Abstract
Recent advances in genomic technology and genome-wide analysis have identified key molecular alterations that are relevant to the diagnosis and prognosis of brain tumors. Molecular information such as mutations in isocitrate dehydrogenase (IDH) genes or 1p/19q co-deletion status will be more actively incorporated into the histological classification of diffuse gliomas. BRAF V600E mutations are found frequently in circumscribed low-grade gliomas such as pleomorphic xanthoastrocytoma (PXA) and extra-cerebellar pilocytic astrocytoma, or epithelioid glioblastomas (E–GBM), a rare variant of GBM. This mutation is relatively rare in other types of diffuse gliomas, especially in adult onset cases. Here, we present an adult onset case of IDH wild-type/BRAF V600E-mutated diffuse glioma, evolving from grade III to grade IV. The tumor displayed atypical exophytic growth and had unusual histological features not fully compatible with, but indicative of PXA and E-GBM. We discuss differential diagnosis of the tumor, and review previously described diffuse gliomas with the BRAF V600E mutation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diffuse gliomas are primary central nervous system tumors, classified as grade II, III and IV by the World Health Organization (WHO) [1]. Grade II and III gliomas often recur and tend to progress to higher grade gliomas, eventually to secondary glioblastoma (GBM). Recent advances in genomic technology and genome-wide analysis have identified key molecular alterations that are relevant to the diagnosis and prognosis of glial tumors [2–5]. Adult onset diffuse gliomas have highly frequent mutations in the isocitrate dehydrogenase (IDH) 1 or 2 genes [4, 6–8]. IDH mutations are typically accompanied by 1p/19q co-deletions or by TP53 mutations in mutually exclusive manner. The status of the 1p/19q co-deletion and TP53 mutation are significantly related to the clinical outcome of IDH-mutated diffuse gliomas [9–11]. Wild-type IDH diffuse gliomas, accounting for around one-fifth of the diffuse gliomas, have a poorer outcome compared to mutated IDH-type gliomas [12].
BRAF point or fusion mutations are also driver mutations in glial and glioneuronal tumors, especially in pediatric onset cases [13–18]. The majority of BRAF mutations are missense mutations at amino acid position 600 that change a valine into a glutamate (BRAF V600E) [17, 19, 20]. The mutated BRAF protein is constitutively activated and enhances proliferation potential through the MAPK/ERK signaling pathway [15–17, 19, 20]. BRAF V600E is frequently found in pleomorphic xanthoastrocytoma (PXA), ganglioglioma (GG) and extra-cerebellar pilocytic astrocytoma [17, 21, 22]. Previous reports indicated that BRAF V600E is also associated with epithelioid GBM (E-GBM), a rare variant of GBM [23–27]. In contrast, BRAF V600E mutations are reported to be rare in diffuse gliomas [12, 17].
Here, we present a rare case of a wild-type IDH/BRAF V600E-mutated diffuse glioma, progressing to GBM. We discuss differential diagnosis of the tumor, and review previously reported diffuse glioma cases with the BRAF mutation.
Clinical summary
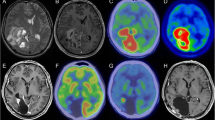
A 37-year-old woman was admitted to our hospital with left hemiparesis and homonymous hemianopia. Her past medical history, including epilepsy, was negative. A slightly hyper-dense mass without cysts and calcifications was found by computed tomography (CT) scans in the right temporal lobe (Fig. 1a). Magnetic resonance imaging (MRI) revealed a lobulated 6.0 × 6.0 cm lesion in the right temporal lobe with nearly homogenous enhancement that extended exophytically into the supra- and retrosellar space (Fig. 1b–d). When removed, the tumor had an intra-axial origin, growing exophytically around the brain stem, and tended to engulf cranial nerves and major vessels. After subtotal removal of the tumor, conventional radiotherapy and chemotherapy with temozolomide were performed. Seventeen months after the first operation, the patient was re-operated because of recurrence. The tumor had the same characteristics as when operated the first time and was subtotally resected. In addition, the patient underwent cyber knife radiosurgery and immunotherapy. Her state of consciousness and physical status gradually deteriorated, and she died from pneumonia 2 years after reoperation.
Computed tomography (CT) scans and magnetic resonance images (MRI) taken before the first operation (a–d). The tumor was slightly hyper-dense on CT scans (a), slightly low-intensity on T1-weighted images (b), T1-weighted gadolinium-enhanced MRI revealed a nearly homogenous enhanced mass, without regions of poor contrast enhancement (c), slightly high-intensity on T2-weighted images (d). Pathological features of the tumor after the first resection (e–j). The plump, eosinophilic cells with short processes proliferated diffusely, and perivascular lymphocytic cuffing was observed (e, f). Tumor cells with small to medium sized vacuoles and PAS-positive eosinophilic granular bodies were present (g, h). The tumor cells were positive for GFAP (i) and CD34 (j). After the second resection, the tumor showed increased cellularity and pleomorphism with microvascular proliferation (k). e–g, k Hematoxylin and eosin. h Periodic aid-Schiff stain. i Immunohistochemistry (IHC) for GFAP. j IHC for CD34. e, k Bar 50 μm. f–j Bar 20 μm
Pathological findings
The tumor had an infiltrative margin, and was mainly composed of plump, round eosinophilic cells with short processes (Fig. 1e, f). Cells with scant cytoplasm and elongated thin processes were also present. Nuclei of the plump cells were occasionally hyperchromatic with prominent nucleoli, and were located eccentrically. A small number of multinucleated cells were also present. Some of these cells contained small- to medium-sized vacuoles (Fig. 1g). A few eosinophilic granular bodies were found (Fig. 1h). There was perivascular lymphocytic cuffing (Fig. 1e), but without increased reticulin fiber deposition, pseudopalisading necrosis and microvascular proliferation. Mitotic rates were 5 per 10 high power fields. The immunohistochemical study was performed with a Ventana XT system (BenchMark® XT; Ventana Medical Systems, Inc., Tuscon, AZ, USA). Sections for nestin, IDH1-H and IDH1-S were probed with primary antibodies diluted in Immuno Shot Mild (Cosmobio, Tokyo, Japan) and were immunostained using the Histofine Simple Stain MAX-PO kit (Nichirei, Tokyo, Japan). INI1 was probed with the EnVision™ System (DAKO Corporation, Carpinteria, CA, USA). The tumor cells were positive for GFAP (Fig. 1i); the cytoplasm of the plump cells was particularly well stained. Expression of nestin, S100 protein and vimentin was strong and diffuse. Many of the tumor cells contained CD34 immunoreactivity (Fig. 1j). The MIB-1 LI was 9.2 % in the main area. The results of the immunohistochemical analysis are summarized in Table 1.
The histological features of the tumor were similar after both resections. The number of tumor cells with enlarged hyperchromatic nuclei and scant cytoplasm increased (Fig. 1k). A higher degree of nuclear pleomorphism was noted, and the multinucleated cells increased in number. There was microvascular proliferation and small foci of necrosis at the periphery of the section. Mitotic figures increased up to 12 mitoses per 10 high power fields. Expression of GFAP was generally decreased compared to the first surgical specimens. The MIB-1 LI peaked at 19 % in the high cellular areas. Expression of CD34 was diffuse in almost all areas. It was observed in differentiated astrocytic, small immature and pleomorphic cells, but became weak in hypercellular areas of the second resection. The tumor cells in both resections were partially positive for neuronal markers such as synaptophysin (<10 %), neurofilament (<3 %) and chromogranin A (<30 %, and generally weak). The tumor was weakly but diffusely positive for p16 and EGFR. Expression of INI1 was preserved in the tumor cells.
Genetic study revealed a BRAF V600E mutation in the initial surgical material. No mutations in exon 4 of IDH1 and IDH2 were found. DNAs were extracted from paraffin-embedded sections. Specimens were deparaffinized, followed proteinase K digestion (Sigma Aldrich, 10 mg/sections), and extracted DNAs were subjected to amplification (Perkin Elmer 9700). The primers for BRAF were F 5′-TGCTTGCTCTGATAGGAAAATG-3′ and R 5′-CCACAAAATGGATCCAGACA-3′ (exon 15, NM_004333), for IDH1 were F 5′-AATGAGCTCTATATGCCATCACTG-3′ and R 5′-AATCACATTATTGCCAACCATGACTTACTTG-3′ (exon 4, NM_005896 in GenBank), and for IDH2 were F 5′-ATCCCACGCCTAGTCCCTGGCTGGACCAAG-3′ and R 5′-CAGAGACAAGAGGATGGCTAGGCGAGGAGC-3′ (exon 4, NM_002168). Products were directly sequenced on a 3730xl DNA Analyzer (Applied Biosystems, Foster City, CA) with the Big Dye Terminator v3.1 Cycle Sequencing Kit (Applied Biosystems).
Discussion
The tumor displayed atypical radiographic features; its growth was apparently exophytic and it had well-demarcated borders. Pathologically, the tumor consisted of GFAP-positive cells with abundant cytoplasm and short stellate processes or scant cytoplasm with elongated processes. Mitotic rates were high, and the tumor was diagnosed as a Grade III anaplastic astrocytoma (WHO classification 2007) [1]. However, the tumor had some specific features. There was a small but not negligible number of multinucleated cells with vacuolated cytoplasm. The presence of a few eosinophilic granular bodies, perivascular cuffing and CD34 immunoreactivity suggested that the tumor shared some pathological characteristics with circumscribed gliomas such as PXA or GG. The tumor cells expressed neuronal markers, synaptophysin, NF and chromogranin A with variable frequency. These cells were morphologically indistinguishable from other astrocytic cells, and not taken to be neuronal components.
It is still debatable whether the tumor should be categorized as a circumscribed/localized astrocytoma. Histological examination of circumscribed gliomas often shows an infiltrative margin as in the present case. The most important differential diagnosis for this case is PXA with anaplastic features. The tumor lacked the classical features of PXA: proliferation of spindle cells with fascicular patterns and a reticular formation. Basically, the tumor was composed of fibrillary or gemistocytic astrocytic cells. Pleomorphism was not prominent; only a small number of vacuolated cells and eosinophilic granular bodies were detected by careful re-evaluation. Anaplastic astrocytomas rarely, but can show exophytic growth [28]. Taking these pathological features into consideration, we tentatively diagnosed the tumor as an anaplastic astrocytoma. Chi et al. [29] reported 7 adult cases of BRAF-mutated diffuse gliomas with atypical radiographic and histological features. They described the gliomas as infiltrating, but with relatively well-demarcated borders, similar to the tumor we described here. The atypical histological features described by the authors included the presence of ependymal-like cells, proliferation of spindle tumor cells into subarachnoid and Virchow-Robin spaces, and piloid growth of tumor cells with Rosenthal fibers. Although the atypical pathological features mentioned by the authors were not necessarily compatible with those of our case, it should be noted that BRAF-mutated diffuse gliomas have somewhat “unusual” histological features.
The BRAF V600E mutation is rare in diffuse gliomas, but certain number of cases has been reported [12, 16–19, 22–27, 29–51]. Through a literature search, total 113 diffuse gliomas were listed (Table 2): 38 cases of grade II, 14 cases of grade III including 2 gliomatosis cerebri, 54 cases of grade IV, 2 cases of grade II–III, and 5 case of grade III–IV. When available, age and gender of the patients, location of the tumor, IDH1 mutation and 1p/19q status were recorded in the table. As previously reported, the BRAF V600E mutation was found preferentially in young patients; 56 patients were 20 years of age or under. Pediatric gliomas and glioneuronal tumors have molecular backgrounds that differ from adult tumors [18, 48]. IDH mutations, a major mutation in adult grade II and III diffuse gliomas, are rare in pediatric gliomas [16, 18, 50]. BRAF V600E mutations were found in 23 % of low-grade diffuse astrocytomas in a large cohort of low-grade pediatric gliomas [18]. Ramkissoon et al. [43] also reported a similar frequency of BRAF V600E mutations in diffuse pediatric astrocytomas; however, this mutation is rare in diffuse adult gliomas, in which the prevalence is estimated at less than 1 % [12].
Affected females seemed to predominate in the listed tumors (39 female, 29 male cases); however, the gender of the other 45 cases was unknown. Most commonly, BRAF-mutated diffuse gliomas arise from the cerebral cortex; the temporal and temporo-parietal lobes seem to be most frequently affected (19 cases).
Among the grade II and III gliomas, 34 cases were astrocytic, 7 cases were oligodendrocytic, one case was oligoastrocytic; the other 12 cases were unspecified. An IDH1 mutation was detected in 6 of the 50 cases investigated: 1 case of diffuse astrocytoma (DA), 2 cases of anaplastic astrocytoma (AA), 1 case of oligodendroglioma (OG) and 2 cases of oligodendroglioma (AO). One case of IDH-mutated OG and 2 cases of AO had concomitant 1p/19q co-deletions. Thus, IDH mutations, 1p/19q co-deletions and BRAF V600E mutations are not necessarily mutually exclusive [37, 41]. The 3 gliomas harboring these three molecular events contained oligodendrocytic components. Neither IDH mutations nor 1p/19q co-deletions were found in the grade IV glioblastomas. Of note, 10 cases of BRAF-mutated diffuse astrocytomas had deletions of CDKN2A, known to be found frequently in PXA [52], and all cases were 20 years of age or under [16, 47, 50]. Recent reports indicated that secondary pediatric high grade gliomas with BRAF mutation and CDKN2A deletion arose from low-grade counterparts after long latency, and showed favorable clinical outcomes compared to GBMs without these molecular alterations [49, 50].
A close association between BRAFV600E mutations and E-GBM has been reported. The other types of grade IV glioblastomas than E-GBM are also associated with this type of mutation (Table 2). Some of the BRAF-mutated GBMs, with both classical and variant histology, progressed from preexisting low-grade gliomas [17, 22, 26, 50], as in our case. Kleinschmidt-DeMasters et al. [23] examined 13 E-GBM, 2 Rhabdoid GBM (R-GBM) and 9 Giant cell GBM (GC-GBM) cases, and identified BRAF V600E mutations in 7/13 (54 %) E-GBMs, but not in R-GBMs or GC-GBMs. E-GBM, a rare morphological variant of glioblastoma, was not yet defined in the 4th edition of WHO classification in 2007. E-GBMs are composed of patternless sheets of “melanoma-like” epithelioid cells with round eosinophilic cytoplasm and eccentrically located nuclei. These cells are discohesive and devoid of stellate cellular processes [53–55]. In our case, eosinophilic round cells, somewhat resembling epithelioid cells, proliferated. However, the cells generally had short thin stellate processes (Fig. 1f, g). When the tumor progressed to Grade IV, tumor cells with faint cytoplasm predominated (Fig. 1k). Large, round mono- or multinucleated eosinophilic cells were also present. These cells were not “melanoma-like”, but resembled the atypical glial cells in classical GBMs. We considered that the histological features of our case were not necessarily compatible with those of E-GBM. As discussed above, the tumor shared some pathological characteristics with PXA. A case of E-GBM arising from PXA was previously reported [26]. Very recently, Alexandrescu et al. reported a series of PXA cases with anaplastic foci resembling E-GBM [56]. Importantly, these cases were strongly associated with BRAFV600E mutations. Our case had histological features not fully compatible with, but indicative of, PXA and E-GBM. Clear histological definition of PXA-E-GBM lineage tumors will be needed for accurate classification of tumors harboring pathological features that are difficult to interpret, as in our case.
R-GBM is also a rare variant that shares some overlapping morphological features with E-GBM [23, 55]. GC-GBM is composed of bizarre, multinucleated giant cells, with occasional reticulin deposits; it was defined as a subtype of GBM in the WHO classification [1]. Histological definitions of these rare subtypes have not been clearly established yet, and these variants are often confused. Inactivation of INI1 is considered to be associated with rhabdoid tumor cells, and focal loss of INI1 protein has been proposed to be an important indicator for the diagnosis of R-GBM [23, 55, 57]. INI1 expression was not examined in all of the cases. Careful re-evaluation will be needed to clarify how the molecular alteration, BRAF mutation, INI1 inactivation and other molecular events that have not yet been evaluated, relate to the histological variants of GBMs.
Our patient survived 2 years after the diagnosis of GBM and multimodal treatments. Some reports indicated that BRAF V600E mutations might be a favorable prognostic factor in adult GBMs with classical histology [29, 58]. In contrast, E-GBMs, in which BRAF mutations are frequent, are known to have an aggressive clinical behavior [24, 26]. The prognostic significance of BRAF mutations in diffuses gliomas should be addressed through longer follow-up of large glioma cohorts. From now on, molecular information with prognostic, predictive and therapeutic value will be actively incorporated into the histological classification of brain tumors. Importantly, the BRAF V600E mutation can be a therapeutic target in glial tumors [14, 36, 46]. Therefore, to find this molecular alteration efficiently, further elucidation of the clinico-pathological features of BRAF-mutated diffuse gliomas will be necessary.
References
Louis D, Ohgaki H, Wiestler O et al (2007) WHO classification of tumours of the central nervous system, 4th edn. International Agency for Research on Cancer, Lyon
Cairncross G, Berkey B, Shaw E et al (2006) Phase III trial of chemotherapy plus radiotherapy compared with radiotherapy alone for pure and mixed anaplastic oligodendroglioma: intergroup Radiation Therapy Oncology Group Trial 9402. J Clin Oncol Off J Am Soc Clin Oncol 24:2707–2714
van den Bent MJ, Carpentier AF, Brandes AA et al (2006) Adjuvant procarbazine, lomustine, and vincristine improves progression-free survival but not overall survival in newly diagnosed anaplastic oligodendrogliomas and oligoastrocytomas: a randomized European Organisation for Research and Treatment of Cancer phase III trial. J Clin Oncol Off J Am Soc Clin Oncol 24:2715–2722
Parsons DW, Jones S, Zhang X et al (2008) An integrated genomic analysis of human glioblastoma multiforme. Science (New York, NY) 321:1807–1812
Weller M, Felsberg J, Hartmann C et al (2009) Molecular predictors of progression-free and overall survival in patients with newly diagnosed glioblastoma: a prospective translational study of the German Glioma Network. J Clin Oncol Off J Am Soc Clin Oncol 27:5743–5750
Balss J, Meyer J, Mueller W et al (2008) Analysis of the IDH1 codon 132 mutation in brain tumors. Acta Neuropathol 116:597–602
Watanabe T, Nobusawa S, Kleihues P et al (2009) IDH1 mutations are early events in the development of astrocytomas and oligodendrogliomas. Am J Pathol 174:1149–1153
Yan H, Parsons DW, Jin G et al (2009) IDH1 and IDH2 mutations in gliomas. New Engl J Med 360:765–773
Ichimura K, Pearson DM, Kocialkowski S et al (2009) IDH1 mutations are present in the majority of common adult gliomas but rare in primary glioblastomas. Neuro Oncol 11:341–347
Ohgaki H, Kleihues P (2009) Genetic alterations and signaling pathways in the evolution of gliomas. Cancer Sci 100:2235–2241
Ichimura K (2012) Molecular pathogenesis of IDH mutations in gliomas. Brain Tumor Pathol 29:131–139
Suzuki H, Aoki K, Chiba K et al (2015) Mutational landscape and clonal architecture in grade II and III gliomas. Nat Genet 47:458–468
Jones DT, Kocialkowski S, Liu L et al (2008) Tandem duplication producing a novel oncogenic BRAF fusion gene defines the majority of pilocytic astrocytomas. Cancer Res 68:8673–8677
Pfister S, Janzarik WG, Remke M et al (2008) BRAF gene duplication constitutes a mechanism of MAPK pathway activation in low-grade astrocytomas. J Clin Investig 118:1739–1749
Jones DTW, Kocialkowski S, Liu L et al (2009) Oncogenic RAF1 rearrangement and a novel BRAF mutation as alternatives to KIAA1549: BRAF fusion in activating the MAPK pathway in pilocytic astrocytoma. Oncogene 28:2119–2123
Schiffman JD, Hodgson JG, VandenBerg SR et al (2010) Oncogenic BRAF mutation with CDKN2A inactivation is characteristic of a subset of pediatric malignant astrocytomas. Cancer Res 70:512–519
Schindler G, Capper D, Meyer J et al (2011) Analysis of BRAF V600E mutation in 1,320 nervous system tumors reveals high mutation frequencies in pleomorphic xanthoastrocytoma, ganglioglioma and extra-cerebellar pilocytic astrocytoma. Acta Neuropathol 121:397–405
Zhang J, Wu G, Miller CP et al (2013) Whole-genome sequencing identifies genetic alterations in pediatric low-grade gliomas. Nat Genet 45:602–612
Davies H, Bignell GR, Cox C et al (2002) Mutations of the BRAF gene in human cancer. Nature 417:949–954
Wan PT, Garnett MJ, Roe SM et al (2004) Mechanism of activation of the RAF-ERK signaling pathway by oncogenic mutations of B-RAF. Cell 116:855–867
Dougherty MJ, Santi M, Brose MS et al (2010) Activating mutations in BRAF characterize a spectrum of pediatric low-grade gliomas. Neuro Oncol 12:621–630
Dias-Santagata D, Lam Q, Vernovsky K et al (2011) BRAF V600E mutations are common in pleomorphic xanthoastrocytoma: diagnostic and therapeutic implications. PLoS One 6:e17948
Kleinschmidt-DeMasters BK, Aisner DL, Birks DK et al (2013) Epithelioid GBMs show a high percentage of BRAF V600E mutation. Am J Surg Pathol 37:685–698
Broniscer A, Tatevossian RG, Sabin ND et al (2014) Clinical, radiological, histological and molecular characteristics of paediatric epithelioid glioblastoma. Neuropathol Appl Neurobiol 40:327–336
Nobusawa S, Hirato J, Kurihara H et al (2014) Intratumoral heterogeneity of genomic imbalance in a case of epithelioid glioblastoma with BRAF V600E mutation. Brain Pathol (Zurich, Switzerland) 24:239–246
Tanaka S, Nakada M, Nobusawa S et al (2014) Epithelioid glioblastoma arising from pleomorphic xanthoastrocytoma with the BRAF V600E mutation. Brain Tumor Pathol 31:172–176
Kleinschmidt-DeMasters BK, Aisner DL, Foreman NK (2015) BRAF VE1 immunoreactivity patterns in epithelioid glioblastomas positive for BRAF V600E mutation. Am J Surg Pathol 39:528–540
Tanaka K, Sasayama T, Kawamura A et al (2006) Isolated oculomotor nerve paresis in anaplastic astrocytoma with exophytic invasion. Neurol Med Chir (Tokyo) 46:198–201
Chi AS, Batchelor TT, Yang D et al (2013) BRAF V600E mutation identifies a subset of low-grade diffusely infiltrating gliomas in adults. J Clin Oncol Off J Am Soc Clin Oncol 31:e233–e236
Knobbe CB, Reifenberger J, Reifenberger G (2004) Mutation analysis of the Ras pathway genes NRAS, HRAS, KRAS and BRAF in glioblastomas. Acta Neuropathol 108:467–470
Basto D, Trovisco V, Lopes JMM et al (2005) Mutation analysis of B-RAF gene in human gliomas. Acta Neuropathol 109:207–210
Jeuken J, van den Broecke C, Gijsen S et al (2007) RAS/RAF pathway activation in gliomas: the result of copy number gains rather than activating mutations. Acta Neuropathol 114:121–133
Hagemann C, Gloger J, Anacker J et al (2009) RAF expression in human astrocytic tumors. Int J Mol Med 23:17–31
MacConaill LE, Campbell CD, Kehoe SM et al (2009) Profiling critical cancer gene mutations in clinical tumor samples. PLoS One 4:e7887
Sievert AJ, Jackson EM, Gai X et al (2009) Duplication of 7q34 in pediatric low-grade astrocytomas detected by high-density single-nucleotide polymorphism-based genotype arrays results in a novel BRAF fusion gene. Brain Pathol (Zurich, Switzerland) 19:449–458
Nicolaides TP, Li H, Solomon DA et al (2011) Targeted therapy for BRAFV600E malignant astrocytoma. Clin Cancer Res Off J Am Assoc Cancer Res 17:7595–7604
Badiali M, Gleize V, Paris S et al (2012) KIAA1549-BRAF fusions and IDH mutations can coexist in diffuse gliomas of adults. Brain Pathol (Zurich, Switzerland) 22:841–847
Horbinski C, Nikiforova MN, Hagenkord JM et al (2012) Interplay among BRAF, p16, p53, and MIB1 in pediatric low-grade gliomas. Neuro Oncol 14:777–789
Kim Y-HH, Nonoguchi N, Paulus W et al (2012) Frequent BRAF gain in low-grade diffuse gliomas with 1p/19q loss. Brain pathology (Zurich, Switzerland) 22:834–840
Lin A, Rodriguez FJ, Karajannis MA et al (2012) BRAF alterations in primary glial and glioneuronal neoplasms of the central nervous system with identification of 2 novel KIAA1549:BRAF fusion variants. J Neuropathol Exp Neurol 71:66–72
Myung JK, Cho H, Park C-KK et al (2012) Analysis of the BRAF(V600E) mutation in central nervous system tumors. Transl Oncol 5:430–436
Bettegowda C, Agrawal N, Jiao Y et al (2013) Exomic sequencing of four rare central nervous system tumor types. Oncotarget 4:572–583
Ramkissoon LA, Horowitz PM, Craig JM et al (2013) Genomic analysis of diffuse pediatric low-grade gliomas identifies recurrent oncogenic truncating rearrangements in the transcription factor MYBL1. Proc Natl Acad Sci USA 110:8188–8193
Bleeker FE, Lamba S, Zanon C et al (2014) Mutational profiling of kinases in glioblastoma. BMC Cancer 14:718
Fernandez-Vega I, Quirk J, Norwood FL et al (2014) Gliomatosis cerebri type 1 with extensive involvement of the spinal cord and BRAF V600E mutation. Pathol Oncol Res POR 20:215–220
Robinson GW, Orr BA, Gajjar A (2014) Complete clinical regression of a BRAF V600E-mutant pediatric glioblastoma multiforme after BRAF inhibitor therapy. BMC Cancer 14:258
Roth JJ, Santi M, Rorke-Adams LB et al (2014) Diagnostic application of high resolution single nucleotide polymorphism array analysis for children with brain tumors. Cancer Genet 207:111–123
Gierke M, Sperveslage J, Schwab D et al (2015) Analysis of IDH1-R132 mutation, BRAF V600 mutation and KIAA1549-BRAF fusion transcript status in central nervous system tumors supports pediatric tumor classification. J Cancer Res Clin Oncol 27 [Epub ahead of print]
Korshunov A, Ryzhova M, Hovestadt V et al (2015) Integrated analysis of pediatric glioblastoma reveals a subset of biologically favorable tumors with associated molecular prognostic markers. Acta Neuropathol 129:669–678
Mistry M, Zhukova N, Merico D et al (2015) BRAF mutation and CDKN2A deletion define a clinically distinct subgroup of childhood secondary high-grade glioma. J Clin Oncol Off J Am Soc Clin Oncol 33:1015–1022
Takahashi Y, Akahane T, Sawada T et al (2015) Adult classical glioblastoma with a BRAF V600E mutation. World J Surg Oncol 13:100
Weber RG, Hoischen A, Ehrler M et al (2007) Frequent loss of chromosome 9, homozygous CDKN2A/p14(ARF)/CDKN2B deletion and low TSC1 mRNA expression in pleomorphic xanthoastrocytomas. Oncogene 26:1088–1097
Kleinschmidt-DeMasters BK, Meltesen L, McGavran L et al (2006) Characterization of glioblastomas in young adults. Brain Pathol (Zurich, Switzerland) 16:273–286
Rodriguez FJ, Scheithauer BW, Giannini C et al (2008) Epithelial and pseudoepithelial differentiation in glioblastoma and gliosarcoma: a comparative morphologic and molecular genetic study. Cancer 113:2779–2789
Bette Kay K-D, Ali HA, Diane KB et al (2010) Epithelioid versus rhabdoid glioblastomas are distinguished by monosomy 22 and immunohistochemical expression of INI-1 but not claudin 6. Am J Surg Pathol 34:341–354
Alexandrescu S, Korshunov A, Lai SH et al (2015) Epithelioid glioblastomas and anaplastic epithelioid pleomorphic xanthoastrocytomas—same entity or first cousins? Brain pathology (Zurich, Switzerland) bpa.12295. [Epub ahead of print]
Shogo E, Shunsuke T, Shigeru Y et al (2013) Primary rhabdoid tumor with low grade glioma component of the central nervous system in a young adult. Neuropathology 33:185–191
Dahiya S, Emnett RJ, Haydon DH et al (2014) BRAF-V600E mutation in pediatric and adult glioblastoma. Neuro Oncol 16:318–319
Acknowledgments
We thank Dr. M Ruberg for a critical reading of the manuscript, Drs. Shinji Ito and Dr. Takashi Komori for the immunohistochemistry, and the latter for kind advice concerning the diagnosis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suzuki, Y., Takahashi-Fujigasaki, J., Akasaki, Y. et al. BRAF V600E-mutated diffuse glioma in an adult patient: a case report and review. Brain Tumor Pathol 33, 40–49 (2016). https://doi.org/10.1007/s10014-015-0234-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10014-015-0234-4