Abstract
d-Amino acid oxidase (DAO) is a peroxisomal flavoenzyme that catalyzes oxidative deamination of a wide range of d-amino acids. Among the possible substrates of DAO in vivo, d-serine is proposed to be a neuromodulator of the N-methyl-d-aspartate (NMDA) type glutamate receptor. The gene for DAO was reported to be associated with schizophrenia. Since DAO is expected to be one of the key enzymes in the regulation of NMDA neurotransmission, the modulation of the enzyme activity is expected to be therapeutical for neuronal disorders. In search of the pathophysiological role of DAO, we analyzed the distribution of DAO mRNA and protein in the rat and human brain. In rat, the distribution of DAO mRNA was newly detected in choroid plexus (CP) epithelial cells in addition to glial cells of pons, medulla oblongata, and especially Bergmann glia of cerebellum. Moreover, to investigate how DAO expression level is altered in schizophrenia, we performed immunohistochemistry in the human brain. In agreement with the results in the rat brain, the immunoreactivity for DAO was detected in glial cells of rhombencephalon and in CP. Furthermore, higher level of DAO expression was observed in schizophrenic CP epithelial cells than that in non-schizophrenic cases. These results suggest that an increase in DAO expression in parts of the brain is involved in aberrant d-amino acid metabolism. In particular, gene expression of DAO in CP suggests that DAO may regulate d-amino acid concentration by modulating the cerebrospinal fluid and may be regarded as a potential therapeutic target for schizophrenia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
d-Amino acid oxidase (DAO; EC 1.4.3.3) is a flavoenzyme that catalyzes the oxidation of d-amino acids to the corresponding imino acids and hydrogen peroxide (H2O2) (Krebs 1935). The imino acid is nonenzymatically hydrolyzed to α-keto acid and ammonia (for reviews, Kawazoe et al. 2007). In mammals, DAO is found at the highest concentrations in the kidney, liver, and brain.
Previously, we determined the primary structures of the porcine, human, rabbit, and mouse kidney DAO mRNAs (Fukui et al. 1987; Momoi et al. 1988, 1990; Tada et al. 1990). We also carried out a series of molecular biological studies on the structure–function relationship of DAO for the porcine (Watanabe et al. 1988; Pollegioni et al. 1994) and human enzymes (Raibekas et al. 2000; Kawazoe et al. 2006, 2007). Recently, we reported the gene expression of DAO in type-1 astrocytes from rat cerebellum and cerebral cortex (Urai et al. 2002) and also demonstrated that extracellular d-serine can gain access to intracellular DAO, being metabolized to produce H2O2 (Park et al. 2006). Moreover, we showed inhibitory effect of the antipsychotic drug and its derivative, risperidone and chlorpromazine oligomer, on human DAO (Abou El-Magd et al. 2009; Iwana et al. 2008). These data indicated the involvement of DAO activity in d-serine metabolism and also suggested that risperidone and chlorpromazine oligomer could act as an active substance to inhibit DAO, which might contribute to the therapeutic effects of these drugs.
d-Serine is present in the mammalian brain (Hashimoto et al. 1992) and is an endogenous modulator of the glycine site of NMDA receptor (Schell et al. 1995; Mothet et al. 2000). Hypofunction of the NMDA receptor has been implicated in the pathology of schizophrenia. Mice expressing only 5% of the normal level of the NR1 subunit of the NMDA receptor exhibited behavioral abnormalities related to schizophrenia, including increased motor activity, stereotype, and deficits in social and sexual interaction (Mohn et al. 1999). It is notable that novel human gene G72 was recently implicated in schizophrenia, and the gene G72 product has been shown to bind with DAO and to enhance its catalytic activity. DAO is itself associated with schizophrenia, and the combination of the G72/DAO genotypes has a synergistic effect on disease risk (Chumakov et al. 2002).
d-Amino acid oxidase has been shown to reduce NMDA receptor-mediated neurotransmission (Mothet et al. 2000). From this result, it has been suggested that increased DAO activity in schizophrenia might contribute, via d-serine decrements, to NMDA receptor dysfunction (Madeira et al. 2008). Recent studies provide some support for this notion. Co-administration of d-serine with antipsychotics can ameliorate some symptoms of the schizophrenia (Tsai et al. 1998). Moreover, d-serine levels were lower in cerebrospinal fluid (CSF) samples of schizophrenic patients when compared to controls (Hashimoto et al. 2005; Yamada et al. 2005; Bendikov et al. 2007).
In search of the pathophysiological role of DAO in the schizophrenic brain, we analyzed distribution of DAO mRNA and protein in almost all brain regions. Especially, we considered that it is possible for DAO to be expressed in choroid plexus (CP) producing CSF, based on the reports that d-serine levels were decreased in CSF samples of schizophrenic patients. In the present study, we show that DAO was expressed in CP and its expression was altered in schizophrenic CP by immunohistochemical analysis. These results suggest that DAO is involved in d-amino acid metabolism in parts of the brain and altered DAO expression is relevant to the pathophysiology of schizophrenia.
Materials and methods
Animals and preparation of tissue
All procedures used throughout this study were conducted according to the Japan guidelines for animal care and were approved by the Animal Care and Use Committee in the University of Tokushima. All efforts were made to minimize the number of animals used in the study. In total, seven male Sprague–Dawley rats (CLEA Japan, Inc., Tokyo, Japan; 10-weeks old) were used. Three rats were used to extract RNA for analysis of DAO mRNA in the brain. For histological analysis, four rats were deeply anesthetized with dimethyl ether, and then were fixed initially by perfusion via the heart with 4% paraformaldehyde in phosphate-buffered saline (PBS), pH 7.2. The brains were removed and fixed by immersion for a further night in the same fixative. Tissues were processed for paraffin wax embedding, using the standard protocols. The tissues were dehydrated in ethanol, cleared in xylene, and embedded in paraffin wax.
RNA isolation and RT-PCR
Total RNA was extracted from each tissues using TRIzol Reagent (Invitrogen Corporation, Carlsbad, CA, USA) according to the supplier’s instructions. Complementary DNA (cDNA) synthesis was carried out using a SuperScript III First Strand Synthesis System for RT-PCR kit (Invitrogen Corporation, Carlsbad, CA, USA) according to the supplier’s instruction. PCR was performed by procedure previously reported (Urai et al. 2002) with some modifications. Synthetic oligonucleotide PCR primers for rat DAO were 5′-GTGGCATCTTTCGAAGAGGT-3′ and 5′-AGGCGTTCTCTTTCTAGCCG-3′. Primers for β-actin were 5′-TTGTAACCAACTGGGACGATATGG-3′ and 5′-GATCTTGATCTTCATGGTGCTAGG-3′. Fifty microliters of reaction mixture containing 2 μl of cDNA sample as template, 500 nM 5′ and 3′ PCR primers, 40 μM deoxyribonucleoside triphosphate (dNTP), 1 mM MgCl2, and 2.5 units of AmpliTaq DNA polymerase (Applied Biosystems, Foster City, CA, USA) in GeneAmp PCR buffer was subjected to amplification in DNA thermal cycler (Applied Biosystems). Following heat denaturation step of enzyme (for 5 min at 95°C), PCR cycles were performed with the following profile: denaturation for 30 s at 94°C, annealing for 120 s at 57°C, and extension for 150 s at 72°C; with unsaturated cycles (for DAO: 34 cycles, for β-actin: 25 cycles). At the end of PCR, the reaction mixture was separated on 2% agarose gel, and then stained in 0.5 μg/ml ethidium bromide solution.
Synthesis of probes for in situ hybridization
The template for RNA probe synthesis was produced with the use of nested PCR method. Rat DAO cDNA fragment (822 bp) was generated from brain total RNA by RT-PCR method using the first pair of primer (sense primer 5′-ACGTTACCACCCAGCCCAA-3′ and the antisense primer 5′-AGGCGTTCTCTTTCTAGCCG-3′). This first PCR product was further amplified with the use of the nested primers (sense primer containing SP6 RNA polymerase promoter sequence (underlined) 5′-ATTTAGGTGACACTATAGAATACATCTATGCGGATCGCTTCAC-3′, antisense primer containing T7 RNA polymerase promoter sequence (underlined) 5’-AATTGTAATACGACTCACTATAGGGCGACTCCTCTCACCACCTCTTCG-3’). We purified the second PCR product using GenElute PCR Clean-up Kit (Sigma, Saint Louis, Missouri, USA) and then used 1 μg of purified product as template to synthesize digoxigenin (DIG)-labeled RNA probes (454 nucleotides for sense probe and 449 nucleotides for antisense probe) according to the manual instructions of DIG RNA Labeling Kit (Roche Diagnostics, Basel, Switzerland). The quality and integrity of the probes were checked on a denaturing polyacrylamide gel. Incorporation of DIG was monitored by dot blot, according to the DIG RNA Labeling Kit protocol (Roche).
In situ hybridization procedures
Paraffin brain sections (6 μm) were mounted on MAS-coated slides (Matsunami Adhesive Silane; Matsunami glass Ind., Ltd, Osaka, Japan), dewaxed, and rehydrated, then treated with 2 μg/ml proteinase K in PBS for 20 min at 37°C. After a wash in PBS three times for 5 min, the section were acetylated for 10 min in freshly prepared 0.25% acetic anhydride in 0.1 M triethanolamine (pH 8.0) for 20 min, then washed in 4 × saline sodium citrate (SSC; 1 × SSC = 0.15 M NaCl, 0.015 M sodium citrate, pH 7.0). Sections were prehybridized by hybridization buffer (4 × SSC, 40% deionized formamide, 10% dextran sulfate, 1 × Denhardt’s solution, 10 mM DTT, 1 mg/ml yeast RNA and 1 mg/ml single-stranded DNA) for 1 h at 57°C. For hybridization, slides were probed with 100 μl hybridization buffer containing 2 ng/ml DIG-labeled RNA probe. The sections were covered with parafilm and were hybridized for 16 h at 57°C in humidified chamber. The sections were washed in 4 × SSC at 57°C, 2 × SSC containing 50% formamide for 1 h at 57°C, and then washed twice in 0.1 × SSC for 1 h at 57°C. The sections were placed in blocking solution containing 0.1 M maleic acid (pH 7.5), 0.15 M NaCl and 1% blocking reagent (Roche). Each section was covered with 400 μl Fab fragments from an anti-DIG antibody conjugated with alkaline phosphatase (1:1,000 dilution, Roche) and incubated for 2 h at room temperature. The sections were washed four times for 15 min in Tris-buffered saline with Tween-20 (TBS-T; 20 mM Tris–HCl, pH 8.0, 0.5 M NaCl and 0.1% Tween-20), and once for 15 min in detection buffer (0.1 M Tris–HCl and 0.1 M NaCl, pH 9.5), then incubated in a nitroblue tetrazolium chloride and 5-bromo-4-chloro-3-indolyl-phosphate (NBT/BCIP) substrate solution overnight at 4°C. The color reaction was stopped by immersing the sections in water for 10 min. The sections were mounted directly in Aqua-Poly/Mount (Polysciences Inc., Eppelheim, Germany).
Preparation of human tissue
Five micrometer-thick serial sections were prepared from autopsied brains of seven schizophrenic patients and seven control subjects together with one amyotrophic lateral sclerosis (ALS) and one cerebral infarction (CI). The tissues were fixed with 4% paraformaldehyde or 10% neutral formalin and embedded in paraffin. Schizophrenic cases included a 73-year-old patient, a 61-year-old patient, a 72-year-old patient, two 76-year-old patients, a 72-year-old patient, and a 67-year-old patient. Non-schizophrenic neurological and psychiatric disease cases included a 66-year-old patient with ALS and a 56-year-old patient with CI. Each case includes frontal lobe, neocortex of temporal lobe, hippocampus, amygdala, thalamus, cerebellum, pons, medulla oblongata, cervical spinal cord, and CP region. Autopsies on all subjects were performed at the National Center Hospital of Neurology and Psychiatry, National Center of Neurology and Psychiatry (NCNP), Tokyo, Japan. Tissue samples were obtained from Research Resource Network.
Human adult normal brain tissues, medulla oblongata, corpus callosum, spinal cord, peripheral nerve, cerebral cortex, mesencephalon, cerebellum, and pons (Human Organ Systems Multiple-Tissue 1, lot no. A605358), were obtained from BioChain Institute, Inc. (Hayward, CA, USA) as a control. Three different control CP sections (lot no. A710241, B303116 and A609356) were used for immunohistochemical analysis. In addition, four control CP sections (55-years old, 63-years old, 73-years old, and 74-years old) were obtained from Tokushima University Hospital, Tokushima, Japan. The present study was approved by the Ethics Committees of NCNP and Tokushima University Hospital.
Western blotting and immunoprecipitation
To generate the anti-human DAO antibody, a purified recombinant human DAO was used as an antigen. The rabbit polyclonal anti-human DAO antibody (SCRUM Inc., Tokyo, Japan) was raised against this full-length human DAO.
For Western blot and immunoprecipitatoin analyses, rat brains were homogenized in RIPA buffer (25 mM Tris–HCl, pH 7.6, 150 mM NaCl, 1% NP-40, 1% sodium deoxycholate and 0.1 % SDS) containing Complete Mini Protease Inhibitor Cocktail (Roche). Protein samples (each 100 μg total protein) were subjected to electrophoresis on 15% polyacrylamide gel, followed by blotting onto Immobilon-P membranes (Millipore, Bedford, MA, USA). Membranes were immersed in blocking buffer (5% skim milk in TBS-T), then were incubated with primary antibody (anti-human DAO 1:3,000; anti-β-actin 1:4,000) in the same buffer. Detection of each protein was carried out with an ECL Plus Western Blotting Detection System (GE Healthcare UK Ltd, Little Chalfont, UK) according to the manufacturer’s instructions. To perform the immunoprecipitation analysis, protein samples (each 1 mg total protein) were mixed with polyclonal anti-porcine DAO antiserum (Fukui et al. 1988). Immunoprecipitates were collected by using Protein G Plus-Agarose (Santa Cruz Biotechnology, Inc., CA, USA), and then analyzed by Western blotting as described above.
Immunocytochemical procedures
For immunocytochemical analysis, human DAO cDNA was inserted into a powerful mammalian expression vector pEF-BOS (Mizushima and Nagata 1990). This plasmid (pEF-BOS-hDAO) was transfected into NIH3T3 cells by FuGENE HD Transfection Reagent (Roche). Transfected NIH3T3 cells were seeded onto poly-l-lysine- coated coverslips and incubated for 48 h at 37°C. The cells were washed in PBS three times and fixed in 4% paraformaldehyde in PBS for 30 min. The endogenous peroxidase was inactivated in PBS with 0.3% H2O2 for 5 min. The membranes were permeabilized in PBS with 0.1% Triton X-100 for 5 min. Subsequently, the cells were blocked for 30 min with blocking buffer (3% BSA/PBS), and then incubated with rabbit anti-human DAO antibodies (1:800) or preimmune rabbit serum (1:800) overnight at 4°C. After being washed in PBS, the cells were treated with peroxidase-conjugated anti-rabbit IgG (1:5,000). The cells were washed three times in PBS, and then incubated in a 3,3′-diaminobenzidine (DAB) solution. The color reaction was stopped by immersing the sections in water. Finally, the cells were counterstained with hematoxylin. For light microscopical analysis, cells were viewed using Optiphoto microscope equipped with a Nikon digital camera SD-Fil (Nikon Corporation, Tokyo Japan).
Immunohistochemical procedures
Immunohistochemistry was performed on the Benchmark-XT (Ventana Medical Systems Inc., Tucson, AZ, USA). The anti-human DAO antibody was diluted by Discovery Antibody Diluent (Ventana Medical Systems Inc.) at a dilution of 1:300 or 1:800. Slides were incubated with the antibody for 32 min at 37°C. The Ventana I-VIEW DAB Universal Kit was the secondary detection method. This was followed by streptavidin-horseradish peroxidase conjugate. Sections were visualized with DAB. Finally, slides were counterstained with hematoxylin. For light microscopical analysis, sections were viewed using Optiphoto microscope equipped with a Nikon digital camera SD-Fil (Nikon Corporation).
Quantification of DAO-expressing CP epithelial cells
The final figures (Fig. 5) were produced from the photomicrographs in Adobe Photoshop, and, when necessary, brightness was adjusted to reflect the natural view through the microscope. The area of DAO-positive epithelial cells and the total area of CP were measured using digitized images and Image-Pro Plus software (version 6.1; Media Cybernetics Inc., Bethesda, MD, USA). The size of the visual field of each image was 270 × 347 μm. The acquisition setting (intensity range of total area R 0–200, G 0–150, B 0–170, intensity range of immunopositive area R 120–155, G 80–170, B 100–140) for each photomicrographs were kept constant during the analysis of each sections. The proportion of the immunopositive CP epithelial cells was counted in each of the seven schizophrenic, two non-schizophrenic, and seven control sections. The normal distribution and the equal variance of the data were checked, and then the differences in the relevant data within and between the schizophrenic and control sections were studied by t-test. Differences were regarded as significant at P < 0.001.
Results
Expression of DAO mRNA in rat tissues
In search of the pathophysiological role(s) of DAO in rat brain, we considered it important to analyze the expression profile of DAO. First, we analyzed distribution of DAO mRNA signals. Total RNA extracts from different brain regions and peripheral tissues were analyzed by RT-PCR using gene-specific primers. Results are illustrated in Fig. 1. A strong signal was detected in tissues, (kidney, liver, and cerebellum), expected to express high levels of DAO (Fig. 1, lanes 4, 5 and 7). In addition, the DAO mRNA expression was confirmed in cerebral cortex (Fig. 1, lane 6), although the level of which was lower than that in cerebellum. These results are consistent with the previous report that DAO mRNA was detected in primary astrocytes cultured from rat cerebellum and cerebral cortex (Urai et al. 2002). Moreover, we considered it possible for DAO to be expressed in CP, main function of which is the production of CSF, and examined the presence of mRNA for DAO. As shown in Fig. 1 lane 8, it was confirmed that DAO mRNA was expressed in the rat CP. In contrast, DAO mRNA was not detected in extracts from lung and heart (Fig. 1, lane 1 and 2).
d-Amino acid oxidase mRNA was detected in several rat tissues by RT-PCR. The RT-PCR was performed by using DAO and β-actin specific primers. The PCR products of predicted size were 398 bp (DAO) and 764 bp (β-actin). Lane 1 DNA size marker, lane 2 lung, lane 3 heart, lane 4 kidney, lane 5 liver, lane 6 cerebral cortex, lane 7 cerebellum, lane 8 choroids plexus. A specific signal for DAO was detected in the kidney, liver, cerebral cortex, cerebellum, and choroid plexus
Distribution of DAO gene expression in rat brain
To determine the regional and cellular distribution of DAO in the rat brain, we investigated the expression pattern of the DAO gene at the mRNA level using in situ hybridization. In the rat cerebellar sections, specific hybridization signals for DAO were found in the Purkinje cell layer. These signals were considered to correspond to Bergmann glial cells, based on their location in surrounding Purkinje cells and the small size of the positive cells compared to those of Purkinje cells. On the other hand, Purkinje cells were invariably negative for staining (Fig. 2a). Furthermore, in the pons sections, the signals were observed in small cells (Fig. 2b). In the medulla oblongata sections, the signals were also observed in many small cells, similar to those in the pons (Fig. 2c). These cells were presumed to be astrocytes, based on their localization and size. Low levels of DAO mRNA were found in the cerebral cortex (Fig. 2d) and hippocampus (Fig. 2e) in the areas surrounding the neuronal cells, and these signals were observed in apparent astrocytes. The expression of DAO mRNA in CP was examined by in situ hybridization analysis. As shown in Fig. 2f, the hybridization signal was clearly detected in CP epithelial cells as expected from the result of RT-PCR analysis. When brain sections were hybridized with DAO specific sense RNA probes, we observed only background labeling (Fig. 2a′–f′).
Distribution of DAO mRNA in situ hybridization signals in several regions of the rat brain. Each figure represents hybridization result with DIG-labeled RNA antisense probe (a–f) and sense probe (a′–f′). a DAO mRNA signals were detected in cerebellum. These signals in the Purkinje cell layer were considered to correspond to Bergmann glial cells (arrows). Purkinje cells were invariably negative for staining (arrowheads). GL granular layer, ML molecular layer, PL Purkinje cell layer. b DAO mRNA signals were detected in pons. These signals were considered to correspond to astrocytes (arrows). c DAO mRNA signals were detected in medulla oblongata. These signals were considered to correspond to astrocytes. d Low levels of DAO mRNA were found in the cerebral cortex in the areas surrounding the neuronal cells, and these signals were observed in apparent astrocytes. e Low levels of DAO mRNA expression were found in the hippocampus in the areas surrounding the neuronal cells, and these signals were observed in apparent astrocytes. f The hybridization signal for DAO was detected in choroid plexus epithelial cells. Scale bar = 50 μm
Expression of DAO protein in rat brain
Expression of endogenous DAO protein was investigated by Western blot analysis on rat brain extracts (Fig. 3a). A strong band at approximately 39 kDa was detected in cerebellum, brainstem, and spinal cord reportedly expressing DAO (Verrall et al. 2007; Moreno et al. 1999; Horiike et al. 1994). On the other hand, DAO could not be detected in choroid plexus, prefrontal cortex, hippocampus, thalamus, and striatum. In order to detect minute amount of DAO proteins, we further performed immunoprecipitation analysis. As shown in Fig. 3b, DAO protein was detected in the prefrontal cortex and thalamus (lane 3 and 6). Moreover, we could confirm the expression of DAO protein in choroid plexus and hippocampus (lane 4 and 5), together with the absence of the signal in striatum (lane 7). Furthermore, immunohistochemical analysis of rat cerebellum and CP, the same tissues as used for in situ hybridization, were performed with antibody to human DAO (Fig. 3c). In the cerebellum, DAO immunoreactivity was detected in the Purkinje cell layers. Only modest levels of immunoreactivity for DAO were found within the CP. These results were consistent with rat DAO mRNA distribution analyzed by in situ hybridization.
Detection of DAO protein expression in rat brain. a Western blot analysis was carried out using rat brain; lane 1 cerebellum, lane 2 brainstem, lane 3 spinal cord, lane 4 choroid plexus, lane 5 prefrontal cortex, lane 6 hippocampus, lane 7 thalamus, lane 8 striatum. A specific signal for DAO was detected at 39 kDa (upper panel). Blots were re-probed with anti-β-actin as a loading control (lower panel). b Immunoprecipitates were analyzed by Western blotting analysis with anti-human DAO antibody using rat brain; lane 1 cerebellum, lane 2 brainstem, lane 3 prefrontal cortex, lane 4 choroid plexus, lane 5 hippocampus, lane 6 thalamus, lane 7 striatum. c Immunohistochemical analysis of rat cerebellum and CP was performed with antibodies to human DAO (immune) and rabbit serum (preimmune). Rat sections were the same as used for in situ hybridization analysis. In rat cerebellum, DAO immunoreactivity was detected in the molecular and Purkinje cell layers. Only modest levels of immunoreactivity for DAO were observed within rat CP. Scale bar = 50 μm
DAO expression pattern in human choroid plexus with psychiatric and neurological disorder
The specificity of anti-human DAO antibody was verified by immunocytochemical analysis (Fig. 4). Specific recognition of DAO with this antibody was confirmed in NIH3T3 cells expressing human DAO without any background signal. To confirm the expression of DAO in human CP and to study the pathophysiological role of DAO expression in the psychiatric and neurological disorder, we first examined DAO distribution in control human CP. Immunohistochemical analysis with the anti-human DAO antibody showed that DAO is expressed in the control human CP as well as in the rat CP (Fig. 5a–c). In agreement with the data derived from in situ hybridization (Fig. 2f) and immunohistochemistry (Fig. 3c), DAO expressing cells were also confirmed in the CP epithelial cells.
Immunohistochemical analysis of human choroid plexus with antibody against human DAO. Regional localization of DAO determined by immunohistochemistry in the control (a–c), schizophrenic (d–f), ALS (g), and CI (h) CP. Shown are all control cases and three typical results of schizophrenic cases. Scale bar = 50 μm
To examine the possible alteration of DAO expression levels in schizophrenic CP compared to controls, we next performed immunohistochemical analysis from postmortem human schizophrenic cases with the anti-DAO antibody. There was no significant difference in the age between control (mean ± SD year, 65.8 ± 6.8) and schizophrenic cases (70.8 ± 5.9), as judged by the comparison between two groups using the t-test (P value = 0.18). Seven schizophrenic CP showed intense immunoreactivity for DAO in epithelial cells (Fig. 5d–f), whereas an ALS sample and a CI sample did not seem to differ from control significantly in DAO immunoreactivity (Fig. 5g, h).
Furthermore, we quantitatively compared the DAO immunopositive areas between control and schizophrenic cases. It was shown that DAO immunopositive area within CP epithelial cell area was measured by selected color range (Fig. 6). In this quantification, the percentage of DAO immunopositive area was calculated 2.8 ± 6.6 (mean ± SD) in seven control cases (Fig. 6). In contrast, the DAO immunopositive area in seven schizophrenic patients (34.5 ± 14.0) was significantly higher than that of control cases (P value = 0.00049). These results support the idea that alteration of DAO expression in CP may be related to pathophysiology of schizophrenia.
The quantitative analysis of DAO-expressing area in CP epithelial cells. The histogram represents comparison of immunopositive areas between schizophrenic and control cases. Schizophrenic (n = 7) and control cases (n = 7) were immunostained with anti-human DAO antibody. Schizophrenic subjects showed increased DAO immunopositive area in the choroid plexus compared to control subjects (*P < 0.001)
Regional distribution of DAO in the control human brain
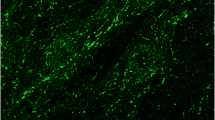
To investigate whether DAO expression pattern in human brain is similar to DAO mRNA expression in rat brain, we performed immunohistochemical analysis in control human brain sections. In the cerebellum, DAO immunoreactivity was detected in the molecular and Purkinje cell layers (Fig. 7a). These signals were considered to correspond to Bergmann glial cells and their processes, based on their location in surrounding Purkinje cells and the morphological feature of the positive cells. On the other hand, the Purkinje cells were unlabeled. Moreover, DAO immunopositive cells were found in the pons (Fig. 7b) and medulla oblongata (Fig. 7c) section. These signals were considered to correspond to astrocytes, based on their morphology. Only modest levels of immunoreactivity for DAO were found within the cerebral cortex (data not shown). These results were consistent with rat DAO mRNA distribution analyzed by in situ hybridization. In addition, the immunoreactivity of DAO in the spinal cord was slightly detected both in the white matter and gray matter (Fig. 7d).
Distribution of DAO-expressing cells in several regions of the control human brain. a In the cerebellum, DAO immunoreactivity was detected in the molecular and Purkinje cell layers. These signals were considered to correspond to Bergmann glial cells and their processes, based on their location in surrounding Purkinje cells and the morphological feature of the positive cells. On the other hand, the Purkinje cells were unlabeled. b DAO immunopositive cells were found in the pons. These signals were considered to correspond to astrocytes, based on their morphology. c DAO immunopositive cells were found in the medulla oblongata section. These signals were considered to correspond to astrocytes, based on their morphology. d DAO immunopositive cells were found in the spinal cord. These signals were considered to correspond to astrocytes, based on their morphology. Scale bar = 50 μm
Comparison of DAO expression pattern with schizophrenic cases
To study the possible alteration of DAO distribution in any brain regions other than CP, we made a comparison of DAO immunoreactivity in schizophrenic cases. First, we analyzed distribution of DAO by using postmortem schizophrenic brain. In the cerebellum from schizophrenic patients, DAO immunoreactivity was strong in the molecular and Purkinje cell layers (Fig. 8a). The distribution of immunoreactivity for DAO was found in the pons with schizophrenia (Fig. 8b). Immunoreactivity for DAO was detected in schizophrenic medulla oblongata, similar to that in the pons (Fig. 8c). In the cervical spinal cord with schizophrenia, the immunoreactivity of DAO was found both in white matter and internal gray matter (Fig. 8d). These signals were considered to correspond to glial cells and their processes, especially Bergmann glia in cerebellum, based on their location and morphological feature of the positive cells. These results were consistent with DAO distribution analyzed in control human brain.
Distribution of DAO-expressing cells in several regions of the human brain from schizophrenic patients. a In the cerebellum, DAO immunoreactivity was detected in the molecular and Purkinje cell layers. These signals were considered to correspond to Bergmann glial cells and their processes, based on their location in surrounding Purkinje cells and the morphological feature of the positive cells. On the other hand, the Purkinje cells were unlabeled. DAO immunopositive cells were found in the pons (b), medulla oblongata (c), and spinal cord (d) section. These signals were considered to correspond to astrocytes, based on their morphology. Scale bar = 50 μm
In the cerebellum and medulla oblongata from schizophrenic patients, DAO immunoreactivity was elevated in schizophrenia compared with controls (Figs. 7, 8). DAO immunoreactivity in pons of schizophrenic cases was similar to that of control case (Fig. 7b, 8b). These results indicated that DAO expression levels in schizophrenic patients is likely to be elevated, although the distribution pattern of DAO expression is similar to that of all cases.
Discussion
The results of our study provide the first description of the histochemical comparison for the DAO expression pattern and expression levels in schizophrenia, ALS, CI, and control brain. Two major conclusions can be drawn from our findings. First, DAO mRNA and protein was distributed in rat and human CP. Second, DAO immunoreactivity in schizophrenic CP was higher than that in other cases including control, ALS, and CI. It is thought that CP has an important role in the homeostasis of nutrients including amino acids in the CSF (Redzic and Segal 2004). These findings suggest that low d-serine levels in CSF in the disorder may have been due to increased DAO expression in the CP. We raise the possibility that an increase in DAO expression in the CP could decrease d-serine availability, thus contributing to NMDA receptor hypofunction thought to occur in schizophrenia. However, this possibility awaits further definitive quantification.
The present study found that DAO mRNA and protein were detected in the cerebellum, in good accord with previous studies of its expression and activity in human (Verrall et al. 2007) and rodent (Horiike et al. 1994; Schell et al. 1995; Moreno et al. 1999). Cerebellar DAO mRNA expression was primarily localized to Bergmann glia (Fig. 2). In the rhombencephalon, the distribution pattern of the DAO mRNA is consistent with previous studies of DAO activity and expression in rat (Horiike et al. 1987, 1994; Moreno et al. 1999) and human (Verrall et al. 2007). The situation regarding DAO in the forebrain has been less clear. Our data confirmed that DAO is expressed, both as mRNA and as protein, in the rat cerebral cortex (prefrontal cortex, hippocampus and thalamus) by in situ hybridization and immunoprecipitation (Figs. 2, 3). These observations were consistent with the Western blotting findings of the human study by Verrall et al. (2007).
Moreover, the distribution of DAO in human was of the same pattern of DAO distribution in rat brain (Figs. 2, 7). DAO expression was not only detected in rat CP epithelial cells but also in human CP epithelial cells. These results suggest that regulatory mechanisms governing the d-serine level of CSF may exist in the CP. d-Aspartate oxidase is a flavoenzyme similar to DAO. d-Aspartate oxidase specifically catalyzes the oxidative deamination of acidic d-amino acids carrying two carboxylic groups such as d-aspartate, d-glutamate, or NMDA. Early biochemical investigations revealed d-aspartate oxidase activity in homogenates of hog CP (Yusko and Neims 1973). The CP has an important role in the homeostasis of nutrients including amino acids in the CSF (Redzic and Segal 2004). The CP is in close contact with the CSF; the CP epithelial cells (constituting the blood–CSF barrier) form an interface between CSF and periphery, since their apical side faces the CSF and their basal side faces fenestrated capillaries (Nathanson and Chun 1989). The exchanges between the blood and the CSF across the CP epithelial cells are tightly regulated, in the presence of interepithelial tight junctions, by various transports and metabolic processes. They also protect the CSF by preventing the entry of other potentially toxic substances (Strazielle et al. 2004). On the other hand, it is thought that d-serine can penetrate the blood–brain barrier much better than other amino acids (i.e., glycine, glutamate) (Bauer et al. 2005; Nishikawa 2005; Takahashi et al. 1997). Thus, DAO may play a role in modulating the d-serine level of CSF while d-serine across the CP epithelial cells. In the previous study, it has been reported that d-serine level was measured in the serum (Hashimoto et al. 2003; Yamada et al. 2005; Ohnuma et al. 2008) and the CSF samples from human (Hashimoto et al. 2005; Bendikov et al. 2007). Based on these results, we speculate that the concentration of d-serine in CSF is lower than that in serum. Taking all of these results together, we hypothesized that d-serine in the blood and CSF was degradated by DAO across the CP. Moreover, DAO expressing in CP may modulate the entry of d-serine into the CSF from blood, and then the levels of the CSF will have some influence on the composition of the brain interstitial fluid and neuronal tissue function.
Comparison of DAO expression in CP between schizophrenic and non-schizophrenic subjects indicated that numbers of DAO expressing cells were increased in schizophrenia. Seven schizophrenic CP showed intense immunoreactivity for DAO in CP epithelial cells (Fig. 5d–f), whereas seven controls, an ALS sample, and a CI sample did not seem to differ significantly in DAO immunoreactivity in CP (Fig. 5a–c, g, h). Furthermore, the DAO immunopositive areas in CP of schizophrenic patients were significantly high in all cases (Fig. 6). Thus, schizophrenic pathophysiology may include that hypofunction of the NMDA receptor was caused by elevation of DAO expression in CP. Previous studies have demonstrated that reduced d/total (d + l) serine ratio in CSF samples from schizophrenia patients compared with control subjects (Hashimoto et al. 2005). In addition, other group recently found that d-serine levels were lower in CSF samples of schizophrenic patient when compared to controls (Bendikov et al. 2007). These results suggest that reduced d-serine levels in CSF were induced by elevation of DAO expression in schizophrenic CP. These results may support a possibility that the elevation of DAO expression level in CP is involved in decreased d-serine level in CSF. We showed the inhibition of the activity of human DAO by two antischizophrenic drugs and its related compounds, risperidone and chlorpromazine, in vitro (Abou El-Magd et al. 2009; Iwana et al. 2008). These results indicate that these drugs are pharmacologically active substances with a possible involvement in the glutamatergic system though the inhibition of DAO. On the other hand, the recent report (Tsai et al. 1998) of significant improvements in negative symptoms obtained following addition of d-serine to conventional neuroleptics regimens may herald an additional, novel approach to schizophrenia treatment. Studies performed with patients indicate that d-serine significantly improves schizophrenia symptoms when used as adjuvant to conventional neuroleptics, and the efficacy and safety of d-serine adjuvant treatment for Occidental schizophrenia patients treated with newer atypical antipsychotics was confirmed (Heresco-Levy et al. 2005). Taken together, co-administration of antipsychotics with d-serine may contribute to the effective dosage of d-serine in CSF through the inhibition of DAO activity in CP. Thus, it may be possible for the regulation of d-serine metabolism by DAO in CP to be a new therapeutic approach for schizophrenia, targeting the NMDA-glycine site.
The association findings relating schizophrenia with genes for d-serine synthesis and metabolizing system indicate a possible molecular pathway involved in susceptibility to the disorder. DAO and serine racemase (converting enzyme from l-serine to d-serine) have been linked to schizophrenia and their aberrant expression has been reported in subjects with schizophrenia (Verrall et al. 2007; Madeira et al. 2008). The imbalance between d-serine production by serine racemase and its degradation by DAO expression could be responsible for a decrease in extracellular d-serine concentration contributing to NMDA hypofunction thought to cause of schizophrenia.
In conclusion, we have shown the expression of DAO in CP and the elevation of DAO expression in schizophrenic patients. Detailed studies on the d-amino acid biosystem in the CSF will be necessary to better understand the pathophysiology of schizophrenia. Furthermore, DAO expressed in CP may be regarded as a potential therapeutic target for schizophrenia.
Abbreviations
- DAO:
-
d-Amino acid oxidase
- NMDA:
-
N-Methyl d-aspartate
- CP:
-
Choroid plexus
- CSF:
-
Cerebrospinal fluid
- cDNA:
-
Complementary DNA
- dNTP:
-
Deoxyribonucleoside triphosphate
- PBS:
-
Phosphate buffer saline
- DIG:
-
Digoxigenin
- MAS:
-
Matsunami adhesive silane
- TEA:
-
Triethanolamine
- SSC:
-
Saline sodium citrate
- TBS-T:
-
Tris-buffered saline with Tween-20
- NBT:
-
Nitroblue tetrazolium
- BCIP:
-
5-Bromo-4-chloro-3indolyl-phosphate
- ALS:
-
Amyotrophic lateral sclerosis
- CI:
-
Cerebral infarction
References
Abou El-Magd RM, Park HK, Kawazoe T, Iwana S, Ono K, Chung SP, Miyano M, Yorita K, Sakai T, Fukui K (2009) The effect of risperidone on d-amino acid oxidase activity as a hypothesis for a novel mechanism of action in the treatment of schizophrenia. J Psychopharmacol (in press) doi:10.1177/0269881109102644
Bauer D, Hamacher K, Bröer S, Pauleit D, Palm C, Zilles K, Coenen HH, Langen KJ (2005) Preferred stereoselective brain uptake of d-serine—a modulator of glutamatergic neurotransmission. Nucl Med Biol 32:793–797. doi:10.1016/j.nucmedbio.2005.07.004
Bendikov I, Nadri C, Amar S, Panizzutti R, Miranda JD, Wolosker H, Agam G (2007) A CSF and postmortem brain study of d-serine metabolic parameters in schizophrenia. Schizophr Res 90:41–51. doi:10.1016/j.schres.2006.10.010
Chumakov I, Blumenfeld M, Guerassimenko O, Cavarec L, Palicio M, Abderrahim H, Bougueleret L, Barry C, Tanaka H, Rosa PL, Puech A, Tahri N, Cohen-Akenine A, Delabrosse S, Lissarrague S, Picard FP, Maurice K, Essioux L, Millasseau P, Grel P, Debailleul V, Simon AM, Caterina D, Dufaure I, Malekzadeh K, Belova M, Luan JJ, Bouillot M, Sambucy JL, Primas G, Saumier M, Boubkiri N, Martin-Saumier S, Nasroune M, Peixoto H, Delaye A, Pinchot V, Bastucci M, Guillou S, Chevillon M, Sainz-Fuertes R, Meguenni S, Aurich-Costa J, Cherif D, Gimalac A, Duijn CV, Gauvreau D, Ouellette G, Fortier I, Raelson J, Sherbatich T, Riazanskaia N, Rogaev E, Raeymaekers P, Aerssens J, Konings F, Luyten W, Macciardi F, Sham PC, Straub RE, Weinberger DR, Cohen N, Cohen D (2002) Genetic and physiological data implicating the new human gene G72 and the gene for d-amino acid oxidase in schizophrenia. Proc Natl Acad Sci USA 99:13675–13680. doi:10.1073/pnas.182412499
Fukui K, Watanabe F, Shibata T, Miyake Y (1987) Molecular cloning and sequence analysis of cDNAs encoding porcine kidney d-amino acid oxidase. Biochemistry 26:3612–3618. doi:10.1021/bi00386a054
Fukui K, Momoi K, Watanabe F, Miyake Y (1988) In vivo and in vitro expression of porcine d-amino acid oxidase: in vitro system for synthesis of functional enzyme. Biochemistry 27:6693–6697. doi:10.1021/bi00418a008
Hashimoto A, Nishikawa T, Hayashi T, Fujii N, Harada K, Oka T, Takahashi K (1992) The presence of free d-serine in rat brain. FEBS Lett 296:33–36. doi:10.1016/0014-5793(92)80397-Y
Hashimoto K, Fukushima T, Shimizu E, Komatsu N, Watanabe H, Shinoda N, Nakazato M, Kumakiri C, Okada S, Hasegawa H, Imai K, Iyo M (2003) Decreased serum levels of d-serine in patients with schizophrenia. Arch Gen Psychiatry 60:572–576
Hashimoto K, Engberg G, Shimizu E, Nordin C, Lindström LH, Iyo M (2005) Reduced d-serine to total serine ratio in the cerebrospinal fluid of drug naive schizophrenic patients. Prog Neuropsychopharmacol Biol Psychiatry 29:767–769. doi:10.1016/j.pnpbp.2005.04.023
Heresco-Levy U, Javitt DC, Ebstein R, Vass A, Lichtenberg P, Bar G, Catinari S, Ermilov M (2005) d-Serine efficacy as add-on pharmacotherapy to risperidone and olanzapine for treatment-refractory schizophrenia. Biol Psychiatry 57:577–585. doi:10.1016/j.biopsych.2004.12.037
Horiike K, Tojo H, Arai R, Yamano T, Nozaki M, Maeda T (1987) Localization of d-amino acid oxidase in Bergmann glial cells and astrocytes of rat cerebellum. Brain Res Bull 19:587–596. doi:10.1016/0361-9230(87)90076-1
Horiike K, Tojo H, Arai R, Nozaki M, Maeda T (1994) d-Amino-acid oxidase is confined to the lower brain stem and cerebellum in rat brain: regional differentiation of astrocytes. Brain Res 652:297–303. doi:10.1016/0006-8993(94)90240-2
Iwana S, Kawazoe T, Park HK, Tsuchiya K, Ono K, Yorita K, Sakai T, Kusumi T, Fukui K (2008) Chlorpromazine oligomer is a potentially active substance that inhibits human d-amino acid oxidase, product of a susceptibility gene for schizophrenia. J Enzyme Inhib Med Chem 23:901–911. doi:10.1080/14756360701745478
Kawazoe T, Tsuge H, Pilone MS, Fukui K (2006) Crystal structure of human d-amino acid oxidase: context-dependent variability of the backbone conformation of the VAAGL hydrophobic stretch located at the si-face of the flavin ring. Protein Sci 15:2708–2717. doi:10.1110/ps.062421606
Kawazoe T, Park HK, Iwana S, Tsuge H, Fukui K (2007a) Human d-amino acid oxidase: an update and review. Chem Rec 7:305–315. doi:10.1002/tcr.20129
Kawazoe T, Tsuge H, Imagawa T, Aki K, Kuramitsu S, Fukui K (2007b) Structural basis of d-DOPA oxidation by d-amino acid oxidase: alternative pathway for dopamine biosynthesis. Biochem Biophys Res Commun 355:385–391. doi:10.1016/j.bbrc.2007.01.181
Krebs HA (1935) Metabolism of amino-acids: deamination of amino-acids. Biochem J 29:1620–1644
Madeira C, Freitas ME, Vargas-Lopes C, Wolosker H, Panizzutti R (2008) Increased brain d-amino acid oxidase (DAAO) activity in schizophrenia. Schizophr Res 101:76–83. doi:10.1016/j.schres.2008.02.002
Mizushima S, Nagata S (1990) pEF-BOS, a powerful mammalian expression vector. Nucleic Acids Res 18:5322
Mohn AR, Gainetdinov RR, Caron MG, Koller BH (1999) Mice with reduced NMDA receptor expression display behaviors related to schizophrenia. Cell 98:427–436. doi:10.1016/S0092-8674(00)81972-8
Momoi K, Fukui K, Watanabe F, Miyake Y (1988) Molecular cloning and sequence analysis of cDNA encoding human kidney d-amino acid oxidase. FEBS Lett 238:180–184. doi:10.1016/0014-5793(88)80252-7
Momoi K, Fukui K, Tada M, Miyake Y (1990) Gene expression of d-amino acid oxidase in rabbit kidney. J Biochem 108:406–413
Moreno S, Nardacci R, Cimini A, Cerù MP (1999) Immunocytochemical localization of d-amino acid oxidase in rat brain. J Neurocytol 28:169–185. doi:10.1023/A:1007064504007
Mothet JP, Parent AT, Wolosker H, Brady RO Jr, Linden DJ, Ferris CD, Rogawski MA, Snyder SH (2000) d-Serine is an endogenous ligand for the glycine site of the N-methyl-d-aspartate receptor. Proc Natl Acad Sci USA 97:4926–4931
Nathanson JA, Chun LL (1989) Immunological function of the blood-cerebrospinal fluid barrier. Proc Natl Acad Sci USA 86:1684–1688
Nishikawa T (2005) Metabolism and functional roles of endogenous d-serine in mammalian brains. Biol Pharm Bull 28:1561–1565. doi:10.1248/bpb.28.1561
Ohnuma T, Sakai Y, Haeshima H, Hatano T, Hanzawa R, Kida S, Shibata N, Suzuki T, Arai H (2008) Changes in plasma glycine, l-serine, and d-serine levels in patients with schizophrenia as their clinical symptoms improve: results from the Juntendo University Schizophrenia Projects (JUSP). Prog Neuropsychopharmacol Biol Psychiatry 32:1905–1912. doi:10.1016/j.pnpbp.2008.07.022
Park HK, Shishido Y, Ichise-Shishido S, Kawazoe T, Ono K, Iwana S, Tomita Y, Yorita K, Sakai T, Fukui K (2006) Potential role for astroglial d-amino acid oxidase in extracellular d-serine metabolism and cytotoxicity. J Biochem 139:295–304. doi:10.1093/jb/mvj036
Pollegioni L, Fukui K, Massey V (1994) Studies on the kinetic mechanism of pig kidney d-amino acid oxidase by site-directed mutagenesis of tyrosine 224 and tyrosine 228. J Biol Chem 269:31666–31673
Raibekas AA, Fukui K, Massey V (2000) Design and properties of human d-amino acid oxidase with covalently attached flavin. Proc Natl Acad Sci USA 97:3089–3093. doi:10.1073/pnas/040559597
Redzic ZB, Segal MB (2004) The structure of the choroid plexus and the physiology of the choroid plexus epithelium. Adv Drug Deliv Rev 56:1695–1716. doi:10.1016/j.addr.2004.07.005
Schell MJ, Molliver ME, Snyder SH (1995) d-Serine, an endogenous synaptic modulator: Localization to astrocytes and glutamate-stimulated release. Proc Natl Acad Sci USA 92:3948–3952
Strazielle N, Khuth ST, Ghersi-Egea JF (2004) Detoxification systems, passive and specific transport for drugs at the blood–CSF barrier in normal and pathological situations. Adv Drug Deliv Rev 56:1717–1740. doi:10.1016/j.addr.2004.07.006
Tada M, Fukui K, Momoi K, Miyake Y (1990) Cloning and expression of a cDNA encoding mouse kidney d-amino acid oxidase. Gene 90:293–297. doi:10.1016/0378-1119(90)90193-U
Takahashi K, Hayashi F, Nishikawa T (1997) In vivo evidence for the link between l- and d-serine metabolism in rat cerebral cortex. J Neurochem 69:1286–1290. doi:10.1046/j.1471-4159.1997.69031286
Tsai G, Yang P, Chung LC, Lange N, Coyle JT (1998) d-Serine added to antipsychotics for the treatment of schizophrenia. Biol Psychiatry 44:1081–1089. doi:10.1016/S0006-3223(98)00279-0
Urai Y, Jinnouchi O, Kwak KT, Suzue A, Nagahiro S, Fukui K (2002) Gene expression of d-amino acid oxidase in cultured rat astrocytes: regional and cell type specific expression. Neurosci Lett 324:101–104. doi:10.1016/S0304-3940(02)00184-2
Verrall L, Walker M, Rawlings N, Benzel I, Kew JN, Harrison PJ, Burnet PW (2007) d-Amino acid oxidase and serine racemase in human brain: normal distribution and altered expression in schizophrenia. Eur J Neurosci 26:1657–1669. doi:10.1111/j.1460-9568.2007.05769
Watanabe F, Fukui K, Momoi K, Miyake Y (1988) Effect of site-specific mutagenesis of tyrosine-55, methionine-110 and histidine-217 in porcine kidney d-amino acid oxidase on its catalytic function. FEBS Lett 238:269–272. doi:10.1016/0014-5793(88)80494-0
Yamada K, Ohnishi T, Hashimoto K, Ohba H, Iwayama-Shigeno Y, Toyoshima M, Okuno A, Takao H, Toyota T, Minabe Y, Nakamura K, Shimizu E, Itokawa M, Mori N, Iyo M, Yoshikawa T (2005) Identification of multiple serine racemase (SRR) mRNA isoforms and genetic analyses of SRR and DAO in schizophrenia and d-serine levels. Biol Psychiatry 57:1493–1503. doi:v0.1016/j.biopsych.2005.03.018
Yusko CS, Neims AH (1973) d-Aspartate oxidase in mammalian brain and choroid plexus. J Neurochem 21:1037–1039. doi:10.1111/j.1471-4159.1973.tb07555
Acknowledgments
This work was supported by a Grant-in-Aid for Scientific Research from the Ministry of Education, Science, Sports and Culture of Japan. Human tissue samples were obtained from the Research Resource Network and Tokushima University Hospital. We wish to thank Dr M. Shono (Division of Biomedical Technology, Support Center for Advanced Medical Sciences, The University of Tokushima) for the assistance with the microscopy and helpful comments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ono, K., Shishido, Y., Park, H.K. et al. Potential pathophysiological role of d-amino acid oxidase in schizophrenia: immunohistochemical and in situ hybridization study of the expression in human and rat brain. J Neural Transm 116, 1335–1347 (2009). https://doi.org/10.1007/s00702-009-0289-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-009-0289-7