Abstract
Patellar tendon autografts are not suitable for multibundle ACL reconstruction, a procedure that reportedly enhances postoperative knee stability. Biomechanical studies recommend lateral placement of the femoral tunnel for single-bundle reconstruction to improve postoperative knee kinematics. We asked whether a lateralized single-bundle patellar tendon graft (LSBP) would provide good short-term results of ACL reconstruction comparable to double-bundle hamstring tendon grafts (DBH). We prospectively followed 144 patients with unilateral ACL rupture treated with either LSBP or DBH in a nonrandomized fashion. Twenty-four female and 31 male patients with LSBP and 44 female and 26 male patients with DBH were followed for a minimum of 24 months (average, 38 months; range, 24–56 months). The patients with LSBP recovered knee extension better at 1 month compared with the patients with DBH, but extension was similar after 3 months. We observed no differences in the side-to-side difference of KT1000™ measurement, pivot shift test, or anterior drawer test between LSBP and DBH. Although better recovery of hamstring strength in LSBP and better recovery of quadriceps strength in DBH were observed in the early postoperative period, these differences disappeared after 12 months. There was no difference in International Knee Documentation Committee objective evaluation between LSBP and DBH at the final followup.
Level of Evidence: Level II, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Arthroscopic ACL reconstruction has been widely accepted as a major option of treatment for ACL-deficient knees, replacing nonoperative treatment [3, 5]. The choice of graft for ACL reconstruction, however, is controversial. Although patellar tendon autograft and hamstring tendon autograft are the most popular graft substitutes, previous prospective, randomized studies suggest differing conclusions regarding whether one of these two autografts was superior to the other in functional outcomes after single-bundle ACL reconstruction. Poolman et al. [34] systematically reviewed 11 published meta-analyses [4, 6–8, 11, 14, 35, 41, 44, 47, 57] comparing patellar tendon graft and hamstring tendon graft for single-bundle ACL reconstruction. Some of these studies reported differences in postoperative knee stability [4, 8, 11, 35, 57], incidence of anterior knee pain [4, 8, 11, 35, 44, 47], and range of knee motion [6–8, 35, 47] between the two grafts. The other studies, however, were inconclusive concerning differences in postoperative knee function, and it was difficult to find evidence indicating the superiority of either type of graft.
However, two biomechanical studies elucidated the force-sharing mechanism in two anatomic bundles of the ACL [9, 38]. Because the posterolateral bundle (PLB) decreases knee laxity, especially rotatory laxity in near extension, neither the patellar tendon nor the hamstring tendon transplanted vertically as the single-bundle graft replacing the anteromedial bundle (AMB) should be sufficient to reproduce function of the normal ACL [49]. This current view has shifted the main focus in ACL reconstruction from simple restoration of anterior knee laxity to restraining more complex loads such as a combined rotatory load, and double-bundle ACL reconstruction has been recommended instead of anteromedial single-bundle reconstruction [28, 51]. Numerous clinical studies suggest double-bundle ACL reconstruction with a hamstring tendon graft provides superior postoperative rotatory laxity compared with single-bundle reconstruction [21, 25, 30, 43, 50, 55]. A patellar tendon autograft, however, is not used as a graft source for double-bundle ACL reconstruction because multiple strands of graft material are required in multibundle reconstruction. For reconstructing with a patellar tendon autograft, the lateralized single-bundle reconstruction technique, in which placement of the femoral tunnel was shifted laterally from the 11 o’clock position to the 10 o’clock position in the right knee and from the 1 o’clock position to the 2 o’clock position in the left knee, has been proposed as an effective restraint of rotatory loads [27]. One biomechanical study reported a laterally placed single-bundle graft functioned to control anterior force and rotatory moment in lower knee flexion comparable to a double-bundle graft [52].
We asked whether lateralized single-bundle patellar tendon graft (LSBP) or double-bundle hamstring tendon graft (DBH) would yield better postoperative outcomes, including (1) incidence of ACL reinjury and contralateral ACL injury; (2) range of knee extension; (3) anterior and rotatory knee laxity; (4) knee extension and flexion muscular strength; (5) incidence of anterior knee pain; and (6) functional knee score.
Materials and Methods
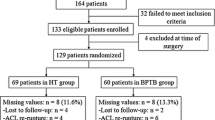
We designed this prospective comparison study to identify any differences in clinical outcomes of ACL reconstruction between LSBP and DBH. From July 2003 to November 2005, we admitted 158 patients for ACL reconstruction. Of the 158 patients, we enrolled 144 for surgical treatment of an isolated unilateral ACL injury meeting the following inclusion criteria: (1) no history of surgeries on bilateral knees; (2) closed femoral and tibial physes on MRI [39]; and (3) no or minimal degenerative osteochondral changes on radiographic examination (Stage 0 or 1 in the Kellgren and Lawrence staging system [24]). None of the 144 patients fulfilling the criteria declined to participate. All patients were competitive amateur athletes or recreational sports players and had injured their ACL in association with sports activities. Patient assignment to the LSBP and DBH groups was not randomized and the choice was made by the patients. The patients received information concerning which graft was to be used at least 1 week before surgery. The following three points were emphasized. First, previous meta-analysis studies of the single-bundle reconstruction have shown patellar tendon graft has an advantage in obtaining knee laxity closer to the normal knee and hamstring tendon graft has an advantage in reducing donor site morbidity, whereas overall clinical outcome of both reconstructions is similar [34]. Second, biomechanical laboratory studies suggest LSBP and DBH improve knee kinematics compared with anteromedial single-bundle reconstruction [27, 28, 51]. Third, differences in overall success rate, incidence of graft failure, or rate of return to sports between LSBP and DBH, however, had not been established. The patients made their decisions concerning graft selection by the day before surgery; 27 female patients (LSBP-F group) and 35 male patients (LSBP-M group) chose the LSBP, and 50 female patients (DBH-F group) and 32 male patients (DBH-M group) chose the DBH (Table 1). Anterior knee laxity, range of knee extension, and muscular strength were selected as key variables because these could be examined quantitatively. Our power analysis showed the smallest study population in each group was 17 for more than 80% of statistical power if there was a difference of 1.0 mm with a standard deviation of 1.0 mm in the side-to-side difference of KT1000™ measurement, a difference of 1.0 cm with a standard deviation of 1.0 cm in the heel height difference, or a difference of 10% with a standard deviation of 10% in the normalized peak torque of knee extension and flexion among the groups. The study design was approved by the ethics committees in our institution, and all patients provided informed consent.
One patient each in the LSBP-F group, the LSBP-M group, and the DBH-F group and three patients in the DBH-M group tore their contralateral ACL in sports activities. These six patients were excluded from this study, and an additional 13 patients were lost to followup owing to unknown change of address or unknown reason. Consequently, 24 (89%) patients in the LSBP-F group, 31 (89%) patients in the LSBP-M group, 44 (88%) patients in the DBH-F group, and 26 (81%) patients in the DBH-M group were followed for a minimum of 24 months (mean, 38 months; range, 24–56 months). Two patients each in the LSBP-F group and the DBH-F group and one patient in the LSBP-M group had graft failure resulting from reinjury and underwent revision reconstruction surgery within 2 years postoperatively. For these five patients, the postoperative clinical data recorded immediately before the revision surgery were included as the data at the final followup. There were no differences in average age, preinjury Tegner activity level [46], period from injury to surgery, or followup period among the four groups. There were no differences in the incidence of meniscus injury or the treatment methods among the four groups (Table 2). We observed no patients with cartilage injury that required supplemental surgical procedures.
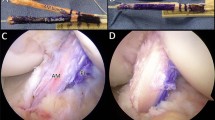
One surgeon (YI) performed or directly supervised (made all important surgical decisions) the ACL reconstructions with LSBP or DBH in all patients. The associated injury of the medial and lateral meniscus was treated with inside-out sutures or partial resection. The small longitudinal tear localized in the posterior portion of the lateral meniscus usually was left without any treatment. For single-bundle reconstruction, a 10-mm-wide bone-patellar tendon-bone was harvested through two horizontal skin incisions made on the patellar and tibial attachment [48]. The tibial tunnel was placed in the anterior half of the ACL tibial footprint using a commercially available tibial aimer (B. Braun Aesculap, Tuttlingen, Germany) (Fig. 1). Based on our anatomic study [20], the guidewire was diverted 35° to 40° in the coronal plane and 40° to 45° in the sagittal plane from the tibial long axis to easily access the target area for the femoral tunnel placement using a transtibial endoscopic technique (Fig. 2). The tibial tunnel was completed using a coring reamer instead of a drill bit to collect the cored cancellous bone. The part of cored cancellous bone was sutured to the graft substance beside the tibial bone plug to infill the empty space in the tibial tunnel and secure the graft closer to the original ACL attachment [32]. The remaining part of the core bone was grafted into the patellar and tibial defects of the graft donor site [48]. A virtual clock face was envisioned on the posterior wall of the intercondylar notch setting 12 o’clock on the top of the intercondylar notch and 6 o’clock on the tibial surface under arthroscopic observation. The guidewire for the femoral tunnel was placed at the 10 o’clock position using a transtibial stepoff guide (Arthrex, Inc, Naples, FL) and overdrilled to 10 or 11 mm of the diameter and 20 to 25 mm of the depth depending on the bone plug size, preserving 2- to 3-mm thickness of the posterior tunnel wall (Figs. 3, 4). The graft was secured using interference screws under manual maximum tensile load near full extension. For double-bundle reconstruction, the semitendinosus tendon and gracilis tendon were harvested with a tendon harvester through an anteromedial oblique skin incision. The gracilis tendon and the proximal half of the semitendinosus tendon were looped and used as the AMB and the distal half of the semitendinosus tendon was looped and used as the PLB. For the AMB, the tibial tunnel was placed in the anteromedial region of the ACL footprint (Fig. 1) at angles of 25° to 30° in the coronal plane and 40° to 45° in the sagittal plane from the tibial long axis (Fig. 2). The femoral tunnel was placed between the 10 and 11 o’clock positions using the transtibial step-off guide (Fig. 5). For the PLB, the tibial tunnel was placed in the posterolateral region of the ACL footprint (Fig. 1) at angles of 35° to 40° in the coronal plane and 30° to 35° in the sagittal plane from the tibial long axis (Fig. 2). The position of the femoral tunnel was determined according to the technique of Yasuda et al. [54]. The center of the femoral tunnel was placed on the virtual vertical line drawn from the contact point between the lateral femoral condyle and the tibial plateau at 90° knee flexion and was 5 to 8 mm apart from the edge of the joint cartilage (Fig. 5). Both grafts were secured to the femur using the EndoButton™ technique [36] (Acufex Microsurgical, Mansfield, MA) and fixed to the tibia with a post screw applying manual maximum tensile load at 20° to 30° knee flexion.
The photographs show the position of the tibial tunnel. (A) The tunnel dilator was inserted into the tibial tunnel placed on the anterior half of the ACL footprint in lateralized single-bundle reconstruction. (B) The gold dilator was inserted into the anteromedial tunnel placed on the anterior half of the footprint, and the silver dilator was inserted into the posterolateral tunnel placed on the posterior half of the footprint in double-bundle reconstruction.
The photographs show the direction of the tibial guidewire in (A) the coronal plane (α angle) and (B) sagittal plane (β angle). In the lateralized single-bundle reconstruction, the guidewire was inserted with 35° to 40° of the coronal angle (α angle) and 40° to 45° of the sagittal angle (β angle) from the tibial long axis. In double-bundle reconstruction, the α angle and β angle were 25° to 30° and 40° to 45° for the AMB and 35° to 40° and 30° to 35° for the PLB.
A photograph shows the position of the femoral tunnel in lateralized single-bundle reconstruction. The virtual clock face was placed on the posterior wall of the intercondylar notch with 12 o’clock on the top of the intercondylar notch and 6 o’clock on the tibial surface under arthroscopic 0bservation. The femoral tunnel (gray circle) was placed at the 10 o’clock position in the right knee.
A photograph shows the position of the femoral tunnel in double-bundle reconstruction. The femoral tunnel of the AMB (light blue circle) was placed between the 10 and 11 o’clock positions in the right knee. The femoral tunnel of the PLB (pink circle) was placed above the contact point between the lateral femoral condyle and the tibial plateau at 90° knee flexion.
From the day after surgery, range of motion exercises and isometric muscle exercises were started. Full weightbearing and closed kinetic chain exercises were allowed between 7 and 14 days. Running and open kinetic chain exercises were allowed at 2 months and 3 months, respectively. Jump-landing exercises were added after 3 months, and twisting and cutting exercises were added after 4 months. Return to full sports activities was permitted after 6 months.
We (ET, AF, HT, the treating surgeons) performed clinical examinations in the outpatient clinic preoperatively and at 1, 3, 6, 12, 18, and 24 months postoperatively and every 6 or 12 months thereafter. The loss of extension was evaluated by measuring heel-height difference in the prone position [37]. Knee laxity was evaluated by a manual maximum laxity test with a KT1000™ arthrometer (MEDmetric Corp, San Diego, CA) that measured the anterior tibial translation applying the manual maximum anterior tibial load, pivot shift test, and anterior drawer test. Evaluation of the muscular strength around the knee was performed preoperatively and restarted 3 months postoperatively. Isokinetic peak torque in concentric knee extension and flexion was measured with an isokinetic dynamometer (Cybex6000; Lumex, Inc, Ronkonkoma, NY) at an angular velocity of 60° per second and the normalized peak torque was determined by dividing by the measurement value of the contralateral uninjured limb. Anterior knee pain was evaluated with a knee walking test and graded into normal, unpleasant, difficult, and impossible [22]. Overall knee function was classified according to the International Knee Documentation Committee (IKDC) objective evaluation form [17].
Differences in heel-height difference, side-to-side difference of KT1000™ measurement, and normalized peak torque in knee extension and flexion among the four groups (the two operations, male and female) were determined by the multiple comparison procedure with Tukey’s honestly significant differences test. Differences in pivot shift test, anterior drawer test, knee walking test, and IKDC evaluation among the four groups were determined by the chi square test. We used SPSS® Version 16.0 software (SPSS Inc, Chicago, IL) for all analyses.
Results
The LSBP-F and the LSBP-M groups had earlier recovery from knee extension deficit compared with the DBH-F and the DBH-F groups. The average (± standard deviation) heel-height differences of the LSBP-F group (2.7 ± 2.5 cm) and the LSBP-M group (2.9 ± 2.2 cm) were smaller than those of the DBH-F group (4.7 ± 2.9 cm) (p = 0.019 and p = 0.040) and the DBH-M group (4.7 ± 2.6 cm) (p = 0.030 and p = 0.046) at 1 month postoperatively (Table 3). The differences in the heel-height difference among the four groups were no longer (p = 0.145 to p = 1.000) present after 3 months postoperatively.
Anterior and rotatory knee laxity measurements were similar (p = 0.064 to p = 1.000) in the four groups. We detected no differences in the side-to-side difference of KT1000™ measurement among the four groups at any time (Table 4). At the final followup, the average side-to-side differences of KT1000™ measurement were 1.4 ± 1.5 mm for the LSBP-F group, 1.1 ± 0.9 mm for the LSBP-M group, 1.3 ± 1.5 mm for the DBH-F group, and 1.3 ± 1.5 mm for the DBH-M group. The number of patients who had a positive pivot shift test (Grades I, II, and III) at the final followup were five (21%) in the LSBP-F group, four (13%) in the LSBP-M group, seven (16%) in the DBH-F group, and five (19%) in the DBH-M group (Table 5). The number of patients who had a positive anterior drawer test (Grades I, II, and III) at the final followup were five (21%) in the LSBP-F group, five (16%) in the LSBP-M group, nine (20%) in the DBH-F group, and five (19%) in the DBH-M group (Table 5). There were no differences in the results of the pivot shift test (p = 0.933) or anterior drawer test (p = 0.879) among the four groups.
The DBH-F and DBH-M groups had earlier recovery of quadriceps strength, whereas the LSBP-F and LSBP-M groups showed earlier recovery of hamstrings strength. At 3 months postoperatively, the normalized peak torque in knee extension of the LSBP-F group (54% ± 16%) was less than those of the DBH-F group (63% ± 17%) (p = 0.047) and the DBH-M group (72% ± 21%) (p = 0.001), and the normalized peak torque in knee extension of the LSBP-M group (59% ± 15%) was less than that of the DBH-M group (p = 0.030) (Table 6). However, the normalized peak torque in knee flexion of the LSBP-F group (82% ± 18%) was greater (p = 0.015) than that of the DBH-F group (72% ± 13%), and that of the LSBP-M group (85% ± 19%) was greater than those of the DBH-F group (p = 0.003) and the DBH-M group (68% ± 7%) (p = 0.001) (Table 7). Also, 6 months postoperatively, the normalized peak torques in knee flexion of the LSBP-F group (92% ± 13%) and the LSBP-M group (93% ± 11%) were greater than those of the DBH-F group (84% ± 12%) (p = 0.040 and p = 0.002) and the DBH-M group (80% ± 9%) (p = 0.002 and p = 0.001). However, no differences (p = 0.575 to p = 1.000) in the normalized peak torques in knee extension or flexion were present among the four groups at the final followup.
The results in the knee walking test were similar (p = 0.916) in the four groups. The number of patients graded as having a normal result in the knee walking test at the final followup were 19 (83%) in the LSBP-F group, 27 (87%) in the LSBP-M group, 37 (84%) in the DBH-F group, and 21 (85%) in the DBH-M group, representing no difference among the four groups (Table 8). Only one patient in the DBH-F group had a result graded as difficult and no patient had a result graded as impossible in the knee walking test.
We observed no difference (p = 0.876) in the IKDC objective evaluation among the four groups. The patients with results graded as normal at the final followup accounted for 71% of the LSBP-F group, 77% of the LSBP-M group, 73% of the DBH-F group, and 73% of the DBH-M group (Table 9). Five of seven patients who had results that were graded as abnormal or severely abnormal had ACL graft reinjuries.
Discussion
In comparison to hamstring tendon autografts, one of the clinical disadvantages of patellar tendon autografts is they are not suitable for multibundle ACL reconstruction, which could improve postoperative knee stability. Biomechanical studies recommend lateral placement of the femoral tunnel for the single-bundle graft to restore knee kinematics closer to double-bundle reconstruction [27, 52]. We compared range of knee extension, anterior and rotatory knee laxity, knee extension and flexion muscular strength, incidence of anterior knee pain, and functional knee score between LSBP and DBH.
We note several limitations. Using the popular surgical technique for each graft, the patellar tendon graft was fixed with interference screws at full extension in single-bundle reconstruction, whereas the hamstring tendon graft was fixed with an EndoButton™ and a post screw at 20° to 30° knee flexion. These multiple variables in graft type and the fixation techniques might have contributed to some of the differences in the results. In addition to the relatively small number of patients, the number of patients differed among the four groups because we did not randomly assign patients to LSBP and DBH. The DBH-F group was largest having 50 patients, whereas the other three groups had 27 to 30 patients. Although the exact reason was unknown; we supposed a cosmetic factor was one of the reasons why the female patients preferred DBH rather than LSBP. Two horizontal incisions are required to harvest a patellar tendon graft, whereas only one oblique incision is used for a hamstring tendon graft. Although the patient profiles, including age, preinjury activity level, period from injury to surgery, and followup, were similar, there might be unknown bias of patient profiles among the four groups. In our evaluation of knee laxity, only anterior knee laxity at lower flexion was examined quantitatively using the KT1000™ arthrometer, whereas anterior knee laxity at deep flexion and rotatory stability were just graded with the anterior drawer test and pivot shift test, respectively. The lack of quantitative measurement in various loading conditions might have obscured small but crucial differences in postoperative knee laxity among the groups. Recently, a new measurement system consisting of electromagnetic sensors was described, which provided some quantitative data to analyze knee kinematics during the pivot shift test [26, 50]. A measurement device that can quantify the rotational change of the knee and the anterior tibial translation in deep flexion needs to be developed.
The patients in the LSBP-F and LSBP-M groups recovered range of knee extension earlier than the patients in the DBH-F and DBH-M groups, representing a smaller heel-height difference at 1 month postoperatively. The flexion angle of the knee at the fixation of the ACL graft might contribute to the difference in extension loss between LSBP and DBH at the postoperative early phase. Because the suspension-type soft tissue fixation with linkage materials has larger loss of fixation compared with the rigid bone-plug fixation with interference screws [40], both hamstring tendon grafts for AMB and PLB were secured simultaneously at 20° to 30° knee flexion, whereas the patellar tendon graft was secured near full extension in this study. Cadaveric studies have reported the PLB shows a tension pattern that is taut in extension and slack in flexion [2] and less isometricity with approximately two times larger length change of the AMB when the intact knee is passively moved through full extension to 90° flexion [15]. Similar results in length change of the transplanted double-bundle grafts were obtained from intraoperative measurements [19, 56]. Therefore, the PLB graft of DBH fixed at 20° to 30° knee flexion applying a manual maximum tensile load might be overloaded when approaching full extension and cause loss of extension. Although some studies have been performed to determine the ideal combination of knee angles and initial graft tension at the fixation of AMB and PLB grafts [16, 29, 53], it has not been established. Because the graft tensioning might contribute to the remodeling process of the graft and to the long-term clinical results consequently, additional study is required.
The patients in the LSBP-F and LSBP-M groups recovered knee extension and hamstring strength earlier, whereas the patients in the DBH-F and DBH-M groups had earlier recovery of quadriceps strength. However, at the final followup more than 2 years after surgery, no differences were detected in any functional evaluation.
Several clinical studies reported better postoperative knee laxity in double-bundle reconstruction compared with single-bundle reconstruction; however, it is still controversial (Table 10). In two articles [1, 12], double-bundle reconstruction, in which the hamstring tendon graft was transplanted into one tibial and two femoral tunnels, did not provide superior postoperative outcomes over single-bundle reconstruction. In the remaining eight articles [21, 25, 30, 31, 43, 45, 50, 55], the AMB and PLB were replicated by grafting the hamstring tendons into two tibial and two femoral tunnels in double-bundle reconstruction. Double-bundle reconstruction obtained better results in the KT1000™/KT2000™ measurement [25, 30, 31, 55], pivot shift test [21, 25, 30, 43, 50, 55], or IKDC objective evaluation [43], or had less frequency of graft failure [21] in seven of eight studies. A recent biomechanical laboratory study showed the two tibial tunnel technique more effectively restores knee kinematics in response to anterior and rotatory loads compared with the one tibial tunnel technique [33] and supported the differences in the results of the clinical studies. These previous comparison studies involved only surgeries using hamstring tendon grafts and it was suitable to simply analyze the effects of different surgical techniques such as single-bundle and double-bundle reconstruction. However, it raises the question whether double-bundle reconstruction with a hamstring tendon graft is superior to ACL reconstruction with other types of graft. Furthermore, because the previous studies had a tendency to focus mainly on comparing the clinical outcomes between anteromedially placed single-bundle reconstruction and double-bundle reconstruction, another question was whether a single-bundle graft transplanted into a lateralized femoral tunnel would obtain the results comparable to double-bundle reconstruction.
We used two types of substitute, patellar tendon graft and hamstring tendon graft; these were transplanted with a lateralized single-bundle reconstruction technique and a double-bundle reconstruction technique. Because the patellar tendon graft could not be used for double-bundle reconstruction, we used two techniques to reinforce postoperative knee stability in single-bundle reconstruction. First, we used an additional bone plug in the tibial tunnel to minimize unfavorable graft-tunnel motion, the so-called windshield wiper phenomenon, and decrease the anterior tibial translation [18]. Second, we used lateral placement of the femoral tunnel to better control rotatory laxity [27]. The combination of these techniques might have contributed to the results of the postoperative knee laxity examinations in the LSBP-F and LSBP-M groups, which were similar to those in the DBH-F and DBH-M groups. However, we have no clear way of confirming whether the results related to these two techniques are attributable to some other variables.
The transtibial endoscopic technique we used for single- and double-bundle reconstructions has been preferred rather than the two-incision technique as a less invasive approach. The laboratory studies, however, showed some technical difficulties in correctly placing the femoral tunnel through the tibial bone tunnel [10, 13, 23]. We carefully placed the femoral tunnel by controlling the direction of the tibial tunnel based on a previous anatomic study [20] in which the ideal direction of the tibial tunnel to access the target area for femoral tunnel placement using the transtibial technique was described. Because displacement of the femoral tunnel drastically alters graft function in single- and double-bundle reconstructions [27, 58], inaccurate positioning of the femoral tunnel could result in inferior postoperative knee laxity. In this study and in previous clinical studies comparing single- and double-bundle reconstructions, however, it was not validated using any imaging techniques postoperatively whether the femoral tunnel was placed in the desired position. To clarify the effects of single- and double-bundle reconstructions on clinical outcomes, it is necessary to postoperatively investigate whether the location of the femoral tunnel is appropriate.
Because the biomechanical behavior of the laterally placed single-bundle graft is close to that of the PLB of the normal ACL, the anterior knee laxity increases going from extension to deep flexion [27]. Theoretically, we expected lateralized single-bundle reconstruction would restore anterior knee stability with lesser degrees of flexion in KT1000™ measurement but not with greater degrees of flexion and a higher rate of positive anterior drawer tests compared with double-bundle reconstruction. However, the data did not support this theoretical expectation and the rates of positive anterior drawer tests in the LSBP-F and LSBP-M groups were lowered to the same level as those in the DBH-F and DBH-M groups at the final followup. Recently, Shino et al. [42] reported the anterior and posterior fibers of the anatomically placed patellar tendon graft could behave and function as the AMB and the PLB of the normal ACL, respectively. Although it was difficult to precisely control fiber orientation of the patellar tendon graft during our surgical procedures, the running course of the anterior and posterior portions of the transplanted patellar tendon graft might correspond to that of the AMB and the PLB of the normal ACL in some patients.
We found similar overall results with ACL reconstructions with LSBP and DBH in our short-term study. We are not implying double-bundle reconstruction does not have any advantages over single-bundle reconstruction. We realize the usefulness of data on a short-term clinical study is limited and the examination techniques available currently may not be sensitive enough to detect small but potentially important differences between ACL reconstructions with LSBP and DBH. However, the data suggest comparable clinical results for ACL reconstruction with DBH or LSBP when placed in the appropriate position laterally instead of anteromedially.
References
Adachi N, Ochi M, Uchio Y, Iwasa J, Kuriwaka M, Ito Y. Reconstruction of the anterior cruciate ligament: single- versus double-bundle multistranded hamstring tendons. J Bone Joint Surg Br. 2004;86:515–520.
Amis AA, Dawkins GP. Functional anatomy of the anterior cruciate ligament: fibre bundle actions related to ligament replacements and injuries. J Bone Joint Surg Br. 1991;73:260–267.
Barrack RL, Bruckner JD, Kneisl J, Inman WS, Alexander AH. The outcome of nonoperatively treated complete tears of the anterior cruciate ligament in active young adults. Clin Orthop Relat Res. 1990;259:192–199.
Biau DJ, Tournoux C, Katsahian S, Schranz PJ, Nizard RS. Bone-patellar tendon-bone autografts versus hamstring autografts for reconstruction of anterior cruciate ligament: meta-analysis. BMJ. 2006;332:995–1001.
Bonamo JJ, Fay C, Firestone T. The conservative treatment of the anterior cruciate deficient-knee: a review. Clin Sports Med. 1993;12:625–636.
Dauty M, Tortellier L, Rochcongar P. Isokinetic and anterior cruciate ligament reconstruction with hamstrings or patella tendon graft: analysis of literature. Int J Sports Med. 2005;26:599–606.
Forster MC, Forster IW. Patellar tendon or four-strand hamstring? A systematic review of autografts for anterior cruciate ligament reconstruction. Knee. 2005;12:225–230.
Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR Jr. Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31:2–11.
Gabriel MT, Wong EK, Woo SL, Yagi M, Debski RE. Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res. 2004;22:85–89.
Giron F, Cuomo P, Edwards A, Bull AM, Amis AA, Aglietti P. Double-bundle “anatomic” anterior cruciate ligament reconstruction: a cadaveric study of tunnel positioning with a transtibial technique. Arthroscopy. 2007;23:7–13.
Goldblatt JP, Fitzsimmons SE, Balk E, Richmond JC. Reconstruction of the anterior cruciate ligament: meta-analysis of patellar tendon versus hamstring tendon autograft. Arthroscopy. 2005;21:791–803.
Hamada M, Shino K, Horibe S, Mitsuoka T, Miyama T, Shiozaki Y, Mae T. Single- versus bi-socket anterior cruciate ligament reconstruction using autogenous multiple-stranded hamstring tendons with EndoButton femoral fixation: a prospective study. Arthroscopy. 2001;17:801–807.
Heming JF, Rand J, Steiner ME. Anatomical limitations of transtibial drilling in anterior cruciate ligament reconstruction. Am J Sports Med. 2007;35:1708–1715.
Herrington L, Wrapson C, Matthews M, Matthews H. Anterior cruciate ligament reconstruction hamstring versus bone-patella tendon-bone grafts: a systematic literature review of outcome from surgery. Knee. 2005;12:41–50
Hollis JM, Takai S, Adams DJ, Horibe S, Woo SL. The effects of knee motion and external loading on the length of the anterior cruciate ligament (ACL): a kinematic study. J Biomech Eng. 1991;113:208–214.
Hoshino Y, Kuroda R, Nagamune K, Nishimoto K, Yagi M, Mizuno K, Yoshiya S, Kurosaka M. The effect of graft tensioning in anatomic 2-bundle ACL reconstruction on knee joint kinematics. Knee Surg Sports Traumatol Arthrosc. 2007;15:508–514.
Irrgang JJ, Ho H, Harner CD, Fu FH. Use of the International Knee Documentation Committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1998;6:107–114.
Ishibashi Y, Rudy TW, Livesay GA, Stone JD, Fu FH, Woo SL. The effect of anterior cruciate ligament graft fixation site at the tibia on knee stability: evaluation using a robotic testing system. Arthroscopy. 1997;13:177–182.
Ishibashi Y, Tsuda E, Fukuda A, Tsukada H, Toh S. Intraoperative biomechanical evaluation of anatomic anterior cruciate ligament reconstruction using a navigation system: comparison of hamstring tendon and bone-patellar tendon-bone graft. Am J Sports Med. 2008;36:1903–1912.
Ishibashi Y, Tsuda E, Sato H, Tanaka T, Kumagai G, Toh S. Anatomical study of appropriate tibial tunnel direction for anatomic femoral tunnel placement and lateral femoral tunnel placement. J Japan Arthrosc Assoc. 2004;29:39–43.
Järvelä T. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective, randomize clinical study. Knee Surg Sports Traumatol Arthrosc. 2007;15:500–507.
Kartus J, Movin T, Karlsson J. Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy. 2001;17:971–980.
Kaseta MK, DeFrate LE, Charnock BL, Sullivan RT, Garrett WE Jr. Reconstruction technique affects femoral tunnel placement in ACL reconstruction. Clin Orthop Relat Res. 2008;466:1467–1474.
Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502.
Kondo E, Yasuda K, Azuma H, Tanabe Y, Yagi T. Prospective clinical comparisons of anatomic double-bundle versus single-bundle anterior cruciate ligament reconstruction procedures in 328 consecutive patients. Am J Sports Med. 2008;36:1675–1687.
Kubo S, Muratsu H, Yoshiya S, Mizuno K, Kurosaka M. Reliability and usefulness of a new in vivo measurement system of the pivot shift. Clin Orthop Relat Res. 2007;454:54–58.
Loh JC, Fukuda Y, Tsuda E, Steadman RJ, Fu FH, Woo SL. Knee stability and graft function following anterior cruciate ligament reconstruction: comparison between 11 o’clock and 10 o’clock femoral tunnel placement. Arthroscopy. 2003;19:297–304.
Mae T, Shino K, Matsumoto N, Nakata K, Nakamura N, Iwahashi T. Force sharing between two grafts in the anatomical two-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14:505–509.
Miura K, Woo SL, Brinkley R, Fu YC, Noorani S. Effects of knee flexion angles for graft fixation on force distribution in double-bundle anterior cruciate ligament grafts. Am J Sports Med. 2006;34:577–585.
Muneta T, Koga H, Mochizuki T, Ju YJ, Hara K, Nimura A, Yagishita K, Sekiya I. A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy. 2007;23:618–628.
Muneta T, Koga H, Morito T, Yagishita K, Sekiya I. A retrospective study of the midterm outcome of two-bundle anterior cruciate ligament reconstruction using quadrupled semitendinosus tendon in comparison with one-bundle reconstruction. Arthroscopy. 2006;22:252–258.
Otsuka H, Ishibashi Y, Tsuda E, Sasaki K, Toh S. Comparison of three techniques of anterior cruciate ligament reconstruction with bone-patellar tendon-bone graft: differences in anterior tibial translation and tunnel enlargement with each technique. Am J Sports Med. 2003;31:282–288.
Petersen W, Tretow H, Weimann A, Herbort M, Fu FH, Raschke M, Zantop T. Biomechanical evaluation of two techniques for double-bundle anterior cruciate ligament reconstruction: one tibial tunnel versus two tibial tunnels. Am J Sports Med. 2007;35:228–234.
Poolman RW, Abouali JA, Conter HJ, Bhandari M. Overlapping systematic reviews of anterior cruciate ligament reconstruction comparing hamstring autograft with bone-patellar tendon-bone autograft: why are they different? J Bone Joint Surg Am. 2007;89:1542–1552.
Prodromos CC, Joyce BT, Shi K, Keller BL. A meta-analysis of stability after anterior cruciate ligament reconstruction as a function of hamstring versus patellar tendon graft and fixation type. Arthroscopy. 2005;21:1202.
Rosenberg TD, Deffner KT. ACL reconstruction: semitendinosus tendon is the graft of choice. Orthopedics. 1997;20:396–398.
Sachs RA, Daniel DM, Stone ML, Garfein RF. Patellofemoral problems after anterior cruciate ligament reconstruction. Am J Sports Med. 1989;17:760–765.
Sakane M, Fox RJ, Woo SL, Livesay GA, Li G, Fu FH. In situ forces in the anterior cruciate ligament and its bundles in response to anterior tibial loads. J Orthop Res. 1997;15:285–293.
Sasaki T, Ishibashi Y, Okamura Y, Toh S, Sasaki T. MRI evaluation of growth plate closure rate and pattern in the normal knee joint. J Knee Surg. 2002;15:72–76.
Scheffler SU, Südkamp NP, Göckenjan A, Hoffmann RF, Weiler A. Biomechanical comparison of hamstring and patellar tendon graft anterior cruciate ligament reconstruction techniques: the impact of fixation level and fixation method under cyclic loading. Arthroscopy. 2002;18:304–315.
Schultz WR, Carr CF. Comparison of clinical outcomes of reconstruction of the anterior cruciate ligament: autogenous patellar tendon and hamstring grafts. Am J Orthop. 2002;31:613–620.
Shino K, Nakata K, Nakamura N, Toritsuka Y, Nakagawa S, Horibe S. Anatomically oriented anterior cruciate ligament reconstruction with a bone-patellar tendon-bone graft via rectangular socket and tunnel: a snug-fit and impingement-free grafting technique. Arthroscopy. 2005;21:1402.
Siebold R, Dehler C, Ellert T. Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2008;24:137–145.
Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE Jr. Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med. 2004;32:1986–1995.
Streich NA, Friedrich K, Gotterbarm T, Schmitt H. Reconstruction of the ACL with a semitendinosus tendon graft: a prospective randomized single blinded comparison of double-bundle versus single-bundle technique in male athletes. Knee Surg Sports Traumatol Arthrosc. 2008;16:232–238.
Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49.
Thompson J, Harris M, Grana WA. Patellofemoral pain and functional outcome after anterior cruciate ligament reconstruction: an analysis of the literature. Am J Orthop. 2005;34:396–399.
Tsuda E, Okamura Y, Ishibashi Y, Otsuka H, Toh S. Techniques for reducing anterior knee symptoms after anterior cruciate ligament reconstruction using a bone-patellar tendon-bone autograft. Am J Sports Med. 2001;29:450–456.
Woo SL, Kanamori A, Zeminski J, Yagi M, Papageorgiou C, Fu FH. The effectiveness of reconstruction of the anterior cruciate ligament with hamstrings and patellar tendon: a cadaveric study comparing anterior tibial and rotational loads. J Bone Joint Surg Am. 2002;84:907–914.
Yagi M, Kuroda R, Nagamune K, Yoshiya S, Kurosaka M. Double-bundle ACL reconstruction can improve rotational stability. Clin Orthop Relat Res. 2007;454:100–107.
Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:660–666.
Yamamoto Y, Hsu WH, Woo SL, Van Scyoc AH, Takakura Y, Debski RE. Knee stability and graft function after anterior cruciate ligament reconstruction: a comparison of a lateral and an anatomical femoral tunnel placement. Am J Sports Med. 2004;32:1825–1832.
Yasuda K, Ichiyama H, Kondo E, Miyatake S, Inoue M, Tanabe Y. An in vivo biomechanical study on the tension-versus-knee flexion angle curves of 2 grafts in anatomic double-bundle anterior cruciate ligament reconstruction: effects of initial tension and internal tibial rotation. Arthroscopy. 2008;24:276–284.
Yasuda K, Kondo E, Ichiyama H, Kitamura N, Tanabe Y, Tohyama H, Minami A. Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy. 2004;20:1015–1025.
Yasuda K, Kondo E, Ichiyama H, Tanabe Y, Tohyama H. Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among 3 different procedures. Arthroscopy. 2006;22:240–251.
Yonetani Y, Toritsuka Y, Yamada Y, Iwahashi T, Yoshikawa H, Shino K. Graft length changes in the bi-socket anterior cruciate ligament reconstruction: comparison between isometric and anatomic femoral tunnel placement. Arthroscopy. 2005;21:1317–1322.
Yunes M, Richmond JC, Engels EA, Pinczewski LA. Patellar versus hamstring tendons in anterior cruciate ligament reconstruction: a meta-analysis. Arthroscopy. 2001;17:248–257.
Zantop T, Diermann N, Schumacher T, Schanz S, Fu FH, Petersen W. Anatomical and nonanatomical double-bundle anterior cruciate ligament reconstruction: importance of femoral tunnel location on knee kinematics. Am J Sports Med. 2008;36:678–685.
Acknowledgments
We thank Eiki Tsushima, PhD, Hirosaki University School of Health Science, for statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent was obtained for participation in this study.
About this article
Cite this article
Tsuda, E., Ishibashi, Y., Fukuda, A. et al. Comparable Results Between Lateralized Single- and Double-bundle ACL Reconstructions. Clin Orthop Relat Res 467, 1042–1055 (2009). https://doi.org/10.1007/s11999-008-0604-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-008-0604-x