Abstract
Purpose
To compare the subjective clinical results as well as manual anterior and rotational stability in patients treated with either single- (SB) or double-bundle (DB) anterior cruciate ligament (ACL) reconstructions.
Methods
Sixty-four patients who had undergone SB or DB hamstring ACL reconstruction with hamstrings were included in a retrospective matched pair analysis. At follow-up IKDC subjective, CKS, KOOS, CKS and a visual analogue satisfaction scale was assessed. A blinded surgeon examined the joint laxity and completed the objective IKDC. The KT-1000 was used to bilaterally test anterior tibial translation. Patients with confounding variables, which statistically influenced the clinical outcome (passive flexion and extension deficits, persistent quadriceps deficit, tibiofemoral osteoarthritis and non-repairable medial meniscus injury), were identified and excluded from the statistical analysis (n = 10).
Results
For all subjective scores, DB patients reported increased scores compared with SB patients. While consistently higher scores were demonstrated, statistical significance was only achieved for the IKDC subjective (P = 0.04) and VAS satisfaction (P = 0.02). Graded stability results of the Lachman, anterior drawer and pivot-shift tests were significantly higher in the DB group and KT-1000 side-to-side difference was significantly better for DB (P = 0.01).
Conclusion
DB ACL reconstruction appeared to more consistently result in significantly higher subjective outcome scores and manual tests of joint stability than SB ACL reconstruction. Besides the surgical technique, normal extension and quadriceps strength after surgery were identified to be an essential component in order to provide the patient with a successful outcome.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Great interest has been directed to the separate reconstruction of the anteromedial (AM) and the posterolateral (PL) bundles of the anterior cruciate ligament (ACL) in order to recreate the natural anatomy [12, 14–17, 22, 23, 44, 53–56, 63, 68] and to restore their biomechanical functions [4, 6, 9–11, 19, 32, 35, 36, 39–42, 45, 48, 50, 51, 59, 65–67, 69, 71, 72]. A precise reconstruction of the anatomical double-bundle (DB) structure of the ACL with its AM and PL insertions might theoretically be of significant clinical benefit for the patient.
According to their distinct insertions sites, each bundle contributes individually to the overall biomechanical function of the ACL. Biomechanical in vitro and in vivo studies suggest that both bundles improve anterior stability of the knee, and that both bundles, and especially the PL bundle, contribute to rotational stability of the knee close to extension [4, 11, 19, 39–41, 48, 50, 61, 65, 72]. Biomechanical studies have also demonstrated that DB reconstruction significantly reduced internal rotation when compared with single-bundle (SB) ACL reconstruction [7, 25, 50]. Clinical studies have supported these concepts, reconfirming superior anterior and rotational stability with DB compared with SB ACL reconstruction. [2, 3, 5, 8, 13, 18, 25–27, 29–31, 37–39, 47, 52, 60, 61, 67, 68, 70, 72, 73] Furthermore, clinical studies have also reported that DB reconstruction resulted in significantly better IKDC [2, 25, 52, 64], subjective Lysholm Score [25], Tegner Score [72] and visual analogue scale (VAS) [2] than SB ACL reconstruction.
However, the subjective clinical benefit of DB ACL reconstruction is still controversial, and the majority of clinical trials [1, 18, 21, 26, 29, 31, 33, 37, 38, 43, 47, 49, 52, 60, 62, 64, 67] as well as a clinical meta-analysis from Meredick et al. [33] have not shown any significant subjective clinical difference between patients treated with either technique. Patient-reported function has been determined to be influenced not only by the type of ACL reconstruction but also by pain and/or function of the non-operative limb [34, 57]. Concomitant injury or factors associated with postoperative rehabilitation such as range of motion and quadriceps strength may influence subjective scores. While providing useful information about patient’s postoperative recovery, subjective scores may be too blunt of a tool to judge differences between two ACL reconstruction surgical techniques. Clinical studies including patients with either concomitant disease or insufficient rehabilitation may cloud the subjective comparison of SB to DB ACL reconstruction.
The purpose of this study was to evaluate the clinical outcomes, patient satisfaction and manual tests of knee stability of patients without concomitant disease or deficits in motion or strength treated with either DB or SB ACL reconstruction. It was hypothesized that when controlling for confounding variables, patients treated with a DB technique would demonstrate increased subjective outcome scores, patient satisfaction scores and manual stability testing.
Materials and methods
Patients
Sixty-eight patients following arthroscopic SB and DB hamstring ACL reconstruction were included in this retrospective matched pair analysis in order to compare the clinical outcomes, patient satisfaction, and knee stability of the two procedures. All patients were examined carefully during pre- and postoperative evaluation and during surgery. Pre- and postoperative evaluation included history, examination, standardized radiographs (anteroposterior and lateral view), and preoperative MRI. Patients were excluded from the study if they had any injury to the contralateral knee, or if they demonstrated a severe injury to involved knee, e.g. additional knee ligament injuries, previous knee ligament surgery, arthritic changes grade 3 or 4 according to Outerbridge, subtotal or total meniscectomy, malalignment or patellar pathology.
Patients were selected to participate in the current investigation from the patient populations of two participating surgeons, provided they met the inclusion criteria, matching was possible and they were willing to attend the clinical follow-up for testing. Prior to participation, patients provided informed consent for the IRB-approved protocol. At the time of testing, 3 patients were identified as having an injured opposite extremity and 1 patient did not attend the follow-up, leaving an active sample of 64 patients. The groups were well matched, as there were no differences in age, sex, height, weight or follow-up.
Surgical techniques and rehabilitation
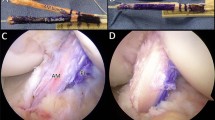
Skin incisions were identical for both groups. The semitendinosus and gracilis tendons were harvested through an anteromedial tibial incision at the pes anserine with a tendon stripper. For the four tunnel DB ACL reconstruction, the semitendinosus tendon (for the AM bundle) and the gracilis tendon (for the PL bundle) were looped over a 20 mm EndoButton CL (Smith and Nephew Endoscopy, Mansfield, Mass., USA). The SB ACL reconstruction utilized a double loop semitendinosus and gracilis graft; therefore, both tendons were looped over one 20 mm EndoButton CL. For both techniques, the distal free ends of the tendons were armed with two No. 2 vicryl sutures using a whip-stitch technique and the grafts were pretensioned on a suture board. The tibial and femoral ACL footprints and the intercondylar notch were cleaned from soft tissue as much as necessary to have an exact arthroscopic view of the insertion sites. No notchplasty was performed. All graft diameters were measured in 0.5 mm steps and the tibial and femoral bone tunnels were drilled accordingly in 0.5 mm steps with a conventional reamer on the tibia and with a headed reamer on the femur.
In SB ACL reconstruction, the tibial bone tunnel was drilled in a 50–55° angle to the tibial plateau. It was positioned in the centre of the native tibial ACL footprint. The femoral bone tunnel was drilled transtibially approximately 4–5 mm inferior to the “over the top position” at the 10:30 h for a right knee and at the 1:30 h position for a left knee at the femoral ACL footprint. The tibial bone tunnel was positioned according to Jackson et al. [28] and Goble et al. [20], and the femoral bone tunnel according to Bernard et al. [7]. A tight press-fit of the two grafts in the bone tunnels was aimed for in all patients. After positioning of the graft, the femoral EndoButton CL was flipped and a 30-mm tibial biodegradable interference screw (Smith and Nephew Endoscopy, Mansfield, Mass., USA) with the same diameter as the tibial bone tunnel or 1 mm larger was inserted.
In four tunnel DB ACL reconstruction, the tibial AM bone tunnel was drilled in a 55° angle and the PL bone tunnel in a 60° angle to the tibial plateau and approximately 1.5 cm (AM bundle) and 3.5 cm (PL bundle) medial to the tibial tuberosity in the coronal plane. Both tibial bone tunnels were positioned in the area intercondylaris anterior respecting the natural border of the tibial ACL footprint according to previous anatomical studies [54]. The femoral AM bone tunnel was drilled 4–5 mm inferior to the “over the top position” at the 10.30 h for a right knee and at the 1.30 h for left knee at the insertion site of the AM bundle [53]. The PL femoral tunnel was drilled at the insertion site of the PL bundle 5–7 mm deep in the notch measured from the shallow (anatomical: inferior) articular cartilage of the lateral femoral condyle. Both femoral bone tunnels were drilled through an accessorial anteromedial portal. We preserved a bone bridge of 1–2 mm between the AM and PL bone tunnels in all patients. After positioning of the two grafts, the two femoral EndoButton CL were flipped. Tibial AM bundle fixation was achieved by an 8 mm or 9 mm by 23 mm long biodegradable interference screw (Arthrex Inc, USA) having the same diameter as that of the AM bone tunnel and tibial PL bundle fixation was by means of a 7 × 23-mm biodegradable interference screw (Arthrex Inc., USA) for all patients. The screws were placed in the most distal part of the bone tunnel keeping a distal cortical contact. The AM bundle was fixed in 60° and the PL bundle in 10° of knee flexion. The postoperative rehabilitation was similar for both groups and was similar to a previous clinical study [52].
Clinical evaluation
At clinical follow-up, all patients were examined by a single experienced orthopaedic surgeon who was not a member of the hospital, nor the operative surgeon for any of the study patients and was blinded to both surgical techniques. The patients themselves were not blinded to the type of procedure.
Bilateral knee extension and flexion ranges of knee motion were measured using standard goniometry, and graded manual muscle tests were performed to assess quadriceps strength by the blinded orthopaedic surgeon. Side-to-side deficits in knee extension, knee flexion, and quadriceps strength were then calculated and used for all analyses. Bilateral knee stability was assessed manually using the Lachman, anterior drawer, and pivot-shift tests. Instrumented side-to-side anterior knee laxity was assessed using the KT-1000, with an anteriorly directed force of 134 N. The objective IKDC was completed by this blinded orthopaedic surgeon. Seated separately, all patients completed the questionnaires necessary to calculate the Cincinnati Knee Score (CKS), Knee Injury and Osteoarthritis Outcome Score (KOOS), International Knee Documentation Committee (IKDC) Subjective Score, and Visual Analogue Scale (VAS) for patient satisfaction.
Statistical analyses
Pearson’s product moment correlation coefficients (r) were calculated to evaluate the relationships between subjective outcome scores and the presence of confounding variables (side-to-side deficits in quadriceps strength, passive knee flexion, passive knee extension, tibiofemoral osteoarthritis, patellofemoral osteoarthritis, unrepairable medial or lateral meniscus injury and concomitant medial collateral ligament injury). Once it was determined which confounding factors significantly influenced outcome scores, patients exhibiting these factors were excluded from the comparison of subjective outcome scores in an attempt to make a more clear comparison of the two reconstruction techniques. After applying the additional exclusion criteria, two-tailed, independent t-tests were used to compare side-to-side passive knee flexion and extension deficits between groups. Mann–Whitney U-tests were used to compare subjective IKDC scores, CKS, KOOS, VAS satisfaction scores. Subjective laxity testing (Lachman, anterior drawer, and pivot-shift tests) and objective IKDC scores were compared between groups using Chi2 tests. All analyses were performed using Statistical Package for the Social Sciences v 17.0 (SPSS Inc., Chicago, IL), and an α-level of P ≤ 0.05 was considered significant.
Results
The five factors that significantly correlated with subjective outcome scores were side-to-side passive knee flexion and extension deficits, persistent quadriceps deficit, tibiofemoral osteoarthritis, and non-repairable medial meniscus injury (Table 1). All patients with persistent quadriceps deficits greater than grade 2, side-to-side extension deficits of ≥5°, side-to-side flexion deficits of ≥15°, tibiofemoral arthritis, or non-repairable medial meniscus injury were then excluded. The remaining 54 patients (28 SB, 26 DB) were then used to compare the two surgical techniques (Table 2).
For all subjective scores, the DB patients reported increased scores compared to the SB patients (Table 3). While consistently higher scores were reported, statistical significance was only achieved for the IKDC subjective score (P = 0.04) and VAS satisfaction (P = 0.02). The mean arc of motion did not differ between the SB group (−1.3–131.4°) and the DB group (−2.1–129.1°), nor did side-to-side knee flexion or extension deficits.
Graded laxity results from the Lachman, anterior drawer, and pivots-shift tests were significantly lower for DB than for SB (Fig. 1) as were the side-to-side differences of anterior translation measured with the KT-1000 (DB group = 1.1 ± 1.0 mm and SB group = 2.2 ± 1.4 mm, P = 0.01) The objective IKDC was normal or nearly normal in 92.0% patients in group SB and 96.2% in group DB (Table 3).
Discussion
The most important finding of the present study was that patients following DB ACL reconstruction demonstrated significantly reduced anterior and rotational laxity with significantly improved subjective IKDC and patient VAS satisfaction scores. The other scoring systems assessed in this study did not demonstrate differences between the two surgical techniques.
A second part of our clinical study was to compare rotational laxity with these same groups of patients using a robotic testing system [7]. When comparing the reconstructed knee to the intact contralateral knee, Branch et al. [7] found that side-to-side differences in internal rotation difference were significantly lower with DB (2°) compared to SB reconstruction (5°). A significantly greater percentage of DB patients (81%) also had both anterior tibial translation and internal rotation similar to the normal contralateral knee, compared to 34% of the SB patients [7]. We concluded that the DB technique more consistently reproduced the biomechanical profile of the uninjured limb.
In recent years, several clinical trials demonstrated improved knee stability with DB ACL reconstruction compared to SB [2, 3, 5, 8, 13, 18, 25–27, 29–31, 37–39, 47, 52, 60, 61, 67, 68, 70, 72, 73]. Aglietti et al. [2] performed a randomized, controlled clinical trial including 70 patients with a minimum follow-up of 2 years and found significantly improved VAS, significantly greater number of “normal knees” according to the objective IKDC final scores, and significantly improved KT-1000 and pivot shift test results with DB compared to SB reconstruction. Significantly improved anterior and rotational stability were also described by Kondo et al. [31], including 328 patients with a minimum follow-up of 2 years and by Yasuda et al. [67] in a comparison of “anatomic” DB reconstruction to “non-anatomic” SB reconstruction including 72 patients with hamstring tendon graft. These findings were reconfirmed by Muneta et al. [37] in a randomized clinical trial including 68 patients. In that report, DB ACL reconstruction using a 4-strand semitendinosus graft demonstrated superior anterior and rotational stability, but no subjective differences were noted between the two techniques.
Significantly better objective IKDC results were observed by Siebold et al. [52] in a randomized clinical trial of SB versus DB ACL reconstruction in 2008 including 70 patients. In addition, anterior and rotational stability were superior with DB compared to SB. Hofbauer et al. [25] reconfirmed these findings and demonstrated significantly higher IKDC and Lysholm scores and a significant greater reduction in internal rotation in the DB patients (16°) compared to SB patients (7°). Similar results were reported by Volpi et al. [64] comparing transtibial SB bone-patellar tendon-bone reconstruction (BPTB) to transtibial DB semitendinosus/gracilis (ST/G) reconstruction in sportive patients. IKDC scores were significantly higher with the DB technique, and only DB patients were able to return to sports at a pre-injury level. A significantly higher Tegner activity level, higher passive range of motion recovery, faster sport resumption and lower pivot-shift was seen by Zaffagnini et al. [72] in a long-term study comparing SB BPTB to non-anatomical DB ST/G ACL reconstruction. They also assessed a lower reintervention rate for DB, similar to the findings of Järvelä et al. [29] in their cohort.
However, a recent meta-analysis comparing the overall outcomes of SB to DB ACL reconstruction performed by Meredick et al. [33] did not find any significant difference between SB and DB techniques. They included four randomized controlled trials. KT-1000 arthrometer side-to-side difference was 0.52 mm closer to normal in patients with DB, but the difference was not significant. In addition, there was no difference in rotational stability evaluated with the pivot-shift test. Similar results between SB and DB ACL reconstruction were also reported by several other authors [1, 21, 24, 29, 43, 49, 58, 62].
On the contrary, when controlling for concomitant disease and factors related to postoperative rehabilitation, our current results demonstrate a difference in the subjective scores between the two ACL reconstruction techniques. Despite only the subjective IKDC and VAS satisfaction scores being statistically significant between the groups, all other subjective scores (KOOS, CKS) were consistently higher in the DB group. In addition to consistent patient-reported subjective results, the three manual tests of anterior and rotational knee stability as well as the KT 1000 demonstrated significantly increased stability with the DB reconstruction.
However, the statistical analyses show that attaining proper motion and strength after surgery is very important in order to provide the patient with a successful outcome. Of the potential confounding variables that were evaluated in the present study, loss of extension significantly correlated with all subjective scores. An inability to full extend the knee may result in quadriceps weakness, fatigue, and patellofemoral pain [46]. This is further supported by the significant correlations between postoperative quadriceps deficit and the CKS, IKDC subjective score, and four of the five subcomponents of the KOOS.
This study is not without limitations. While we attempted to control for confounding variables that may influence subjective scores by applying secondary exclusion criteria, our sample size was reduced. It is unclear if a larger sample size would have resulted in statistical differences for a greater proportion of the subjective scoring systems. Also, this study utilized manual tests and the KT1000 for assessing joint stability, which may also limit our ability to truly gauge potential differences between ACL reconstruction techniques. Furthermore, transtibial drilling was used in the SB group compared to an anteromedial portal approach in DB, which might have influenced femoral bone tunnel positioning.
Conclusion
DB ACL reconstruction resulted in significantly higher subjective outcome scores and manual tests of joint stability than SB ACL reconstruction. Normal extension and quadriceps strength after surgery were identified to be essential components in order to provide the patient with a successful outcome. Therefore, it is clinically relevant to not only to focus on the type of ACL reconstruction (SB/DB) but also on regaining a full range of motion and quadriceps strength.
References
Adachi N, Ochi M, Uchio Y, Iwasa J, Kuriwaka M, Ito Y (2004) Reconstruction of the anterior cruciate ligament. Single-versus double-bundle multistranded hamstring tendons. J Bone Joint Surg Br 86:515–520
Aglietti P, Giron F, Losco M, Cuomo P, Ciardullo A, Mondanelli N (2010) Comparison between single-and double-bundle anterior cruciate ligament reconstruction: a prospective, randomized, single-blinded clinical trial. Am J Sports Med 38:25–34
Ahn JH, Lee SH (2007) Anterior cruciate ligament double-bundle reconstruction with hamstring tendon autografts. Arthroscopy 23:109.e1–4
Amis AA, Zavras TD (1995) Isometricity and graft placement during anterior cruciate ligament reconstruction. Knee 2:5–17
Araki D, Kuroda R, Kubo S, Fujita N, Tei K, Nishimoto K, Hoshino Y, Matsushita T, Matsumoto T, Nagamune K, Kurosaka M (2011) A prospective randomised study of anatomical single-bundle versus double-bundle anterior cruciate ligament reconstruction: quantitative evaluation using an electromagnetic measurement system. Int Orthop 35:439–446
Bellier G, Christel P, Colombet P, Djian P, Franceschi JP, Sbihi A (2004) Double-stranded hamstring graft for anterior cruciate ligament reconstruction. Arthroscopy 20:890–894
Bernard M, Hertel P, Hornung H, Cierpinski T (1997) Femoral insertion of the ACL. Radiographic quadrant method. Am J Knee Surg 10:14–21
Branch TP, Siebold R, Freedberg HI, Jacobs CA (2011) Double-bundle ACL reconstruction demonstrated superior clinical stability to single-bundle ACL reconstruction: a matched-pairs analysis of instrumented tests of tibial anterior translation and internal rotation laxity. Knee Surg Sports Traumatol Arthrosc 19:432–440
Buoncristiani AM, Tjoumakaris FP, Starman JS, Ferretti M, Fu FH (2006) Anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy 22:1000–1006
Cha PS, Brucker PU, West RV, Zelle BA, Yagi M, Kurosaka M, Fu FH (2005) Arthroscopic double bundle anterior cruciate ligament reconstruction: an anatomic approach. Arthroscopy 21:1275–1277
Colombet P, Menetrey J, Panisset JC, Société française d’arthroscopie (2008) The effect of the posterolateral bundle in the anterior cruciate ligament reconstruction. Rev Chir Orthop Reparatrice Appar Mot 94:369–371
Colombet P, Robinson J, Christel P, Franceschi JP, Djian P, Bellier G, Sbihi A (2006) Morphology of anterior cruciate ligament attachment for anatomic reconstruction: a cadaveric dissection and radiographic study. Arthroscopy 22:984–992
Colombet P, Robinson J, Jambou S, Allard M, Bousquet V, de Lavigne C (2006) Two-bundle, four-tunnel anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 14:629–636
Duthon VB, Barea C, Abrassart S, Fasel JH, Fritschy D, Ménétrey J (2006) Anatomy of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 14:204–213
Edwards A, Bull AM, Amis AA (2007) The attachments of the anteromedial and posterolateral fibre bundles of the anterior cruciate ligament: part1: tibial attachment. Knee Surg Sports Traumatol Arthrosc 15:1414–1421
Edwards A, Bull AM, Amis AA (2008) The attachments of the anteromedial and posterolateral fibre bundles of the anterior cruciate ligament. Part 2: femoral attachment. Knee Surg Sports Traumatol Arthrosc 16:29–36
Ferretti M, Levicoff EA, Macpherson TA, Moreland MS, Cohen M, Fu FH (2007) The fetal anterior cruciate ligament: an anatomic and histologic study. Arthroscopy 23:278–282
Fu Fh, Shen W, Starman JS, Okeke N, Irrgang JJ (2008) Primary anatomic double-bundle anterior cruciate ligament reconstruction: a preliminary 2-year prospective study. Am J Sports Med 36:1263–1274
Gabriel MT, Wong EK, Woo SL, Yagi M, Debski RE (2004) Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res 22:85–89
Goble EM, Downey DJ, Wilcox TR (1995) Positioning of the tibial tunnel for anterior cruciate ligament reconstruction. Arthroscopy 11:688–695
Hamada M, Shino K, Horibe S, Mitsuoka T, Miyama T, Shiozaki Y, Mae T (2001) Single-versus bi-socket anterior cruciate ligament reconstruction using autogenous multiple-stranded hamstring tendons with EndoButton femoral fixation: a prospective study. Arthroscopy 17:801–807
Hara K, Mochizuki T, Sekiya I, Yamaguchi K, Akita K, Muneta T (2009) Anatomy of normal human anterior cruciate ligament attachments evaluated by divided small bundles. Am J Sports Med 37:2386–2391
Harner CD, Baek GH, Vogrin TM, Carlin GJ, Kashiwaguchi S, Woo SL (1999) Quantitative analysis of human cruciate ligament insertions. Arthroscopy 15:741–749
Ho JY, Gardiner A, Shah V, Steiner ME (2009) Equal kinematics between central anatomic single-bundle and double-bundle anterior cruciate ligament reconstructions. Arthroscopy 25:464–472
Hofbauer M, Valentin P, Kdolsky R, Ostermann RC, Graf A, Figl M, Aldrian S (2010) Rotational and translational laxity after computer-navigated single- and double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 18:1201–1207
Ibrahim SA, Hamido F, Al Misfer AK, Mahgoob A, Ghafar SA, Alhran H (2009) Anterior cruciate ligament reconstruction using autologous hamstring double bundle graft compared with single bundle procedures. J Bone Joint Surg Br 91:1310–1315
Ishibashi Y, Tsuda E, Fukuda A, Tsukada H, Toh S (2008) Stability evaluation of single-bundle and double-bundle reconstruction during navigated ACL reconstruction. Sports Med Arthrosc 16:77–83
Jackson DW, Gasser SI (1994) Tibial tunnel placement in ACL reconstruction. Arthroscopy 10:124–131
Järvelä T, Moisala AS, Sihvonen R, Järvelä S, Kannus P, Järvinen M (2008) Double-bundle anterior cruciate ligament reconstruction using hamstring autografts and bioabsorbable interference screw fixation: prospective, randomized, clinical study with 2-year results. Am J Sports Med 36:290–297
Kim SJ, Jo SB, Kumar P, Ks Oh (2009) Comparison of single- and double-bundle anterior cruciate ligament reconstruction using quadriceps tendon-bone autografts. Arthroscopy 25:70–77
Kondo E, Yasuda K, Azuma H, Tanabe Y, Yagi T (2008) Prospective clinical comparisons of anatomic double-bundle versus single-bundle anterior cruciate ligament reconstruction procedures in 328 consecutive patients. Am J Sports Med 36:1675–1687
Marcacci M, Molgora AP, Zaffagnini S, Vascellari A, Iacono F, Presti ML (2003) Anatomic double-bundle anterior cruciate ligament reconstruction with hamstrings. Arthroscopy 19:540–546
Meredick RB, Vance KJ, Appleby D, Lubowitz JH (2008) Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med 36:1414–1421
Mizner R, Snyder-Mackler L (2005) Altered loading during walking and sit-to-stand is affected by quadriceps weakness after total knee arthroplasty. J Orthop Res 23:1083–1090
Monaco E, Labianca L, Conteduca F, De Carli A, Ferretti A (2007) Double bundle or single bundle plus extraarticular tenodesis in ACL reconstruction? A CAOS study. Knee Surg Sports Traumatol Arthrosc 15:1168–1174
Morimoto Y, Ferretti M, Ekdahl M, Smolinski P, Fu FH (2009) Tibiofemoral joint contact area and pressure after single-bundle and double-bundle anterior cruciate ligament reconstruction. Arthroscopy 25:62–69
Muneta T, Koga H, Mochizuki T, Ju YJ, Hara K, Nimura A, Yagishita K, Sekiya I (2007) A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy 23:618–628
Muneta T, Koga H, Morito T, Yagishita K, Sekiya I (2006) A retrospective study of the midterm outcome of two-bundle anterior cruciate ligament reconstruction using quadrupled semitendinosus tendon in comparison with one-bundle reconstruction. Arthroscopy 22:252–258
Muneta T, Sekiya I, Yagishita K, Ogiuchi T, Yamamoto H, Shinomiya K (1999) Two-bundle reconstruction of the anterior cruciate ligament using semitendinosus tendon with endobuttons: operative technique and preliminary results. Arthroscopy 15:618–624
Musahl V, Voos JE, O’Loughlin PF, Choi D, Stueber V, Kendoff D, Pearle AD (2010) Comparing stability of different single- and double-bundle anterior cruciate ligament reconstruction techniques: a cadaveric study using navigation. Arthroscopy 26:S41–S48
Musahl V, Bedi A, Citak M, O’Loughlin P, Choi D, Pearle AD (2011) Effect of single-bundle and double-bundle anterior cruciate ligament reconstructions on pivot-shift kinematics in anterior cruciate ligament- and meniscus-deficient knees. Am J Sports Med 39:289–295
Otsubo H, Shino K, Nakamura N, Nakata K, Nakagawa S, Koyanagi M (2007) Arthroscopic evaluation of ACL grafts reconstructed with the anatomical two-bundle technique using hamstring tendon autograft. Knee Surg Sports Traumatol Arthrosc 15:720–728
Park S, Jung YB, Jung HJ, Jung HJ, Shin HK, Kim E, Song KS, Kim GS, Cheon HY, Kim S (2010) Outcome of arthroscopic single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a preliminary 2-year prospective study. Arthroscopy 26:630–636
Petersen W, Zantop T (2007) Anatomy of the anterior cruciate ligament with regard to its two bundles. Clin Orthop Relat Res 454:35–47
Pombo MW, Shen W, Fu FH (2008) Anatomic double-bundle anterior cruciate ligament reconstruction: where are we today? Arthroscopy 24:1168–1177
Sachs RA, Daniel DM, Stone ML, Garfein RF (1989) Patellofemoral problems after anterior cruciate ligament reconstruction. Am J Sports Med 17:760–765
Sadoghi P, Müller PE, Jansson V, van Griensven M, Kröpfl A, Fischmeister MF (2011) Reconstruction of the anterior cruciate ligament: a clinical comparison of bone-patellar tendon-bone single bundle versus semitendinosus and gracilis double bundle technique. Int Orthop 35:127–133
Sakana M, Fox RJ, Woo SL, Livesay GA, Li G, Fu FH (1997) In situ forces in the anterior cruciate ligament and its bundles in response to anterior tibial loads. J Orthop Res 15:285–293
Sastre S, Popescu D, Núñez M, Pomes J, Tomas X, Peidro L (2010) Double-bundle versus single-bundle ACL reconstruction using the horizontal femoral position: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 18:32–36
Seon JK, Gadikota HR, Wu JL, Sutton K, Gill TJ, Li G (2010) Comparison of single- and double-bundle anterior cruciate ligament reconstructions in restoration of knee kinematics and anterior cruciate ligament forces. Am J Sports Med 38:1359–1367
Shino K, Nakata K, Nakamura N, Toritsuka Y, Horibe S, Nakagawa S, Suzuki T (2008) Rectangular tunnel double-bundle anterior cruciate ligament reconstruction with bone-patellar tendon-bone graft to mimic natural fiber arrangement. Arthroscopy 24:1178–1183
Siebold R, Dehler C, Ellert T (2008) Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy 24:137–145
Siebold R, Ellert T, Metz S, Metz J (2008) Femoral insertions of the anteromedial and posterolateral bundles of the anterior cruciate ligament: morphometry and arthroscopic orientation models for double-bundle bone tunnel placement–a cadaver study. Arthroscopy 24:585–592
Siebold R, Ellert T, Metz S, Metz J (2008) Tibial insertions of the anteromedial and posterolateral bundles of the anterior cruciate ligament: morphometry, arthroscopic landmarks, and orientation model for bone tunnel placement. Arthroscopy 24:154–161
Siebold R, Zantop T (2009) Anatomic double-bundle ACL reconstruction: a call for indications. Knee Surg Sports Traumatol Arthrosc 17:211–212
Song EK, Oh LS, Gill TJ, Li G, Gadikota HR, Seon JK (2009) Prospective comparative study of anterior cruciate ligament reconstruction using the double-bundle and single-bundle techniques. Am J Sports Med 37:1705–1711
Stratford P, Kennedy D (2006) Performance measures were necessary to obtain a complete picture of osteoarthritic patients. J Clin Epidemiol 59:160–167
Streich NA, Friedrich K, Gotterbarm T, Schmitt H (2008) Reconstruction of the ACL with a semitendinosus tendon graft: a prospective randomized single blinded comparison of double-bundle versus single-bundle technique in male athletes. Knee Surg Sports Traumatol Arthrosc 16:232–238
Tashman S, Kopf S, Fu FH (2008) The kinematic basis of ACL reconstruction. Oper Tech Sports Med 16:116–118
Toritsuka Y, Amano H, Kuwano M, Iwai T, Mae T, Ohzono K, Shino K (2009) Outcome of double-bundle ACL reconstruction using hamstring tendons. Knee Surg Sports Traumatol Arthrosc 17:456–463
Tsai AG, Wijdicks CA, Walsh MP, Laprade RF (2010) Comparative kinematic evaluation of all-inside single-bundle and double-bundle anterior cruciate ligament reconstruction: a biomechanical study. Am J Sports Med 38:263–272
Tsuda E, Ishibashi Y, Fukuda A, Tsukada H, Toh S (2009) Comparable results between lateralized single- and double-bundle ACL reconstructions. Clin Orthop Relat Res 467:1042–1055
van Eck CF, Lesniak BP, Schreiber VM, Fu FH (2010) Anatomic single- and double-bundle anterior cruciate ligament reconstruction flowchart. Arthroscopy 26:258–268
Volpi P, Cervellin M, Denti M, Bait C, Melegati G, Quaglia A, de Girolamo L (2010) ACL reconstruction in sports active people: transtibial DB technique with ST/G vs. transtibial SB technique with BPTB: preliminary results. Injury 41:1168–1171
Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL (2002) Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med 30:660–666
Yasuda K, Kondo E, Ichiyama H, Kitamura N, Tanabe Y, Tohyama H, Minami A (2004) Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy 20:1015–1025
Yasuda K, Kondo E, Ichiyama H, Tanabe Y, Tohyama H (2006) Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among 3 different procedures. Arthroscopy 22:240–251
Yasuda K, Tanabe Y, Kondo E, Kitamura N, Tohyama H (2010) Anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy 26:S21–S34
Zaffagnini S, Bruni D, Russo A, Takazawa Y, Lo Presti M, Giordano G, Marcacci M (2008) ST/G ACL reconstruction: double strand plus extra-articular sling vs double bundle, randomized study at 3-year follow-up. Scand J Med Sci Sports 18:573–581
Zaffagnini S, Bruni D, Marcheggiani Muccioli GM, Bonanzinga T, Lopomo N, Bignozzi S, Marcacci M (2011) Single-bundle patellar tendon versus non-anatomical double-bundle hamstrings ACL reconstruction: a prospective randomized study at 8-year minimum follow-up. Knee Surg Sports Traumatol Arthrosc 19:390–397
Zantop T, Diermann N, Schumacher T, Schanz S, Fu FH, Petersen W (2008) Anatomical and non-anatomical double-bundle anterior cruciate ligament reconstruction: importance of femoral tunnel location on knee kinematics. Am J Sports Med 36:678–685
Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W (2007) The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med 35:223–227
Zhao J, Peng X, He Y, Wang J (2006) Two-bundle anterior cruciate ligament reconstruction with eight-stranded hamstring tendons: Four-tunnel technique. Knee 13:36–41
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Siebold, R., Branch, T.P., Freedberg, H.I. et al. A matched pairs comparison of single- versus double-bundle anterior cruciate ligament reconstructions, clinical results and manual laxity testing. Knee Surg Sports Traumatol Arthrosc 19 (Suppl 1), 4–11 (2011). https://doi.org/10.1007/s00167-011-1475-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1475-3