Abstract
The purposes of this study were to establish the technique to arthroscopically identify the resident’s ridge without bony notchplasty even in patients with chronic ACL insufficiency and to elucidate if the ridge could be used as a landmark for anatomical femoral tunnel for ACL graft. There were 50 consecutive patients undergoing arthroscopic ACL reconstruction. With the thigh kept horizontal using a leg holder, a meticulous effort was made to find out a linear ridge running proximo-distal in a posterior one-third of the lateral notch wall, after removal of superficial soft tissue with radiofrequency energy. If the ridge was found, a socket with a rectangular aperture of 5 × 10 mm was created just behind the ridge. At 3–4-weeks post surgery, three-dimensional computed tomography (3-D CT) was performed to geographically identify the location of the ridge using the socket as a reference. Arthroscopically, a linear ridge running from superior-anterior to inferior-posterior on the lateral notch wall was consistently observed 7–10 mm anterior to the posterior articular cartilage margin of the lateral femoral condyle in all of the patients. The 3-D CT pictures proved the arthroscopically identified ridge to be the resident’s ridge. The resident’s ridge is arthroscopically identifiable after non-mechanical removal of the soft tissues without bony notchplasty. The ridge is a useful landmark for anatomical femoral tunnel drilling in arthroscopic ACL reconstruction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The anterior cruciate ligament (ACL) attaches to the posterior-superior border of the lateral wall of the intercondylar notch of the femur, forming a crescent shape area adjacent to the posterior cartilage margin of the lateral femoral condyle [1–3, 6]. Mae et al. [9] described that the center of the posterolateral bundle footprint was located 5 mm anterior to the posterior margin at 9 or 3 o’clock of the notch and that of the anteromedial bundle footprint was situated 5 mm anterior to the posterior margin at 10 or 2 o’clock. A more recent cadaveric study by Siebold et al. [15] reported the center of the anteromedial bundle of ACL was located 3–4 mm “lower” to the over-the-top position or at 1-o’clock position in their clock expression. Steckel et al. [16] radiographically demonstrated the exact location of the femoral insertions of the anteromedial and posterolateral bundles of ACL in their cadaveric study. Thus, the technique to arthroscopically delineate the ACL femoral attachment area or identify the anterior border of ACL femoral attachment area in patients with chronic ACL-deficiency has not been established. Therefore, it has generally been advocated to place the femoral tunnel as deeply as possible after reducing the lateral wall of the notch with a burr to confirm the true over-the-top position [8]. Although such notchplasty has frequently been combined with arthroscopic ACL reconstruction, its adverse biomechanical effects on ACL grafts have been reported [7, 10].
The resident’s ridge is a nearly longitudinal ridge, three quarters of the way back on the roof to lateral border of the notch. The idea to use this ridge as a landmark for femoral bone tunnel placement is not a new idea but was already described by Clancy and coworkers some years ago. Hutchinson and Ash [8] reported that the ridge was present in 90% of the cadaveric knees they dissected, that it was located just anterior to the ACL attachment, and that the cortical bone of the attachment area behind the ridge was thicker. Ferretti et al. [5] found this ridge not only in adults but in fetuses, and renamed it the lateral intercondylar ridge. Shino et al. [14] suggested that the ridge could be estimated on three-dimensional computed tomography (3-D CT) images. A more recent study using high-resolution volume-rendering computed tomography by Purnell et al. [11] demonstrated that the anterior fibers of the ACL inserted immediately posterior to the most prominent edge of this ridge. Thus, the resident’s ridge could be a potential landmark as the anterior border of the ACL femoral attachment to delineate the attachment area behind it.
It would be beneficial if the anatomical femoral tunnel could be created inside the attachment area upon the base of thicker cortical bone without notchplasty at the time of arthroscopic ACL reconstruction. Our hypotheses were that the resident’s ridge could be visualized without notchplasty and that the ridge was a useful reference landmark for anatomical femoral tunnel in patients with chronic ACL insufficiency as well as those with acute ACL tears. The purposes of this study were, therefore, to establish the technique to arthroscopically identify the resident’s ridge without bony notchplasty and to elucidate if the ridge could be used as a landmark for anatomical femoral tunnel drilling in ACL reconstruction.
Materials and methods
Fifty consecutive patients undergoing primary ACL reconstruction with the autogenous bone–patellar tendon–bone graft of 10 mm in width because of chronic instability or acute/subacute ACL tear were involved. They consisted of 46 males and 4 females with a mean age of 21 years ranging from 14 to 32 years. All of them consented to prospectively undergo CT evaluation to critically evaluate the bone plug-socket integration at 3–4 weeks postoperatively. The average time interval between the injury and the surgery was 117 days with a range from 7 to 620 days. The senior author (K.S.) performed all the surgeries. Those who had undergone a previous surgery to the index knee, those who showed radiographically moderate to severe osteoarthritic changes, or those who combined injury to the posterior cruciate ligament were excluded.
At the time of arthroscopic ACL reconstruction, it was our routine to put the thigh into horizontal position with a leg holder to obtain a consistent view of the intercondylar notch including the ACL femoral attachment area, regardless of knee flexion angle. The following three portals were utilized: the anterolateral portal, the anteromedial portal, and the far anteromedial portal: an accessory portal 2–2.5 cm posterior to the anteromedial portal [12]. The former two portals were mainly for viewing, and the last one is for instruments to get more perpendicular access to the lateral notch wall. First, soft tissues in the notch were roughly excised with mechanical instruments including a powered shaver. Then, the remaining fibrous tissues on posterior-superior half of the lateral notch wall were delicately removed using a radiofrequency device (Bevel 30 A2630-01, ArthroCare Co., Sunnyvale, CA, USA) through the far anteromedial portal with the controller set at 6, while viewing via the anteromedial portal through a 45° oblique 4-mm arthroscope. Care was taken to adjust the obliquity of the scope along the axis of the ACL femoral attachment and to completely preserve undulation of the bony surface around the attachment area. Clearage was finalized with gentle use of a small curette, if required. Thus, the anterior half of the notch was always left intact (Figs. 1a, b, 2a, b). After this maneuver, a meticulous effort was made to find out a linear ridge in a posterior one-third of the lateral notch wall. If the ridge was found, then a socket with a rectangular aperture of 5 × 10 mm was created just behind it in inside-out fashion through the far anteromedial portal with the knee flexed beyond 135°. Attention was paid to make the long axis of the aperture parallel to the ridge (Figs. 1c, 2c).
a Arthroscopic view around the ACL femoral attachment area in the left knee of a 22-year-old male patient who sustained the injury 91 days previously through the anteromedial portal. b The same view after clearage. Black arrows show the nearly longitudinal resident’s ridge 8 mm anterior to the posterior articular cartilage margin of the lateral femoral condyle. c Arthroscopic view of the rectangular aperture of the femoral socket shown by a white arrow behind the ridge (black arrows). d 3-D CT picture showing the socket (white arrow) behind the ridge (black arrows)
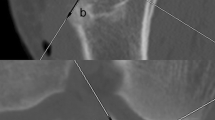
a Arthroscopic view of the ACL femoral stump in the left knee of an 18-year-old male patient who sustained the injury 16 days previously through the anteromedial portal. b The same view after clearage. Black arrows show the resident’s ridge 9 mm anterior to the posterior articular cartilage margin of the lateral femoral condyle. c Arthroscopic view of the rectangular aperture of the femoral socket shown by a white arrow behind the ridge (black arrows). d 3-D CT picture showing the socket (white arrow) behind the ridge (black arrows)
At 3–4 weeks postoperatively, two-dimensional (2-D) CT was obtained using the Asteion 4 Multislice CT System (Toshiba Medical Systems, Tochigi, Japan) under 120 kVp and 150 mA. Scan parameters were as follows: matrices of 512 × 512, gantry tilt of 0-degree, slice thickness of 1.00-mm, and beam pitch of 0.75-s gantry rotation. Then, the 2-D images were reconstructed for a 160-mm field of view with 1.00-mm retrospective slice thickness to obtain 90–120 slices. The three-dimensional (3-D) shaded volume-rendering (SVR) images were reconstituted using Alatoview workstation (Toshiba Corporation, Tokyo, Japan) in which the program stated an accuracy of ±0.1 mm or ±0.1 degree. Using an image processing software, the distal femur was longitudinally cut to remove the medial condyle, and the lateral aspect of the intercondylar notch wall was observed.
Results
Arthroscopically, a ridge running in line from superior-anterior to inferior-posterior on the lateral notch wall was consistently identified at 7–10 mm anterior to the posterior articular cartilage margin of the lateral femoral condyle in all of the 38 patients with chronic ACL insufficiency (Fig. 1b). In the remaining 12 patients with ACL acute/subacute tears, the similar ridge was found in the same position as the anterior border of the residual femoral stump (Fig. 2b). The ridge was more prominent in its superior portion. Its midpoint was located 7–10 mm anterior to the posterior articular cartilage margin of the lateral femoral condyle.
On the 3-D CT images, a nearly longitudinal linear ridge just anterior-inferior to the rectangular aperture of the socket was consistently observed in all of the 50 patients. The aperture of the socket was located between the ridge and the posterior articular cartilage margin of the lateral femoral condyle, and its long axis was parallel to the ridge (Figs. 1d, 2d). The mean distance from the peak of the ridge to the anterior-inferior borders of the sockets was 1.9 ± 0.7 mm with a range from 0.8 to 3.3 mm.
As the positional relationship between the created socket and the ridge projected on the 3-D CT images coincided with that at the time of arthroscopy, the ridge was geographically proved to be the resident’s ridge.
The mean length of the ridge was 18.8 ± 1.4 mm with a range from 16.1 to 21.6 mm. The average maximum distance from the ridge to the posterior margin of the lateral notch wall was 9.3 ± 0.8 mm with a range from 7.7 to 10.8 mm. The ridge and the distal femoral axis formed a mean angle of 31.1 ± 2.0° with a range from 26° to 36° (Fig. 3).
3-D CT pictures showing the lateral aspect of the intercondylar notch wall after the ACL reconstruction. a Lateral view. I length of the resident’s ridge; d maximum distance from the ridge to the posterior margin of the lateral wall of the notch. Ø angle between the resident’s ridge (R) and the distal femoral axis (A). b 30° posterior-oblique view more clearly showing the resident’s ridge (black arrows)
Discussion
The most important finding in this study was that we have established the technique to arthroscopically delineate ACL femoral attachment area using the resident’s ridge as a landmark without bony notchplasty even in patients with chronic ACL-deficiency. While Hutchinson and Ash macroscopically found the resident’s ridge was present in 90% of the cadaveric knees they dissected, a combination of arthroscopy-magnified visualization through the anteromedial portal and the current soft tissue-removing technology using radiofrequency energy to preserve bony surface have made it possible to identify the ridge in 100% of the patients [8]. Thus, the arthroscopic technique shown in the current study is useful to consistently create anatomical femoral tunnel in ACL reconstruction without notchplasty.
While the cortical bone in the femoral attachment area behind the resident’s ridge is thicker as shown by Hutchinson and Ash, many surgeons have been using a burr to take down or flatten resident’s ridge to assure clear visualization and access to the over-the-top position during preparation of the intercondylar notch or notchplasty [8]. However, its use may not be recommended because of the following reasons: (1) loss of thicker cortical bone of the ACL attachment area might result in weakening of the tunnel aperture, and lead to potential widening of the femoral tunnel; (2) more bleeding might be brought from the exposed cancellous bone; and (3) ACL graft forces during passive flexion–extension movement increase markedly after notchplasty of only 2 mm [7, 10]. Thus, the technique shown in this study to visualize the resident’s ridge without bony notchplasty is more preferable to preserve the normal notch anatomy (Fig. 1b, 2b).
Some may be concerned with the adverse effect of radiofrequency energy used for superficial soft tissue clearage on the graft healing or remodeling. As it usually takes just a few minutes to clean up the soft tissues, only superficial soft tissues or cells around the attachment area might have been damaged. Actually, we have neither observed significant burn on the bony surface after soft tissue clearage (Figs. 1, 2) nor a patient suffering from poor graft healing. If the prolonged use of radiofrequency energy is avoided, cells from the bone marrow and from the surrounding area could be assumed to remain viable to contribute to graft healing.
Researchers have shown that the bony surface of the ACL attachment area as a direct type insertion onto the femur shows a concavity on bare bone surface [18]. The area is crescent in shape and located just posterior to the resident’s ridge/the lateral intercondylar ridge, and posteriorly extends to the posterior cartilage margin of the lateral femoral condyle [1–3, 6]. Ferretti et al. [5] showed the ridge on a 3-D laser picture of the lateral femoral condyle. Steckel et al. [16] clarified radiographical locations of the femoral insertions of the anteromedial and posterolateral bundles of ACL. Purnell et al. [11] demonstrated the resident’s ridge as the anterior border of ACL using high-resolution volume-rendering computed tomography. The location and shape of the attachment area depicted on the 3-D CT pictures in this study are in agreement with those former studies. This suggests that computed tomography is one of the feasible ways to visualize the attachment area in humans.
The 3-D CT evaluation in the current study showed that the maximum distance from the ridge to the posterior margin of the lateral notch wall or the width of the crescent-shaped area behind the ridge was less than 10 mm in most patients. This suggests that a single rectangular socket of 5 × 10 mm or two smaller round tunnels is more desirable than a single round tunnel of 10 mm or greater [9, 13, 16]. It is our belief that creating the tunnels inside the attachment areas is essential to avoid graft impingement to PCL or to the notch without notchplasty.
There are still controversies on surgical approaches to create anatomical femoral tunnel. Takahashi et al. [17] has introduced laser beam to aim at femoral tunnel through a tibial guide to facilitate the transtibial tunnel approach. However, the relatively narrow attachment area located far back in the lateral notch wall may not allow us to consistently drill robust anatomical femoral tunnel without cortical blowout through the central tibial tunnel [2, 4, 9, 13, 14]. Therefore, the trans-portal approach rather than the transtibial tunnel one may be recommended.
Currently, computer-assisted navigation ACL surgery is one of the topics in this field. As this resident’s ridge could be clearly visualized on the 3-D CT images, correct registration of the ridge as a reference landmark would be helpful to accurately create an anatomical femoral tunnel in CT-based computer-navigation ACL reconstruction.
Conclusions
The resident’s ridge is a useful landmark for the ACL femoral attachment area. The ridge is arthroscopically identifiable on the lateral intercondylar notch wall by non-mechanical removal of the soft tissues using radiofrequency energy without bony notchplasty. Thus, the resident’s ridge could be used as a reference landmark for anatomical femoral tunnel drilling in arthroscopic ACL reconstruction.
References
Amis AA, Jacob RP (1998) Anterior cruciate ligament graft positioning, tensioning and twisting. Knee Surg Sports Traumatol Arthosc 6:S2–S12
Arnold MP, Kooloos J, van Kampen A (2001) Single-incision misses the anatomical femoral anterior cruciate ligament insertion: a cadaver study. Knee Surg Sports Traumatol Arthosc 9:194–199
Colombet P, Robinson J, Christel P, Franceschi J-P, Dijan P, Bellier G, Sbihi A (2006) Morphology of anterior cruciate ligament attachments for anatomical reconstruction: a cadaveric dissection and radiographic study. Arthroscopy 22:984–992
Dargel J, Schmidt-Wiethoff R, Fischer S, Mader K, Koebke J, Schneider T (2009) Femoral bone tunnel placement using the transtibial tunnel or the anteromedial portal in ACL reconstruction: a radiographic evaluation. Knee Surg Sports Traumatol Arthosc 17:220–227
Ferretti M, Ekdahl M, Shen W, Fu FH (2007) Osseous landmarks of the femoral attachment of the anterior cruciate ligament: an anatomic study. Arthroscopy 23:1218–1225
Giron F, Cuomo P, Aglietti P, Bull AMJ, Amis AA (2006) Femoral attachment of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthosc 14:250–256
Hame SL, Markolf KL, Hunter M, Oakes D, Zoric B (2003) Effects of notchplasty and femoral tunnel position on excursion patterns of an anterior cruciate ligament graft. Arthroscopy 19:340–345
Hutchinson MR, Ash SA (2003) Resident’s ridge: assessing the cortical thickness of the lateral wall and roof of the intercondylar notch. Arthroscopy 19:931–935
Mae T, Shino K, Matsumoto N, Hamada M, Nakata K (2007) Two-bundle ACL reconstruction using autogenous hamstring tendons—anatomical twin tunnel vs. Rosenberg’s bi-socket procedure: a biomechanical comparison in laxity match pretension. Knee Surg Sports Traumatol Arthosc 15:328–334
Markolf KL, Hame JF, Hunter M, Oakes D, Gause P (2002) Biomechanical effects of femoral notchplasty in anterior cruciate ligament reconstruction. Am J Sports Med 30:83–89
Purnell ML, Larson AI, Clancy WG (2008) Anterior cruciate ligament insertions on the tibia and femur and their relationships to critical bony landmarks using high-resolution volume-rendering computed tomography. Am J Sports Med 36:2083–2090
Shino K, Horibe S, Hamada M, Nakamura N, Nakata K, Mae T, Toritsuka Y (2002) Allograft anterior cruciate ligament reconstruction. Tech Knee Surg 1:78–85
Shino K, Nakata K, Nakamura N, Mae T, Ohtsubo H, Iwahashi T, Nakagawa S (2005) Anatomical ACL reconstruction using two double-looped hamstring tendon grafts via twin femoral and triple tibial tunnels. Oper Tech Orthop 15:130–134
Shino K, Nakata K, Horibe S, Nakamura N, Toritsuka Y, Nakagawa S, Suzuki T (2008) Rectangular tunnel double-bundle anterior cruciate ligament reconstruction with bone–patellar tendon–bone graft to mimic natural fiber arrangement. Arthroscopy 24:1178–1183
Siebold R, Ellert T, Metz S, Metz J (2008) Femoral insertions of the anteromedial and posterolateral bundles of the anterior cruciate ligament: morphometry and arthroscopic orientation models for double-bundle bone tunnel placement—a cadaver study. Arthroscopy 24:585–592
Steckel H, Musahl V, Fu FH (2009) The femoral insertions of the anteromedial and posterolateral bundles of the anterior cruciate ligament: a radiographic evaluation. Knee Surg Sports Traumatol Arthosc, (in press) published online. doi:10.1007/s00167-009-0852-7
Takahashi T, Takeda H, Watanabe S, Yamamoto H (2009) Laser-guided placement of the tibial guide in the transtibial technique for anterior cruciate ligament reconstruction. Arthroscopy 25:212–214
Weiler A, Scheffler S, Apreleva M (2005) Healing of ligament and tendon to bone. In: Walsh WR (ed) Orthopaedic biology and medicine: repair and regeneration of ligaments, tendons, and joint capsule. Humana Press, Totowa, pp 201–231
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
(AVI 9036 kb)
Rights and permissions
About this article
Cite this article
Shino, K., Suzuki, T., Iwahashi, T. et al. The resident’s ridge as an arthroscopic landmark for anatomical femoral tunnel drilling in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 18, 1164–1168 (2010). https://doi.org/10.1007/s00167-009-0979-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-009-0979-6