Abstract
Purpose
To compare objective measures of in vivo joint laxity between patients treated with single-bundle (SB) or double-bundle (DB) anterior cruciate ligament (ACL) reconstructions.
Methods
Sixty-four patients matched by age, height, weight, and that had undergone unilateral SB or DB hamstring ACL reconstruction participated in this study. Bilateral anterior tibial translation (ATT) was recorded using the KT1000 arthrometer, and a robotic testing system was used to assess side-to-side differences in rotational characteristics. Each reconstruction was evaluated to determine how well it mimicked the anteroposterior (AP) and rotational biomechanics of the normal knee. A reconstruction was defined as mimicking the normal knee if ATT and internal rotation (IR) were within 3 mm and 3.5°, respectively.
Results
Side-to-side differences in ATT were significantly higher for the SB group (2.2 ± 1.4 mm) than the DB group (1.1 ± 1.0 mm, P = 0.001). While relative side-to-side differences in IR did not differ between the SB (1.3°) and DB groups (1.1°, P = 0.82), absolute IR differences were significantly less with the DB reconstruction (2.1° vs. 4.7°, P = 0.001). A significantly greater percentage of DB patients (81%, P = 0.0003) had both ATT and IR similar to the normal knee, compared to 34% of the SB patients; however, IKDC subjective scores did not differ between groups. Regardless of technique, patients with the greatest rotational laxity of their non-operative knee demonstrated significantly worse IKDC scores.
Conclusion
DB reconstruction resulted in reduced side-to-side differences in both ATT and IR. The DB technique more consistently reproduced the biomechanical profile of the uninjured limb than did the SB technique without increasing the risk of over-constraining the knee.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite demonstrating inferior knee stability when compared to double-bundle (DB) ACL reconstruction, [14, 15, 18, 19, 21, 29, 43, 50, 51] single-bundle (SB) ACL reconstruction techniques have provided successful clinical outcomes for many patients [2, 5, 12, 31, 34, 41, 42]. Subjective scores provide useful information about a patient’s postoperative recovery however, may be too blunt of a tool to judge differences between two surgical techniques. Patient-reported function scores have been determined to be influenced by pain and/or function of the non-operative limb [17, 28, 46]. In addition, factors associated with postoperative rehabilitation such as range of motion and quadriceps strength may influence subjective scores, again questioning the sole use of these measures for clinical decision-making.
While short-term clinical results may not be affected by reduced stability, the long-term implications of reduced stability have been demonstrated to be involved with the etiology of osteoarthritis in ACL reconstructed knees [9, 10, 20, 48]. To ensure both short- and long-term clinical success, accurately assessing true knee instability in all its forms is vital prior to, during, and following ACL reconstruction. Subjective tests of joint stability may limit our ability to truly gauge potential differences between ACL reconstruction techniques. The ligaments, tendons, and capsular structures are interdependent, work together as a system, and are related to one another in a complex manner [30]. Characterizing the direction and magnitude of knee laxity is correspondingly complex, as it is related not only to the relative stiffness of these structures, but also to their three-dimensional positions and orientations.
Specifically, while results of the pivot shift test have been previously reported to be significantly correlated with subjective outcome measures, [22] this test has been described as being a difficult test for clinicians to interpret [23]. It is also difficult to attain an accurate impression of laxity during the pivot shift in the presence of muscle guarding as evidenced by the dramatic differences between pivot shift results when testing injured patients in an awake or anesthetized states. Due to the inherent variability of subjective manual laxity testing, an objective clinical comparison of the potential biomechanical advantages of DB reconstruction techniques has not been performed to date.
The purpose of this study was to compare instrumented tests of knee stability between patients treated with an arthroscopic four-tunnel DB ACL reconstruction to those with a SB ACL reconstruction with autologous quadruple hamstrings. We hypothesized that the DB technique would demonstrate improved anterior and rotational stability compared to the SB ACL reconstruction.
Materials and methods
Patients with a minimum of one-year follow-up following SB or DB hamstring ACL reconstruction [43] were included in a matched-pairs analysis in order to compare the clinical outcomes, patient satisfaction, and manual and instrumented knee stability of the two procedures. Inclusion criteria for the matched-pair analysis were as follows: age, time from injury to surgery, uninjured contralateral knee, and no severe injury to secondary restraints at time of operation and follow-up. Examples of severe injury or secondary restraints included additional knee ligament injuries, previous knee ligament surgery, arthritic changes of Outerbridge grade 3 or 4, [32] malalignment, and pathology to the patella. Patients were examined carefully during pre- and postoperative clinical evaluation, and any evidence of other ligament injury was also noted at the time of surgery in order to identify and exclude those patients with evidence of a combined ligament injury from this matched-pairs analysis.
The study was conducted in November, 2007, and 68 patients were included in the matched-pair analysis. Patients were selected to participate in the current investigation from the patient populations of two participating surgeons provided they met the inclusion criteria, matching was possible, and they were willing to attend the clinical follow-up for testing. Prior to participation, patients provided informed consent for the IRB-approved protocol. At the time of testing, 3 patients were identified as having an injured opposite extremity and 1 patient did not attend the follow-up, leaving an active sample of 64 patients. The groups were well matched, as there were no differences in age, sex, height, weight, or follow-up (Table 1).
Surgical techniques
Skin incisions were identical for both the SB and DB groups, and no notchplasties were performed. Both techniques have been previously reported, and tunnel locations for the SB and DB techniques are presented in Figs. 1 and 2 [43]. The SB ACL reconstruction utilized a double loop semitendinosis and gracilis graft; therefore, both tendons were looped over one 20-mm EndoButton CLTM. After positioning of the graft, the femoral EndoButton CLTM was flipped and the tibial biodegradable interference screw (Smith and Nephew Endoscopy, Mansfield, MA, USA) was inserted. The 30-mm long screw was the same diameter as the tibial bone tunnel or 1 mm larger [44]. In four-tunnel DB ACL reconstruction (Fig. 2), the semitendinosus tendon (for the AM bundle) and the gracilis tendon (for the PL bundle) were looped over a 20-mm EndoButton CLTM (Smith and Nephew Endoscopy, Mansfield, MA, USA). After positioning of the two grafts, the two femoral EndoButton CLTM were flipped. Tibial AM bundle fixation was by means of a 8- or 9-mm by 23-mm biodegradable interference screw (Arthrex Inc, Naples, FL) having the same diameter or 1 mm larger as the AM bone tunnel, and tibial PL bundle fixation was by means of a 7 × 23 mm biodegradable interference screw (Arthrex Inc., Naples, FL) for all patients. The AM bundle was fixed in 60° and the PL bundle in 10° of knee flexion. No bone grafting was used in either tunnel [43].
Tibial and femoral tunnel placement for the single-bundle reconstruction technique. Reprinted from Arthroscopy: the Journal of Arthroscopic and Related Research, [43] with permission from the Arthroscopy Association of North America
Tibial and femoral tunnel placement for the double-bundle reconstruction technique. Reprinted from Arthroscopy: the Journal of Arthroscopic and Related Research, [43] with permission from the Arthroscopy Association of North America
Data collection
At clinical follow-up, patients were asked to complete the International Knee Documentation Committee (IKDC) 2000 questionnaire during the same visit in order to calculate the subjective IKDC score. All patients were examined by a single, experienced orthopedic surgeon. This independent surgeon was not affiliated with the operating surgeons’ facility, was not the operative surgeon for any of the study patients, and was blinded to the surgical technique during data collection. The patients themselves were not blinded to the type of procedure at follow-up. Anterior stability of both limbs was assessed using a manual maximum test with the KT1000™ (MEDmetric® Corp., San Diego, CA), and side-to-side differences in anterior tibial translation (ATT) were calculated between the reconstructed and normal knee.
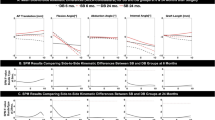
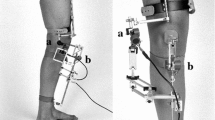
Rotational laxity was examined using a custom robotic knee testing system (RKT, Fig. 3) using previously reported testing procedures [3]. Patients were positioned supine with knees flexed to approximately 25°. Simultaneous bilateral testing was performed with every patient, with the RKT cycling the lower extremities into tibial external rotation until the torque threshold of 5.65 Nm was achieved, at which point the RKT rotated the tibia into internal rotation (IR) until the threshold of 5.65 Nm was again achieved. Three preconditioning cycles were performed, followed by four test cycles. Independent examiners using the RKT were blinded to the surgical technique. All rotational stability data were collected by independent surgeons and researchers that are not affiliated with the operating surgeons’ facility. All data were collected over the course of 2 days, and the surgeons and researchers responsible for data collection were not informed of each patient’s surgical technique until after all data had been collected. There were two separate, but identical RKT systems used during testing. The RKT consisted of a special system of servo motors and ankle and hip entrapment devices designed to isolate rotation at the knee and ankle, and the rotational measures have previously demonstrated excellent reliability (ICC = 0.97) [3].
In order to describe the loading characteristics of the joint specifically during IR, the torque and rotational displacement data for the concentric loading phase of each patient’s four cycles of IR were used for analysis. The slope between 0 and 1 Nm was calculated in an effort to describe the compliance of the joint in a neutral position, and the slope between 4.65 and 5.65 Nm was also calculated in an effort to describe the endpoint stiffness (Fig. 4). For both neutral compliance and endpoint stiffness, values were expressed as Nm/° with lower values being associated with a “looser” joint and higher values being associated with a “tighter” joint.
Internal rotation loading curve from 0 to 5.65 Nm of torque for a single patient. For this patient, the reconstructed knee had a greater degree of maximal internal rotation at 5.65 Nm of torque than the normal knee. The slope of Line A is representative of the neutral compliance of the normal knee, and slope of Line B represents the neutral compliance of the reconstructed knee. The slope of Line C represents the endpoint stiffness of the normal knee, and the slope of Line D represents the endpoint stiffness of the reconstructed knee
Statistical analyses
Two-tailed, independent t-tests were used to compare dependent variables between the group of SB and DB ACL patients. Dependent variables included: IKDC subjective scores, relative and absolute side-to-side differences in tibial IR (°) and anterior translation (mm), as well as neutral compliance (Nm/°), and IR endpoint stiffness (Nm/°) of the reconstructed and normal contralateral knees. Absolute side-to-side differences were defined as the absolute value of the difference in either translation or rotation between the two knees and were calculated in order to determine the magnitude of differences regardless of direction. Relative side-to-side differences were defined as the amount of either translation or rotation of the operative knee subtracted from the value measured of the contralateral knee. It has been previously suggested that DB reconstruction may over-constrain the joint, relative side-to-side differences were calculated in order to determine whether there was a directional bias in one or both the surgical techniques. The variability of side-to-side differences in both ATT and IR was compared between the two groups using an F-test of the equality of two variances. In order to evaluate the relationships between the dependent variables, Spearman’s rho correlations coefficients were calculated.
Fisher’s exact tests were used to compare the prevalence of knees with side-to-side differences within 3 mm and 3.5° of ATT and IR, respectively, between the two surgical groups. The 3 mm of anterior displacement was based the original work of Daniel et al. [8] that 3 mm of additional anterior tibial displacement during KT1000 testing when compared to the healthy contralateral limb was consistent with the presence of an ACL injury. The target of 3.5° was used as it was consistent with a previous in vivo study of knee kinematics in which patients with unilateral ACL tears demonstrated 3.5° greater tibial IR with the ACL deficient knee than with the healthy knee [11].
In a previous unpublished study (Branch et al. 2005), we determined that patients with greater rotational laxity of the non-operative limb demonstrated significantly reduced subjective postoperative outcomes. In the current study, we attempted to evaluate whether patients with greater maximal IR of the contralateral healthy knee demonstrated lower IKDC subjective scores, regardless of surgical technique. Patients were divided into quartiles based on tibial IR of the normal knee. We then compared IKDC between three groups: the 25% (16 patients) with the greatest amount of IR, the 50% that surrounded the mean (32 patients), and the 25% (16 patients) with the least amount of IR. By classifying the three groups, the data was not normally distributed, and a Kruskal–Wallis test was used to compare the groups.
All analyses were performed using Statistical Package for the Social Sciences v 17.0 (SPSS Inc., Chicago, IL), and an α-level of P ≤ 0.05 was considered significant.
Results
There were no differences in IKDC subjective scores between the SB (79.4, 95% CI, 73.9–84.9) and DB groups (82.2, 95% CI, 76.5–87.8; P = 0.49). Side-to-side differences in anterior translation were significantly lower for the DB group (1.1 mm, 95% CI, 0.8–1.5 mm) than the SB group (2.2 mm, 95% CI, 1.7–2.7 mm, P = 0.001). Relative side-to-side differences in maximal IR did not differ between SB (1.3°, 95% CI, −0.6 to 3.3°) and DB groups (1.1°, 95% CI, 0.3–1.9°; P = 0.82); however, the DB group demonstrated significantly lower absolute side-to-side differences (2.1°, 95% CI, 1.6–2.6°; P = 0.001) than the SB group (4.7°, 95% CI, 3.6–5.8°). The lack of relative differences coupled with the significant absolute differences suggests that the magnitude of side-to-side differences is greater with the SB technique, and that neither technique consistently resulted in under- or over-constraint. In addition, the variability of the SB technique was significantly greater for both side-to-side differences in ATT (P = 0.05) and IR (P = 0.0007) than that of the DB technique.
A significantly greater proportion (26/32, 81%) of the DB patients demonstrated symmetrical reconstructions, whereas 11/32 (34%) SB patients were reconstructed within 3 mm of anterior translation and 3.5° of IR (P = 0.0003, Fig. 5). No patients in either group had greater ATT of the normal knee when compared to the reconstructed knee. In the SB group, 11 were within 3 mm and 3.5°, nine were within 3 mm but under-constrained more than 3.5°, seven were within 3 mm but over-constrained more than 3.5°, three were under-constrained in anterior translation but were within 3.5° of IR, and two were under-constrained in both translation and rotation. In the DB group, 26 were within 3 mm and 3.5°, and the remaining six knees were within 3 mm but were under-constrained in rotation.
Graphical representation of the side-to-side differences in internal rotation (x-axis) and anterior translation (y-axis) for each patient treated with a single-bundle reconstruction and b double-bundle reconstruction. Side-to-side values were calculated by subtracting values measured with the operative knee from the values measured with the normal knee. Positive values are indicative of under-constraint, and negative values are indicative of over-constraint
The knees reconstructed with the SB technique demonstrated significantly reduced neutral compliance (0.21 Nm/°, 95% CI, 0.18–0.23 Nm/°) when compared to the DB group (0.24 Nm/°, 95% CI, 0.22–0.26; P = 0.03). Lower slopes are indicative of increased compliance, or a “looser” knee. The two groups did not differ in endpoint compliance of the operative limb, nor did they differ in either neutral compliance or endpoint stiffness of the non-operative contralateral knee. Furthermore, when dividing the entire sample population of 64 patients into three groups based on maximal IR of the non-operative limb, the most lax group demonstrated significantly lower IKDC postoperative scores than the other two groups Fig. 6.
Regardless of reconstruction technique, patients were divided into three groups based on the maximum internal rotation of the contralateral, non-operative knee (Most lax 25% (16 knees, "Lax"), the middle 50% that surrounded the mean (32 knees, "Normal"), and the tightest 25% (16 knees, "Tight"). The Lax group demonstrated significantly lower postoperative IKDC Subjective Scores than both the Normal and Tight groups
Discussion
The most important findings of this study were that DB ACL reconstruction demonstrated superior anteroposterior (AP) and rotational laxity when compared to SB reconstruction and that a much greater percentage of DB reconstructions recreated AP and rotational stability similar to the contralateral healthy knee. The second most important finding was that regardless of the type of reconstruction that was used, the patients with the greatest rotational laxity of the contralateral healthy knee demonstrated significantly worse IKDC scores. The following discussion has therefore been separated into two sections addressing (1) the comparison of SB and DB ACL reconstruction techniques and (2) considerations related to the laxity of the non-operative limb.
Comparison of the SB and DB techniques
The results supported the hypotheses that the DB technique would demonstrate reduced anterior and rotational laxity and more consistently mimicked that of the uninjured contralateral limb. The side-to-side anterior laxity results in the current study demonstrated a statistically significant difference between the two techniques of 1.1 mm. These results are consistent with the results of a 2008 meta-analysis reported mean reduction in side-to-side differences in anterior translation of 0.52 mm with a DB reconstruction [27]. More recent studies have reported that DB techniques did not result in statistically significant side-to-side translation reductions, demonstrating 0.6-mm [43] and 0.2-mm [15] reductions when compared to a SB technique at a short-term follow-up. Regardless of whether a study demonstrated statistically significant differences between the techniques, the clinical relevance of sub-millimeter differences between the techniques has been questioned [27].
Increased laxity has been associated with not only abnormal translation, but also abnormal rotation of the tibia with respect to the femur [10]. With increased laxity comes greater and more abrupt joint motion, as well as less congruent contact between poorly fitting joint surfaces [10]. The two most common long-term failure mechanisms after ACL reconstruction are the development of osteoarthritis (OA) requiring surgical intervention or failure of the graft, and both may be dependent on joint laxity.
Increased laxity may result in damage to the articular cartilage and/or menisci, which further contribute to the progression of OA [10]. While increased laxity in each of the three planes of motion has been individually implicated in the development of OA, [10, 20, 24, 35, 37–40, 45, 47, 49] excessive tibial rotation has been specifically suggested to be involved with the progression of knee OA [33, 45]. Furthermore, 20–25% of poor outcomes following ACL reconstruction have been suggested to be attributed to rotational instability [52].
Recent studies performed at the time of surgery (time zero) using computer-assisted navigation have reported conflicting results when comparing SB and DB reconstructions. In a study of 90 patients, Ishibashi et al. [16] reported improved anterior and rotational stability with a DB technique, highlighting the importance of both the AM and PL bundles. On the contrary, in a study of 20 patients, Ferretti et al. reported that DB reconstruction provided no additional stability when compared to a more anatomic SB technique [13]. While studies such as these are necessary to improve our understanding of joint kinematics at the time of surgery, it remains unclear if anterior and rotational laxity measurements determined at time zero influence the long-term clinical and radiographic outcomes. Furthermore, the performance of intraoperative manual evaluations is still subject to the same inherent limitations of inter- and intra-tester reliability as the manual clinical exam and does not allow for bilateral comparison [4].
The current study utilized instrumented laxity evaluation systems to compare SB and DB reconstructions at median follow-up of more than 15 months. The results of the current study demonstrated that DB reconstruction did indeed restore the native function of the ACL more consistently than the SB technique. Relative side-to-side differences in tibial IR did not differ between groups; however, the DB demonstrated significantly lower absolute side-to-side differences. These results highlight the concept that solely looking at group means may not provide a clear comparison of surgical techniques. If errors are evenly distributed both above and below the mean, incorrect interpretation of results may occur. In the current study, relative differences were similar between groups; however, when evaluating the absolute magnitude of error from the targeted range of ±3.5° of tibial IR, the SB group had significantly larger side-to-side differences. While either technique may result in the restoration of normal knee rotational kinematics, less variable results were demonstrated with the DB technique, resulting in more consistent restoration of rotational kinematics. The differences in variability between the SB and DB group are clearly depicted in Fig. 5.
Many comparative clinical studies have reported improved pivot shift results with DB reconstruction techniques [6, 15, 18, 19, 29, 43, 51]; however, recent cadaveric studies have suggested that improved stability achieved with DB techniques may come at a price [25, 26, 36]. Over-correction of rotational laxity may reduce the incidence of grade 1 pivot shift tests, [15, 43] but may also over-constrain the joint, thus potentially increasing the risk of early graft failure by increasing forces in the PL graft [25, 26, 36]. Cook et al. [7] demonstrated contrary results in their cadaveric study. The authors utilized a custom 6 degree of freedom robot to recreate the pivot shift test in the laboratory. Using 125 N anterior load with combined 10 Nm valgus and 5 Nm IR torques, they reported that the DB technique yielded 81% recovery of the mechanics of the ACL-intact state, compared to only 43% of the recovery yielded by the SB technique [7]. The current clinical investigation very closely matched the results of Cook et al., as our results demonstrated that the DB technique more consistently recreated the patients’ normal knee biomechanics. Side-to-side differences in anterior translation and IR were significantly lower for the DB group, and 81% of the DB reconstructions closely matched the biomechanical profile of the normal knee compared to 34% of the SB reconstructions. Furthermore, none of the DB reconstructions were over-constrained in rotation.
Laxity of the non-operative limb
In addition to the comparison of the two surgical techniques, we also compared IKDC subjective scores between patients based on the rotational laxity of their contralateral normal knee. In a previous study, we determined that patients with a unilateral ACL tear had increased tibial IR of the contralateral normal knee when compared to a group of healthy volunteers [3]. Building on this concept, when we divided the current study patients into groups based on rotational laxity of the normal knee, the group with the greatest amount of tibial rotation demonstrated significantly worse IKDC scores when compared to the other groups. In short, excessive tibial IR of the normal knee may be a risk factor for ACL injury and may also be a risk factor for a poor postoperative outcomes following ACL reconstruction. Considering the statement from Zaffagnini et al. [52] that 20–25% of poor outcomes following ACL reconstruction may be attributed to rotational instability, we suggest that this subgroup of rotationally lax patients may require more complex reconstruction to control rotation. Future studies are needed to determine whether additional stability provided by double-bundle reconstruction or reconstruction with a lateral extra-articular augmentation results in improved clinical outcomes in this subgroup of rotationally lax patients.
Limitations
This study was not without limitation. The average follow-up of patients in this study was 16 months. It has been reported that the properties of the graft may continue to change up to 2 years following surgery, and it is possible that the results reported at 16 months could differ from those potentially collected at a later follow-up. In addition, we attempted to control for ankle motion with the use of dorsiflexion wedges; however, motion at that joint did occur during testing. While motion did occur, by testing a subset of 48 knees with the integrated use of electromagnetic sensors, we were able to identify the relative amount of rotation that could be attributed to the knee, and these results were demonstrated to have excellent reliability. While this measurement system has demonstrated excellent reliability, validation studies comparing results of this non-invasive system with other direct measures of skeletal motion, such as surgical navigation, have not been performed to date. The measurements derived from this non-invasive system may have been influenced by soft tissue artifact and/or voluntary muscle activation. In addition, while the instrumented laxity tests were performed in a single degree of knee flexion, which is consistent with the positioning used during clinical examination, it is unclear if similar results could be expected at other flexion angles.
The reader should be cautioned that we only evaluated one SB and DB technique, and these results may not be able to be generalized to all ACL reconstruction techniques, graft types, fixation methods, etc. The results of the current study suggest that achieving appropriate AP and rotational biomechanics can be very difficult with this SB technique. Other SB techniques have been reported to allow for more anatomic tunnel placement [1], and future instrumented clinical studies are warranted to determine whether these more anatomic SB techniques are able to more consistently reproduce the biomechanical characteristics of the normal knee than the techniques used in the current study. Future studies are also necessary to determine whether a more anatomic reconstruction using either a single- or double-bundle technique improves postoperative outcomes for the apparent difficult group of patients who demonstrate the greatest IR of their normal contralateral knee.
Conclusion
The theoretical advantage/benefit of anatomic ACL reconstruction is the potentially improved ability to restore biomechanical and clinical characteristics similar to that of the uninjured joint [53]. While the current results suggest that this can be achieved with either a SB or DB technique, DB ACL reconstruction more consistently reproduced the biomechanical profile of the uninjured limb than did the SB technique. The DB technique demonstrated significantly reduced side-to-side differences in ATT and IR, and a significantly greater proportion of the DB reconstructions were within 3 mm of anterior translation and 3.5° of IR when compared to the healthy contralateral knee.
References
Abebe E, Mooreman CI, Dziedzic T, Spritzer C, Cothran R, Taylor D, Garrett WJ, DeFrate L (2009) Femoral tunnel placement during anterior cruciate ligament reconstruction: an in vivo imaging analysis comparing transtibial and 2-incision tibial tunnel-independent techniques. Am J Sports Med 37:1904–1911
Anderson A, Snyder R, Lipscomb AS (1994) Anterior cruciate ligament reconstruction using the semitendinosus and gracilis tendons augmented by the losee iliotibial band tenodesis. A long-term study. Am J Sports Med 22:620–626
Branch T, Browne J, Campbell J, Siebold R, Freedberg H, Arendt E, Lavoie F, Neyret P, Jacobs C (2009) Rotational laxity greater in patients with contralateral anterior cruciate ligament injury than healthy volunteers. Knee Surg Sports Traumatol Arthrosc. doi: 10.1007/s00167-009-1010-y. Available electronically December 18, 2009
Branch T, Mayr H, Browne J, Campbell J, Stoehr A, Jacobs C (2010) Instrumented examination of anterior cruciate ligament injuries: minimizing flaws of the manual clinical examination. Arthroscopy 26:997–1004
Buss D, Warren R, Wickiewicz T, Galinat B, Panariello R (1993) Arthroscopically assisted reconstruction of the anterior cruciate ligament with use of autogenous patellar-ligament grafts. J Bone Joint Surg (Am) 75-A:1346–1355
Colombet P, Robinson J, Jambou S, Allard M, Bousquet V, de Lavigne C (2006) Two-bundle, four-tunnel anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 14:629–636
Cook A, Koh J, Ren Y, Zhang L (2009) Anatomic single-bundle versus double-bundle anterior cruciate ligament reconstruction: a biomechanical analysis of stability. Proc AAOSM 2009 Specialty Day:36
Daniel D, Malcom L, Losse G, Stone M, Sachs R, Burks R (1985) Instrumented measurement of anterior laxity of the knee. J Bone Joint Surg Am 67:720–726
Daniel D, Stone M, Dobson B (1994) Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med 22:632–644
Dayal N, Chang A, Dunlop D, Hayes K, Chang R, Cahue S, Song J, Torres L, Sharma L (2008) The natural history of anteroposterior laxity and its role in knee osteoarthritis progression. Arthritis Rheum 52:2343–2349
DeFrate L, Papannagari R, Gill T, Moses J, Pathare N, Li G (2006) The 6 degrees of freedom kinematics of the knee after anterior cruciate ligament deficiency: an in vivo imaging analysis. Am J Sports Med 34:1240–1246
Feller J, Webster K (2003) A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med 31:564–573
Ferretti A, Monaco E, Labianca L, Conteduca F, De Carli A (2008) Double-bundle anterior cruciate ligament reconstruction: a computer-assisted orthopaedic surgery study. Am J Sports Med 36:760–766
Hamada M, Shino K, Horibe S, Mitsuoka T, Miyama T, Shiozaki Y, Mae T (2001) Single- versus bi-socket anterior cruciate ligament reconstruction using autogenous multiple-stranded hamstring tendons with EndoButton femoral fixation: a prospective study. Arthroscopy 17:801–807
Hofbauer M, Valentin P, Kdolsky R, Ostermann R, Graf A, Figl M, Aldrian S (2009) Rotational and translational laxity after computer-navigated single- and double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. doi: 10.1007/s00167-009-0992-9. Available electronically November 28, 2009
Ishibashi Y, Tsuda E, Yamamoto Y, Tsukada H, Toh S (2009) Navigation evaluation of the pivot-shift phenomenon during double-bundle anterior cruciate ligament reconstruction: is the posterolateral bundle more important? Arthroscopy 25:488–495
Jacobs C, Christensen C (2009) Correlations between Knee Society Function Scores and functional force measures. Clin Orthop Relat Res 467:2414–2419
Jarvela T (2007) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective, randomize clinical study. Knee Surg Sports Traumatol Arthrosc 15:500–507
Jarvela T, Moisala A-S, Sihvonen R, Jarvela S, Kannus P, Jarvinen M (2008) Double-bundle anterior cruciate ligament reconstruction using hamstring autografts and bioabsorbable interference screw fixation: prospective, randomized, clinical study with 2-year results. Am J Sports Med 36:290–297
Jonsson H, Riklund-Ahlstrom K, Lind J (2004) Positive pivot shift after ACL reconstruction predicts later osteoarthritis: 63 patients followed 5–9 years after surgery. Acta Orthop Scand 75:594–599
Kim S-J, Chang J-H, Kim T-W, Jo S-B, Oh K-S (2009) Anterior cruciate ligament reconstruction with use of a single or double-bundle technique in patients with generalized ligamentous laxity. J Bone Joint Surg (Am) 91-A:257–262
Kocher M, Steadman J, Briggs K, Sterett W, Hawkins R (2004) Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med 32:629–634
Lane C, Warren R, Pearle A (2008) The pivot shift. J Am Acad Orthop Surg 16:679–688
Leitze Z, Losee R, Jokl P, Johnson T, Feagin J (2005) Implications of the pivot shift in the ACL-deficient knee. Clin Orthop Related Res 436:229–236
Markolf K, Park S, Jackson S, McAllister D (2008) Simulated pivot-shift testing with single and double-bundle anterior cruciate ligament reconstructions. J Bone Joint Surg (Am) 90-A:1681–1689
Markolf K, Park S, Jackson S, McAllister D (2009) Anterior-posterior and rotatory stability of single and double-bundle anterior cruciate ligament reconstructions. J Bone Joint Surg (Am) 91-A:107–118
Meredick R, Vance K, Appleby D, Lubowitz J (2008) Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med 36:1414–1421
Mizner R, Snyder-Mackler L (2005) Altered loading during walking and sit-to-stand is affected by quadriceps weakness after total knee arthroplasty. J Orthop Res 23:1083–1090
Muneta T, Koga H, Mochizuki T, Ju Y-J, Hara K, Nimura A, Yagishita K, Sekiya I (2007) A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy 23:618–628
Noyes F, Grood E, Butler D, Malek M (1980) Clinical laxity tests and functional stability of the knee: biomechanical concepts. Clin Orthop Related Res 146:84–89
O’Neill D (1996) Arthroscopically assisted reconstruction of the anterior cruciate ligament. A prospective randomized analysis of three techniques. J Bone Joint Surg (Am) 78-A:803–813
Outerbridge R (1961) The etiology of chondromalacia patellae. J Bone Joint Surg (Br) 43-B:752–757
Ristanis S, Stergiou N, Patras K, Tsepis E, Moraiti C, Georgoulis A (2006) Follow-up evaluation 2 years after ACL reconstruction with bone-patellar tendon-bone graft shows that excessive tibial rotation persists. Clin J Sport Med 16:111–116
Sajovic M, Vengust V, Komadina R, Tavcar R, Skaza K (2006) A prospective, randomized comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: five-year follow-up. Am J Sports Med 34:1933–1940
Schmitt L, Rudolph K (2007) Influences on knee movement strategies during walking in persons with medial knee osteoarthritis. Arthritis Rheum 57:1018–1026
Seon J, Gadikota H, Wu J-L, Sutton K, Gill T, Li G (2010) Comparison of single- and double-bundle anterior cruciate ligament reconstructions in restoration of knee kinematics and anterior cruciate ligament forces. Am J Sports Med 38:1559–1567
Sharma L, Cahue S, Song J, Hayes K, Pai Y-C, Dunlop D (2003) Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum 48:3359–3370
Sharma L, Eckstein F, Song J, Guermazi A, Prasad P, Kapoor D, Cahue S, Marshall M, Hudelmaier M, Dunlop D (2008) Relationship of meniscal damage, meniscal extrusion, malalignment, and joint laxity to subsequent cartilage loss in osteoarthritic knees. Arthritis Rheum 58:1716–1726
Sharma L, Hayes K, Felson D, Buchanan T, Kirwan-Mellis G, Lou C, Pai Y-C, Dunlop D (1999) Does laxity alter the relationship between strength and physical function in knee osteoarthritis? Arthritis Rheum 42:25–32
Sharma L, Lou C, Felson D, Dunlop D, Kirwan-Mellis G, Hayes K, Weinrach D, Buchanan T (1999) Laxity in healthy and osteoarthritic knees. Arthritis Rheum 42:861–870
Shelbourne K, Urch S (2000) Primary anterior cruciate ligament reconstruction using the contralateral autogenous patellar tendon. Am J Sports Med 28:651–658
Shelbourne K, Vanadurongwan B, Gray T (2007) Primary anterior cruciate ligament reconstruction using contralateral patellar tendon autograft. Clin Sports Med 26:549–565
Siebold R, Dehler C, Ellert T (2008) Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy 24:137–145
Siebold R, Ellert T, Metz S, Metz J (2008) Tibial insertions of the anteromedial and posterolateral bundles of the anterior cruciate ligament: morphometry, arthroscopic landmarks, and orientation model for bone tunnel placement. Arthroscopy 24:154–161
Stergiou N, Ristanis S, Moraiti C, Georgoulis A (2007) Tibial rotation in anterior cruciate ligament (ACL)-deficient and ACL-reconstructed knees. A theoretical proposition for the development of osteoarthritis. Sports Med 37:601–613
Stratford P, Kennedy D (2006) Performance measures were necessary to obtain a complete picture of osteoarthritic patients. J Clin Epidemiol 59:160–167
van der Esch M, Steultjens M, Knol D, Dinant H, Dekker J (2006) Joint laxity and the relationship between muscle strength and functional ability in patients with osteoarthritis of the knee. Arthritis Rheum 55:953–959
van der Hart C, van den Bekerom M, Patt T (2008) The occurrence of osteoarthritis at a minimum of ten years after reconstruction of the anterior cruciate ligament. J Orthop Surg Res 3:24. doi:10.1186/1749-799X-3-24. Available electronically June 10, 2008
Wada M, Imura S, Baba H, Shimada S (1996) Knee laxity in patients with osteoarthritis and rheumatoid arthritis. Br J Rheumatol 35:560–563
Yagi M, Kuroda R, Nagamune K, Yoshiya S, Kurosaka M (2006) Double-bundle ACL reconstruction can improve rotational stability. Clin Orthop Related Res 454:100–107
Yasuda K, Kondo E, Ichiyama H, Tanabe Y, Tohyama H (2006) Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among 3 different procedures. Arthroscopy 22:240–251
Zaffagnini S, Bignozzi S, Martelli S, Imakiire N, Lopomo N, Marcacci M (2006) New intraoperative protocol for kinematic evaluation of ACL reconstruction: preliminary results. Knee Surg Sports Traumatol Arthrosc 14:811–816
Zantop T, Petersen W, Sekiya J, Musahl V, Fu F (2006) Anterior cruciate ligament anatomy and function relating to anatomical reconstruction. Knee Surg Sports Traumatol Arthrosc 14:982–992
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Branch, T.P., Siebold, R., Freedberg, H.I. et al. Double-bundle ACL reconstruction demonstrated superior clinical stability to single-bundle ACL reconstruction: a matched-pairs analysis of instrumented tests of tibial anterior translation and internal rotation laxity. Knee Surg Sports Traumatol Arthrosc 19, 432–440 (2011). https://doi.org/10.1007/s00167-010-1247-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-010-1247-5