at the same PCR conditions. All cases demonstrated the same results as in first analysis.
Statistical analysis
Student’s t test was used to examine the relation of absence or presence of BRAF V600E mutation with age, two-tailed Fisher’s exact test was used to examine the relation of BRAF V600E mutation and gender for distinct tumor groups. Two-tailed Fisher’s exact test was used to examine associations of tumor location and BRAF mutation status for cerebellar versus extra-cerebellar PA I and for temporal versus non-temporal supratentorial GG.
Results
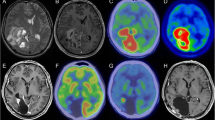
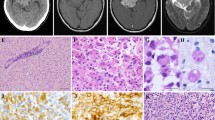
A total of 93 BRAF V600E mutations were detected among the 1,320 tumors with evaluable sequencing results. All mutations were heterozygous with one remaining wild-type allele (Fig. 1). In each mutant case, an exchange of T to A at c.1799 was observed (c.1799T>A). Matched constitutive (leukocyte) DNA was available from 16 patients with BRAF V600E mutant tumors. None of the 16 constitutive DNAs carried a BRAF V600E, thus indicating an acquired (somatic) origin of the mutation in the corresponding tumors. In addition to the 93 BRAF V600E mutations, one PXA II was found that carried a three base pair insertion (c.1797_1798insACA) between codon 599 and 600 coding for threonine (p.T599_V600insT). Two PA I cases also harbored a three base pair insertion coding for threonine between codon 599 and 600, both of which have previously been described in detail elsewhere [7]. The frequencies of BRAF V600E mutations in different brain tumor entities are listed in Table 1. Notably, frequent BRAF V600E mutations were observed in PXA II (42/64; 66%), aPXA (15/23; 65%), GG I (14/77; 18%), GG III (3/6) and PA I (9/97; 9%). In other types of gliomas, BRAF V600E mutations were less common and restricted to GBM (2/115; 2%), A III (2/58; 3%), O II (1/64; 2%) gcGBM (1/15; 7%), secGBM (1/18; 6%) and GS (1/16; 6%). One instance of BRAF V600E mutation each was identified among the few available cases of gliomatosis cerebri (N = 5) and SEGA (N = 3). All other investigated nervous system tumors lacked BRAF codon 600 alterations.
For lesions with frequent BRAF mutations and sufficiently high case numbers, an analysis of mutation frequency by patient age was performed (Fig. 2). Student’s t test was used to calculate statistically significant differences of mean age. No significant differences were seen for PA I, GG I and PXA II. For aPXA, BRAF V600E mutation is highly significantly associated with younger patient age; patients with BRAF-mutant tumors had a mean age of 18 years while patients with BRAF-wild-type tumors had a mean age of 38 years (p = 0.001). In fact, all 10 pediatric aPXA had BRAF V600E mutations (100%), while the mutation frequency in adult patients was merely 38% (Table 1). Likewise, BRAF mutations in GBM and A III of this series all occurred in pediatric patients, with 2/36 pediatric GBM and 2/6 pediatric A III carrying BRAF V600E mutations. No association between BRAF mutation and gender was observed (data not shown).
BRAFV600E mutation in relation to age. No significantly different age distribution was observed for pilocytic astrocytoma (a), ganglioglioma WHO grade I (b) and pleomorphic xanthoastrocytoma WHO grade II (c). For pleomorphic xanthoastrocytoma with anaplasia the presence of BRAFV600E was significantly associated with younger patient age (d; p = 0.001)
Data on BRAF V600E status and tumor location of PA I, GG and PXA and is given in Table 2. A strong association of tumor location and BRAF V600E mutation was observed in PA I. Eight of 41 (20%) extra-cerebellar PA I were BRAF V600E-mutant, whereas only 1 of 53 (2%) cerebellar PA I had this alteration (p = 0.009 via Fisher’s exact test). Among extra-cerebellar PA I, highest rates were observed in diencephalic tumors with 4 of 12 (33%) of tumors being BRAF V600E-mutant. For GG, BRAF V600E mutations were more frequent in temporal location (11/39; 28%), but no significant differences were observed compared to non-temporal supratentorial tumors (3/18; 17%, p = 0.51). Location data of PXA was only available for 29 cases. Among these, an association of location and mutation frequency was not evident.
Additional clinical and molecular data of the six adult cases with BRAF V600E mutation not diagnosed as GG, PXA or PA I are summarized in Table 3. The location was recorded in three cases, all of which affected the temporal lobe. Of note, the gcGBM occurred in a 22-year-old patient, presented as a cystic lesion with adjacent tumor nodule and reportedly had progressed from a WHO grade II astrocytoma not diagnosed in any of the participating institutions. The SEGA case presented in a 59-year-old patient, without other evidence of tuberous sclerosis and with the unusual occurrence of a WHO grade II ependymoma at the same tumor location 19 months after resection. The BRAF V600E mutant O II lacked isocitrate dehydrogenase 1/2 (IDH1/2) gene mutation and loss of heterozygosity of 1p/19q, both molecular aberrations that are highly characteristic for oligodendroglial tumors.
Discussion
Recent data from a phase I clinical trial with the specific inhibitor PLX4032 in patients with metastasized BRAF V600E mutant malignant melanoma nourishes the hope that BRAF V600E mutation may become a prime target of cancer therapy in the near future [10]. The present study aimed at identifying subsets of nervous system tumors carrying this specific genetic alteration that might be feasible targets for future clinical trials. We demonstrate that two-thirds of PXA, including classical (WHO grade II) tumors and PXA with anaplasia, are characterized by this specific BRAF point mutation. This corroborates recent observations in smaller tumor series that demonstrated BRAF V600E mutations in few cases of PXA [6, 12, 30]. PXA is a relatively rare tumor entity, accounting for less than 1% of all astrocytic tumors. It typically affects children and young adults and is mostly located in the superficial cortex often extending into the adjacent leptomeninges. It has relatively distinct morphological features, namely pleomorphic and lipidized astrocytic cells, eosinophilic granular bodies, a variably dense reticulin network and prominent perivascular lymphocytic infiltrates [26]. The most frequent genetic alteration of PXA described to date is a homozygous deletion of 9p21.3, including the tumor suppressor gene CDKN2A (p16INK4a), which was detected in 6 of 10 (60%) tumors investigated by array-based comparative genomic hybridization [38]. There may well be a functional connection between CDKN2A deletion and the high BRAF mutation rate detected in this study. It has previously been demonstrated that BRAF V600E mutation results in an induction of p16INK4a and that this leads to senescence in human melanocytic nevi [28]. Moreover, expression of activated BRAF alone is not sufficient for gliomagenesis in a mouse model, but the combination of activated BRAF with CDKN2A loss is transforming [33]. Thus, it seems possible that in human PXA, BRAF V600E induced senescence may be circumvented by concomitant homozygous deletion of CDKN2A. A similar connection may exist for other pediatric malignant astrocytomas where 5 of 7 BRAF V600E mutated tumors have been shown to carry concomitant homozygous deletions of CDKN2A [34]. In one PXA II and two PA I of this series, we observed a different type of BRAF mutation resulting in an insertion of threonine between amino acid position 599 and 600 of BRAF. Analogous insertions have previously been described in PA I as well as one tubular adenocarcinoma of the pancreas and were shown to mimic the activating BRAF V600E mutation functionally [7, 20, 24].
GG was the second most frequently mutated CNS tumor entity. In our cohort, the BRAF mutation frequency was slightly lower than what was expected from a previous investigation of pediatric GG in which 9 of 18 GG (50%) harbored BRAF V600E mutations [6]. Still, our data of a large cohort demonstrate that this genetic aberration is moderately frequent (~20%) in this tumor type and is also found in adult GG. In addition, we show that GG III may have an increased rate of mutations with 3 of 6 tumors in our series carrying mutations. PXA and GG show widely overlapping clinical and histological features and diagnostic distinction may occasionally be difficult. Interestingly, there is ample evidence of transitional tumors with either focal or intermixed features of both PXA and GG [13, 22, 25, 31, 35, 37]. Thus, it seems possible that a subgroup of GG is characterized by BRAF V600E mutation and may be more closely related to PXA. Future morphological studies on GG with BRAF mutations may clarify this issue. Intriguingly, a fraction of around 10% of GG is also characterized by a homozygous deletion of 9p21 including CDKN2A, further indicating a possible relation to PXA [6].
BRAF fusion is the main activating alteration of the RAS/RAF/MEK/ERK kinase pathway in PA I [19, 20, 32]. BRAFV600E mutations and BRAF fusion are expected to represent mutually exclusive events. Several studies have shown BRAF fusion to be substantially more frequent in cerebellar than in extra-cerebellar PA I [12, 16, 17, 19, 23]. Our data indicate that contrary to BRAF fusion, BRAFV600E is significantly more frequent in extra-cerebellar PA I (~20%) than in cerebellar tumors (~2%). While the reason for this is not clear, this observation may have clinical consequences concerning future patient stratification. While most PA I are curable through surgery, outcome may be worse when neuroanatomic realities preclude complete surgical resection as may frequently be the case for deep-seated midline tumors of the diencephalon and brain stem [3]. We here demonstrate that extra-cerebellar PA I and especially diencephalic tumors have frequent BRAFV600E mutations and thus represent feasible targets for future clinical trials targeting this specific alteration. The association of BRAFV600E and tumor location may further in part explain our slightly higher BRAFV600E mutation rate compared to previous reports [12, 17, 19, 32, 40] as a relatively high proportion of extra-cerebellar PA I were analyzed in this study.
All other investigated CNS tumor entities were characterized by low BRAF codon 15 mutation frequencies or completely lacked this alteration. As reported before, our data corroborate that BRAF V600E mutation is rare or absent in adult high-grade glioma [2, 8, 14, 18, 21]. Furthermore, no BRAF codon 600 alteration was detected in tumors of the meninges and the PNS. As in a previous study, no BRAF mutations were detected among 58 pituitary adenomas [9]. A recent study detected BRAF V600E mutations in 3/3 unusual cases of AT/RT [6]; all three tumors had evolved from lower grade lesions, one from a GG, two from PXA II, two of these cases have been described in detail elsewhere [1, 4]. In line with additional cases investigated by Dougherty and colleagues [6], no BRAF codon 600 hot-spot mutations were observed in 14 AT/RT that had typical clinical courses.
As further discussed below, younger patient age is associated with BRAF mutation in certain tumor types. Even in pediatric tumors, BRAF mutations were detected almost exclusively in PXA, GG and PA I. The only exceptions were pediatric GBM and A III, with 2 of 36 GBM and 2/6 A III showing a BRAF V600E mutation. This is in line with a recent report on high BRAF V600E mutation rates in pediatric high-grade glioma [34]. Of note, in the almost 300 remaining pediatric brain tumors in our series the BRAF V600E mutation was absent. A further observation corroborating the role of patient age and BRAF mutation status comes from our cohort of aPXA patients, in which all pediatric cases had the V600E mutation, whereas adult patients harbored this mutation in only 38% of the cases. The reason for this is not clear, although it is possible that the adult group may have included other brain tumors typically occurring at older age, with sometimes strongly overlapping morphology, especially GBM, gcGBM or GS.
Previous investigations have observed infrequent mutations at the codon 600 hot-spot region of BRAF in adult gliomas, notably in 1 of 12 O II and 1 of 14 GS [18, 21]. We also detected 6 BRAF V600E mutant adult gliomas of diverse histologies. As listed in Table 3, the BRAF mutated O II, gcGBM and SEGA demonstrated somewhat unusual clinical and molecular characteristics and some of these lesions may well represent unrecognized PXA. To resolve this issue, future studies should follow the clinical course of adult BRAF-mutant glioma patients to see if these lesions behave more like a PXA than a malignant (WHO grade III or IV) glioma.
The high mutation rates in PXA, GG and extra-cerebellar PA I implicate BRAF V600E mutation as a valuable diagnostic marker. Detection of a BRAF V600E mutation in a pleomorphic glioma should prompt consideration of PXA. In case of a high-grade glioma with an unusually benign clinical course BRAF V600E mutation may indicate misclassification of a PXA or GG. Further, BRAF V600E may aid in the differentiation of extra-cerebellar PA I and diffuse astrocytoma WHO grade II as has previously been demonstrated for BRAF fusion [23]. Caution has to be taken though, as BRAF V600E has been detected in several cases of pediatric diffuse astrocytomas WHO grade II [34] and is likely less tumor type specific than BRAF fusion.
In summary, we demonstrate high mutation frequencies of BRAF V600E in distinct subtypes of brain tumors: most notably, the majority of PXA are characterized by this specific genetic alteration. The high mutation frequencies in PXA, GG and extra-cerebellar PA I make BRAF V600E alteration a valuable diagnostic marker for these rare tumor entities. Following PA I, PXA is the next tumor entity predominantly occurring in children and young adults that is characterized by very frequent alterations in the RAS/RAF/MEK/ERK kinase pathway. Further analysis of PXA without BRAF V600E will clarify whether the RAS/RAF/MEK/ERK kinase pathway is activated by other means in the remaining tumors and whether PXA represents a “single pathway disease” as has been postulated for PA I. Although PXA, GG and extra-cerebellar PA I constitute rare brain tumor types, future clinical trials should address whether BRAF V600E mutant tumor patients will benefit from BRAF V600E-directed targeted therapies.
References
Allen JC, Judkins AR, Rosenblum MK et al (2006) Atypical teratoid/rhabdoid tumor evolving from an optic pathway ganglioglioma: case study. Neuro Oncol 8:79–82
Basto D, Trovisco V, Lopes JM et al (2005) Mutation analysis of B-RAF gene in human gliomas. Acta Neuropathol 109:207–210
Bowers DC, Gargan L, Kapur P et al (2003) Study of the MIB-1 labeling index as a predictor of tumor progression in pilocytic astrocytomas in children and adolescents. J Clin Oncol 21:2968–2973
Chacko G, Chacko AG, Dunham CP et al (2007) Atypical teratoid/rhabdoid tumor arising in the setting of a pleomorphic xanthoastrocytoma. J Neurooncol 84:217–222
Davies H, Bignell GR, Cox C et al (2002) Mutations of the BRAF gene in human cancer. Nature 417:949–954
Dougherty MJ, Santi M, Brose MS et al (2010) Activating mutations in BRAF characterize a spectrum of pediatric low-grade gliomas. Neuro Oncol
Eisenhardt AE, Olbrich H, Roring M et al (2010) Functional characterization of a BRAF insertion mutant associated with pilocytic astrocytoma. Int J Cancer
El-Habr EA, Tsiorva P, Theodorou M et al (2010) Analysis of PIK3CA and B-RAF gene mutations in human astrocytomas: association with activation of ERK and AKT. Clin Neuropathol 29:239–245
Ewing I, Pedder-Smith S, Franchi G et al (2007) A mutation and expression analysis of the oncogene BRAF in pituitary adenomas. Clin Endocrinol (Oxf) 66:348–352
Flaherty KT, Puzanov I, Kim KB et al (2010) Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med 363:809–819
Forbes SA, Bhamra G, Bamford S et al (2008) The catalogue of somatic mutations in cancer (COSMIC). Curr Protoc Hum Genet, chap 10, unit 10 11
Forshew T, Tatevossian RG, Lawson AR et al (2009) Activation of the ERK/MAPK pathway: a signature genetic defect in posterior fossa pilocytic astrocytomas. J Pathol 218:172–181
Furuta A, Takahashi H, Ikuta F et al (1992) Temporal lobe tumor demonstrating ganglioglioma and pleomorphic xanthoastrocytoma components. Case report. J Neurosurg 77:143–147
Hagemann C, Gloger J, Anacker J et al (2009) RAF expression in human astrocytic tumors. Int J Mol Med 23:17–31
Hoeflich KP, Herter S, Tien J et al (2009) Antitumor efficacy of the novel RAF inhibitor GDC-0879 is predicted by BRAFV600E mutational status and sustained extracellular signal-regulated kinase/mitogen-activated protein kinase pathway suppression. Cancer Res 69:3042–3051
Horbinski C, Hamilton RL, Nikiforov Y et al (2010) Association of molecular alterations, including BRAF, with biology and outcome in pilocytic astrocytomas. Acta Neuropathol 119:641–649
Jacob K, Albrecht S, Sollier C et al (2009) Duplication of 7q34 is specific to juvenile pilocytic astrocytomas and a hallmark of cerebellar and optic pathway tumours. Br J Cancer 101:722–733
Jeuken J, van den Broecke C, Gijsen S et al (2007) RAS/RAF pathway activation in gliomas: the result of copy number gains rather than activating mutations. Acta Neuropathol 114:121–133
Jones DT, Kocialkowski S, Liu L et al (2008) Tandem duplication producing a novel oncogenic BRAF fusion gene defines the majority of pilocytic astrocytomas. Cancer Res 68:8673–8677
Jones DT, Kocialkowski S, Liu L et al (2009) Oncogenic RAF1 rearrangement and a novel BRAF mutation as alternatives to KIAA1549:BRAF fusion in activating the MAPK pathway in pilocytic astrocytoma. Oncogene 28:2119–2123
Knobbe CB, Reifenberger J, Reifenberger G (2004) Mutation analysis of the Ras pathway genes NRAS, HRAS, KRAS and BRAF in glioblastomas. Acta Neuropathol 108:467–470
Kordek R, Biernat W, Sapieja W et al (1995) Pleomorphic xanthoastrocytoma with a gangliomatous component: an immunohistochemical and ultrastructural study. Acta Neuropathol 89:194–197
Korshunov A, Meyer J, Capper D et al (2009) Combined molecular analysis of BRAF and IDH1 distinguishes pilocytic astrocytoma from diffuse astrocytoma. Acta Neuropathol 118:401–405
Kubo T, Kuroda Y, Kokubu A et al (2009) Resequencing analysis of the human tyrosine kinase gene family in pancreatic cancer. Pancreas 38:e200–e206
Lindboe CF, Cappelen J, Kepes JJ (1992) Pleomorphic xanthoastrocytoma as a component of a cerebellar ganglioglioma: case report. Neurosurgery 31:353–355
Louis DN, Ohgaki H, Wiestler OD et al (2007) WHO classification of tumors of the central nervous system. IARC, Lyon
Michaloglou C, Vredeveld LC, Mooi WJ et al (2008) BRAF(E600) in benign and malignant human tumours. Oncogene 27:877–895
Michaloglou C, Vredeveld LC, Soengas MS et al (2005) BRAFE600-associated senescence-like cell cycle arrest of human naevi. Nature 436:720–724
Montagut C, Settleman J (2009) Targeting the RAF–MEK–ERK pathway in cancer therapy. Cancer Lett 283:125–134
Murray JC, Donahue DJ, Malik SI et al (2010) Temporal lobe pleomorphic xanthoastrocytoma and acquired BRAF mutation in an adolescent with the constitutional 22q11.2 deletion syndrome. J Neurooncol
Perry A, Giannini C, Scheithauer BW et al (1997) Composite pleomorphic xanthoastrocytoma and ganglioglioma: report of four cases and review of the literature. Am J Surg Pathol 21:763–771
Pfister S, Janzarik WG, Remke M et al (2008) BRAF gene duplication constitutes a mechanism of MAPK pathway activation in low-grade astrocytomas. J Clin Invest 118:1739–1749
Robinson JP, VanBrocklin MW, Guilbeault AR et al (2010) Activated BRAF induces gliomas in mice when combined with Ink4a/Arf loss or Akt activation. Oncogene 29:335–344
Schiffman JD, Hodgson JG, VandenBerg SR et al (2010) Oncogenic BRAF mutation with CDKN2A inactivation is characteristic of a subset of pediatric malignant astrocytomas. Cancer Res 70:512–519
Sugita Y, Irie K, Ohshima K et al (2009) Pleomorphic xanthoastrocytoma as a component of a temporal lobe cystic ganglioglioma: a case report. Brain Tumor Pathol 26:31–36
Tannapfel A, Sommerer F, Benicke M et al (2003) Mutations of the BRAF gene in cholangiocarcinoma but not in hepatocellular carcinoma. Gut 52:706–712
Vajtai I, Varga Z, Aguzzi A (1997) Pleomorphic xanthoastrocytoma with gangliogliomatous component. Pathol Res Pract 193:617–621
Weber RG, Hoischen A, Ehrler M et al (2007) Frequent loss of chromosome 9, homozygous CDKN2A/p14(ARF)/CDKN2B deletion and low TSC1 mRNA expression in pleomorphic xanthoastrocytomas. Oncogene 26:1088–1097
Yang H, Higgins B, Kolinsky K et al (2010) RG7204 (PLX4032), a selective BRAFV600E inhibitor, displays potent antitumor activity in preclinical melanoma models. Cancer Res 70:5518–5527
Yu J, Deshmukh H, Gutmann RJ et al (2009) Alterations of BRAF and HIPK2 loci predominate in sporadic pilocytic astrocytoma. Neurology 73:1526–1531
Acknowledgments
We would like to thank Kerstin Lindenberg and Britta Friedensdorf for excellent technical assistance. We thank the tissuebank of the National Center of Tumor Diseases Heidelberg for supplying us with tumor material. This work was supported by the Bundesministerium für Bildung und Forschung (BMBF–01ES0730 and 01GS0883).
Author information
Authors and Affiliations
Corresponding author
Additional information
G. Schindler and D. Capper contributed equally to this work.
Rights and permissions
About this article
Cite this article
Schindler, G., Capper, D., Meyer, J. et al. Analysis of BRAF V600E mutation in 1,320 nervous system tumors reveals high mutation frequencies in pleomorphic xanthoastrocytoma, ganglioglioma and extra-cerebellar pilocytic astrocytoma. Acta Neuropathol 121, 397–405 (2011). https://doi.org/10.1007/s00401-011-0802-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-011-0802-6