Abstract
Purpose
The aim of this systematic review was to apply the anatomic ACL reconstruction scoring checklist (AARSC) and to evaluate the degree to which clinical studies comparing single-bundle (SB) and double-bundle (DB) ACL reconstructions are anatomic.
Methods
A systematic electronic search was performed using the databases PubMed (MEDLINE), EMBASE and Cochrane Library. Studies published from January 1995 to January 2014 comparing SB and DB ACL reconstructions with clinical outcome measurements were included. The items from the AARSC were recorded for both the SB and DB groups in each study.
Results
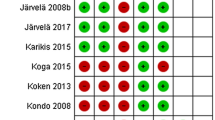
Eight-thousand nine-hundred and ninety-four studies were analysed, 77 were included. Randomized clinical trials (29; 38 %) and prospective comparative studies (29; 38 %) were the most frequent study type. Most studies were published in 2011 (19; 25 %). The most commonly reported items for both SB and DB groups were as follows: graft type (152; 99 %), femoral and tibial fixation method (149; 97 % respectively), knee flexion angle during graft tensioning (124; 81 %) and placement of the tibial tunnel at the ACL insertion site (101; 66 %). The highest level of documentation used for ACL tunnel position for both groups was often one dimensional, e.g. drawing, operative notes or o’clock reference. The DB reconstruction was in general more thoroughly reported. The means for the AARSC were 6.9 ± 2.8 for the SB group and 8.3 ± 2.8 for the DB group. Both means were below a proposed required minimum score of 10 for anatomic ACL reconstruction.
Conclusions
There was substantial underreporting of surgical data for both the SB and DB groups in clinical studies. This underreporting creates difficulties when analysing, comparing and pooling results of scientific studies on this subject.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The goals of anterior cruciate ligament (ACL) reconstruction are the restoration of normal knee anatomy and function, reestablishment of biological and biomechanical homeostasis and prevention of osteoarthritis (OA). The traditional transtibial technique has come under recent scrutiny as it has been shown that it results in a non-anatomic reconstruction with regards to the native ACL footprints and therefore may cause suboptimal knee kinematics [45, 46, 74, 92]. Focus is now on anatomic reconstruction, with greater emphasis on tunnel position in the native ACL footprint, functional restoration of the ACL to its native dimensions, collagen orientation and insertion sites. Both biomechanical and clinical trials have shown superior results in support of this technique [11, 30, 57]. It must be stressed that double-bundle (DB) ACL reconstruction is not synonymous with anatomic ACL reconstruction [39]. It is merely a step closer to replicating the native ACL anatomy; it can still be performed non-anatomically. The theoretical advantage is that DB ACL reconstruction allows for individualizing the surgical procedure to each patient, of more complete footprint restoration, and that the two bundles can be tensioned separately, mimicking the native tension patterns of the ACL bundles.
With the emergence of the term anatomic ACL reconstruction, many authors have claimed their adoption of anatomic ACL reconstruction techniques. However, two previous systematic reviews indicated that often only limited information is provided by the authors when outlining the specifics of their anatomic ACL reconstruction [84, 85]. Furthermore, variations in anatomic techniques were found. To further evaluate the possible benefit of performing anatomic reconstruction and to be better equipped when comparing studies, it is important to use standardized and thoroughly evaluated criteria for what constitutes anatomic ACL reconstruction. This has led to the development and validation of the anatomic ACL reconstruction scoring checklist (AARSC) by van Eck et al. [82]. An international expert panel of orthopaedic surgeons listed potential criteria for what constitutes an anatomic ACL reconstruction. These criteria were evaluated and expanded by a global panel of orthopaedic surgeons. A modified list containing 17 items with the maximum score of 19 was created (Table 1). The new list was verified by a large number of peer reviewers from four high-impact orthopaedic sports medicine journals. The score was then tested for validity and reliability, and all items were evaluated for internal consistency. This scoring system allows for the grading of ACL reconstruction procedures in individual patients, for review of the documentation of surgical methods in published studies on anatomic ACL reconstructions and for peer review of scientific manuscripts.
The goal of this systematic review was to apply the AARSC on current clinical studies comparing SB and DB ACL reconstructions. It was hypothesized that reported data in studies comparing SB and DB ACL reconstructions would fall below a proposed minimum required score of 10 for anatomic ACL reconstruction, illustrating the heterogeneity of current literature on the subject.
Materials and methods
This systematic review was conducted following the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines [53].
Eligibility criteria
Inclusion criteria were clinical therapeutic studies that compare SB and DB primary ACL reconstructions. Prognostic and diagnostic studies were generally excluded unless there was a clear relation between the outcome measures and the surgical technique. Economical and decision analysis studies were excluded. Studies with skeletally mature, living human subjects with isolated total ACL rupture were eligible for inclusion. Concomitant meniscus and minor cartilage injuries were not criteria for exclusion. Only papers written in English were included [65].
Information sources and search
Electronic search
A systematic electronic search was performed using PubMed (MEDLINE), EMBASE and Cochrane Library. Studies that were published from January 1995 to August 2011 were included. An additional updated search was performed in January of 2014 only from the PubMed (MEDLINE) database, and relevant studies published between August 2011 and January 2014 were included. Execution and validation of the search was attained from two experts in electronic search methods at the **MASKED** Library. The following search terms were used in the fields title, Abstract and Keywords: ‘anterior cruciate ligament’ OR ‘ACL’ AND ‘reconstruction’ OR ‘surgery’ AND ‘1995:3000’ (see “Appendix” for complete search string) [65].
Data collection and analysis
Study selection
Three researchers sorted the studies based on the abstracts from the electronic search. Each reviewer sorted one database, which in turn was validated twice by the other reviewers. The included studies were categorized into study types proposed by the Oxford Centre for Evidence-Based Medicine and into the category SB, DB or SB versus DB reconstruction. Only studies comparing SB to DB ACL reconstruction were included in this systematic review regardless of graft type or fixation method. The study was processed in full text and analysed if the abstract did not provide enough data to make a decision. The analysis was not performed in a blinded fashion, i.e. the researchers were not blinded to author, year and journal of publication. Disagreement between the reviewers was resolved by consensus or by discussion with the senior author when consensus was not reached.
Data collection process
The data were extracted from the included papers by the first two authors through utilization of a computerized database created in Microsoft Access (version 2010, Microsoft Corporation, Redmond, WA, USA). Each study was validated twice by the first author.
Data items
The data that were obtained from the included papers were the following: author, year, title, journal, volume, issue, pages, ISSN, DOI, abstract, author address, database provider, category, study type, level of evidence and country. In addition, the items from the AARSC were extracted for both SB and DB groups (Table 1). In some studies, there were comparisons for more than two groups. In these cases, the scoring system was applied to all groups, and thereafter, only the highest scoring group from the SB and/or DB group was included. The study needed to state clearly the item from the scoring system, e.g. the authors needed to state that they visualized the ACL insertion sites, otherwise no points were given. For a point to be awarded for a specific criterion in the score, the criterion in question had to be applied to all patients in the SB or DB group. Furthermore, outside-in drilling of the femoral tunnel was classified as transportal drilling.
Synthesis of results
Statistical analysis of the data was performed using the IBM SPSS Statistics (version 21, IBM Corporation, USA). Descriptive statistics were used to summarize all data recorded. The comparison of AARSC score depending on the level of evidence and year of publication for the SB and DB groups was performed using one-way ANOVA. Alpha was set to 0.05.
Results
Study selection
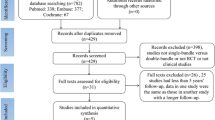
An initial electronic search yielded 5,608 studies in PubMed (MEDLINE), 5,421 studies in EMBASE and 700 studies in the Cochrane Library. Duplicates were removed. There were 7,154 studies left in which 3,757 were excluded based on the abstracts and 1,887 based on full-text assessment. A total of 1,510 studies were included in the database and categorized into SB, DB and SB versus DB ACL reconstruction. Fifty-one studies were categorized as studies comparing SB and DB ACL reconstructions. An updated search was performed in January 2014 only from the PubMed database. Of these, a total of 26 studies were included. This amounted to 77 studies in total included in this systematic review (Fig. 1) [1–10, 12–17, 20, 22–24, 26–31, 33–38, 40–44, 47–52, 54–56, 58, 59, 61, 62, 64, 66–68, 71–73, 75–81, 86–91, 93–99].
Characteristics of studies
The time span of the included studies stretches from 2004 to 2014. Most studies were published in 2011 (19; 25 %) and thereafter 2012 (12; 16 %). The top three journals were Arthroscopy (19; 25 %), Knee Surgery Sports Traumatology Arthroscopy (KSSTA) (18; 23 %) and Am J Sports Med (AJSM) (16; 21 %). Together they represented 69 % of all included studies. Subgroup analysis revealed that the most randomized clinical trials (RCT) were published in KSSTA (n = 7) followed by AJSM (n = 6) and Arthroscopy (n = 5). Of these RCTs, AJSM had six studies classified as category 1 in level of evidence, KSSTA five studies, and Arthroscopy four studies. The top five countries in terms of number of studies were Japan (17; 22 %), Italy (12; 16 %), South Korea (9; 12 %), China (7; 9 %) and Germany and Finland both (5; 6 %). Most studies were RCTs (29; 38 %), and the least common were case series (4; 5 %) (Table 2). Level of evidence category 2 was most common (30; 39 %) (Table 3). The most common graft types were hamstrings tendon graft for both groups (Table 4).
Synthesis of results
Femur-related items
Thirty (39 %) in the SB group and 41 (53 %) in the DB group described visualizing the femoral ACL insertion site. Twenty-eight (36 %) in the SB group and 42 (55 %) in the DB group reported placement of the femoral tunnels in the ACL insertion site. Subgroup analysis revealed that 6 (8 %) in the SB group and 8 (10 %) in the DB group stated placement in the femoral ACL insertion site but did not report visualization of the insertion site (Table 5). Moreover, 22 (29 %) in the SB group and 34 (44 %) in the DB group reported both placement and visualization of the femoral ACL insertion site. Also, 17 (22 %) in the SB group and 24 (31 %) in the DB group stated transportal drilling of the femur tunnel(s) and placement of the tunnel(s) in the femoral ACL insertion site. Eleven (14 %) in the SB group and 18 (23 %) in the DB group reported placement of the tunnel(s) in the ACL insertion site but did not report transportal drilling. The use of an accessory medial portal was reported more often in the DB group (25; 32 %) than in the SB group (9; 12 %). Six studies (8 %) in the SB group and 16 (21 %) in the DB group documented the use of an accessory medial portal and placement of the tunnel(s) at the insertion site of the femur. Measurements of the femoral ACL insertion site dimensions were only reported in one study for SB (1; 1 %) and DB (1; 1 %) groups. Femoral fixation methods were documented in all but three studies (74; 96 %) for SB groups and in all but two studies (75; 97 %) for DB groups.
Tibia-related items
Twenty-nine studies (38 %) in the SB group and 39 (51 %) in the DB group described visualizing the tibial ACL insertion site; however, 44 (57 %) in the SB group and 57 (74 %) in the DB group reported that the tibial tunnel was placed in the insertion site of the ACL (Table 1). Subgroup analysis revealed that 22 (29 %) in the SB group and 23 (30 %) in the DB group did not document visualization of the insertion site but claimed placement in the insertion site (Table 5). Furthermore, 7 (9 %) in the SB group and 5 (6 %) in the DB group documented visualization of the insertion site but did not claim placement in the insertion site. Twenty-two (29 %) in the SB group and 34 (44 %) in the DB group reported both visualization and placement of the ACL insertion site. Measurements of the tibial ACL insertion site dimensions were only reported in one study for SB (1; 1 %) and DB (1; 1 %) groups. Tibial fixation methods were documented in all but three studies (74; 96 %) for SB groups and in all but two studies (75; 97 %) for DB groups.
Documentation of tunnel position
The highest level of documentation used for ACL tunnel position for both groups was most often the scoring item with zero point allocation (84; 55 %), i.e. drawing, diagram, operative note, dictation or o’clock reference (Table 1). The second most common was two-dimensional images (44; 29 %) and thereafter three-dimensional images (26; 17 %).
Single-bundle versus double-bundle
The DB reconstruction was reported more thoroughly in several items, especially the usage of accessory medial portal, visualization of the insertion sites, drilling technique and placement and fixation of the graft(s) (Table 1).
Anatomic ACL score
Calculation of the AARSC score reveals a mean score of 6.9 ± 2.8 for the SB group and 8.3 ± 2.8 for the DB group (Table 6). There were no significant differences in the AARSC score for either the SB or DB group depending on the level of evidence of the study with p = 0.126 (n.s) and p = 0.226 (n.s) respectively, or the year of publication with p = 0.745 (n.s) and p = 0.717 (n.s) for SB and DB groups respectively.
Discussion
The most important finding from this systematic review is that there is a substantial underreporting of surgical data with means in AARSC well below the proposed required minimum score of 10. This makes any pooling and comparing of outcomes measures across studies difficult, if not impossible.
Most studies are published in recent years and in the journals Arthroscopy (25 %), KSSTA (23 %) and AJSM (21 %). The trend is an annual increase in the number of studies. This is not surprising as the surgical technique is relatively new. A positive finding is that most studies are RCTs and that there are fewer case series. This is promising and a trend that hopefully will continue in the future. Japan and Italy are the countries with most studies, contributing 22 and 12 % of all studies in this review, respectively. However, it must be stressed that despite the trend of increasing Level of evidence with time, we see that studies are still lacking in documentation [65]. It is at the level of peer review that we can stress the importance of adequate documentation and improvements are expected in the future.
A majority in both the SB group and the DB group report placement of the tibial tunnel(s) at the insertion site for the native ACL. However, only approximately half of those claim visualization of the insertion site. Only 29 % in the SB group and 44 % in the DB group report both visualization and anatomical placement on the tibial side. Absent reporting may not necessarily be synonymous with absent visualization; however, this is related to how the scoring system is implemented.
The bony landmarks of the femoral notch, the lateral inter-condylar ridge and the lateral bifurcate ridge constitute an important aid in the placement of the tunnels, and this is a significant finding in recent years [100]. In total for both groups, only approximately 10 % report visualization of the lateral inter-condylar ridge and 6 % the lateral bifurcate ridge. The lateral inter-condylar ridge is of special interest in both groups as it defines the superior border for the footprint [19, 60, 70]. The lateral bifurcate ridge marks the border between the AM and PL bundles [18]. Therefore, the latter is a vital component in the placement of the tunnels in DB reconstruction. Also, the landmarks are present in both sub-acute and chronic cases without a significant difference in presence [83]. Thirty-nine per cent in the SB group and 53 % in the DB group claim visualization of the femoral insertion sites, which is comparable with the number of studies that state placement on the femoral insertion sites. Overall this illustrates a substantial underreporting that creates an uncertainty when assessing the outcomes of the studies. The utilization of an accessory medial portal facilitates both the visualization of the ACL footprint on the femur and also provides a portal for drilling [8]. Only 35 % in the SB group and 42 % in the DB group report transportal drilling. Some studies did, however, report the use of transportal drilling of the PL bundle and transtibial drilling of the AM bundle. These studies were not awarded a point for transportal drilling, as it was necessary that all tunnel drillings can be performed independently. This is not optimal as the femoral insertion site for the AM bundle can in some cases be reached through the tibial tunnel; however, a consensus was reached in order to create homogenous reporting [46]. The implementation of transportal drilling can to a certain extent reduce the inherent restrictions when drilling through a tibial tunnel [21, 25, 32, 63]. Furthermore, there are several studies that report difficulty in reaching the anatomic femoral insertion sites through transtibial drilling [11, 45, 46]. Caution is therefore warranted when studies claim anatomical placement solely facilitated though transtibial drilling, especially in DB ACL reconstruction.
The measurement of the tibial and femoral ACL footprint aids the orthopaedic surgeon in both placement of the tunnel and individualization of the reconstruction to the patient and is seldom technically challenging for the surgeon. These measurements were only provided in one instance (1 %) in the SB group and one instance (1 %) in the DB group, and only two studies claimed individualization. Today, experienced orthopaedic surgeons often describe attempts to individualize the surgical procedure to most patients. In this individualization, several factors are taken into account, e.g. native ACL insertion site size, graft thickness, acceptance of harvest-site morbidity and notch size. The quadriceps tendon and the patellar tendon offer possibilities of preoperative measurement and therefore preoperative individualization; this is not the case with hamstrings tendon autografts. Of course, individualization is not possible if patients are randomized, and this should be taken into account as most included studies in this review are RCTs. Also, in comparative studies in general there is an inherent difficulty to individualize in this way as most studies are conducted following strict surgical methods. Regardless of these obvious restrictions, we propose increased attention to intraoperative measurements and reporting detail, to achieve more individualization of ACL reconstruction in the future.
The majority of the studies document tunnel position with diagrams or operative notes, which does not yield any points in the AARSC. Documentation of the tunnel position is especially important in studies comparing two different surgical techniques. Two-dimensional images especially clear arthroscopic pictures are easy to use and store, and present valuable information to the reader. In the future, image documentation of tibial and femoral tunnel placement should be a prerequisite with all major journals, especially in scientific papers claiming anatomic ACL reconstruction. Several studies utilize the o’clock reference which has several limitations making it difficult to reproduce [69]. Hence, when radiographic figures are not presented, one should thoroughly and meticulously describe the tunnel position, preferably with reference to the bony landmarks [83].
The AARSC has only recently been developed and not yet implemented in a systematic review or clinical study. The reliability and the validity of the scoring system have been assessed [82]. The maximum score is 19 points. In this systematic review, the calculated mean for the SB group was 6.9 ± 2.8 and 8.3 ± 2.8 for the DB group. It is difficult to evaluate these values, as it has not previously been reported. A classification and grouping with cut-offs for the score is planned. Based on their clinical experience, the senior authors of this systematic review propose a minimum score of 10 for anatomic ACL reconstruction. The mean score for SB and DB reconstructions in this study fell well below this minimum required score. As previously stated, unreported items are not synonymous with not performed. In many cases, these procedures are performed by experienced surgeons who may not report their technique in the papers, regarding this as redundant or obvious information. With today’s high level of medical research and in the light of new fields of focus in ACL reconstruction, researchers and surgeons, experienced and less so alike, should be required to provide sufficient information on their surgical technique allowing readers a fair comparison and interpretation of the outcomes. Without this information, it may be difficult to pool the outcomes of studies and understand what we actually are comparing.
A limitation of this study was that the data extraction was not performed in a blinded fashion. However, two independent reviewers selected all the papers and extracted all the data. Furthermore, the first authors validated the extracted data by processing the included studies once again after data extraction. Outcomes were not extracted, as it was not the aim of the systematic review. Hence, several topics regarding clinical outcomes were removed from the PRISMA guidelines, as they were not applicable to this systematic review. The utilized scoring system is a newly developed one and has not previously been implemented; however, it has been tested for reliability and validity. Test–retest reliability still needs to be confirmed over a longer period of time. As a result of this, many of the papers included in the systematic review are older than the score itself.
In the future, comparison between clinical trials could be facilitated by implementing tools such as standardized clinical tests or standardized surgical procedures. The AARSC could be a valuable tool to assist with clinical outcomes research. Future research should focus on improving surgical techniques and their documentation.
Conclusions
The most important findings in this systematic review were that there was a substantial underreporting of surgical data in both SB (6.9 points) and DB (8.3 points) groups. The calculated means of AARSC were below the proposed required minimum score of 10/19 for anatomic ACL reconstruction. This underreporting creates difficulty when comparing and pooling the results of these studies and warrants improvement in future studies on ACL reconstruction.
References
Achtnich A, Stiepani H, Forkel P, Metzlaff S, Hanninen EL, Petersen W (2013) Tunnel widening after anatomic double-bundle and mid-position single-bundle anterior cruciate ligament reconstruction. Arthroscopy 29(9):1514–1524
Adachi N, Ochi M, Uchio Y, Iwasa J, Kuriwaka M, Ito Y (2004) Reconstruction of the anterior cruciate ligament. Single- versus double-bundle multistranded hamstring tendons. J Bone Joint Surg Br 86(4):515–520
Aglietti P, Giron F, Cuomo P, Losco M, Mondanelli N (2007) Single-and double-incision double-bundle ACL reconstruction. Clin Orthop Relat Res 454:108–113
Aglietti P, Giron F, Losco M, Cuomo P, Ciardullo A, Mondanelli N (2010) Comparison between single-and double-bundle anterior cruciate ligament reconstruction: a prospective, randomized, single-blinded clinical trial. Am J Sports Med 38(1):25–34
Ahlden M, Sernert N, Karlsson J, Kartus J (2013) A prospective randomized study comparing double- and single-bundle techniques for anterior cruciate ligament reconstruction. Am J Sports Med 41(11):2484–2491
Aldrian S, Valentin P, Wondrasch B, Krusche-Mandl I, Ostermann RC, Platzer P, Hofbauer M (2013) Gender differences following computer-navigated single- and double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Surg Traumatol Arthrosc 22(9):2145–2152
Araki D, Kuroda R, Kubo S, Fujita N, Tei K, Nishimoto K, Hoshino Y, Matsushita T, Matsumoto T, Nagamune K, Kurosaka M (2011) A prospective randomised study of anatomical single-bundle versus double-bundle anterior cruciate ligament reconstruction: quantitative evaluation using an electromagnetic measurement system. Int Orthop 35(3):439–446
Araujo PH, van Eck CF, Macalena JA, Fu FH (2011) Advances in the three-portal technique for anatomical single- or double-bundle ACL reconstruction. Knee Surg Sports Surg Traumatol Arthrosc 19(8):1239–1242
Asagumo H, Kimura M, Kobayashi Y, Taki M, Takagishi K (2007) Anatomic reconstruction of the anterior cruciate ligament using double-bundle hamstring tendons: surgical techniques, clinical outcomes, and complications. Arthroscopy 23(6):602–609
Bahl V, Goyal A, Jain V, Joshi D, Chaudhary D (2013) Effect of haemarthrosis on the rehabilitation of anterior cruciate ligament reconstruction-single bundle versus double bundle. J Orthop Surg Res. 8:5
Bedi A, Musahl V, Steuber V, Kendoff D, Choi D, Allen AA, Pearle AD, Altchek DW (2011) Transtibial versus anteromedial portal reaming in anterior cruciate ligament reconstruction: an anatomic and biomechanical evaluation of surgical technique. Arthroscopy 27(3):380–390
Beyaz S, Ozkoc G, Akpinar S, Demir S, Adam M, Tuncay IC (2012) Comparison of tunnel expansion and isometric muscle strength after ACL reconstruction with single- or dual-bundle hamstring allograft: a prospective, randomized study. Acta Orthop Traumatol Turc. 46(5):353–360
Branch TP, Siebold R, Freedberg HI, Jacobs CA (2011) Double-bundle ACL reconstruction demonstrated superior clinical stability to single-bundle ACL reconstruction: a matched-pairs analysis of instrumented tests of tibial anterior translation and internal rotation laxity. Knee Surg Sports Surg Traumatol Arthrosc 19(3):432–440
Claes S, Neven E, Callewaert B, Desloovere K, Bellemans J (2011) Tibial rotation in single- and double-bundle ACL reconstruction: a kinematic 3-D in vivo analysis. Knee Surg Sports Surg Traumatol Arthrosc 19(Suppl 1):S115–S121
Dejour D, Vanconcelos W, Bonin N, Saggin PR (2013) Comparative study between mono-bundle bone-patellar tendon-bone, double-bundle hamstring and mono-bundle bone-patellar tendon-bone combined with a modified Lemaire extra-articular procedure in anterior cruciate ligament reconstruction. Int Orthop 37(2):193–199
Ferretti A, Monaco E, Labianca L, Conteduca F, De Carli A (2008) Double-bundle anterior cruciate ligament reconstruction: a computer-assisted orthopaedic surgery study. Am J Sports Med 36(4):760–766
Ferretti A, Monaco E, Labianca L, De Carli A, Maestri B, Conteduca F (2009) Double-bundle anterior cruciate ligament reconstruction: a comprehensive kinematic study using navigation. Am J Sports Med 37(8):1548–1553
Ferretti M, Ekdahl M, Shen W, Fu FH (2007) Osseous landmarks of the femoral attachment of the anterior cruciate ligament: an anatomic study. Arthroscopy 23(11):1218–1225
Fu FH, Jordan SS (2007) The lateral intercondylar ridge—a key to anatomic anterior cruciate ligament reconstruction. J Bone Joint Surg Am 89(10):2103–2104
Fujita N, Kuroda R, Matsumoto T, Yamaguchi M, Yagi M, Matsumoto A, Kubo S, Matsushita T, Hoshino Y, Nishimoto K, Araki D, Kurosaka M (2011) Comparison of the clinical outcome of double-bundle, anteromedial single-bundle, and posterolateral single-bundle anterior cruciate ligament reconstruction using hamstring tendon graft with minimum 2-year follow-up. Arthroscopy 27(7):906–913
Giron F, Buzzi R, Aglietti P (1999) Femoral tunnel position in anterior cruciate ligament reconstruction using three techniques. A cadaver study. Arthroscopy 15(7):750–756
Gobbi A, Mahajan V, Karnatzikos G, Nakamura N (2011) Single- versus double-bundle ACL reconstruction: is there any difference in stability and function at 3-year followup? Clin Orthop Relat Res 470(3):824–834
Gong X, Jiang D, Wang YJ, Wang J, Ao YF, Yu JK (2013) Second-look arthroscopic evaluation of chondral lesions after isolated anterior cruciate ligament reconstruction: single- versus double-bundle reconstruction. Am J Sports Med 41(10):2362–2367
Hantes ME, Tsarouhas A, Giakas G, Spiropoulos G, Sideris V, Christel P, Malizos KN (2012) Effect of fatigue on tibial rotation after single- and double-bundle anterior cruciate ligament reconstruction: a 3-dimensional kinematic and kinetic matched-group analysis. Am J Sports Med 40(9):2045–2051
Harner CD, Honkamp NJ, Ranawat AS (2008) Anteromedial portal technique for creating the anterior cruciate ligament femoral tunnel. Arthroscopy 24(1):113–115
Hemmerich A, van der Merwe W, Batterham M, Vaughan CL (2011) Double-bundle ACL surgery demonstrates superior rotational kinematics to single-bundle technique during dynamic task. Clin Biomech (Bristol, Avon) 26(10):998–1004
Hemmerich A, van der Merwe W, Batterham M, Vaughan CL (2011) Knee rotational laxity in a randomized comparison of single- versus double-bundle anterior cruciate ligament reconstruction. Am J Sports Med 39(1):48–56
Hofbauer M, Valentin P, Kdolsky R, Ostermann RC, Graf A, Figl M, Aldrian S (2010) Rotational and translational laxity after computer-navigated single- and double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 18(9):1201–1207
Hussein M, van Eck CF, Cretnik A, Dinevski D, Fu FH (2012) Individualized anterior cruciate ligament surgery: a prospective study comparing anatomic single- and double-bundle reconstruction. Am J Sports Med 40(8):1781–1788
Hussein M, van Eck CF, Cretnik A, Dinevski D, Fu FH (2012) Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3- to 5-year follow-up. Am J Sports Med 40(3):512–520
Ibrahim SA, Hamido F, Al Misfer AK, Mahgoob A, Ghafar SA, Alhran H (2009) Anterior cruciate ligament reconstruction using autologous hamstring double bundle graft compared with single bundle procedures. J Bone Joint Surg Br 91(10):1310–1315
Inoue M, Tokuyasu S, Kuwahara S, Yasojima N, Kasahara Y, Kondo E, Onodere S, Yasuda K (2010) Tunnel location in transparent 3-dimensional CT in anatomic double-bundle anterior cruciate ligament reconstruction with the trans-tibial tunnel technique. Knee Surg Sports Traumatol Arthrosc 18(9):1176–1183
Ishibashi Y, Tsuda E, Fukuda A, Tsukada H, Toh S (2008) Intraoperative biomechanical evaluation of anatomic anterior cruciate ligament reconstruction using a navigation system: comparison of hamstring tendon and bone-patellar tendon-bone graft. Am J Sports Med 36(10):1903–1912
Izawa T, Okazaki K, Tashiro Y, Matsubara H, Miura H, Matsuda S, Hashizume M, Iwamoto Y (2011) Comparison of rotatory stability after anterior cruciate ligament reconstruction between single-bundle and double-bundle techniques. Am J Sports Med 39(7):1470–1477
Jarvela T (2007) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective, randomize clinical study. Knee Surg Sports Traumatol Arthrosc 15(5):500–507
Jarvela T, Moisala AS, Paakkala T, Paakkala A (2008) Tunnel enlargement after double-bundle anterior cruciate ligament reconstruction: a prospective, randomized study. Arthroscopy 24(12):1349–1357
Jarvela T, Moisala AS, Sihvonen R, Jarvela S, Kannus P, Jarvinen M (2008) Double-bundle anterior cruciate ligament reconstruction using hamstring autografts and bioabsorbable interference screw fixation: prospective, randomized, clinical study with 2-year results. Am J Sports Med 36(2):290–297
Kanaya A, Ochi M, Deie M, Adachi N, Nishimori M, Nakamae A (2009) Intraoperative evaluation of anteroposterior and rotational stabilities in anterior cruciate ligament reconstruction: lower femoral tunnel placed single-bundle versus double-bundle reconstruction. Knee Surg Sports Traumatol Arthrosc 17(8):907–913
Karlsson J, Irrgang JJ, van Eck CF, Samuelsson K, Mejia HA, Fu FH (2011) Anatomic single- and double-bundle anterior cruciate ligament reconstruction, part 2: clinical application of surgical technique. Am J Sports Med 39(9):2016–2026
Kawaguchi Y, Kondo E, Kitamura N, Kai S, Inoue M, Yasuda K (2011) Comparisons of femoral tunnel enlargement in 169 patients between single-bundle and anatomic double-bundle anterior cruciate ligament reconstructions with hamstring tendon grafts. Knee Surg Sports Traumatol Arthrosc 19(8):1249–1257
Kim SH, Jung YB, Song MK, Lee SH, Jung HJ, Lee HJ, Jung HS, Siti HT (2013) Comparison of double-bundle anterior cruciate ligament (ACL) reconstruction and single-bundle reconstruction with remnant pull-out suture. Knee Surg Sports Traumatol Arthrosc 25(1):70–77
Kim SJ, Chang JH, Kim TW, Jo SB, Oh KS (2009) Anterior cruciate ligament reconstruction with use of a single or double-bundle technique in patients with generalized ligamentous laxity. J Bone Joint Surg Am 91(2):257–262
Kim SJ, Jo SB, Kumar P, Oh KS (2009) Comparison of single- and double-bundle anterior cruciate ligament reconstruction using quadriceps tendon-bone autografts. Arthroscopy 25(1):70–77
Kondo E, Yasuda K, Azuma H, Tanabe Y, Yagi T (2008) Prospective clinical comparisons of anatomic double-bundle versus single-bundle anterior cruciate ligament reconstruction procedures in 328 consecutive patients. Am J Sports Med 36(9):1675–1687
Kopf S, Forsythe B, Wong AK, Tashman S, Anderst W, Irrgang JJ, Fu FH (2010) Nonanatomic tunnel position in traditional transtibial single-bundle anterior cruciate ligament reconstruction evaluated by three-dimensional computed tomography. J Bone Joint Surg Am 92(6):1427–1431
Kopf S, Pombo MW, Shen W, Irrgang JJ, Fu FH (2011) The ability of 3 different approaches to restore the anatomic anteromedial bundle femoral insertion site during anatomic anterior cruciate ligament reconstruction. Arthroscopy 27(2):200–206
Lao ML, Chen JH, Wang CJ, Siu KK (2013) Functional outcomes of Y-graft double-bundle and single-bundle anterior cruciate ligament reconstruction of the knee. Arthroscopy 29(9):1525–1532
Lee S, Kim H, Jang J, Seong SC, Lee MC (2012) Intraoperative correlation analysis between tunnel position and translational and rotational stability in single- and double-bundle anterior cruciate ligament reconstruction. Arthroscopy 28(10):1424–1436
Lui PP, Cheng YY, Yung SH, Hung AS, Chan KM (2012) A randomized controlled trial comparing bone mineral density changes of three different ACL reconstruction techniques. Knee 19(6):779–785
Maestro A, Sicilia A, Rodriguez L, Garcia P, Fdez-Lombardia J, Guerado E (2012) ACL reconstruction with single tibial tunnel: single versus double bundle. J Knee Surg 25(3):237–243
Misonoo G, Kanamori A, Ida H, Miyakawa S, Ochiai N (2011) Evaluation of tibial rotational stability of single-bundle vs. anatomical double-bundle anterior cruciate ligament reconstruction during a high-demand activity—a quasi-randomized trial. Knee 19(2):87–93
Miura K, Ishibashi Y, Tsuda E, Fukuda A, Tsukada H, Toh S (2010) Intraoperative comparison of knee laxity between anterior cruciate ligament-reconstructed knee and contralateral stable knee using navigation system. Arthroscopy 26(9):1203–1211
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
Monaco E, Labianca L, Conteduca F, De Carli A, Ferretti A (2007) Double bundle or single bundle plus extraarticular tenodesis in ACL reconstruction? A CAOS study. Knee Surg Sports Traumatol Arthrosc 15(10):1168–1174
Muneta T, Koga H, Mochizuki T, Ju YJ, Hara K, Nimura A, Yagishita K, Sekiya I (2007) A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy 23(6):618–628
Muneta T, Koga H, Morito T, Yagishita K, Sekiya I (2006) A retrospective study of the midterm outcome of two-bundle anterior cruciate ligament reconstruction using quadrupled semitendinosus tendon in comparison with one-bundle reconstruction. Arthroscopy 22(3):252–258
Musahl V, Voos JE, O’Loughlin PF, Choi D, Stueber V, Kendoff D, Pearle AD (2010) Comparing stability of different single- and double-bundle anterior cruciate ligament reconstruction techniques: a cadaveric study using navigation. Arthroscopy 26(9 Suppl):S41–S48
Nunez M, Sastre S, Nunez E, Lozano L, Nicodemo C, Segur JM (2012) Health-related quality of life and direct costs in patients with anterior cruciate ligament injury: single-bundle versus double-bundle reconstruction in a low-demand cohort—a randomized trial with 2 years of follow-up. Arthroscopy 28(7):929–935
Park SJ, Jung YB, Jung HJ, Shin HK, Kim E, Song KS, Kim GS, Cheon HY, Kim S (2010) Outcome of arthroscopic single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a preliminary 2-year prospective study. Arthroscopy 26(5):630–636
Petersen W, Tillmann B (1999) Structure and vascularization of the cruciate ligaments of the human knee joint. Anat Embryol 200(3):325–334
Plaweski S, Grimaldi M, Courvoisier A, Wimsey S (2011) Intraoperative comparisons of knee kinematics of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 19(8):1277–1286
Plaweski S, Petek D, Saragaglia D (2011) Morphometric analysis and functional correlation of tibial and femoral footprints in anatomical and single bundle reconstructions of the anterior cruciate ligament of the knee. Orthop Traumatol Surg Res 97(6 Suppl):S75–S79
Rue JP, Ghodadra N, Lewis PB, Bach BR Jr (2008) Femoral and tibial tunnel position using a transtibial drilled anterior cruciate ligament reconstruction technique. J Knee Surg 21(3):246–249
Sadoghi P, Muller PE, Jansson V, van Griensven M, Kropfl A, Fischmeister MF (2011) Reconstruction of the anterior cruciate ligament: a clinical comparison of bone-patellar tendon-bone single bundle versus semitendinosus and gracilis double bundle technique. Int Orthop 35(1):127–133
Samuelsson K, Desai N, McNair E, van Eck CF, Petzold M, Fu FH, Bhandari M, Karlsson J (2013) Level of evidence in anterior cruciate ligament reconstruction research: a systematic review. Am J Sports Med 41(4):924–934
Sastre S, Popescu D, Nunez M, Pomes J, Tomas X, Peidro L (2010) Double-bundle versus single-bundle ACL reconstruction using the horizontal femoral position: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 18(1):32–36
Seon JK, Park SJ, Lee KB, Yoon TR, Seo HY, Song EK (2009) Stability comparison of anterior cruciate ligament between double- and single-bundle reconstructions. Int Orthop 33(2):425–429
Seon JK, Song EK, Bae BH, Park SJ, Yoon TR, Cho SG, Lee JJ, Kim MS (2007) Kinematic study following double-bundle, anterior cruciate ligament reconstruction. Int Orthop 31(5):623–628
Shen W, Forsythe B, Ingham SM, Honkamp NJ, Fu FH (2008) Application of the anatomic double-bundle reconstruction concept to revision and augmentation anterior cruciate ligament surgeries. J Bone Joint Surg Am 90(Suppl 4):20–34
Shino K, Suzuki T, Iwahashi T, Mae T, Nakamura N, Nakata K, Nakagawa S (2010) The resident’s ridge as an arthroscopic landmark for anatomical femoral tunnel drilling in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 18(9):1164–1168
Siebold R, Branch TP, Freedberg HI, Jacobs CA (2011) A matched pairs comparison of single- versus double-bundle anterior cruciate ligament reconstructions, clinical results and manual laxity testing. Knee Surg Sports Traumatol Arthrosc 19(Suppl 1):S4–S11
Siebold R, Dehler C, Ellert T (2008) Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy 24(2):137–145
Song EK, Oh LS, Gill TJ, Li G, Gadikota HR, Seon JK (2009) Prospective comparative study of anterior cruciate ligament reconstruction using the double-bundle and single-bundle techniques. Am J Sports Med 37(9):1705–1711
Strauss EJ, Barker JU, McGill K, Cole BJ, Bach BR Jr, Verma NN (2011) Can anatomic femoral tunnel placement be achieved using a transtibial technique for hamstring anterior cruciate ligament reconstruction? Am J Sports Med 39(6):1263–1269
Streich NA, Friedrich K, Gotterbarm T, Schmitt H (2008) Reconstruction of the ACL with a semitendinosus tendon graft: a prospective randomized single blinded comparison of double-bundle versus single-bundle technique in male athletes. Knee Surg Sports Traumatol Arthrosc 16(3):232–238
Suomalainen P, Jarvela T, Paakkala A, Kannus P, Jarvinen M (2012) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomized study with 5-year results. Am J Sports Med 40(7):1511–1518
Suomalainen P, Moisala AS, Paakkala A, Kannus P, Jarvela T (2011) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: randomized clinical and magnetic resonance imaging study with 2-year follow-up. Am J Sports Med 39(8):1615–1622
Takeda Y, Sato R, Ogawa T, Fujii K, Naruse A (2009) In vivo magnetic resonance imaging measurement of tibiofemoral relation with different knee flexion angles after single- and double-bundle anterior cruciate ligament reconstructions. Arthroscopy 25(7):733–741
Tsarouhas A, Iosifidis M, Kotzamitelos D, Spyropoulos G, Tsatalas T, Giakas G (2010) Three-dimensional kinematic and kinetic analysis of knee rotational stability after single- and double-bundle anterior cruciate ligament reconstruction. Arthroscopy 26(7):885–893
Tsarouhas A, Iosifidis M, Spyropoulos G, Kotzamitelos D, Tsatalas T, Giakas G (2011) Tibial rotation under combined in vivo loading after single- and double-bundle anterior cruciate ligament reconstruction. Arthroscopy 27(12):1654–1662
Tsuda E, Ishibashi Y, Fukuda A, Tsukada H, Toh S (2009) Comparable results between lateralized single- and double-bundle ACL reconstructions. Clin Orthop Relat Res 467(4):1042–1055
van Eck CF, Gravare-Silbernagel K, Samuelsson K, Musahl V, van Dijk CN, Karlsson J, Irrgang JJ, Fu FH (2013) Evidence to support the interpretation and use of the anatomic anterior cruciate ligament reconstruction checklist. J Bone Joint Surg Am 95(20):e153
van Eck CF, Morse KR, Lesniak BP, Kropf EJ, Tranovich MJ, van Dijk CN, Fu FH (2010) Does the lateral intercondylar ridge disappear in ACL deficient patients? Knee Surg Sports Traumatol Arthrosc 18(9):1184–1188
van Eck CF, Samuelsson K, Vyas SM, van Dijk CN, Karlsson J, Fu FH (2011) Systematic review on cadaveric studies of anatomic anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 19(Suppl 1):S101–S108
van Eck CF, Schreiber VM, Mejia HA, Samuelsson K, van Dijk CN, Karlsson J, Fu FH (2010) “Anatomic” anterior cruciate ligament reconstruction: a systematic review of surgical techniques and reporting of surgical data. Arthroscopy 26(9 Suppl):S2–S12
Ventura A, Iori S, Legnani C, Terzaghi C, Borgo E, Albisetti W (2013) Single-bundle versus double-bundle anterior cruciate ligament reconstruction: assessment with vertical jump test. Arthroscopy 29(7):1201–1210
Ventura A, Legnani C, Terzaghi C, Borgo E (2012) Single- and double-bundle anterior cruciate ligament reconstruction in patients aged over 50 years. Arthroscopy 28(11):1702–1709
Volpi P, Cervellin M, Denti M, Bait C, Melegati G, Quaglia A, de Girolamo L (2010) ACL reconstruction in sports active people: transtibial DB technique with ST/G vs. transtibial SB technique with BPTB: preliminary results. Injury 41(11):1168–1171
Wang HJ, Ao YF, Chen LX, Gong X, Wang YJ, Ma Y, Leung KK, Yu JK (2011) Second-look arthroscopic evaluation of the articular cartilage after primary single-bundle and double-bundle anterior cruciate ligament reconstructions. Chin Med J (Engl) 124(21):3551–3555
Wang JH, Kim JG, Lee do K, Lim HC, Ahn JH (2012) Comparison of femoral graft bending angle and tunnel length between transtibial technique and transportal technique in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 20(8):1584–1593
Wang JQ, Ao YF, Yu CL, Liu P, Xu Y, Chen LX (2009) Clinical evaluation of double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: a prospective, randomized and controlled study. Chin Med J (Engl) 122(6):706–711
Woo SL, Kanamori A, Zeminski J, Yagi M, Papageorgiou C, Fu FH (2002) The effectiveness of reconstruction of the anterior cruciate ligament with hamstrings and patellar tendon. A cadaveric study comparing anterior tibial and rotational loads. J Bone Joint Surg Am 84-A(6):907–914
Xu Y, Ao YF, Wang JQ, Cui GQ (2014) Prospective randomized comparison of anatomic single- and double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 22(2):308–316
Yagi M, Kuroda R, Nagamune K, Yoshiya S, Kurosaka M (2007) Double-bundle ACL reconstruction can improve rotational stability. Clin Orthop Relat Res 454:100–107
Yasuda K, Kondo E, Ichiyama H, Tanabe Y, Tohyama H (2006) Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among 3 different procedures. Arthroscopy 22(3):240–251
Zaffagnini S, Bruni D, Marcheggiani Muccioli GM, Bonanzinga T, Lopomo N, Bignozzi S, Marcacci M (2011) Single-bundle patellar tendon versus non-anatomical double-bundle hamstrings ACL reconstruction: a prospective randomized study at 8-year minimum follow-up. Knee Surg Sports Traumatol Arthrosc 19(3):390–397
Zaffagnini S, Bruni D, Russo A, Takazawa Y, Lo Presti M, Giordano G, Marcacci M (2008) ST/G ACL reconstruction: double strand plus extra-articular sling vs double bundle, randomized study at 3-year follow-up. Scand J Med Sci Sports 18(5):573–581
Zaffagnini S, Signorelli C, Lopomo N, Bonanzinga T, Marcheggiani Muccioli GM, Bignozzi S, Visani A, Marcacci M (2011) Anatomic double-bundle and over-the-top single-bundle with additional extra-articular tenodesis: an in vivo quantitative assessment of knee laxity in two different ACL reconstructions. Knee Surg Sports Traumatol Arthrosc 20(1):153–159
Zhang Z, Gu B, Zhu W, Zhu L (2013) Double-bundle versus single-bundle anterior cruciate ligament reconstructions: a prospective, randomized study with 2-year follow-up. Eur J Orthop Surg Traumatol 24(4):559–565
Ziegler CG, Pietrini SD, Westerhaus BD, Anderson CJ, Wijdicks CA, Johansen S, Engebretsen L, LaPrade RF (2011) Arthroscopically pertinent landmarks for tunnel positioning in single-bundle and double-bundle anterior cruciate ligament reconstructions. Am J Sports Med 39(4):743–752
Acknowledgments
The authors did not receive any outside funding or grants directly related to the research presented in this manuscript. The Department of Orthopedic Surgery from the University of Pittsburgh receives funding from Smith and Nephew to support research related to reconstruction of the ACL.
Author information
Authors and Affiliations
Corresponding author
Additional information
All authors contributed to the preparation of this work.
Appendix: Complete search string for systematic electronic search
Appendix: Complete search string for systematic electronic search
(‘Anterior Cruciate Ligament’ [Mesh] OR ‘anterior cruciate ligament’ [tiab] OR ACL [tiab]) AND (‘Surgical Procedures, Operative’ [Mesh] OR surgical [tiab] OR surgery [tiab] OR reconstruction [tiab] OR reconstructive [tiab] OR reconstructed [tiab]) AND (English [lang] AND (‘1995’ [PDAT]: ‘3000’ [PDAT])).
Rights and permissions
About this article
Cite this article
Desai, N., Alentorn-Geli, E., van Eck, C.F. et al. A systematic review of single- versus double-bundle ACL reconstruction using the anatomic anterior cruciate ligament reconstruction scoring checklist. Knee Surg Sports Traumatol Arthrosc 24, 862–872 (2016). https://doi.org/10.1007/s00167-014-3393-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3393-7