Abstract
Purpose
Combinations of intra- and extra-articular procedures have been proposed for anterior cruciate ligament reconstruction with the aim of achieving an optimal control of translational and rotational knee laxities. Recently, the need for better reproducing the structural and functional behavior of the native anterior cruciate ligament led to the definition of anatomic double-bundle surgical approach. This study aimed to quantitatively verify whether the in vivo static and dynamic behavior obtained using over-the-top single-bundle with extra-articular tenodesis reconstruction was comparable to the results achieved by anatomic double-bundle approach.
Methods
Thirty-five consecutive patients, with an isolated anterior cruciate ligament injury, were included in the study. Standard clinical laxities and pivot-shift test were quantified before and after anterior cruciate ligament reconstruction by means of a surgical navigation system dedicated to kinematic assessment; displacements of medial and lateral compartment during stress tests were also analyzed.
Results
Single-bundle with extra-articular tenodesis approach presented statistically better laxity reduction in varus/valgus stress test at full extension and in internal/external rotation at 90° of flexion; lateral plasty controlled better the lateral compartment during drawer test and varus/valgus stress test both at 0° and 30° of flexion and both the compartments during internal/external rotation at 90° of flexion. On the other hand, pivot-shift phenomenon was better controlled by anatomic double-bundle reconstruction.
Conclusions
Both the reconstructions worked similarly for static knee laxity. The extra-articular procedure played an important role in better constraining the displacement of lateral tibial compartment, whereas the anatomic double-bundle reconstruction better restored the dynamic behavior of knee joint highlighted under pivot-shift stress test.
Study design
Case series.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The optimal anterior cruciate ligament (ACL) reconstruction is still a highly demanding clinical issue in orthopedic research [4, 1]. In vitro and in vivo studies highlighted that pure single-bundle (SB) ACL surgery was not completely able to functionally restore knee rotational stability patterns [26, 28].
In the past decades, several surgical reconstructions, combining intra- and extra-articular procedures, have been proposed with the aim of improving the control of both knee translational and rotational laxities. The application of a lateral tendon, as extra-articular plasty, had the advantage of mechanically acting on the lateral periphery of the joint, thus preventing the subluxation of the tibial plateaux and protecting overloads on the novel ACL graft [13].
The clinical need for better reproducing the anatomic structure and functional behavior of the native ACL led to the development of new surgical procedures, dedicated to better control rotational and dynamic laxities of the knee [22], and to reproduce the kinematics of the normal joint [29]; this clinical research specifically led to the development of double-bundle (DB) ACL reconstructions [1, 14, 23].
Short-term results obtained from the clinical and biomechanical comparisons performed both on DB and SB techniques are however still contradictory [4, 20, 21, 25]. Specifically, the surgical complexity of the DB technique, the increased risk of complications, the growing probability of surgical errors related to tunnels execution, and the additional costs for the National Health System raised issues about the feasibility and reasonability of these techniques [5].
In order to demonstrate the clinical superiority of DB techniques, several authors exploited computer-assisted surgery technology and in particular the use of navigation systems; this equipment allowed in fact the direct comparison of the ACL reconstruction techniques from the point of view of passive stability and laxity measurement [7, 17, 28, 30]. This knowledge improved the understanding of the biomechanical behavior given by the two bundles through the development of specific in vitro studies [16]; there are however some contradictory results in demonstrating the better performance of DB reconstruction in in vivo conditions, above all for what concerns static laxities [4]. Kinematic navigation systems additionally allowed to perform a quantitative analysis also of the pivot-shift (PS) phenomenon; this test was demonstrated to be the most reliable one in the quantitative assessment of dynamic stability [12]. A navigated PS test was therefore confirmed to be essential in quantitatively demonstrating the real efficacy of a specific surgical technique.
Although considered clinically antiquated, the single-bundle reconstruction with an extra-articular tenodesis presented some advantages related to positive clinical outcomes [15], technical ease, effectiveness of the surgical procedure, and extremely low costs [13]. In 2007, Monaco et al. [19] yet performed a first quantitative analysis of the positive influence of an extra-articular tenodesis in standard SB reconstruction on knee internal rotation during rotational stress test, acquiring the kinematic information by means of a navigation system. However, they did not include in their analyze the dynamic stability achievable by each reconstruction.
The goal of this work was to in vivo analyze the static and the dynamic behavior of knee joint quantifying the execution of both standard clinical stress tests and PS test. We specifically hypothesized that the clinical performance of the over-the-top SB reconstruction with an extra-articular tenodesis (SBLP) was however comparable to the more actual concept of anatomic DB (ADB) ACL reconstruction.
Materials and methods
We included in this study 35 consecutive patients with an isolated anterior cruciate ligament injury that underwent between September 2007 and April 2010 both anatomic double-bundle (ADB Group—15 patients) and over-the-top single-bundle with additional lateral plasty (SBLP Group—20 patients) ACL reconstruction. The average age was 34.0 ± 8.7 years, specifically 32.8 ± 7.1 years for ADB group and 35.2 ± 9.7 years for SBLP; no statistical differences were found in demography between the two groups (independent Student’s t test, n.s.). All the included lesions were preoperatively identified by the expert surgeon as chronic ACL lesions. Patients presenting previous ligament surgeries, additional ligament tears, or severe arthroscopically identified chondral defects were excluded from the analysis. Both reconstructions applied to SBLP and ADB group were executed by the same expert surgeon who moreover performed all the intraoperative kinematic tests. The choice of the specific reconstruction was consecutively performed by the expert surgeon according to predefined research protocols approved by the institutional review board of the institute. All ACL lesions were additionally confirmed by arthroscopy. Preoperative International Knee Documentation Committee (IKDC) objective grading identified 1 normal (B) grade (1 SBLP patient), 17 abnormal (C) grade (9 ADB and 8 SBLP patients), and 17 severely abnormal (D) grade (7 ADB and 10 SBLP patient). Differences in preoperative IKDC score between ADB and SBLP group were not statistically significant (Pearson Chi-square, n.s.).
Navigation system and surgical procedure
In order to evaluate joint laxity and passive kinematics, we adopted a surgical navigation system (BLU-IGS, Orthokey, Lewes, Delaware, DE, USA) equipped with a software specifically dedicated to kinematic acquisitions (KLEE, Orthokey, Lewes, Delaware, DE, USA) [16]. The reliability of the navigation system, demonstrated both in static laxity tests and pivot-shift analysis, was previously discussed and analyzed [11, 12, 18]; literature specifically reported very good reliability in pivot-shift analysis (with a mean intra-tester ICC about 0.98 for the determined parameters) and an intra-tester repeatability of about 1 mm for drawer/Lachman, 1° for varus/valgus stress test and 2° for internal/external rotation stress test.
Standard surgical equipment was used to perform both the analyzed ACL surgical reconstructions. In particular, both anatomic double-bundle ACL reconstruction, as reported by Shen et al. [24], and over-the-top single-bundle with the additional extra-articular tenodesis on the lateral compartment, as reported by Marcacci et al. [13] were performed using semitendinosus and gracilis tendons. The preparation of the patients and the proposed surgical techniques was not modified by the introduction of the navigation system.
Testing protocol
After performing the anatomic registration phase required by the navigation system [18] and before fixing the grafts, the operating surgeon manually performed at maximum force the clinical laxity tests [17] and the pivot-shift test [12]. In particular, according to the defined acquisition protocol, the surgeon performed:
-
anterior/posterior displacement at 30° of flexion (Lachman test—AP30) and at 90° of flexion (drawer test—AP90), internal/external rotation at 30° (IE30) and 90° of flexion (IE90), varus/valgus test at 0° (VV0) and 30° of flexion (VV30) in order to highlight knee static stability.
-
Pivot-shift (PS) test was used to determine dynamic stability. PS test was strictly executed following the clinical grading defined by Jacob et al. [8].
The reliability of both laxity tests performed at maximum force and the pivot-shift was evaluated in previous studies [11, 14, 18].
After fixing the graft as described by the specific surgical procedures, the previously described clinical tests were repeated and acquired by the navigation system. During the whole set of tests and reconstructions, the examiner was always the same and he was blinded for test quantitative results in order to avoid bias in the acquisitions.
Data and statistical analysis
The whole set of kinematic data was acquired and off-line elaborated by means of MATLAB framework (The Mathworks Inc., Natick, Massachusetts, MA, USA).
In particular, the global amount of varus/valgus rotation, internal/external rotation, and antero/posterior displacement obtained during the test were analyzed for ACL-deficient and ACL-reconstructed knees. In order to highlight the possible specific contribution of the extra-articular tenodesis, we also analyzed the antero/posterior displacement of both lateral and medial compartment during AP30, AP90, IE30, and IE90, and maximal medial and maximal lateral joint opening during VV0 and VV30, i.e., the maximal distance between the epicondyle and the corresponding reference point on the tibial plateaux during VV tests (Fig. 1).
According to Lopomo et al. [12], we analyzed the maximal anterior displacement of the lateral tibial compartment and the area included by the translation during PS phenomenon with respect to flexion/extension angle, and additionally the posterior acceleration reached by the lateral compartment during tibial reduction [10].
Comparisons of preoperative and postoperative laxities were made using paired Student’s t test within the same group; comparison between ADB and SBLP groups was performed using independent Student’s t test, analyzing both starting preoperative condition and postoperative one, in order to verify both the uniformity between the two groups and which were the differences introduced by each specific reconstruction. The presence of outliers from data parameters was checked using the Thompson Tau method [2]. Statistical significance for all the tests was set at 95% (p = 0.05).
Results
In Table 1, we reported for each reconstruction the global amount of AP translations, VV rotation, and IE rotation related to each performed static laxity test. Statistically significant reduction in the global amount of static laxities was observed for both ADB and SBLP reconstruction (p < 0.05), due to the introduction of the graft. Furthermore, no statistical difference was found between the 2 groups for neither pre- nor postoperative absolute values (n.s.).
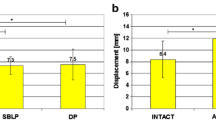
Statistically significant differences were instead identified between the 2 groups considering the value of laxity reduction (i.e., pre–post values) as highlighted in Fig. 2. Specifically, we found differences in laxity reduction during VV0 and during IE90.
Focusing on the behavior of each compartment (Table 2), we found in each group a statistically significant reduction in the global AP displacement and joint opening (p < 0.05). Furthermore, no statistical difference was found between ADB and SBLP group for neither pre- nor postoperative absolute value (n.s.). On the other hand, statistically significant differences were found between the 2 groups considering the value of reduction as highlighted in Fig. 3. In particular, we found differences in lateral compartment displacement during AP90, in maximal lateral joint opening during VV0 and VV30, and in both medial and lateral AP displacement during IE90.
Laxity reduction of the lateral compartment (Lateral) and the medial compartment (Medial): differences in AP displacements for AP30/AP90 and IE30/IE90 tests were analyzed, whereas differences in maximal medial/lateral joint opening were reported for VV0/VV30 tests. The differences between pre- and post-reconstruction are reported for each kinematic test, highlighting both SBLP and ADB group. * p < 0.05
All the dynamic parameters analyzed for the lateral tibial plateaux (i.e., the peak of displacement in anterior direction, the corresponding area included by the curve and acceleration due to tibial reduction) were significantly reduced in both the groups (p < 0.0005). For what concerns the differences introduced by the two surgical techniques, the two groups presented similar preoperative areas (n.s.), whereas ADB patients revealed less “hysteretic” area (that is correlated to knee dynamic laxity) after the reconstruction (p = 0.0005). Moreover, there were no statistical differences in anterior translation before the reconstruction (n.s.), whereas the anterior displacement, obtained during PS test, was significantly higher in SBLP patients after the reconstruction (p = 0.0009). The accelerations considered during tibial reduction were statistically the same in preoperative condition (n.s.), whereas SBLP patients presented more acceleration after the reconstruction (p = 0.0060) compared to ADB. The obtained results for PS test are reported in Fig. 4.
Discussion
One of the most important finding we highlighted in the present study was the different behavior expressed by two different ACL reconstructions in controlling static and dynamic instability. Specifically, we found that the additional extra-articular procedure—acting on the lateral periphery of the joint—was more effective in controlling lateral joint opening during VV stress both at 0° and 30° of flexion confirming also what was reported by Bignozzi et al. [3]. Furthermore, the lateral plasty was able to give a better contribution in restraining AP translation of the lateral compartment at 90° of flexion. Differently from what highlighted by Monaco et al. [19] for static rotation, we found that an additional constraint applied to the lateral side could achieve better results in containing IE rotation at 90° of flexion, acting on the translation of both lateral and medial compartment. On the other hand, ADB showed to have a better performance in controlling dynamic laxity [12] that has been proven to be correlated to PS phenomenon [8, 9]. In the performed study, we found that all ACL-deficient knees showed positive PS test before surgery, revealing huge values in the tibial subluxation and in the acceleration reached by the tibia during the reduction. In this study, ADB revealed to have a better control of the dynamic knee laxity, since both the areas and the peaks of the lateral compartment displacement during PS test presented a higher reduction when compared to SBLP.
The obtained results confirmed the biomechanical principle, acting on the periphery in order to obtain a better lever arm and thus to control rotational motion. ADB reconstruction, better reproducing the native insertion areas, allowed on the other hand a better control of the combined translations and rotations (i.e., the dynamic behavior of the knee joint). Moreover, also the acceleration reached during PS test was more reduced in ADB group, thus ensuring a more physiologic smooth kinematics.
The present study presented some limitations; specifically, we performed the measurements for VV, IE, and AP laxities during surgery with an inflated tourniquet that might have increased muscle tension influencing test outcomes. Test conditions remained, however, the same for all the tests and patients, thus ensuring data congruence and granting data comparison. Moreover, although our tests were manually performed at manual maximum force by the same surgeon—thus not directly controlling loads and torques—the reliability of these measurements has already been proven [12, 17] and it was congruent with the differences we highlighted between the 2 groups.
This study represented one of the first quantitative analysis performed in in vivo conditions by means of a navigation system on both static and dynamic knee stability, achievable with the use of two different surgical approaches: the anatomic DB and the over-the-top SB combined with extra-articular tenodesis. Computer-assisted surgery has been demonstrating the advantage of extremely precise quantification for both the static and the dynamic behavior of the knee joint [6, 17, 28, 30].
Conclusion
Concluding our results suggested that the use of additional extra-articular procedure could be taken into consideration as an easy surgical procedure in patient not involved in high demanding sport activities, even if the anatomic double-bundle reconstruction could allow a better control of the dynamic instability of the joint. Moreover—although further analyses of these patients at long-term follow-up are required—the better kinematic pattern obtained with ADB could be able to avoid the degenerative joint diseases often observed even in highly satisfactory ACL reconstruction [27].
References
American Society of Mechanical Engineer (2006) Test uncertainty. ANSI/ASME PTC 19.1–2005—Part I
Bignozzi S, Zaffagnini S, Lopomo N et al (2009) Does a lateral plasty control coupled translation during antero-posterior stress in single-bundle ACL reconstruction? An in vivo study. Knee Surg Sports Traumatol Arthrosc 17:65–70
Boyer J, Meislin RJ (2010) Double-bundle versus single-bundle ACL reconstruction. Bull NYU Hosp Joint Dis 68:119–126
Brophy RH, Pearle AD (2009) Single-bundle anterior cruciate ligament reconstruction: a comparison of conventional, central, and horizontal single-bundle virtual graft positions. Am J Sports Med 37:1317–1323
Colombet PD, Robinson JR (2008) Computer-assisted, anatomic, double-bundle anterior cruciate ligament reconstruction. Arthroscopy 24:1152–1160
Crawford C, Nyland J, Landes S et al (2007) Anatomic double bundle ACL reconstruction: a literature review. Knee Surg Sports Traumatol Arthrosc 15:946–964
Ferretti A, Monaco E, Labianca L et al (2009) Double-bundle anterior cruciate ligament reconstruction: a comprehensive kinematic study using navigation. Am J Sports Med 37:1548–1553
Jakob RP, Stäubli HU, Deland JT (1987) Grading the pivot shift. Objective tests with implications for treatment. J Bone Joint Surg Br 69:294–299
Kocher MS, Steadman JR, Briggs KK et al (2004) Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med 32:629–634
Kuroda R, Hoshino Y, Nagamune K et al (2008) Intraoperative measurement of pivot shift by electromagnetic sensors. Oper Tech Orthop 18:190–195
Lopomo N, Bignozzi S, Martelli S et al (2009) Reliability of a navigation system for intra-operative evaluation of antero-posterior knee joint laxity. Comput Biol Med 39:280–285
Lopomo N, Zaffagnini S, Bignozzi S et al (2010) Pivot-shift test: analysis and quantification of knee laxity parameters using a navigation system. J Orthop Res 28:164–169
Marcacci M, Zaffagnini S, Iacono F et al (1998) Arthroscopic intra- and extra-articular anterior cruciate ligament reconstruction with gracilis and semitendinosus tendons. Knee Surg Sports Traumatol Arthrosc 6:68–75
Marcacci M, Molgora AP, Zaffagnini S et al (2003) Anatomic double-bundle anterior cruciate ligament reconstruction with hamstrings. Arthroscopy 19:540–546
Marcacci M, Zaffagnini S, Giordano G et al (2009) Anterior cruciate ligament reconstruction associated with extra-articular tenodesis: a prospective clinical and radiographic evaluation with 10–13 year follow-up. Am J Sports Med 37:707–714
Markolf KL, Park S, Jackson SR, McAllister DR (2008) Simulated pivot-shift testing with single and double-bundle anterior cruciate ligament reconstructions. J Bone Joint Surg Am 90(8):1681–1689
Martelli S, Zaffagnini S, Bignozzi S et al (2007) KIN-Nav navigation system for kinematic assessment in anterior cruciate ligament reconstruction: features, use, and perspectives. Proc Inst Mech Eng H 221:725–737
Martelli S, Lopomo N, Bignozzi S et al (2007) Validation of a new protocol for navigated intraoperative assessment of knee kinematics. Comput Biol Med 37:872–878
Monaco E, Labianca L, Conteduca F et al (2007) Double bundle or single bundle plus extraarticular tenodesis in ACL reconstruction? A CAOS study. Knee Surg Sports Traumatol Arthrosc 15:1168–1174
Park SJ, Jung YB, Jung HJ et al (2010) Outcome of arthroscopic single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a preliminary 2 year prospective study. Arthroscopy 26(5):630–636
Sastre S, Popescu D, Núñez M et al (2010) Double-bundle versus single-bundle ACL reconstruction using the horizontal femoral position: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 18(1):32–36
Sbihi A, Franceschi JP, Christel P et al (2004) Anterior cruciate ligament reconstruction: biomechanical comparison on cadaver specimens using a single or double hamstring technique. Rev Chir Orthop Reparatrice Appar Mot 90:643–650
Schreiber VM, Van Eck CF, Fu FH (2010) Anatomic double-bundle ACL reconstruction. Sports Med Arthrosc 18:27–32
Shen W, Jordan S, Fu F (2007) Review article: anatomic double bundle anterior cruciate ligament reconstruction. J Orthop Surg (Hong Kong) 15:216–221
Song EK, Oh LS, Gill TJ et al (2009) Prospective comparative study of anterior cruciate ligament reconstruction using the double-bundle and single-bundle techniques. Am J Sports Med 37:1705–1711
Tashman S, Kopf S, Fu FH (2008) The kinematic basis of ACL reconstruction. Oper Tech Sports Med 16:116–118
Vairo GL, McBrier NM, Miller SJ et al (2010) Premature knee osteoarthritis after anterior cruciate ligament reconstruction dependent on autograft. J Sport Rehabil 19:86–97
Yamamoto Y, Ishibashi Y, Tsuda E et al (2008) Single- versus double-bundle anterior cruciate ligament reconstruction results using navigation: the japanese experience. Oper Tech Orthop 18:173–180
Yoo YS, Jeong WS, Shetty NS et al (2010) Changes in ACL length at different knee flexion angles: an in vivo biomechanical study. Knee Surg Sports Traumatol Arthrosc 18(3):292–297
Zaffagnini S, Klos TV, Bignozzi S (2010) Computer-assisted anterior cruciate ligament reconstruction: an evidence-based approach of the first 15 years. Arthroscopy 26:546–554
Acknowledgments
The authors would like to thank all the nurses and staff at Istituto Ortopedico Rizzoli (Bologna, Italy) and also all the people at Laboratorio di Biomeccanica ed Innovazione Tecnologica (Bologna, Italy)—in particular Mr. Emil Ferretti for his great contribution in the management of our technological equipment.
Conflict of interest
The authors certify that the above-named manuscript describes our own original work on properly conducted and documented research and that all authors contributed to the conception and design of the study or acquisition of data, analysis and interpretation of data, and revising the final version of the article. All authors believe that the manuscript represents honest work. This paper has not been submitted to, or published by, any other journal, nor will it be submitted to any other journal without prior written notification to the Editor in Chief that the manuscript is to be withdrawn.
The authors declare that there was neither financial nor personal relationship including employment, consultancies, stock ownership, honoraria, paid expert testimony, patent applications/registration, and grants with other people or organization that could inappropriately influence (bias) their work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zaffagnini, S., Signorelli, C., Lopomo, N. et al. Anatomic double-bundle and over-the-top single-bundle with additional extra-articular tenodesis: an in vivo quantitative assessment of knee laxity in two different ACL reconstructions. Knee Surg Sports Traumatol Arthrosc 20, 153–159 (2012). https://doi.org/10.1007/s00167-011-1589-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1589-7