Abstract
We conducted a prospective randomised study of anatomical single-bundle (A-SB group) versus double-bundle (A-DB group) anterior cruciate ligament (ACL) reconstruction using the hamstrings tendons. Twenty patients with unilateral ACL deficiency were randomised into two groups. We created the bone tunnels at the position of the original insertion of the anteromedial bundle footprint and posterolateral bundle footprint in the A-DB group and at the central position between these two bundles in the A-SB group. All of the patients were tested before ACL reconstruction and one year after surgery. The KT-1000 measurements, isokinetic muscle peak torque and heel-height difference were evaluated and the general knee condition was assessed by Lysholm score. For pre- and postoperative stability assessment, we used the six-degrees-of-freedom of knee kinematic measurement system using an electromagnetic device (the EMS) for quantitative assessment during the Lachman test and the pivot shift test. There were no significant differences in the KT-1000 measurements, isokinetic muscle peak torque, heel-height difference, and Lysholm score at one-year follow-up between these two groups. The EMS data showed there were significant differences in the acceleration of the pivot shift test between the operated knee and the contralateral normal knees in the A-SB group. In conclusion, clinical outcomes were equally good in both groups. However, the EMS data showed the anatomical double-bundle ACL reconstruction tended to be biomechanically superior to the single-bundle reconstruction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) disruption is a common cause of anterior knee instability, particularly as a result of sports activities. On the basis of several biomechanical studies [1–4], double-bundle ACL reconstruction, which is designed to reproduce both the anteromedial bundle (AMB) and the posterolateral bundle (PLB), has become increasingly popular over the past decade, because this procedure has been able to more closely restore the rotational stability compared with the conventional single-bundle technique [5, 6]. Zantop et al. reported that the AMB and the PLB stabilise the knee joint in response to anterior tibial loads and combined rotatory loads in a synergistic way [7]. Yagi et al. reported that anatomical double-bundle ACL reconstruction guaranteed similar results to the physiologically intact knee and provided a better control of rotational stability compared with AM single-bundle and PL single-bundle reconstruction [5].
Traditionally ACL reconstruction procedures have focused on reproducing only the AMB. These methods may not completely restore the complex function of the native ACL [8–11]. Ristanis et al. suggested that single-bundle ACL reconstruction did not restore the functional dynamic stability of the knee in terms of internal-external rotation of the tibia even when tibial translation was restored [12]. By contrast, some studies have suggested that the rotational torque can be controlled by making a femoral tunnel at the anatomical position compared with that made at the anteromedial single-bundle reconstruction [8, 13]. Loh et al. suggested that lateralised femoral tunnel placement could lead to better control of abnormal knee kinematics especially against a rotational load [13].
Several in vivo and in vitro comparative studies of single-bundle versus double-bundle ACL reconstruction were performed and the integrity of double-bundle reconstruction was introduced [14–18]. However, a meta-analysis which compared the clinical outcome of single-bundle versus double-bundle ACL reconstruction was recently reported by Meredick et al. [19]. They showed that double-bundle reconstruction does not result in clinically significant differences in the KT-1000 measurement and pivot shift test compared with single-bundle ACL reconstruction. However, operative techniques of single-bundle reconstruction were inconsistent in this study. Most of them described the femoral tunnel placement as clock face references, although the shapes of the medial surface of the lateral condyles were three-dimensional. As Fu and Shen mentioned [20, 21], the clock face position may have been unclear in 3D description and we suspected that these studies were not suitable for comparative study of anatomical single-bundle versus double-bundle ACL reconstruction.
The purpose of this study was to assess the clinical outcome of anatomical single-bundle versus double-bundle ACL reconstruction using a prospective randomised study design and to evaluate the quantitative knee kinematics data using an electromagnetic measurement system in these two procedures. We postulated that anatomical double-bundle reconstruction results in better restoration of knee kinematics than the anatomical single-bundle procedure.
Materials and methods
Patients
A prospective randomised study was carried out on 20 consecutive patients with chronic ACL deficiency in one knee and had an indication for ACL reconstruction. They were randomised with closed envelopes into two groups according to their sex and age. The first group including ten patients underwent anatomical single-bundle ACL (A-SB group). The second group of ten patients underwent the anatomical double-bundle reconstruction (A-DB group). Details of the surgical procedures are described later. None of the patients had medial, lateral, or posterior instability as evaluated by physical examinations or had any history of surgery on either knee. Complete ACL tear was confirmed in every patient and no chondral lesions in the medial or lateral condyles were observed arthroscopically at the time of surgery. In the A-SB group, there were five women and five men with an average age of 24.7 ± 11.8 (mean ± standard deviation) years. In the A-DB group, there were five women and five men with an average age of 25.2 ± 12.1 years. They were followed-up in person for 12.0 ± 2.3 months in the A-SB group and 13.5 ± 3.2 in the A-DB group. No statistical differences were noted among these two groups with regard to sex, age, and the follow-up period (Table 1). All patients followed the same postoperative program. Jogging was permitted at four months with a gradual return to full sports activity, including competitive sports, at eight months.
All patients were informed that they were going to be in a study. Institutional review board approval was obtained from our institution prior to proceeding with this study and our protocol was also approved.
Surgical technique
An experienced surgeon performed or directly supervised all surgery. The semitendinosus and gracilis tendons were harvested for ACL graft. To make a fair comparison, the total number of strands prepared for the implanted graft was standardised at four in these two groups. The actual graft constitution in each group was as follows: double semitendinosus tendon for the anteromedial bundle (AMB) and double gracilis tendon for the posterolateral bundle (PLB) graft in the double-bundle reconstruction, and combined double semitendinosus and gracilis tendons in the single-bundle reconstruction.
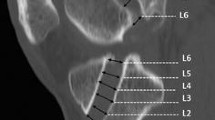
First, to perform the anatomical reconstruction, we identified the original position of the AMB and PLB insertion for both the femoral and tibial side. Arthroscopy confirmed the centre of the femoral attachment of the PLB was located on a line drawn vertically from the point of tibiofemoral contact at 90° of knee flexion, at a distance of 5–8 mm from the edge of the joint cartilage. In contrast, the location of the centre of the AMB insertion point was 5–8 mm medial to the posterolateral bundle [6]. We created the bone tunnels at the position of the original insertion of the AMB and PLB footprint in the A-DB group (Fig. 1 A-1,2) and at the central position between these two bundles in the A-SB group (Fig. 1 B-1,2) by an outside-in tibial drill hole and an inside-out femoral drill hole.
For the anatomical double-bundle reconstruction, we created two femoral and two tibial tunnels to reproduce the AMB and PLB. First, we created the femoral tunnel for the PLB through a far anteromedial accessory portal. After placing a pilot pin, the femoral PLB tunnel was created using the cannulated drills for the ENDOBUTTON System (Smith & Nephew Endoscopy, Andover, MA, USA), and the tunnel size and depth was matched to the size of the PLB. Two tibial tunnels were created in the next step. The tibial drill guide was adjusted to a 45° angle sagittal to the horizontal tibial surface for both AMB and PLB drilling. For frontal angles, tibial drill holes were created at approximate angles of 20° and 45° medially for the AMB and PLB. The femoral tunnel of the AMB was created through a transtibial AMB drill hole after all the other drill holes were created. Continuous Loop Endo Button (Smith & Nephew Endoscopy, Andover, MA, USA) was used for femoral fixation and No.2 Ethybond Sutures (Ethicon, Somerville, NJ, USA) were tied to the unlooped end of the hamstrings graft. The PLB graft was passed through using the lead suture. After passing the PLB graft, the AMB graft was passed through using the transtibial guide wire. For the graft fixation, a single 6.5-mm cancellous post screw with washer (Synthes, Pennsylvania, PA, USA) was used and sutures were tied to a fixation post screw. During tibial fixation, manual maximum force was applied to the PLB graft at 15° and to the AMB at 60° of knee flexion.
For the anatomical single-bundle reconstruction, single femoral and single tibial tunnels were created at the central position between the original insertion of the AMB and PLB. The femoral tunnel was made through the medial accessory portal. The graft was fixed to the femur and tibia in the same manner as in the anatomical double-bundle reconstruction. During tibial fixation, manual maximum force was applied at 15° of knee flexion.
Evaluations
A single surgeon performed preoperative assessment and follow-up examinations one year after surgery. Heel-height difference (HHD) was measured to evaluate the lack of extension [22]. Knee extensor and flexor peak torques were isokinetically measured with a Biodex Dynamometer (Biodex Corp., Shirley, New York, USA) at 60°/sec. Clinical results were evaluated using Lysholm score and one leg hop. Manual knee laxity test (the Lachman test and the pivot shift test) and anterior laxity at manual maximum stress using KT-1000 arthrometer (MEDmetric Corp, San Diego, CA, USA) [23, 24] were also evaluated. Results of the arthrometric measurements were recorded as the side-to-side difference between the injured and uninjured knees.
For pre- and postoperative stability assessment, we used the six-degrees-of-freedom of knee measurement system with an electromagnetic device (FASTRAK, Polhemus, VT, USA) [25–27]. For quantitative comparison, the side-to-side difference of anterior tibial translation during the Lachman test and the acceleration of the sudden reduction of the tibia during the pivot shift test were used for evaluation [25].
Electromagnetic measurement system
The configuration of the electromagnetic measurement system is shown in Fig. 2. Six-degrees-of-freedom of knee kinematics was measured using an electromagnetic device (FASTRAK, Polhemus, Colchester, VT, USA). The detail of this electromagnetic measurement system was reported by Hoshino et al. [25]. This system consists of a transmitter that produces an electromagnetic field and three electromagnetic receivers (Fig. 2a). Two of the receivers are used for motion measurement of the tibia and femur and are attached to a plastic brace by a circumferential Velcro strap placed on the thigh and the calf (Fig. 2b). A third receiver attached to a specially-made stylus is used for digitising anatomical landmarks before the six-degrees-of-freedom kinematics measurement is performed. Seven anatomical landmarks were acquired to define the coordinate system (Fig. 2c). The acquired position data of each landmark was converted to the relative position of the electromagnetic receivers attached to either the thigh or the calf and used to provide each coordinate system on the femur and the tibia.
a Configuration of the newly-developed electromagnetic measurement system. b Two of the receivers were attached to a plastic brace by a circumferential Velcro strap placed on the thigh and on the lower leg. A third receiver was attached to a specially-made stylus. c The stylus was used for digitising anatomical landmarks before the six-degrees-of-freedom of knee kinematics measurement was performed
Six-degrees-of-freedom of knee kinematics were calculated by modifying the principle of a three-cylinder open-chain mechanism proposed by Grood et al. using the bone axis of the femur instead of the mechanical axis [28]. The six degrees of freedom were described in terms of flexion, external rotation, adduction, anterior translation, distraction, and lateral shift. These six parameters represent a joint static relationship between the femur and tibia.
Statistical evaluation
The statistical evaluation was carried out by means of the Student t-test for manual knee laxity, KT-1000 arthrometric measurements, heel height difference, knee extensor and flexor muscle peak torques, Lysholm score and one legged hop. The analysis of variance (ANOVA) was used for the comparison of the pre- and post-operative electromagnetic measurement data. A multiple comparison with the Fischer’s PLSD was applied only to the data considered significant by the ANOVA. Significance level was determined at 5%.
Results
No postoperative complication occurred among either group and all patients returned to their previous sports activity level. At one-year follow-up, in the pivot-shift test, three patients were evaluated as grade 1+ in the A-SB group and one patient was evaluated as grade 1+ in the A-DB group (Table 2). In the Lachman test, there was no significant difference between the two groups (Table 2). According to the KT-1000 arthrometric measurements, preoperative mean side-to-side differences were 5.2 ± 1.5 mm in the A-SB group and 6.0 ± 2.7 mm in the A-DB group. At the one-year follow-up, mean side-to-side differences were 1.8 ± 1.7 mm in the A-SB group and 0.7 ± 1.8 mm in the A-DB group. In both groups, the side-to-side differences were significantly improved; however, there were no statistical differences between two groups postoperatively (Fig. 3). Postoperative knee extensor and flexor muscle isokinetic peak torques at 60º/s were 92.1 ± 13.7% and 90.2 ± 17.8%, respectively, in the A-SB group and 84.9 ± 20.4% and 92.0 ± 14.6 % in the A-DB group, respectively. Postoperative knee extension limitation with heel height differences were 11.0 ± 15.2 mm in the A-SB group and 18.8 ± 16.9 mm in the A-DB group. Lysholm scores were 96.1 ± 4.5 in the A-SB group and 94.3 ± 8.8 in the A-DB group. In one-legged hop, percent ratios of contralateral normal knees were 88.2 ± 12.0% in the A-SB group and 89.9 ± 15.2% in the A-DB group. There were no significant differences for these three physical findings between these two groups (Table 3).
In the quantitative measurement of the Lachman test, side to side differences were −1.23 ± 5.5 mm in the A-SB group and −0.47 ± 4.9 mm in the A-DB group; these differences were not significant (Fig. 4).
By contrast, a significant difference was found in the quantitative measurement of the pivot shift test using our newly developed electromagnetic measurement system at one-year follow-up. In the A-SB group, the acceleration during the pivot shift test in the operative knees was −940.36 ± 524.36 mm/s2, while the contralateral knees was −640.13 ± 137.68 mm/s2. There was significant difference between the operated knees and the contralateral intact knees (P < 0.05) in the A-SB group. However, in the A-DB group, no significant difference was found between the operated knees and the contralateral intact knees (the acceleration during the pivot shift test in the operative knees was −701.48 ± 225.81 mm/s2 and that of the contralateral intact knees was −685.11 ± 261.79 mm/s2) (Fig. 5).
Quantitative evaluation of the pivot shift test using the electromagnetic measurement system. There was significant difference between the operated knees and the contralateral intact knees in the anatomical single-bundle (A-SB) group. However, in the anatomical double-bundle (A-DB) group, no significant difference was found between the operated knees and the contralateral intact knees. The significance level was 5%
Discussion
The goal of ACL reconstruction is to restore normal knee kinematics and to allow the patients to return to a previous level of function. Several biomechanical studies demonstrate that double-bundle ACL reconstruction improves anterior tibial translation and rotation [1, 2, 29]. Other reports support the integrity of this procedure, which was designed to reproduce the AMB and PLB, and it has theoretic advantages in controlling rotational torque proved by robotic study [3, 4, 7]. Moreover, several in vivo studies have also supported these in vitro biomechanical reports [15, 16, 18, 30]. Yasuda et al. reported that side-to-side KT-2000 measurements and pivot shift examination of anatomical double-bundle ACL reconstruction showed significantly better results than in the single-bundle procedure [18]. Although there were biomechanical advantages in double-bundle ACL reconstruction, clinical results did not show any significant improvement over the conventional procedure [31]. A meta-analysis of single-bundle versus double-bundle ACL reconstruction from Meredick et al. also supported these results. They reported that double-bundle reconstruction did not result in clinically significant differences in the KT-1000 measurement or pivot shift test [19].
However, several series of comparative or randomised studies were reported in which operative techniques of single-bundle reconstruction were inconsistent. Yasuda et al. compared the outcomes of AM single-bundle reconstruction, non-anatomical double-bundle reconstruction and anatomical double-bundle reconstruction [18]. The meta-analysis by Meredick et al. also included several trials of the single-bundle technique [19]. This is unlikely to represent the true outcome of single-bundle versus double-bundle ACL reconstruction. Regarding the femoral tunnel position, Järvelä, Muneta, Asagumo and Streich et al. described by the o’clock position [15, 16, 32, 33]. However, Fu and Shen et al. have stated that the position of the clock varies depending on whether the clock face references the anterior versus the posterior aspect of the notch and does not adequately address the depth of the medial surface on the lateral condyle. Additionally, the clock position varies with knee flexion angles [20, 21].
In the single-bundle reconstruction, some studies have suggested that the rotational torque can be controlled by making a femoral tunnel at the anatomical position compared to that made at the anteromedial single-bundle reconstruction [8, 13]. Loh et al. suggested that lateralised femoral tunnel placement could lead to better control of abnormal knee kinematics, especially against a rotational load [13]. We focused on making bone tunnels at the anatomical insertion in both groups.
Additionally, to compare the clinical evaluation quantitatively, Kasović et al. demonstrated the electromyographic difference among two different techniques using bone–patella tendon–bone graft, hamstrings tendon graft in ACL reconstruction and a healthy group [34]. In a two-year follow-up, the hamstrings tendon graft group achieved the maximum amplitude of biceps femoris muscle signal statistically significantly later than the bone–patella tendon–bone group, whereas the rectus femoris muscle in the hamstrings tendon graft group improved statistically significantly earlier than the healthy group in that study. Thus, electromyographic evaluation might be useful for one of the quantitative evaluation devices after ACL surgery. We used the three-dimensional electromagnetic measurement system and collected the knee kinematics data during the Lachman test and the pivot shift test to compare the knee instability quantitatively, because subjective non-parametrical assessments of these tests lack objectivity.
Our data show no significant difference in the manual Lachman test, the manual pivot shift test, the knee extension with heel height difference, the knee flexion and extension muscle peak torques at 60 degrees, the Lysholm score and one-legged hop. Only the acceleration of the sudden tibial reduction during the pivot shift test, which is a quantitative evaluation of pivot shift, showed better restoration in double-bundle reconstruction than in anatomical single-bundle reconstruction. Our early results seem to agree with the results of previously published biomechanical studies. On the other hand, it is unclear how this significant difference in abnormal knee kinematics of the pivot shift test affects the clinical outcome because our study showed no significant difference in clinical score between double-bundle and single-bundle ACL reconstruction.
There are some limitations in the data analysis in this study. First, the follow-up period was only one year because accurate assessment with the patient under general anaesthesia was possible only when the post screw was removed one year after surgery. Second, the validity and accuracy of the measurement system have not been wholly confirmed. We are currently collecting data to clarify these issues, and our preliminary results show this measurement system provides comparable repeatability to those of other measurement systems such as the KT-1000 [25, 26]. Third, in the pivot-shift test we sometimes have to perform the manoeuvre more than once to elicit the shift phenomenon. Therefore, we performed the pivot shift test five times and used the highest values for the study; thus, a potential bias may exist. However, we also believe we have overcome these potential limitations somewhat by maximising the accuracy of the data by quantitative evaluation of rotatory instability under general anaesthesia in a randomised study. Fourth, the number of patients was small. We need a larger number of patients to research the clinical outcome and allow quantitative knee kinematics data.
In conclusion, this prospective randomised study showed clinical outcomes were equally good in both groups and the anatomically positioned femoral tunnel technique of single-bundle reconstruction restored the normal knee kinematics as confirmed by conventional evaluation. However, the electromagnetic measurement data showed that the anatomical double-bundle ACL reconstruction tended to be biomechanically superior to the single-bundle reconstruction. Despite this, there are disadvantages in double-bundle reconstruction, such as additional surgical time, cost, and increased technical complexity so it remains to be seen whether it is worthwhile performing double-bundle anatomical reconstruction in clinical practice. Additional refinement of the reconstructive method is required to obtain optimum clinical results.
References
Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL (2002) Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med 30:660–666
Tashman S, Collon D, Anderson K, Kolowich P, Anderst W (2004) Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. Am J Sports Med 32:975–983
Petersen W, Tretow H, Weimann A, Herbort M, Fu FH, Raschke M, Zantop T (2007) Biomechanical evaluation of two techniques for double-bundle anterior cruciate ligament reconstruction: one tibial tunnel versus two tibial tunnels. Am J Sports Med 35:228–234. doi:10.1177/0363546506294468
Morimoto Y, Ferretti M, Ekdahl M, Smolinski P, Fu FH (2009) Tibiofemoral joint contact area and pressure after single- and double-bundle anterior cruciate ligament reconstruction. Arthroscopy 25:62–69. doi:10.1016/j.arthro.2008.08.014
Yagi M, Kuroda R, Nagamune K, Yoshiya S, Kurosaka M (2007) Double-bundle ACL reconstruction can improve rotational stability. Clin Orthop Relat Res 454:100–107. doi:10.1097/BLO.0b013e31802ba45c
Yasuda K, Kondo E, Ichiyama H, Kitamura N, Tanabe Y, Tohyama H, Minami A (2004) Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy 20:1015–1025. doi:10.1016/j.arthro.2004.08.010
Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W (2007) The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med 35:223–227. doi:10.1177/0363546506294571
Woo SL, Kanamori A, Zeminski J, Yagi M, Papageorgiou C, Fu FH (2002) The effectiveness of reconstruction of the anterior cruciate ligament with hamstrings and patellar tendon. A cadaveric study comparing anterior tibial and rotational loads. J Bone Joint Surg Am 84-A:907–914
Georgoulis AD, Papadonikolakis A, Papageorgiou CD, Mitsou A, Stergiou N (2003) Three-dimensional tibiofemoral kinematics of the anterior cruciate ligament-deficient and reconstructed knee during walking. Am J Sports Med 31:75–79
Brandsson S, Karlsson J, Sward L, Kartus J, Eriksson BI, Karrholm J (2002) Kinematics and laxity of the knee joint after anterior cruciate ligament reconstruction: pre- and postoperative radiostereometric studies. Am J Sports Med 30:361–367
Bush-Joseph CA, Hurwitz DE, Patel RR, Bahrani Y, Garretson R, Bach BR Jr, Andriacchi TP (2001) Dynamic function after anterior cruciate ligament reconstruction with autologous patellar tendon. Am J Sports Med 29:36–41
Ristanis S, Giakas G, Papageorgiou CD, Moraiti T, Stergiou N, Georgoulis AD (2003) The effects of anterior cruciate ligament reconstruction on tibial rotation during pivoting after descending stairs. Knee Surg Sports Traumatol Arthrosc 11:360–365. doi:10.1007/s00167-003-0428-x
Loh JC, Fukuda Y, Tsuda E, Steadman RJ, Fu FH, Woo SL (2003) Knee stability and graft function following anterior cruciate ligament reconstruction: comparison between 11 o'clock and 10 o'clock femoral tunnel placement. 2002 Richard O'Connor Award paper. Arthroscopy 19:297–304. doi:10.1053/jars.2003.50084
Aglietti P, Giron F, Cuomo P, Losco M, Mondanelli N (2007) Single-and double-incision double-bundle ACL reconstruction. Clin Orthop Relat Res 454:108–113. doi:10.1097/BLO.0b013e31802baaf4
Jarvela T, Moisala AS, Sihvonen R, Jarvela S, Kannus P, Jarvinen M (2008) Double-bundle anterior cruciate ligament reconstruction using hamstring autografts and bioabsorbable interference screw fixation: prospective, randomized, clinical study with 2-year results. Am J Sports Med 36:290–297. doi:10.1177/0363546507308360
Muneta T, Koga H, Mochizuki T, Ju YJ, Hara K, Nimura A, Yagishita K, Sekiya I (2007) A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy 23:618–628. doi:10.1016/j.arthro.2007.04.010
Siebold R, Dehler C, Ellert T (2008) Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy 24:137–145. doi:10.1016/j.arthro.2007.11.013
Yasuda K, Kondo E, Ichiyama H, Tanabe Y, Tohyama H (2006) Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among 3 different procedures. Arthroscopy 22:240–251. doi:10.1016/j.arthro.2005.12.017
Meredick RB, Vance KJ, Appleby D, Lubowitz JH (2008) Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med 36:1414–1421. doi:10.1177/0363546508317964
Fu FH (2008) The clock-face reference: simple but nonanatomic. Arthroscopy 24:1433, author reply 1434. doi:10.1016/j.arthro.2008.09.003
Shen W, Forsythe B, Ingham SM, Honkamp NJ, Fu FH (2008) Application of the anatomic double-bundle reconstruction concept to revision and augmentation anterior cruciate ligament surgeries. J Bone Joint Surg Am 90(Suppl 4):20–34. doi:10.2106/JBJS.H.00919
Schlegel TF, Boublik M, Hawkins RJ, Steadman JR (2002) Reliability of heel-height measurement for documenting knee extension deficits. Am J Sports Med 30:479–482
Daniel DM, Malcom LL, Losse G, Stone ML, Sachs R, Burks R (1985) Instrumented measurement of anterior laxity of the knee. J Bone Joint Surg Am 67:720–726
Daniel DM, Stone ML, Sachs R, Malcom L (1985) Instrumented measurement of anterior knee laxity in patients with acute anterior cruciate ligament disruption. Am J Sports Med 13:401–407
Hoshino Y, Kuroda R, Nagamune K, Yagi M, Mizuno K, Yamaguchi M, Muratsu H, Yoshiya S, Kurosaka M (2007) In vivo measurement of the pivot-shift test in the anterior cruciate ligament-deficient knee using an electromagnetic device. Am J Sports Med 35:1098–1104. doi:10.1177/0363546507299447
Araki D, Kuroda R, Murata H, Nagamune K, Nishimoto K, Hoshino Y, Kubo S, Kurosaka M (2008) Quantitative measurement of the Lachman test using an electromagnetic measurement system. In: Proceedings of the 54th annual meeting of the Orthopaedic Research Society, San Francisco
Kubo S, Muratsu H, Yoshiya S, Mizuno K, Kurosaka M (2007) Reliability and usefulness of a new in vivo measurement system of the pivot shift. Clin Orthop Relat Res 454:54–58. doi:10.1097/BLO.0b013e31802b4a38
Grood ES, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 105:136–144
Seon JK, Song EK, Bae BH, Park SJ, Yoon TR, Cho SG, Lee JJ, Kim MS (2007) Kinematic study following double-bundle, anterior cruciate ligament reconstruction. Int Orthop 31:623–628. doi:10.1007/s00264-006-0244-2
Seon JK, Park SJ, Lee KB, Yoon TR, Seo HY, Song EK (2009) Stability comparison of anterior cruciate ligament between double- and single-bundle reconstructions. Int Orthop 33:425–429. doi:10.1007/s00264-008-0530-2
Adachi N, Ochi M, Uchio Y, Iwasa J, Kuriwaka M, Ito Y (2004) Reconstruction of the anterior cruciate ligament. Single- versus double-bundle multistranded hamstring tendons. J Bone Joint Surg Br 86:515–520
Asagumo H, Kimura M, Kobayashi Y, Taki M, Takagishi K (2007) Anatomic reconstruction of the anterior cruciate ligament using double-bundle hamstring tendons: surgical techniques, clinical outcomes, and complications. Arthroscopy 23:602–609. doi:10.1016/j.arthro.2007.01.009
Streich NA, Friedrich K, Gotterbarm T, Schmitt H (2008) Reconstruction of the ACL with a semitendinosus tendon graft: a prospective randomized single blinded comparison of double-bundle versus single-bundle technique in male athletes. Knee Surg Sports Traumatol Arthrosc 16:232–238. doi:10.1007/s00167-007-0480-z
Kasovic M, Mejovsek M, Matkovic B, Jankovic S, Tudor A (2010) Electromyographic analysis of the knee using fixed-activation threshold after anterior cruciate ligament reconstruction. Int Orthop. doi:10.1007/s00264-010-1050-4
Acknowledgement
We would like to thank Ms. Janina Tubby for her excellent editing assistance in preparing this manuscript.
Conflict of interest
We did not receive any outside funding or grants in support of our research for or preparation of this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Araki, D., Kuroda, R., Kubo, S. et al. A prospective randomised study of anatomical single-bundle versus double-bundle anterior cruciate ligament reconstruction: quantitative evaluation using an electromagnetic measurement system. International Orthopaedics (SICOT) 35, 439–446 (2011). https://doi.org/10.1007/s00264-010-1110-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-010-1110-9