Abstract
In the brain, d-amino acid oxidase (DAAO) is a peroxisomal flavoenzyme. Through oxidative deamination by DAAO, d-serine, the main coagonist of synaptic N-methyl-d-aspartate receptors (NMDARs), is degraded into α-keto acids and ammonia; flavin adenine dinucleotide (FAD) is simultaneously reduced to dihydroflavine-adenine dinucleotide (FADH2), which is subsequently reoxidized to FAD, with hydrogen peroxide produced as a byproduct. NMDAR hypofunction is implicated in the pathogenesis of schizophrenia. In previous studies, compared with control subjects, patients with schizophrenia had lower d-serine levels in peripheral blood and cerebrospinal fluid but higher DAAO expression and activity in the brain. Inhibiting DAAO activity and slowing d-serine degradation by using DAAO inhibitors to enhance NMDAR function may be a new strategy for use in the treatment of schizophrenia. The aim of this leading article is to review the current research in DAAO inhibitors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Sodium benzoate and luvadaxistat (TAK-831) are two potent d-amino acid oxidase (DAAO) inhibitors. Clinical evidence suggests that both may be promising therapeutic agents to treat schizophrenia. |
Adjuvant treatment with sodium benzoate improved psychotic symptoms and cognitive impairment in patients with chronic schizophrenia. |
The results of INTERACT, a phase II trial, revealed that add-on TAK-831 improved cognitive function but not the negative symptoms of schizophrenia. |
The exact mechanism of action of DAAO inhibitors remains unclear. |
1 Introduction
Schizophrenia is a severe mental disorder, with an incidence of approximately 1% in all races [1]. In addition to positive and negative symptoms, cognitive impairment plays a major role in determining the overall function of patients with schizophrenia [2,3,4]. However, current antipsychotics developed based on dopaminergic and serotonergic theories have limited efficacy in negative symptoms and cognitive impairment [5, 6]. N-methyl-d-aspartate receptor (NMDAR) hypofunction is implicated in the pathogenesis of schizophrenia [7,8,9,10,11]. Ketamine and phencyclidine (PCP), two NMDAR antagonists, produced schizophrenia-like negative symptoms and cognitive impairment [12, 13]. Hyperlocomotion and increased stereotyped behaviors in knockout mice with NR1 subunit deficits were attenuated through treatment with antipsychotics [14]. In a genome-wide association study (GWAS) by the Psychiatric Genomic Consortium [15], 108 loci surpassed genome-wide significance; among them, several genes, including GRM3, GRIN2A, SRR and GRIA1, were related to glutamatergic transmission. The results of a recently published GWAS [16] employing a fine-mapping approach supported the pathological roles of two glutamatergic transmission-related genes, GRIN2A and SP4, in schizophrenia. The structures of NMDARs comprise several different combinations of subunits, such as GluN1/GluN2, GluN1/GluN2/GluN3 and GluN1/GluN3. NMDAR activation requires the simultaneous binding of glutamate and positive allosteric modulators (glycine or d-serine) to the GluN2 subunit and the glycine modulatory site (GMS) on the GluN1 subunit, respectively [17]. In general, GMSs are not fully saturated [18,19,20], and a small change in the concentrations of coagonists may alter NMDAR activity [21]. Clinical trials have demonstrated that some NMDAR-enhancing agents were beneficial to schizophrenia [22,23,24,25], even to antipsychotic-resistant schizophrenia [26, 27]. The results of a meta-analysis [28] which enrolled 40 randomized controlled trials of NMDAR-enhancing agents indicated that add-on treatment of NMDAR-enhancing agents significantly improved the negative symptoms in schizophrenia, even in treatment-refractory schizophrenia.
d-Serine, the main coagonist of synaptic NMDARs, is involved in excitatory neurotransmission, synaptic plasticity and cognitive behavior [29,30,31,32]. l-Serine is converted into d-serine through isomerization reactions catalyzed by serine racemase (SR) [33, 34]. Thereafter, d-serine is degraded by SR again through an α,β-elimination reaction [33, 35] or by d-amino acid oxidase (DAAO) through oxidative deamination [35, 36] and is ultimately removed from the synapse by the alanine-serine-cysteine transporter (Asc-1) [37, 38]. In the brain, DAAO is a peroxisomal flavoenzyme [35, 36]. Through oxidative deamination by DAAO, d-serine is degraded into α-keto acids and ammonia; flavin adenine dinucleotide (FAD) is simultaneously reduced to dihydroflavine-adenine dinucleotide (FADH2), which is subsequently reoxidized to FAD, with hydrogen peroxide produced as a byproduct [36] (Fig. 1). Compared with control samples, patients with schizophrenia had lower d-serine levels in peripheral blood [39, 40] and the cerebrospinal fluid [41] but higher DAAO expression and activity in the brain [42,43,44,45,46]. Inhibiting DAAO activity and slowing d-serine degradation by using DAAO inhibitors to enhance NMDAR function may be a new strategy for use in the treatment of schizophrenia [47]. The results of INTERACT, a 12-week, multicenter, randomized, double-blind, placebo-controlled, parallel-group phase II trial, showed that luvadaxistat (TAK-831), a highly selective and potent DAAO inhibitor, improved the cognitive function of patients with schizophrenia [47]. Sodium benzoate, another potent DAAO inhibitor, improved not only psychotic symptoms and cognitive impairment in schizophrenia but also cognitive function in early-stage Alzheimer disease and late-life depression [48,49,50,51]. DAAO inhibitors may be another promising therapeutic approach [52, 53] capable of overcoming the limitations of current antipsychotics. However, the mechanism of action of DAAO inhibitors remains unclear. Evidence suggested that it may be related to redox modulation instead of an indirect increase in the d-serine level [54].
d-Serine metabolism by d-amino acid oxidase (DAAO). l-Serine is converted into d-serine through isomerization reactions catalyzed by serine racemase (SR) [33, 34]. Thereafter, through oxidative deamination by DAAO [35, 36], d-serine is degraded into α-keto acids and ammonia; flavin adenine dinucleotide (FAD) is simultaneously reduced to dihydroflavine-adenine dinucleotide (FADH2), which is subsequently reoxidized to FAD, with hydrogen peroxide produced as a byproduct [36]
2 Evidence from Preclinical Studies
Inhibition of DAAO activity reversed schizophrenia-like behavior and prepulse inhibition in mutant mice with NR1 subunit deficits and mice treated with MK-801 [55, 56]. Mutant mice with DAAO deficiency exhibited superior recognition memory performance and elevated D-serine levels in the hippocampus as well as increased anxiety-like behaviors [57, 58].
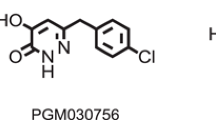
Numerous DAAO inhibitors, including 5-methylpyrazole-3-carbo-xylic acid (AS057278) [59], 6-chlorobenzo[d]isoxazol-3-ol (CBIO) [56, 60, 61], 4H-thieno[3,2-b] pyrrole-5-carboxylic acid (compound 8) [62], sodium benzoate [63], 4-hydroxy-6-{2-[4(trifluoromethyl)phenyl]ethyl}-pyridazin-3(2H)-one (TAK-831) [64] and 4-hydroxypyridazin-3(2H)-one (compound 30) [65] have been investigated.
Chronic administration of AS057278, a selective DAAO inhibitor, increased d-serine in the cortex and normalized PCP-induced hyperlocomotion in rats [59]. Sershen et al. [61] employed the PCP-treated mouse model to explore whether CBIO and sodium benzoate increase the d-serine level in the brain and inhibit PCP-induced locomotor activity or not. The results indicated that d-serine inhibited PCP-induced hyperactivity and suggested an interaction between sodium benzoate and d-serine with unknown mechanisms other than DAAO inhibition. Fradley et al. [66] showed that TAK-831 improved cognitive deficits and negative symptoms in an animal model of schizophrenia. Nagy et al. [65] investigated the effects of a novel DAAO inhibitor (compound 30) on cognitive function (measured by passive avoidance learning) and neuronal firing activity in rats. Their results revealed that low doses of DAAO inhibitor (compound 30) seemed to exhibit efficacy similar to that of high doses of d-serine, with fewer side effects. The results also revealed a relationship between the neural and behavioral action of DAAO inhibition.
3 Evidence from Clinical Trials
3.1 Sodium Benzoate
Clinical evidence supported that sodium benzoate improved not only psychotic symptoms and cognitive impairment in schizophrenia but also cognitive function in early-stage Alzheimer disease and late-life depression [48,49,50,51, 54, 67, 68]. The contents of those studies are briefly summarized in Table 1.
Lane et al. [48] conducted a 6-week, randomized, double-blind, placebo-controlled trial in which sodium benzoate (1 g/day) was administered as an adjuvant therapy to patients with chronic schizophrenia who had been stabilized with antipsychotics for at least 3 months. The results revealed that sodium benzoate improved both the positive and negative symptoms of schizophrenia and enhanced cognitive function in the domains of processing speed and visual memory. Lin et al. [50] conducted a 12-week, randomized, double-blind, placebo-controlled trial in which dual NMDAR enhancers, sarcosine and sodium benzoate, were applied to treat chronic schizophrenia. The results showed that patients treated with a combination of sarcosine and sodium benzoate exhibited greater cognitive improvement than did those treated with sarcosine alone or placebo.
In clinical practice, clozapine is used as the last-line antipsychotic for patients with schizophrenia previously observed to be refractory to standard treatments with at least two specific antipsychotics [1]. Previous studies have indicated that the efficacy of clozapine could not be augmented with NMDAR-enhancing agents [69,70,71]. This finding may be attributed to the fact that clozapine itself already acts as a potential NMDAR enhancer [72,73,74,75], thus attenuating the effectiveness of glycine, d-serine, and glycine transporter-1 (GlyT1) inhibitor. A 6-week, randomized, double-blind, placebo-controlled trial [54] investigated the efficacy of sodium benzoate as adjunctive therapy for clozapine-resistant schizophrenia. The enrolled patients were allocated into three treatment groups: sodium benzoate 1 g/day, sodium benzoate 2 g/day and placebo. The results were more promising than those of previous studies on clozapine augmentation with other NMDA-enhancing agents [70,71,72]; both doses of sodium benzoate improved the negative symptoms and benzoate 2 g/day improved positive symptoms. The serum DAAO levels of the patients in the 2 g/day sodium benzoate group decreased more compared with those of the patients in the placebo group. However, the blood levels of five amino acids (d-serine, l-serine, glycine, d-alanine and l-alanine) in each of the groups did not change significantly from baseline to the endpoint. Importantly, the changes of serum catalase (CAT), a vital antioxidant, were correlated with the improvement of overall symptoms and positive symptoms in the sodium benzoate groups [54].
Lin et al. [49] conducted a 24-week, randomized, double-blind, placebo-controlled trial which showed that sodium benzoate significantly improved cognitive function in patients with early-stage Alzheimer disease. Recently, sodium benzoate was also found to improve cognitive function in women (but not in men) with behavioral and psychological symptoms of dementia [67]. Lane et al. [68] performed the resting-state functional magnetic resonance imaging to analyze regional homogeneity and local functional connectivity in patients with mild cognitive impairment. The results showed that sodium benzoate was able to alter the brain activity; the alteration of brain activity was correlated with the change in cognitive function of the patients. In another study [51], patients with geriatric depression were treated with sodium benzoate, sertraline (a commonly used antidepressant) or placebo for 8 weeks; the results showed that compared with the placebo group, those treated with sodium benzoate (but not those treated with sertraline) had substantial improvements in cognitive function and perceived stress scores.
In contrast to other clinical trials for chronic, treatment-resistant, or clozapine-resistant schizophrenia [48, 50, 54], a 12-week, randomized, double-blind, placebo-controlled trial [76] that evaluated the efficacy of sodium benzoate (1000 mg/day) as an adjuvant treatment for early psychosis revealed that compared with placebo controls, add-on treatment of sodium benzoate did not produce better outcomes. The results were possibly influenced by recruiting patients who were younger (mean age of 21 years) with recent-onset disorder and a broader range of diagnoses in this study, including schizophrenia, schizophreniform disorder, affective psychosis, delusional disorder and other forms of psychosis not otherwise specified. The previous study reported the difference between bipolar disorder and schizophrenia on d-serine levels. Compared with the control subjects, patients with bipolar disorder had higher d-serine levels [77].
3.2 TAK-831
TAK-831is a highly selective DAAO inhibitor. Yoneyama et al. [64] investigated the brain distribution of TAK-831 in rats. The results showed remarkably different distribution between target (cerebellum) and reference (frontal cortex) regions. At a daily dose of 600 mg, TAK-831 achieved a target occupancy rate of over 90% [78] and was well tolerated with mild adverse events [79]. The results of the phase II trial released in March 2021 revealed that add-on luvadaxistat (TAK-831) improved not negative symptoms but cognitive function in patients with schizophrenia [47]. Further, there has been an ongoing randomized, double-blind, parallel, placebo-controlled phase II trial with a 12-month open-label extension to evaluate the efficacy of add-on luvadaxistat (TAK-831) in treating cognitive impairment in patients with schizophrenia [80].
4 Analysis of the Mechanism of Action of DAAO Inhibitors
The exact mechanism of action of DAAO inhibitors remains unclear [53]. Preclinical and clinical studies revealed that TAK-831 increased d-serine levels [66, 79], whereas sodium benzoate did not change d-serine levels [61, 63]. Instead, the correlation between the changes in the catalase and the improvements of overall symptoms and positive symptoms was found in patients treated with sodium benzoate [54]. Overall, the mechanism of action of DAAO inhibitors may still be related to the enhancement of NMDAR function [53]. Schizophrenia is a highly heterogeneous disease in which oxidative stress may play a central role in pathogenesis [81]. Accumulating evidence suggests that schizophrenia is associated with redox imbalance [81, 82]. Lower aconitase, nicotinamide adenine dinucleotide dehydrogenase (NADH), and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) levels were identified in patients with schizophrenia than in people without schizophrenia in postmortem studies [83]. Analyses of plasma and cerebrospinal fluid revealed that patients with schizophrenia had lower glutathione (GSH) levels and higher oxidized glutathione levels than people without schizophrenia [84, 85]. Higher levels of thiobarbituric acid–reactive substances (TBARS) and lower catalase (CAT) and superoxide dismutase (SOD) activity were observed in schizophrenia [86, 87]. Changes in GSH, SOD and CAT levels were associated with changes in clinical symptoms of schizophrenia, indicating that these redox-involved factors may have potential to be biomarkers of schizophrenia and may be helpful in monitoring disease progression [54, 86,87,88,89,90]. There is a reciprocal connection between NMDAR activity and redox modulation. Cysteine residues of NMDAR are involved in redox modulation [91], and NMDAR dysfunction may lead to decreased antioxidant capacity, resulting in oxidative stress which in turn causes downregulation of NMDARs [82, 92]. Both ketamine and phencyclidine decreased glutathione levels in rat models of schizophrenia [93, 94]. Deficiency of the NMDAR subunit GluN2A resulted in vulnerability to redox dysregulation and delayed the maturation of paravalbumin interneurons [95, 96] which is considered to be a key pathophysiological mechanism of schizophrenia [82, 97, 98].
4.1 Sodium Benzoate Enhances NMDAR Function Through its Antioxidant Properties
DAAO inhibitors, such as sodium benzoate, may enhance NMDAR function through antioxidant activity instead of by inhibiting DAAO. Evidence showed that sodium benzoate modulates antioxidant defense mechanisms in a dose-dependent manner [99,100,101,102,103]. El-Shennawy et al. [99] administered sodium benzoate to male rats at doses of 0, 1, 10, 50, 100, 250, 500 and 1000 mg/kg/day for 90 consecutive days. The results revealed that subchronic use of sodium benzoate was risky at both low and high doses, and the toxicity of it was dose dependent. Sodium benzoate impaired the reproductive system, resulting in decreased sperm count, sperm motility, testicular 17β-hydroxysteroid dehydrogenase (17β-HSD) and 17-ketosteroid reductases (17-KSR) activity; increased abnormal sperm and alteration of hormone levels. Overall, as the dose of sodium benzoate increased from 100 mg/kg/day, testicular nitric oxide (NO), malondialdehyde (MDA), xanthine oxidase (XO), tumor necrosis factor (TNF)-α, interleukin (IL)-6, p53 protein, and caspase-3 activity increased significantly; by contrast, levels of the antioxidant enzymes glutathione peroxidase (GPx), glutathione S-transferase (GST), CAT, SOD, GSH and total antioxidant capacity (TAC) decreased significantly. Olofinnade et al. [102] distributed 40 male rats into four groups: the control group and three groups that received sodium benzoate at doses of 125, 250 and 500 mg/kg/day, respectively, for 8 consecutive weeks. Consequently, the hematological effects of and oxidative stress induced by sodium benzoate were also dose dependent. Significant decrease in serum MDA levels and increase in TAC were found as the dose of sodium benzoate increased. In addition, a significant increase in serum SOD and decrease in serum TNF-α were found in the group that received sodium benzoate at 125 mg/kg/day. However, the caspase-3 levels and renal function of the sodium benzoate groups did not differ significantly from those of the control group. Khan et al. [104] distributed 25 male rats into five groups: the control group and four groups that received sodium benzoate at doses of 70, 200, 400 and 700 mg/kg/day, respectively, for 30 consecutive days. The activities of antioxidant enzymes SOD, CAT, GST and GPx in the liver gradually decreased in the groups receiving the daily doses of 200 mg/kg and higher. These changes were not observed in the group that received sodium benzoate at 70 mg/kg/day. The mitochondria are the primary sites of intracellular reactive oxygen species (ROS) production [105, 106]. Mitochondrial dysfunction causes excessive ROS production, resulting in oxidative stress. Protein DJ-1, with antioxidant properties, is involved in regulating the quality of and oxidative stress in mitochondria [107]. Xu et al. [103] observed that a single dose of sodium benzoate (i.e., 100 mg or 200 mg/kg) improved cognitive function, upregulated mitochondrial DJ-1 and the antiapoptotic factor Bcl-2 and reduced the levels of proapoptotic factors (e.g., cleaved caspase-3 and cleaved caspase-9) and ROS production in rats with intracranial hemorrhage. By contrast, with higher doses and prolonged use of sodium benzoate, the production of excessive levels of mitochondrial transcription factor A (mtTFA) and mitochondrial uncoupling protein 2 (UCP2), proteins associated with mitochondrial function, may lead to mitochondrial dysfunction [99].
5 Conclusions
An animal study showed that d-serine had poor ability to pass the blood–brain barrier (BBB) and higher doses were thus required [108]; administration of d-serine, particularly at high doses [109], increased the risk of nephrotoxicity in rats [110]. However, clinical trials reported nonsignificant increases in nephrotoxicity induced by high-dose (>60 mg/kg/day) d-serine administration [111,112,113]. Whether long-term administration of d-serine in high doses inflicts nephrotoxicity or peripheral nerve injury [114] in humans remains uncertain. Co-administration of DAAO inhibitors reduced the required d-serine dose and DAAO activity, thus attenuating the risks of side effects [56, 115]. d-Serine-induced nephrotoxicity was not reported in DAAO knockout rats [116]. Possibly, high-dose d-serine degraded by DAAO may increase the production of hydrogen peroxide [117] and reduce glutathione concentrations [118], leading to cell damage and oxidative stress. Antioxidant properties of sodium benzoate may also prevent oxidative stress which may be induced by high-dose d-serine. Collectively, DAAO inhibitors have the potential to serve as an effective treatment for schizophrenia. The efficacy and safety of TAK-831 and sodium benzoate are dose-dependent [66, 79, 102, 103]. In rat models, the toxicity of sodium benzoate on the reproductive system and liver and renal function were dose- and duration-dependent [99, 104, 119, 120]. No side effects have been observed in previous clinical trials [48,49,50,51, 54, 76], which may be due to the doses used being below the maximum dose recommended by the Food and Drug Administration [121]. In the future, researchers should conduct trials that involve various populations and test several dosages of DAAO inhibitors with longer study duration to further elucidate the clinical efficacy and safety of DAAO inhibitors as a potential treatment for schizophrenia and other neurocognitive disorders.
References
Correll CU, Howes OD. Treatment-resistant schizophrenia: definition, predictors, and therapy options. J Clin Psychiatry. 2021;82:5. https://doi.org/10.4088/JCP.MY20096AH1C.
Lewis DA, Lieberman JA. Catching up on schizophrenia: natural history and neurobiology. Neuron. 2000;28:325–34. https://doi.org/10.1016/s0896-6273(00)00111-2.
Green MF, Schooler NR, Kern RS, Frese FJ, Granberry W, Harvey PD, et al. Evaluation of functionally meaningful measures for clinical trials of cognition enhancement in schizophrenia. Am J Psychiatry. 2011;168:400–7. https://doi.org/10.1176/appi.ajp.2010.10030414.
Lin CH, Huang CL, Chang YC, Chen PW, Lin CY, Tsai GE, et al. Clinical symptoms, mainly negative symptoms, mediate the influence of neurocognition and social cognition on functional outcome of schizophrenia. Schizophr Res. 2013;146:231–7. https://doi.org/10.1016/j.schres.2013.02.009.
Iyo M, Tadokoro S, Kanahara N, Hashimoto T, Niitsu T, Watanabe H, et al. Optimal extent of dopamine D2 receptor occupancy by antipsychotics for treatment of dopamine supersensitivity psychosis and late-onset psychosis. J Clin Psychopharmacol. 2013;33:398–404. https://doi.org/10.1097/JCP.0b013e31828ea95c.
Stępnicki P, Kondej M, Kaczor AA. Current concepts and treatments of schizophrenia. Molecules. 2018;23:2087. https://doi.org/10.3390/molecules23082087.
Balu DT. The NMDA receptor and schizophrenia: from pathophysiology to treatment. Adv Pharmacol Sci. 2016;76:351–82. https://doi.org/10.1016/bs.apha.2016.01.006.
Coyle JT. NMDA receptor and schizophrenia: a brief history. Schizophr Bull. 2012;38:920–6. https://doi.org/10.1093/schbul/sbs076.
Kantrowitz JT, Javitt DC. N-methyl-d-aspartate (NMDA) receptor dysfunction or dysregulation: the final common pathway on the road to schizophrenia? Brain Res Bull. 2010;83:108–21. https://doi.org/10.1016/j.brainresbull.2010.04.006.
Lin CH, Lane HY. Early identification and intervention of schizophrenia: insight from hypotheses of glutamate dysfunction and oxidative stress. Front Psychiatry. 2019;10:93. https://doi.org/10.3389/fpsyt.2019.00093.
Verrall L, Burnet PW, Betts JF, Harrison PJ. The neurobiology of d-amino acid oxidase and its involvement in schizophrenia. Mol Psychiatry. 2010;15:122–37. https://doi.org/10.1038/mp.2009.99.
Coyle JT. Glutamate and schizophrenia: beyond the dopamine hypothesis. Cell Mol Neurobiol. 2006;26:365–84. https://doi.org/10.1007/s10571-006-9062-8.
Krystal JH, Karper LP, Seibyl JP, Freeman GK, Delaney R, Bremner JD, et al. Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans: psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatry. 1994;51:199–214. https://doi.org/10.1001/archpsyc.1994.03950030035004.
Mohn AR, Gainetdinov RR, Caron MG, Koller BH. Mice with reduced NMDA receptor expression display behaviors related to schizophrenia. Cell. 1999;98:427–36. https://doi.org/10.1016/s0092-8674(00)81972-8.
Ripke S, Neale BM, Corvin A, Walters JTR, Farh K-H, Holmans PA, et al. Psychosis Endophenotypes International, C. Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511:421–7. https://doi.org/10.1038/nature13595.
Trubetskoy V, Pardiñas AF, Qi T, Panagiotaropoulou G, Awasthi S, Bigdeli TB, et al. Mapping genomic loci implicates genes and synaptic biology in schizophrenia. Nature. 2022;604:502–8. https://doi.org/10.1038/s41586-022-04434-5.
Nakazawa K, Sapkota K. The origin of NMDA receptor hypofunction in schizophrenia. Pharmacol Ther. 2020;205: 107426. https://doi.org/10.1016/j.pharmthera.2019.107426.
Fuchs SA, Berger R, Klomp LWJ, de Koning TJ. d-Amino acids in the central nervous system in health and disease. Mol Genet Metab. 2005;85:168–80. https://doi.org/10.1016/j.ymgme.2005.03.003.
Price GW, Ahier RG, Middlemiss DN, Singh L, Tricklebank MD, Wong EH. In vivo labelling of the NMDA receptor channel complex by [3H]MK-801. Eur J Pharmacol. 1988;158:279–82. https://doi.org/10.1016/0014-2999(88)90080-5.
Bergeron R, Meyer TM, Coyle JT, Greene RW. Modulation of N-methyl-d-aspartate receptor function by glycine transport. Proc Natl Acad Sci USA. 1998;95:15730–4. https://doi.org/10.1073/pnas.95.26.15730.
Fossat P, Turpin FR, Sacchi S, Dulong J, Shi T, Rivet JM, et al. Glial D-serine gates NMDA receptors at excitatory synapses in prefrontal cortex. Cereb Cortex. 2012;22:595–606. https://doi.org/10.1093/cercor/bhr130.
Lane HY, Chang YC, Liu YC, Chiu CC, Tsai GE. Sarcosine or d-serine add-on treatment for acute exacerbation of schizophrenia: a randomized, double-blind, placebo-controlled study. Arch Gen Psychiatry. 2005;62:1196–204. https://doi.org/10.1001/archpsyc.62.11.1196.
Lane HY, Liu YC, Huang CL, Chang YC, Liau CH, Perng CH, et al. Sarcosine (N-methylglycine) treatment for acute schizophrenia: a randomized, double-blind study. Biol Psychiatry. 2008;63:9–12. https://doi.org/10.1016/j.biopsych.2007.04.038.
Lane HY, Lin CH, Huang YJ, Liao CH, Chang YC, Tsai GE. A randomized, double-blind, placebo-controlled comparison study of sarcosine (N-methylglycine) and d-serine add-on treatment for schizophrenia. Int J Neuropsychopharmacol. 2010;13:451–60. https://doi.org/10.1017/s1461145709990939.
Tsai G, Yang P, Chung LC, Lange N, Coyle JT. d-Serine added to antipsychotics for the treatment of schizophrenia. Biol Psychiatry. 1998;44:1081–9. https://doi.org/10.1016/s0006-3223(98)00279-0.
Heresco-Levy U, Javitt DC, Ebstein R, Vass A, Lichtenberg P, Bar G, et al. d-Serine efficacy as add-on pharmacotherapy to risperidone and olanzapine for treatment-refractory schizophrenia. Biol Psychiatry. 2005;57:577–85. https://doi.org/10.1016/j.biopsych.2004.12.037.
Krystal JH. Capitalizing on extrasynaptic glutamate neurotransmission to treat antipsychotic-resistant symptoms in schizophrenia. Biol Psychiatry. 2008;64:358–60. https://doi.org/10.1016/j.biopsych.2008.06.011.
Goh KK, Wu TH, Chen CH, Lu ML. Efficacy of N-methyl-d-aspartate receptor modulator augmentation in schizophrenia: a meta-analysis of randomised, placebo-controlled trials. J Psychopharmacol (Oxford, England). 2021;35:236–52. https://doi.org/10.1177/0269881120965937.
Guercio GD, Panizzutti R. Potential and challenges for the clinical use of d-serine as a cognitive enhancer. Front Psychiatry. 2018;9:14. https://doi.org/10.3389/fpsyt.2018.00014.
Gustafson EC, Stevens ER, Wolosker H, Miller RF. Endogenous d-serine contributes to NMDA-receptor-mediated light-evoked responses in the vertebrate retina. J Neurophysiol. 2007;98:122–30. https://doi.org/10.1152/jn.00057.2006.
Kartvelishvily E, Shleper M, Balan L, Dumin E, Wolosker H. Neuron-derived d-serine release provides a novel means to activate N-methyl-d-aspartate receptors. J Biol Chem. 2006;281:14151–62. https://doi.org/10.1074/jbc.M512927200.
Levin R, Dor-Abarbanel AE, Edelman S, Durrant AR, Hashimoto K, Javitt DC, et al. Behavioral and cognitive effects of the N-methyl-d-aspartate receptor co-agonist d-serine in healthy humans: initial findings. J Psychiatr Res. 2015;61:188–95. https://doi.org/10.1016/j.jpsychires.2014.12.007.
Foltyn VN, Bendikov I, De Miranda J, Panizzutti R, Dumin E, Shleper M, et al. Serine racemase modulates intracellular d-serine levels through an alpha, beta-elimination activity. J Biol Chem. 2005;280:1754–63. https://doi.org/10.1074/jbc.M405726200.
Baumgart F, Rodríguez-Crespo I. d-Amino acids in the brain: the biochemistry of brain serine racemase. FEBS J. 2008;275:3538–45. https://doi.org/10.1111/j.1742-4658.2008.06517.x.
Wolosker H. Serine racemase and the serine shuttle between neurons and astrocytes. Biochem Biophys Acta. 2011;1814:1558–66. https://doi.org/10.1016/j.bbapap.2011.01.001.
Pollegioni L, Piubelli L, Sacchi S, Pilone MS, Molla G. Physiological functions of d-amino acid oxidases: from yeast to humans. Cell Mol Life Sci. 2007;64:1373–94. https://doi.org/10.1007/s00018-007-6558-4.
Matsuo H, Kanai Y, Tokunaga M, Nakata T, Chairoungdua A, Ishimine H, et al. High affinity d- and l-serine transporter Asc-1: cloning and dendritic localization in the rat cerebral and cerebellar cortices. Neurosci Lett. 2004;358:123–6. https://doi.org/10.1016/j.neulet.2004.01.014.
Rutter AR, Fradley RL, Garrett EM, Chapman KL, Lawrence JM, Rosahl TW, et al. Evidence from gene knockout studies implicates Asc-1 as the primary transporter mediating d-serine reuptake in the mouse CNS. Eur J Neurosci. 2007;25:1757–66. https://doi.org/10.1111/j.1460-9568.2007.05446.x.
Calcia MA, Madeira C, Alheira FV, Silva TC, Tannos FM, Vargas-Lopes C, et al. Plasma levels of d-serine in Brazilian individuals with schizophrenia. Schizophr Res. 2012;142:83–7. https://doi.org/10.1016/j.schres.2012.09.014.
Hashimoto K, Fukushima T, Shimizu E, Komatsu N, Watanabe H, Shinoda N, et al. Decreased serum levels of d-serine in patients with schizophrenia: evidence in support of the N-methyl-d-aspartate receptor hypofunction hypothesis of schizophrenia. Arch Gen Psychiatry. 2003;60:572–6. https://doi.org/10.1001/archpsyc.60.6.572.
Bendikov I, Nadri C, Amar S, Panizzutti R, De Miranda J, Wolosker H, et al. A CSF and postmortem brain study of d-serine metabolic parameters in schizophrenia. Schizophr Res. 2007;90:41–51. https://doi.org/10.1016/j.schres.2006.10.010.
Burnet PWJ, Eastwood SL, Bristow GC, Godlewska BR, Sikka P, Walker M, et al. d-Amino acid oxidase activity and expression are increased in schizophrenia. Mol Psychiatry. 2008;13:658–60. https://doi.org/10.1038/mp.2008.47.
Madeira C, Freitas ME, Vargas-Lopes C, Wolosker H, Panizzutti R. Increased brain d-amino acid oxidase (DAAO) activity in schizophrenia. Schizophr Res. 2008;101:76–83. https://doi.org/10.1016/j.schres.2008.02.002.
Ono K, Shishido Y, Park HK, Kawazoe T, Iwana S, Chung SP, et al. Potential pathophysiological role of d-amino acid oxidase in schizophrenia: immunohistochemical and in situ hybridization study of the expression in human and rat brain. J Neural Transm (Vienna). 2009;116:1335–47. https://doi.org/10.1007/s00702-009-0289-7.
Sacchi S, Rosini E, Pollegioni L, Molla G. d-Amino acid oxidase inhibitors as a novel class of drugs for schizophrenia therapy. Curr Pharm Des. 2013;19:2499–511. https://doi.org/10.2174/1381612811319140002.
Verrall L, Walker M, Rawlings N, Benzel I, Kew JNC, Harrison PJ, et al. d-Amino acid oxidase and serine racemase in human brain: normal distribution and altered expression in schizophrenia. Eur J Neurosci. 2007;26:1657–69. https://doi.org/10.1111/j.1460-9568.2007.05769.x.
Neurocrine Biosciences, Inc. Neurocrine biosciences announces top-line results from phase II INTERACT study evaluating luvadaxistat (NBI-1065844) for the treatment of negative symptoms and cognitive impairment associated with schizophrenia (CIAS). [Internet]. Neurocrine; 2021 [cited 2022 Aug 27]. Available from: https://www.prnewswire.com/news-releases/neurocrine-biosciences-announces-top-line-results-from-phase-ii-interact-study-evaluating-luvadaxistat-nbi-1065844-for-the-treatment-of-negative-symptoms-and-cognitive-impairment-associated-with-schizophrenia-cias-301238086.html.
Lane HY, Lin CH, Green MF, Hellemann G, Huang CC, Chen PW, et al. Add-on treatment of benzoate for schizophrenia: a randomized, double-blind, placebo-controlled trial of d-amino acid oxidase inhibitor. JAMA Psychiat. 2013;70:1267–75. https://doi.org/10.1001/jamapsychiatry.2013.2159.
Lin CH, Chen PK, Chang YC, Chuo LJ, Chen YS, Tsai GE, et al. Benzoate, a d-amino acid oxidase inhibitor, for the treatment of early-phase Alzheimer disease: a randomized, double-blind, placebo-controlled trial. Biol Psychiatry. 2014;75:678–85. https://doi.org/10.1016/j.biopsych.2013.08.010.
Lin CY, Liang SY, Chang YC, Ting SY, Kao CL, Wu YH, et al. Adjunctive sarcosine plus benzoate improved cognitive function in chronic schizophrenia patients with constant clinical symptoms: a randomised, double-blind, placebo-controlled trial. World J Biol Psychiatry. 2017;18:357–68. https://doi.org/10.3109/15622975.2015.1117654.
Lin C-H, Wang S-H, Lane H-Y. Effects of sodium benzoate, a d-amino acid oxidase inhibitor, on perceived stress and cognitive function among patients with late-life depression: a randomized, double-blind, sertraline- and placebo-controlled trial. Int J Neuropsychopharmacol. 2022;25:545–55. https://doi.org/10.1093/ijnp/pyac006.
Lin CH, Lane HY, Tsai GE. Glutamate signaling in the pathophysiology and therapy of schizophrenia. Pharmacol Biochem Behav. 2012;100:665–77. https://doi.org/10.1016/j.pbb.2011.03.023.
Harrison PJ. d-Amino acid oxidase inhibition: a new glutamate twist for clozapine augmentation in schizophrenia? Biol Psychiatry. 2018;84:396–8. https://doi.org/10.1016/j.biopsych.2018.06.001.
Lin CH, Lin CH, Chang YC, Huang YJ, Chen PW, Yang HT, et al. Sodium benzoate, a d-amino acid oxidase inhibitor, added to clozapine for the treatment of schizophrenia: a randomized, double-blind, placebo-controlled trial. Biol Psychiatry. 2018;84:422–32. https://doi.org/10.1016/j.biopsych.2017.12.006.
Labrie V, Wang W, Barger SW, Baker GB, Roder JC. Genetic loss of d-amino acid oxidase activity reverses schizophrenia-like phenotypes in mice. Genes Brain Behav. 2010;9:11–25. https://doi.org/10.1111/j.1601-183X.2009.00529.x.
Hashimoto K, Fujita Y, Horio M, Kunitachi S, Iyo M, Ferraris D, et al. Co-administration of a d-amino acid oxidase inhibitor potentiates the efficacy of d-serine in attenuating prepulse inhibition deficits after administration of dizocilpine. Biol Psychiatry. 2009;65:1103–6. https://doi.org/10.1016/j.biopsych.2009.01.002.
Labrie V, Duffy S, Wang W, Barger SW, Baker GB, Roder JC. Genetic inactivation of d-amino acid oxidase enhances extinction and reversal learning in mice. Learn Mem. 2009;16:28–37. https://doi.org/10.1101/lm.1112209.
Pritchett D, Hasan S, Tam SK, Engle SJ, Brandon NJ, Sharp T, et al. d-Amino acid oxidase knockout (Dao(−/−) ) mice show enhanced short-term memory performance and heightened anxiety, but no sleep or circadian rhythm disruption. Eur J Neurosci. 2015;41:1167–79. https://doi.org/10.1111/ejn.12880.
Adage T, Trillat AC, Quattropani A, Perrin D, Cavarec L, Shaw J, et al. In vitro and in vivo pharmacological profile of AS057278, a selective d-amino acid oxidase inhibitor with potential anti-psychotic properties. Eur Neuropsychopharmacol. 2008;18:200–14. https://doi.org/10.1016/j.euroneuro.2007.06.006.
Ferraris D, Duvall B, Ko YS, Thomas AG, Rojas C, Majer P, et al. Synthesis and biological evaluation of d-amino acid oxidase inhibitors. J Med Chem. 2008;51:3357–9. https://doi.org/10.1021/jm800200u.
Sershen H, Hashim A, Dunlop DS, Suckow RF, Cooper TB, Javitt DC. Modulating NMDA receptor function with d-amino acid oxidase inhibitors: understanding functional activity in PCP-treated mouse model. Neurochem Res. 2016;41:398–408. https://doi.org/10.1007/s11064-016-1838-8.
Smith SM, Uslaner JM, Yao L, Mullins CM, Surles NO, Huszar SL, et al. The behavioral and neurochemical effects of a novel d-amino acid oxidase inhibitor compound 8 [4H-thieno [3,2-b]pyrrole-5-carboxylic acid] and d-serine. J Pharmacol Exp Ther. 2009;328:921–30. https://doi.org/10.1124/jpet.108.147884.
Matsuura A, Fujita Y, Iyo M, Hashimoto K. Effects of sodium benzoate on pre-pulse inhibition deficits and hyperlocomotion in mice after administration of phencyclidine. Acta Neuropsychiatrica. 2015;27:159–67. https://doi.org/10.1017/neu.2015.1.
Yoneyama T, Sato S, Sykes A, Fradley R, Stafford S, Bechar S, et al. Mechanistic multilayer quantitative model for nonlinear pharmacokinetics, target occupancy and pharmacodynamics (PK/TO/PD) relationship of d-amino acid oxidase inhibitor, TAK-831 in mice. Pharm Res. 2020;37:164. https://doi.org/10.1007/s11095-020-02893-x.
Nagy LV, Bali ZK, Kapus G, Pelsőczi P, Farkas B, Lendvai B, et al. Converging evidence on d-amino acid oxidase-dependent enhancement of hippocampal firing activity and passive avoidance learning in rats. Int J Neuropsychopharmacol. 2021;24:434–45. https://doi.org/10.1093/ijnp/pyaa095.
Fradley R, Goetghebeur P, Miller D, Burley R, Serrats J. S22 Pre-clinical assessment of Tak-831, a selective d-amino acid oxidase inhibitor, in animal models of schizophrenia. Schizophr Bull. 2019;45:S313–4. https://doi.org/10.1093/schbul/sbz020.567.
Lin CH, Chen PK, Wang SH, Lane HY. Effect of sodium benzoate on cognitive function among patients with behavioral and psychological symptoms of dementia: secondary analysis of a randomized clinical trial. JAMA Netw Open. 2021;4: e216156. https://doi.org/10.1001/jamanetworkopen.2021.6156.
Lane HY, Tu CH, Lin WC, Lin CH. Brain activity of benzoate, a d-amino acid oxidase inhibitor, in patients with mild cognitive impairment in a randomized, double-blind, placebo controlled clinical trial. Int J Neuropsychopharmacol. 2021;24:392–9. https://doi.org/10.1093/ijnp/pyab001.
Evins AE, Fitzgerald SM, Wine L, Rosselli R, Goff DC. Placebo-controlled trial of glycine added to clozapine in schizophrenia. Am J Psychiatry. 2000;157:826–8. https://doi.org/10.1176/appi.ajp.157.5.826.
Tsai GE, Yang P, Chung LC, Tsai IC, Tsai CW, Coyle JT. d-Serine added to clozapine for the treatment of schizophrenia. Am J Psychiatry. 1999;156:1822–5. https://doi.org/10.1176/ajp.156.11.1822.
Lane HY, Huang CL, Wu PL, Liu YC, Chang YC, Lin PY, et al. Glycine transporter I inhibitor, N-methylglycine (sarcosine), added to clozapine for the treatment of schizophrenia. Biol Psychiatry. 2006;60:645–9. https://doi.org/10.1016/j.biopsych.2006.04.005.
Evins AE, Amico ET, Shih V, Goff DC. Clozapine treatment increases serum glutamate and aspartate compared to conventional neuroleptics. J Neural Transm (Vienna). 1997;104:761–6. https://doi.org/10.1007/bf01291892.
Schwieler L, Linderholm KR, Nilsson-Todd LK, Erhardt S, Engberg G. Clozapine interacts with the glycine site of the NMDA receptor: electrophysiological studies of dopamine neurons in the rat ventral tegmental area. Life Sci. 2008;83:170–5. https://doi.org/10.1016/j.lfs.2008.05.014.
Kubota T, Jibiki I, Enokido F, Nakagawa H, Watanabe K. Effects of MK-801 on clozapine-induced potentiation of excitatory synaptic responses in the perforant path-dentate gyrus pathway in chronically prepared rabbits. Eur J Pharmacol. 2000;395:37–42. https://doi.org/10.1016/s0014-2999(00)00150-3.
Yamamori H, Hashimoto R, Fujita Y, Numata S, Yasuda Y, Fujimoto M, et al. Changes in plasma d-serine, l-serine, and glycine levels in treatment-resistant schizophrenia before and after clozapine treatment. Neurosci Lett. 2014;582:93–8. https://doi.org/10.1016/j.neulet.2014.08.052.
Scott JG, Baker A, Lim C, Foley S, Dark F, Gordon A, et al. Effect of sodium benzoate vs placebo among individuals with early psychosis: a randomized clinical trial. JAMA Netw Open. 2020. https://doi.org/10.1001/jamanetworkopen.2020.24335.
Hashimoto K. Serine enantiomers as diagnostic biomarkers for schizophrenia and bipolar disorder. Eur Arch Psychiatry Clin Neurosci. 2016;266:83–5. https://doi.org/10.1007/s00406-015-0602-4.
Berkhout J, Post TM, Xu L, Zhang L, Wendland J, Faessel H, et al. Application of population PK/PD modeling and simulation to inform the design of a dose-finding study in patients with schizophrenia. Population Approach Group in Europe. 2019.
Wang H, Norton J, Xu L, DeMartinis N, Sen R, Shah A, et al. Results of a randomized double-blind study evaluating luvadaxistat in adults with Friedreich ataxia. Ann Clin Transl Neurol. 2021;8:1343–52. https://doi.org/10.1002/acn3.51373.
Neurocrine medical information call center. Study to evaluate the efficacy, safety, and tolerability of luvadaxistat in subjects with cognitive impairment associated with schizophrenia (ERUDITE). [Internet]. ClinicalTrials.Gov; 2022[cited 2022 Aug 27]. Available from: https://clinicaltrials.gov/ct2/show/NCT05182476.
Ermakov EA, Dmitrieva EM, Parshukova DA, Kazantseva DV, Vasilieva AR, Smirnova LP. Oxidative stress-related mechanisms in schizophrenia pathogenesis and new treatment perspectives. Oxid Med Cell Longev. 2021. https://doi.org/10.1155/2021/8881770.
Steullet P, Cabungcal JH, Monin A, Dwir D, O’Donnell P, Cuenod M, et al. Redox dysregulation, neuroinflammation, and NMDA receptor hypofunction: a “central hub” in schizophrenia pathophysiology? Schizophr Res. 2016;176:41–51. https://doi.org/10.1016/j.schres.2014.06.021.
Martins-de-Souza D, Harris LW, Guest PC, Bahn S. The role of energy metabolism dysfunction and oxidative stress in schizophrenia revealed by proteomics. Antioxid Redox Signal. 2011;15:2067–79. https://doi.org/10.1089/ars.2010.3459.
Raffa M, Atig F, Mhalla A, Kerkeni A, Mechri A. Decreased glutathione levels and impaired antioxidant enzyme activities in drug-naive first-episode schizophrenic patients. BMC Psychiatry. 2011;11:124. https://doi.org/10.1186/1471-244X-11-124.
Do KQ, Cabungcal JH, Frank A, Steullet P, Cuenod M. Redox dysregulation, neurodevelopment, and schizophrenia. Curr Opin Neurobiol. 2009;19:220–30. https://doi.org/10.1016/j.conb.2009.05.001.
Carvalho AF, Solmi M, Sanches M, Machado MO, Stubbs B, Ajnakina O, et al. Evidence-based umbrella review of 162 peripheral biomarkers for major mental disorders. Transl Psychiatry. 2020;10:152. https://doi.org/10.1038/s41398-020-0835-5.
Flatow J, Buckley P, Miller BJ. Meta-analysis of oxidative stress in schizophrenia. Biol Psychiatry. 2013;74:400–9. https://doi.org/10.1016/j.biopsych.2013.03.018.
Nucifora LG, Tanaka T, Hayes LN, Kim M, Lee BJ, Matsuda T, et al. Reduction of plasma glutathione in psychosis associated with schizophrenia and bipolar disorder in translational psychiatry. Transl Psychiatry. 2017;7: e1215. https://doi.org/10.1038/tp.2017.178.
Đorđević VV, Lazarević D, Ćosić V, Knežević M, Đorđević VB. Age-related changes of superoxide dismutase activity in patients with schizophrenia. Vojnosanit Pregl. 2017;74:31–7. https://doi.org/10.2298/VSP141202142D.
Huo L, Lu X, Wu F, Chang C, Ning Y, Zhang XY. Elevated activity of superoxide dismutase in male late-life schizophrenia and its correlation with clinical symptoms and cognitive deficits. BMC Psychiatry. 2021;21:606. https://doi.org/10.1186/s12888-021-03604-5.
Choi YB, Lipton SA. Redox modulation of the NMDA receptor. Cell Mol Life Sci CMLS. 2000;57:1535–41. https://doi.org/10.1007/pl00000638.
Hardingham GE, Bading H. Synaptic versus extrasynaptic NMDA receptor signalling: implications for neurodegenerative disorders. Nat Rev Neurosci. 2010;11:682–96. https://doi.org/10.1038/nrn2911.
Radonjić NV, Knezević ID, Vilimanovich U, Kravić-Stevović T, Marina LV, Nikolić T, et al. Decreased glutathione levels and altered antioxidant defense in an animal model of schizophrenia: long-term effects of perinatal phencyclidine administration. Neuropharmacology. 2010;58:739–45. https://doi.org/10.1016/j.neuropharm.2009.12.009.
Sampaio L, Cysne Filho F, de Almeida JC, Diniz D, Patrocínio C, de Sousa C, et al. Advantages of the alpha-lipoic acid association with chlorpromazine in a model of schizophrenia induced by ketamine in rats: behavioral and oxidative stress evidences. Neuroscience. 2018;373:72–81. https://doi.org/10.1016/j.neuroscience.2018.01.008.
Steullet P, Cabungcal JH, Coyle J, Didriksen M, Gill K, Grace AA, et al. Oxidative stress-driven parvalbumin interneuron impairment as a common mechanism in models of schizophrenia. Mol Psychiatry. 2017;22:936–43. https://doi.org/10.1038/mp.2017.47.
Cardis R, Cabungcal JH, Dwir D, Do KQ, Steullet P. A lack of GluN2A-containing NMDA receptors confers a vulnerability to redox dysregulation: consequences on parvalbumin interneurons, and their perineuronal nets. Neurobiol Dis. 2018;109(Pt A):64–75. https://doi.org/10.1016/j.nbd.2017.10.006.
Hardingham GE, Do KQ. Linking early-life NMDAR hypofunction and oxidative stress in schizophrenia pathogenesis. Nat Rev Neurosci. 2016;17:125–34. https://doi.org/10.1038/nrn.2015.19.
Bókkon I, Antal I. Schizophrenia: redox regulation and volume neurotransmission. Curr Neuropharmacol. 2011;9:289–300. https://doi.org/10.2174/157015911795596504.
El-Shennawy L, Kamel M, Khalaf A, Yousef MI. Dose-dependent reproductive toxicity of sodium benzoate in male rats: inflammation, oxidative stress and apoptosis. Reprod Toxicol (Elmsford, NY). 2020;98:92–8. https://doi.org/10.1016/j.reprotox.2020.08.014.
Yetuk G, Pandir D, Bas H. Protective role of catechin and quercetin in sodium benzoate-induced lipid peroxidation and the antioxidant system in human erythrocytes in vitro. Sci World J. 2014. https://doi.org/10.1155/2014/874824.
Khan IS, Ali MN, Hamid R, Ganie SA. Genotoxic effect of two commonly used food dyes metanil yellow and carmoisine using Allium cepa L. as indicator. Toxicol Rep. 2020;7:370–5. https://doi.org/10.1016/j.toxrep.2020.02.009.
Olofinnade AT, Onaolapo AY, Onaolapo OJ, Olowe OA. The potential toxicity of food-added sodium benzoate in mice is concentration-dependent. Toxicol Res. 2021;10:561–9. https://doi.org/10.1093/toxres/tfab024.
Xu W, Li T, Gao L, Lenahan C, Zheng J, Yan J, et al. Sodium benzoate attenuates secondary brain injury by inhibiting neuronal apoptosis and reducing mitochondria-mediated oxidative stress in a rat model of intracerebral hemorrhage: possible involvement of DJ-1/Akt/IKK/NFκB pathway. Front Mol Neurosci. 2019;12:105. https://doi.org/10.3389/fnmol.2019.00105.
Khan IS, Dar KB, Ganie SA, Ali MN. Toxicological impact of sodium benzoate on inflammatory cytokines, oxidative stress and biochemical markers in male Wistar rats. Drug Chem Toxicol. 2022;45:1345–54. https://doi.org/10.1080/01480545.2020.1825472.
Dias V, Junn E, Mouradian MM. The role of oxidative stress in Parkinson’s disease. J Parkinsons Dis. 2013;3:461–91. https://doi.org/10.3233/JPD-130230.
Tirichen H, Yaigoub H, Xu W, Wu C, Li R, Li Y. Mitochondrial reactive oxygen species and their contribution in chronic kidney disease progression through oxidative stress. Front Physiol. 2021;12: 627837. https://doi.org/10.3389/fphys.2021.627837.
Dolgacheva LP, Berezhnov AV, Fedotova EI, Zinchenko VP, Abramov AY. Role of DJ-1 in the mechanism of pathogenesis of Parkinson’s disease. J Bioenerg Biomembr. 2019;51:175–88. https://doi.org/10.1007/s10863-019-09798-4.
Takahashi K, Hayashi F, Nishikawa T. In vivo evidence for the link between l- and d-serine metabolism in rat cerebral cortex. J Neurochem. 1997;69:1286–90. https://doi.org/10.1046/j.1471-4159.1997.69031286.x.
Hasegawa H, Masuda N, Natori H, Shinohara Y, Ichida K. Pharmacokinetics and toxicokinetics of d-serine in rats. J Pharm Biomed Anal. 2019;162:264–71. https://doi.org/10.1016/j.jpba.2018.09.026.
Carone FA, Ganote CE. d-Serine nephrotoxicity. The nature of proteinuria, glucosuria, and aminoaciduria in acute tubular necrosis. Arch Pathol. 1975;99:658–62.
Meftah A, Hasegawa H, Kantrowitz JT. d-Serine: a cross species review of safety. Front Psychiatry. 2021;12: 726365. https://doi.org/10.3389/fpsyt.2021.726365.
Kantrowitz JT, Epstein ML, Lee M, Lehrfeld N, Nolan KA, Shope C, et al. Improvement in mismatch negativity generation during d-serine treatment in schizophrenia: correlation with symptoms. Schizophr Res. 2018;191:70–9. https://doi.org/10.1016/j.schres.2017.02.027.
Ermilov M, Gelfin E, Levin R, Lichtenberg P, Hashimoto K, Javitt DC, et al. A pilot double-blind comparison of d-serine and high-dose olanzapine in treatment-resistant patients with schizophrenia. Schizophr Res. 2013;150:604–5. https://doi.org/10.1016/j.schres.2013.09.018.
Choi SR, Roh DH, Yoon SY, Choi HS, Kang SY, Han HJ, et al. Astrocyte d-serine modulates the activation of neuronal NOS leading to the development of mechanical allodynia in peripheral neuropathy. Mol Pain. 2019;15:1744806919843046. https://doi.org/10.1177/1744806919843046.
Williams RE, Lock EA. Sodium benzoate attenuates d-serine induced nephrotoxicity in the rat. Toxicology. 2005;207:35–48. https://doi.org/10.1016/j.tox.2004.08.008.
Maekawa M, Okamura T, Kasai N, Hori Y, Summer KH, Konno R. d-Amino-acid oxidase is involved in d-serine-induced nephrotoxicity. Chem Res Toxicol. 2005;18:1678–82. https://doi.org/10.1021/tx0500326.
Park HK, Shishido Y, Ichise-Shishido S, Kawazoe T, Ono K, Iwana S, et al. Potential role for astroglial d-amino acid oxidase in extracellular d-serine metabolism and cytotoxicity. J Biochem. 2006;139:295–304. https://doi.org/10.1093/jb/mvj036.
Krug AW, Völker K, Dantzler WH, Silbernagl S. Why is d-serine nephrotoxic and alpha-aminoisobutyric acid protective? Am J Physiol Renal Physiol. 2007;293:F382–90. https://doi.org/10.1152/ajprenal.00441.2006.
Mahmoud GS, Sayed SA, Abdelmawla SN, Amer MA. Positive effects of systemic sodium benzoate and olanzapine treatment on activities of daily life, spatial learning and working memory in ketamine-induced rat model of schizophrenia. Int J Physiol Pathophysiol Pharmacol. 2019;11:21–30.
Zeghib K, Boutlelis DA. Food additive (sodium benzoate)-induced damage on renal function and glomerular cells in rats; modulating effect of aqueous extract of Atriplex halimus L. Iran J Pharm Res IJPR. 2021;20:296–306. https://doi.org/10.22037/ijpr.2020.111634.13272.
Chesapeake biological laboratories, inc. Highlights of prescribing information. [Internet]. U.S. Food and Drug Administration.2011 [cited 2022 Aug 27]. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/020645s008lbl.pdf.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This work was supported by National Health Research Institutes, Taiwan (NHRI-EX111-11133NI), Ministry of Science and Technology, Taiwan (109-2314-B-039-039-MY3; MOST 111-2622-B-039-002) and China Medical University Hospital, Taiwan (DMR-111-243, DMR-HHC-111-9).
Conflict of interest
The authors declare no conflict of interest. The sponsors were not involved in the conceptualization of the study; the collection and interpretation of the data; the writing of the article or the decision to submit the article for publication.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Author contributions
Conceptualization, H-YL and C-HL; writing—original draft preparation, C-YK; writing—review and editing, H-YL and C-HL. All authors have read and agreed to the published version of the manuscript and to be accountable for the work.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kuo, CY., Lin, CH. & Lane, HY. Targeting d-Amino Acid Oxidase (DAAO) for the Treatment of Schizophrenia: Rationale and Current Status of Research. CNS Drugs 36, 1143–1153 (2022). https://doi.org/10.1007/s40263-022-00959-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-022-00959-5