Abstract
Irregular N-methyl-d-aspartate receptor (NMDAR) function is one of the main hypotheses employed to facilitate understanding of the underlying disease state of schizophrenia. Although direct agonism of the NMDAR has not yielded promising therapeutics, advances have been made by modulating the NMDAR co-agonist site which is activated by glycine and d-serine. One approach to activate the co-agonist site is to increase synaptic d-serine levels through inhibition of d-amino acid oxidase (DAO), the major catabolic clearance pathway for this and other d-amino acids. A number of DAO inhibitors have been developed but most have not entered clinical trials. One exception to this is sodium benzoate which has demonstrated efficacy in small trials of schizophrenia and Alzheimer’s disease. Herein we provide data on the effect of sodium benzoate and an optimised Takeda compound, PGM030756 on ex vivo DAO enzyme occupancy and cerebellar d-serine levels in mice. Both compounds achieve high levels of enzyme occupancy; although lower doses of PGM030756 (1, 3 and 10 mg/kg) were required to achieve this compared to sodium benzoate (300, 1000 mg/kg). Cerebellar d-serine levels were increased by both agents with a delay of approximately 6 h after dosing before the peak effect was achieved. Our data and methods may be useful in understanding the effects of sodium benzoate that have been seen in clinical trials of schizophrenia and Alzheimer’s disease and to support the potential clinical assessment of other DAO inhibitors, such as PGM030756, which demonstrate good enzyme occupancy and d-serine increases following administration of low oral doses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dysfunction of the NMDAR has been a much studied area of neurochemistry, with a particular focus on the treatment of schizophrenia [1]. Whilst direct agonism of the receptor has not proved to be a fruitful therapeutic route due to excitotoxicity [2], alternative methods for modulating the receptor have continued to be of interest. The use of Glycine Transporter 1 (Gly-T1) inhibitors to maintain and enhance the levels of glycine acting on NMDA receptors as a co-agonist has led to the identification of numerous compounds as potential antipsychotics [3]. In particular, bitopertin, was evaluated in Phase III clinical trials by Roche but subsequently discontinued [4]. An alternative to targeting glycine could be to consider the co-agonist, d-serine. Although glycine and d-serine act upon the same site there are numerous differences: d-serine is a more potent co-agonist at the NMDAR [5] and endogenous glycine is present at saturating levels whereas d-serine is not [6]. Other differences may also have physiological relevance. For example, evidence has been presented that glycine might act as an extra-synaptic NMDAR co-agonist, whilst d-serine may work within the synapse [7]. Furthermore, it is highly likely that the two co-agonists will produce different effects depending on the subunit composition and localisation of the NMDAR receptor complexes across different brain regions [7].
d-Amino acid oxidase (DAO), first discovered over 80 years ago [8], represents a key catabolic route for small neutral amino acids such as d-alanine, d-serine, d-leucine and d-proline [9]. Genetic and pharmacological studies have implicated the enzyme in the etiology of schizophrenia [9]. From a genetic perspective, a DAO knock out mouse has been shown to have increased extra-cellular d-serine levels, glycine site occupancy and enhanced NMDAR function in vivo [10]. Moreover, this mouse strain exhibits some protection against behaviours induced by agents thought to induce psychotic states, such as PCP. Whilst not optimised for this mechanism, a number of therapeutic agents have been shown to inhibit DAO, albeit relatively weakly. For example, sodium benzoate is probably the most structurally simple DAO inhibitor, is widely used as a food additive and forms a component of two drugs with sodium phenyl acetate (Ucephan and Ammonul) [11]. Sodium benzoate has been shown to have a benign safety profile and has recently been demonstrated to have some efficacy in small clinical trials for schizophrenia [12] (adjunct therapy) and Alzheimer’s disease [13] with a further Phase II study being planned [14]. Likewise, some other pharmaceuticals have been shown to display weak inhibitory activity towards DAO. For example, Acyclovir, the antiviral drug, has been shown to be a slow-binding inhibitor [15] and the antipsychotics blonanserin [16] (IC50 = 5.3 μM), risperidone [16] (IC50 = 4.7 μM) and chlorpromazine (IC50 = 11.6 μM) [17, 18] have been shown to have inhibitory activity towards DAO.
A number of potent and selective DAO inhibitors have been developed by various pharmaceutical companies and these have been reviewed recently [19]. Of note, both Merck [20] and Sepracor [21, 22] developed the same heterocyclic carboxylic acid (4H-furo[3,2-b]pyrrole-5-carboxylic acid), with the latter company advancing it to Phase I clinical trials (as SEP-227900) before discontinuing its development [23]. During the time that many of these discoveries were published, we [24] and scientists at Astellas [25, 26] were working on a series of 2-hydroxypyridazonones as DAO inhibitors which are less acidic and therefore have improved brain penetration over formal carboxylic acids.
From the extensive work described above it is clear that DAO-mediated regulation of (central) amino acids is an area of interest with potential in treating disease. Although direct mediation of NMDA receptors has not been shown, there are several markers that can be used to show in vivo/ex vivo inhibition of DAO. These include changes in peripheral and central (cerebellar) concentrations of d and l-serine as well as % enzyme occupancy (%EO). Sodium benzoate is a weak inhibitor of the DAO enzyme [27,28,29] with a number of other potential modes of action [30,31,32,33] and is now being investigated in clinical trials. To understand better the in vitro effects of sodium benzoate we have profiled its effects on the inhibition of DAO and compared these activities with those of a potent selective DAO inhibitor from an in house series, PGM030756.
Materials and Methods
Sodium benzoate was purchased from Sigma Aldrich in the UK (Cat No. 71295 Lot BCBH8216V). PGM030756 and PGM019260 were prepared in the laboratories at Takeda Cambridge Ltd according to the procedures described in the Supplementary Information.

Human DAO Assays
The functional activity of compounds inhibiting the DAO enzyme was determined by measuring the production of H2O2 using the Amplex® Red (Invitrogen) detection method [34]. The changes in fluorescence were monitored using a fluorescence plate reader (Envision, Perkin Elmer). DAO activity was detected upon addition of d-serine at a concentration equivalent to its Km (1.2 mM, in-house data) and suppression of this response was observed with the application of inhibitor compounds. Detailed protocols for the assay and generation of the DAO enzyme and cells can be found in the Supplementary Information.
Structural Biology
The recombinant, untagged, human DAO [hDAO (residues 1-347)] was cloned into thepET21a vector and recombinant BL21(DE3) E. coli were generated to express the protein. Large scale production of recombinant protein was carried out in 10 l of BL21(DE3) E. coli cells utilizing IPTG for induction. The protein was isolated and purified as previously described [35] with the addition of 200 µM sodium benzoate being present in all buffers. The monomeric peak from the final size exclusion step was pooled and the protein concentrated to 5 mg/ml for crystallization in a buffer consisting of 0.1 M Tris pH 8.0, 5% glycerol, and 200 µM sodium benzoate. Crystals suitable for data collection were grown at 277 K in hanging drops over a reservoir containing 0.9 M succinate pH 7.0, 0.1 M Tris pH 8.5, 2 µM sodium benzoate by mixing protein and reservoir in a 1:1 ratio. Yellow crystals with benzoate bound in the active site appeared over 1–2 days and were subsequently transferred to soak drops containing the reservoir solution, without sodium benzoate, and with the addition of 5 mM compound. The crystals were left to incubate for 24 h over a reservoir with the same contents as the soak drop. Immediately prior to snap freezing in liquid nitrogen, the crystals were passed through a cryo-protecting soak drop containing the same ingredients as the soak drop with the addition of 25% ethylene glycol. X-ray diffraction data sets were collected at the ALS beamline 5.0.3 on an ADSC Q315R detector from single cryogenically protected crystals. hDAO crystals belong to the orthorhombic space group P21212, and contain two enzyme molecules in the asymmetric unit. The data was reduced by the HKL2000 software package [36]. Structures were determined by the molecular replacement method using MOLREP [37] of the CCP4 program suite. Multiple cycles of model building with XtalView [38] or COOT [39] and refinement with REFMAC [40] were performed to improve model quality. The coordinates and structure factors have been deposited in ProteinData Bank with accession code 2DU8.
Animals
Male C57BL/6J mice weighing 20–30 g were used. Studies were either run at Takeda Cambridge Ltd (animals purchased from Charles River Laboratories) or at Suven Life Sciences Hyderabad, India [41] (animals purchased from Vivo Biotech Ltd). Animals were housed in groups of four or five per cage with food and water available ad libitum. All procedures were performed in accordance with the Animals (Scientific Procedures) Act 1986.
Compounds
Sodium benzoate was dissolved in 0.9% Saline and administered intraperitoneally (i.p.) at 100, 300 or 1000 mg/kg in a dose volume of 10 ml/kg. PGM030756 was suspended in 1% Tween 80 in 0.5% methylcellulose and administered orally (p.o.) at 1, 3 and 10 mg/kg in a dose volume of 10 ml/kg. PGM019260 was dissolved in 10% DMSO 90% HPβCD and dosed at 60 μg/kg intravenously (i.v.) in a dose volume of 5 ml/kg.
d-Serine Measurement in Brain and Plasma
Mice were administered compound and were sacrificed by decapitation at 2, 6 or 10 h post dose. Blood samples were collected, brain was removed and cerebellum dissected on ice. Plasma and tissue samples were frozen on dry ice and stored at −80 °C until analysis using LC-MS/MS. Samples were sent to Sumika Chemical Analysis Service Ltd (Japan) [42] for analysis of d-serine using LC-MS/MS.
In Vivo Enzyme Occupancy
PGM019260, was used as a tracer compound to measure enzyme occupancy of DAO. The tracer compound was administered via the tail vein 2, 4 or 8 h after dosing of test compounds. Mice were sacrificed by decapitation 20 min after tracer administration. Trunk blood was collected for compound analysis, brain removed and cerebral cortex and cerebellum dissected on ice. Plasma and tissue samples were frozen on dry ice and stored at -80 °C. Compound levels were quantified by LC-MS/MS.
Enzyme Occupancy Calculation
DAO enzyme occupancy was measured using the ratio method, where the ratio of total binding to the nonspecific binding of the tracer was generated. The cerebellum represents the area of high enzyme density and hence total binding and the forebrain an area of low enzyme density and hence non-specific binding.
Ratiot is the ratio of tracer concentration in the cerebellum to the forebrain in animals pre-treated with test compound. Ratioc is the mean ratio of tracer concentrations in cerebellum to the forebrain in vehicle treated animals.
Statistics
Data are presented as mean ± standard deviation (S.D.) Statistical differences were identified using analysis of variance (ANOVA) followed by Dunnett’s post-hoc test. GraphPad Prism (San Diego, California) was used for statistical analysis.
Compound Analysis
Trunk blood was collected from mice undergoing enzyme occupancy studies. Plasma was collected and samples were analysed by HPLC for compound levels.
Results
Sodium Benzoate
In Vitro Potency of Sodium Benzoate
The in vitro potency of sodium benzoate has been described in the literature on several occasions previously with Kd/Ki measured in the micromolar (Ki = 7 μM [27]) or even millimolar concentration range (Kd = 18.8 mM [28]). In this study we found it to have no significant effects even at the highest concentrations tested (10 μM) in both human and mouse assays, therefore the IC50 is considered to be >10 μM.
Structural Biology
The X-ray crystal structure of the complex between DAO and sodium benzoate has already been published [27, 29] and this ligand could be displaced by either PGM030756 or PGM019260 to produce complexes between the heterocycles and the enzymes (Fig. 1). In each case the interactions were similar in that the cyclic hydroxyamide binds to the Arg283 (mimicking the carboxylic acid interaction of sodium benzoate) and the (hetero-) aromatic rings likely form a π-stacking interaction with the co-factor, FAD.
Effect of Sodium Benzoate on d-serine
Plasma d-serine levels were initially decreased following 1000 mg/kg sodium benzoate administration. However, at 6 h post dose the d-serine levels were significantly increased compared to vehicle and this increase was maintained at 10 h post dose (Fig. 2).
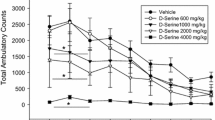
Administration of sodium benzoate dose dependently increased cerebellar d-serine levels 2 h after administration at 300 and 1000 mg/kg (Fig. 3). The dose of 100 mg/kg had no effect on d-serine levels at the time points examined. Due to the lack of effect on d-serine increases with 100 mg/kg sodium benzoate, this dose was not profiled further. The d-serine increase seen after the 300 mg/kg dose had returned to baseline after 6 h and the increase seen after the 1000 mg/kg dose had returned to baseline after 10 h. Cerebellar l-serine levels were unchanged following sodium benzoate administration however plasma levels were significantly decreased, a result also observed by Javitt [43], and Hashimoto [44] (Table 1).
In Vivo DAO Enzyme Occupancy of Sodium Benzoate
Pre-treatment of sodium benzoate caused a dose dependent decrease in tracer (PGM019260) concentrations in the cerebellum compared to vehicle treated animals (Fig. 4). At 2 h post dose of 1000 mg/kg sodium benzoate, the tracer concentrations in the cerebellum were reduced to non-specific levels equating to an enzyme occupancy value of ≥95% sodium benzoate. This was sustained until 4 h post dose and fell to below 40% at 8 h post dose. The lower dose of 300 mg/kg i.p. reached 70% enzyme occupancy 2 h post dose and declined steadily, returning to baseline 8 h post dose.
Plasma Exposure of Sodium Benzoate in Mice
These enzyme occupancy data are consistent with the plasma exposure of sodium benzoate (Fig. 5). At 300 mg/kg i.p. relatively low plasma levels are seen at 2 h and by 4 h the levels are below levels of quantification. In contrast, at 1000 mg/kg i.p. high plasma levels are seen at 2 h and although there is significant decrease by 4 h there is still a substantial plasma concentration which likely explains the retained enzyme occupancy shown in Fig. 4.
In Vitro Potency of PGM030756
PGM030756 and PGM019260 show highly potent DAO inhibition in human enzyme and cell-based assays and also across species in a mouse cell-based assay (Table 2).
Effect of PGM030756 on d-Serine
PGM030756 (3, 10, 30 mg/kg p.o.) dose dependently increased cerebellar d-serine levels 2 h post dose and these increases were maintained up to 10 h post dose of 10 and 30 mg/kg with peak increase at 6 h post dose (Fig. 6).
Plasma Exposure of PGM030756 in Mice
PGM030756 shows excellent plasma exposure following oral dosing (Fig. 7) with peak recorded plasma levels at over 9000 ng/ml. Therefore, based on these differences and those from the in vitro potency, much lower doses of PGM030756 were studied following oral administration.
PGM030756 dosed at 10 mg/kg p.o. reached >80% enzyme occupancy 2 h post administration, which was sustained for at least 4 h decreasing to 50% after 8 h post dose (Fig. 8). The lower doses of 3 and 1 mg/kg reached 70 and 40% respectively after 2 h post dose and had returned to baseline by 8 h post dose.
In Vivo DAO Enzyme Occupancy of PGM030756
Discussion
Inhibition of DAO leads to an increase in the levels of d-serine; a co-agonist of the NMDA receptor [45] as well as a direct agonist of the GluRδ2 receptor [46]. It has been postulated that an increase in this amino acid in systems with a dysregulation; e.g. schizophrenia, may lead to an amelioration of disease symptoms. To understand the pre-clinical and therefore clinical effects of DAO inhibitors, it is important to characterise their capacity to engage with the target in vivo. This supporting pre-clinical data may facilitate the development of biomarkers that may support clinical assessment.
Such strategies have been described in the scientific literature, for example in Astra Zeneca’s “5Rs” [47] and “Pfizer’s three pillars” [48] which put forward the reasoning that evidence for target engagement linked to biological effect are required to permit the effective evaluation of compounds in clinical development.
PGM030756 is a very potent inhibitor of DAO (IC50 = 9.6, 10 and 4.6 nM respectively in human enzyme, human recombinant cell and mouse recombinant cell assays), whereas sodium benzoate is a much weaker ligand with Kd/Ki’s measured in the micromolar (Ki = 7 μM [27]) or even millimolar concentration range (Kd = 18.8 mM [28]). In our hands, sodium benzoate showed an IC50 of >10 μM in human enzyme, human recombinant cell and mouse recombinant cell assays. However our structural biology analysis, in support of the literature [27, 29], demonstrates that sodium benzoate binds to DAO and we show that PGM030756 competes for the same binding site. Also important is the selectivity of the compounds. Both were tested across a wide range of assays at 10 μM with there being a weak interaction between PGM030756 and 5-LO and no significant interactions of sodium benzoate even at 10 μM. Whilst these data allow us to confirm that PGM030756 has a wide selectivity window (≥723-fold) it can only be stated that sodium benzoate has no other activities (from those assayed) at which it is likely to be more potent than against DAO.
The enzyme occupancy work has shown that both sodium benzoate and PGM030756 inhibit DAO, but with differing potencies. Although we initially started to profile sodium benzoate at doses of 100, 300 and 1000 mg/kg, it was clear that the 100 mg/kg dose caused no detectable changes in d-serine in the cerebellum and so was not profiled further. Also, due to the low potency and the poor oral bioavailability of sodium benzoate, it was administered i.p. to ensure sufficient occupancy at the target site could be achieved. This was not necessary for PGM030756 due to its increased potency and improved bioavailability and so this compound was dosed p.o. A dose of 1000 mg/kg i.p. of sodium benzoate resulted in close to 100% occupancy in the cerebellum at 2 h, whereas a similar level of occupancy was reached with a dose of 10 mg/kg of PGM030756 p.o. Plasma concentrations of sodium benzoate show that occupancy is retained in the cerebellum for considerably longer than the compound can be detected in the plasma. This is also seen for PGM030756 and would suggest that both of these DAO inhibitors are retained in tissues containing the enzyme.
Our data support the hypothesis of the Pfizer group [49] in that we observe significant increases in plasma and cerebellar d-serine with sodium benzoate (Fig. 3) following a hysteresis and these effects are seen at the middle dose (300 mg/kg i.p.) but are most prominent at highest dose (1000 mg/kg i.p.) and at the 6 h time point. These increases are supported by DAO enzyme occupancy data which suggest that at 1000 mg/kg i.p. near complete occupancy is achieved for a significant length of time (>4 h) and at the 300 mg/kg dose the highest occupancy recorded is only 70% at 2 h and reduces rapidly. The greatest increases are seen in the cerebellum at 1000 mg/kg 6 h post dose where the levels of d-serine change approximately fourfold.
As discussed earlier, PGM030756 is a much more potent inhibitor of the DAO enzyme with greater plasma exposure and so was dosed orally at considerably lower doses. For this compound, the most prominent increases in cerebellar d-serine are seen at 10 and 30 mg/kg p.o., at the 6 h time point (Fig. 6) and this is supported by the enzyme occupancy at these doses. Once again, at these doses enzyme occupancy of 70–90% is observed initially and occupancy is maintained for a prolonged period of time leading to extensive suppression of the DAO enzyme’s ability to clear d-serine from the synapse. The greatest increases in d-serine (approximately threefold) occur in the cerebellum at the highest does (30 mg/kg) at 6 h post-dose.
Although maximum occupancy of both compounds is seen after 2 h, a hysteresis effect is seen on the d-serine response. From the data published here and our in-house behavioural data (unpublished), we believe that it is the increases in d-serine which drive the behavioural effects seen with DAO inhibitors. The largest d-serine increase in our data set occurs at 6 h in the cerebellum; 4 h after 100% occupancy is detected. This delay may be due to the time required for serine racemase to synthesise more d-serine from l-serine, although we have not tested this. Indeed, Strick [49] has not only demonstrated this hysteresis but also developed a pk/pd model to explain it. Unpublished in-house data has also shown that d-serine changes in brain regions other than the cerebellum are negligible and this may be due to lack of expression of DAO in regions other than the hindbrain in the rodent [50, 51]. The hysteresis effect and specific expression pattern of DAO may be what has led to some discrepancies in the published literature between the positive behavioural effects of sodium benzoate and its ability to increase d-serine levels; something that we believe is vital in a DAO inhibitor. Sodium benzoate (1000 mg/kg) has been shown to reverse PCP-induced pre-pulse inhibition and hyperlocomotion after 1 h [52] but no corresponding d-serine increases could be detected. From our data, we predict that it is likely that 100% EO was achieved in the cerebellum at this dose but that d-serine increases in the plasma could not be detected and in fact this is what was seen in the study. We also postulate that increases in d-serine in the brain are only detectable in the cerebellum and only after a significant period of time has passed that allows d-serine accumulation. Sodium benzoate at lower doses (400 mg/kg) has also been shown to significantly reduce PCP-induced hyperlocomotion when in combination with d-serine (600 mg/kg) [43]. Although this dose of sodium benzoate does not achieve 100 EO% and from our data is predicted to not cause an increase in d-serine, it is likely that the combination of sodium benzoate and d-serine together leads to an overall efficacious effect. Again, d-serine levels appear not to have been elevated although this may be due to the fact that whole brain homogenates were used, so diluting out the effect in the hindbrain. However, as Javitt et al. [43] suggest, this does not rule out the possibility that sodium benzoate reverses PCP-induced behaviours through some other mechanism of action.
Sodium benzoate is not the only DAO inhibitor to have been investigated in the literature. As previously mentioned, a number of potent and selective DAO inhibitors have been developed by various other pharmaceutical companies. Researchers from Johns Hopkins university published data on 3 of their own tool compounds showing that they inhibited DAO peripherally [53]. Interestingly Rojas et al. [53] detected an increase in plasma d-serine in mice but this could not be detected in either baboons or dogs. The authors commented that this increase in d-serine after DAO inhibition may be a phenomenon that is restricted to rodents and therefore is of no interest when it comes to treating human conditions. However, our in-house experience (unpublished) suggests that this lack of efficacy across species may be something that is specific to either these molecules or the method of d-serine detection used and believe DAO to be a valid target for the treatment of diseases involving irregular NMDA function.
Summary
We provide further support to the observation that sodium benzoate acts as a weak DAO inhibitor and that it is likely that its behavioural effects are driven through d-serine increases. We have compared its profile with that of a more potent DAO inhibitor, PGM030756 which shows target engagement at low doses (10–30 mg/kg p.o.) whilst sodium benzoate needs to be dosed at 300 or even 1000 mg/kg i.p. to achieve similar effects. According to the known hysteresis mechanism, peak increases in cerebellar d-serine can be measured approximately 6 h after administration of both compounds.
Our data and methods may be useful in understanding the effects of sodium benzoate that have been seen in clinical trials of schizophrenia and Alzheimer’s disease and to support the clinical assessment of other DAO inhibitors, such as PGM030756, which demonstrate good enzyme occupancy and d-serine increases following administration of low oral doses.
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
References
Coyle JT (2012) NMDA Receptor and schizophrenia: a brief history. Schizophr Bull 38:920–926
Choi DW, Koh JY, Peters S (1988) Pharmacology of glutamate neurotoxicity in cortical cell culture: attenuation by NMDA antagonists. J Neurosci 8:185–196
Harvey RJ, Yee BK (2013) Glycine transporters as novel therapeutic targets in schizophrenia, alcohol dependence and pain. Nat Rev Drug Disc 12:866–885
Roche press release. http://www.roche.com/media/store/releases/med-cor-2014-01-21.htm
Matsui T, Sekiguchi M, Hashimoto A, Tomita U, Nishikawa T, Wada K (1995) Functional comparison of D-serine and glycine in rodents: the effect on cloned NMDA receptors and the extracellular concentration. J Neurochem 65:454–458
Paoletti P, Bellone C, Zhou Q (2013) NMDA receptor subunit diversity: impact on receptor properties, synaptic plasticity and disease. Nat Rev Neurosci 14:383–400
Papouin T, Ladépêche L, Ruel J, Sacchi S, Labasque M, Hanini M, Groc L, Pollegioni L, Mothet JP, Oliet SH (2012) Synaptic and extrasynaptic NMDA receptors are gated by different endogenous coagonists. Cell 150:633–646
Krebs HA (1935) Metabolism of amino acids: deamination of amino acids. Biochem J 29:1620–1644
Verall L, Burnett PW, Betts JF, Harrison PJ (2010) The neurobiology of D-amino acid oxidase its involvement in schizophrenia. Mol Psych 15:122–137
Almond SL, Fradley RL, Armstrong EJ, Heavens RB, Rutter AR, Newman RJ, Chiu CS, Konno R, Hutson PH, Brandon NJ (2006) Behavioral and biochemical characterization of a mutant mouse strain lacking D-amino acid oxidase activity and its implications for schizophrenia. Mol Cell Neurosci 32:324–334
Misel ML, Gish RG, Patton H, Mendler M (2013) Sodium benzoate for the treatment of hepatic encephalopathy. Gastroenterol Hepatol 9:219–227
Lane H-Y, Lin C-H, Green MF, Helleman G, Huang C-C, Chen P-W, Tun R, Chang Y-C, Tsai GE (2013) Add on treatment of benzoate for schizophrenia. A randomized, double blind, placebo-controlled trial of D-amino acid oxidase inhibitor. JAMA Psychiatry 70:1267–1275
Lin C-H, Chen P-K, Chang Y-C, Chuo L-J, Chen Y-S, Tsai GE, Lane H-Y (2014) Benzoate, a D-amino acid oxidase inhibitor, for the treatment of early phase Alzheimer’s disease: a randomised, double blind, placebo controlled trial. Biol Psychiatry 75:678–685
See https://clinicaltrials.gov/ct2/show/NCT01908192?term=benzoate&rank=2
Katane M, Matsuda S, Saitoh Y, Sekine M, Furuchi T, Koyama N, Nakagome I, Tomoda H, Hirono S (2013) The antiviral drug Acyclovir is a slow-binding inhibitor of D-amino acid oxidase. Biochemistry 52:5665–5674
Shishikura M, Hakariya H, Iwasa S, Yoshio T, Ichiba H, Yorita K, Fukui K Fukushima T (2014) Evaluation of human D-amino acid oxidase inhibition by antipsychotic drugs in vitro. Biosci Trends 8:149–154
Yagi K, Nagatsu T, Ozawa T (1956) Inhibitory action of chlorpromazine on the oxidation of D-amino acid in the diencephalon part of the brain. Nature 177:891–892
Iwana S, Kawazoe T, Park HK, Tsuchiya K, Ono K, Yorita K, Sakai T, Kusumi T, Fukui K (2008) Chlorpromazine oligomer is potentially active substance that inhibits D-amino acid oxidase, product of susceptibility gene for schizophrenia. J Enz Inh Med Chem 23:901–911
Sacchi S, Rosini E, Pollegioni L, Molla G (2013) D-Amino acid oxidase inhibitors as a novel class of drugs for schizophrenia therapy. Curr Pharm Des 19:2499–2511
Sparey T, Abeywickrema P, Almond S, Brandon N, Byrne N, Campbell A, Hutson PH, Jacobson M, Jones B, Munshi S, Pascarella D, Pike A, Prasad GS, Sachs N, Sakatis M, Sardana V, Venkatraman S, Young MB (2008) The discovery of fused pyrrole carboxylic acids as novel, potent D-amino acid oxidase (DAO) inhibitors. Bioorg Med Chem Letts 18:3386–3391
Hopkins SC, Campbell UC, Heffernan ML, Spear KL, Jeggo RD, Spanswick DC, Varney MA, Large TH (2013) Effect of D-amino acid oxidase inhibition on memory performance and long-term potentiation in vivo. Pharmacol Res Pers 1:1–9
Dorsey JM, Heffernan MR, Fang QK, Foglesong RJ, Hopkins SC, Ogbu CO, Soukri M, Spear K Sepracor Inc. (2008) Fused Heterocycles US20080004328
Knezevic NN, Cicmil N, Knezevic I, Candido KD (2015) Discontinued neuropathic pain therapy between 2009–2015. Expert Opin Investig Drugs 24:1631–1646
Farnaby W, Fieldhouse C, Hazel K, Kerr C, Kinsella N, Livermore D, Merchant K, Miller D, Pyridazinone compounds and their use as DAO inhibitors WO2013/027000; WO2014/096757
Hondo T, Warizaya M, Niimi T, Namatame I, Yamaguchi T, Nakanishi K, Hamajima T, Harada K, Sakashita H, Matsumoto Y, Orita M, Takeuchi M (2013) 4-Hydroxypyridazin-3(2H)-one derivatives as novel D-amino acid oxidase inhibitors. J Med Chem 56:3582–3592
Hondo T, Warizaya M, Niimi T, Namatame I, Nakanishi K, Harada K, Dihydroxy aromatic heterocyclic compound WO2013/073577
Kawazoe T, Tsuge H, Pilone MS, Fukui K (2006) Crystal structure of human D-amino acid oxidase: context-dependent variability of the backbone conformation of the VAAGL hydrophobic stretch located at the si-face of the Flavin ring. Protein Sci 15:2708–2717
Pollegioni L, Piubelli L, Sacchi S, Pilone MS, Molla G (2007) Physiological functions of D-amino acid oxidases: from yeast to humans. Cell Mol Life Sci 64:1373–1394
Sodium benzoate DAO complex PDB ID: 2DU8
Kundu M, Mondal S, Roy A, Martinson JL, Pahan K (2016) Sodium benzoate, a food additive and metabolite of cinnamon, enriches regulatory T-cells via STAT6-mediated upregulation of TGF-β. J Immunol 197(8):3099–3110
Modi KK, Jana M, Mondal S, Pahan K (2015) Sodium benzoate, a metabolite of cinnamon and a food additive, upregulates ciliary neurotrophic factor in astrocytes and oligodendrocytes. Neurochem Res 40:2333–2347
Brahmachari S, Pahan K (2007) Sodium benzoate, a food additive and metabolite of cinnamon, modifies T-cells at multiple steps and inhibits adoptive transfer of experimental allergic encephalomyelitis. J Immunol 179:275–283
Rezaei N, Amirghofran Z, Nikseresht A, Ashjazade N, Zoghi S, Tahvili S, Kamali-Servestani E (2016) In vitro effects of sodium benzoate on Th1/Th2 deviation in patients with multiple sclerosis. Immunol Invest 45:679–691
Brandish PE, Chiu CS, Schneeweis J, Brandon NJ, Leech CL, Kornienko O, Scolnick EM, Strulovici B, Zheng W (2006) A cell-based ultra-high-throughput screening assay for identifying inhibitors of D-amino acid oxidase. J Biomol Screen 11:481–487
Molla G, Sacchi S, Bernasconi M, Pilone MS, Fukui K, Pollegioni L (2006) Characterization of human D-amino acid oxidase. FEBS Lett 580:2358–2364
Otwinowski Z, Minor W (1997) Processing of X-ray diffraction data collected in oscillation mode. Methods Enzymol 276:307
Vagin A, Teplyakov A (1997) MOLREP: an automated program for molecular replacement. J Appl Cryst 30:1022–1025
McRee DE (1999) XtalView/Xfit—A versatile program for manipulating atomic coordinates and electron density. J Struct Biol 125:156–165
Emsley P, Cowtan K (2004) Coot: model-building tools for molecular graphics. Acta Cryst D 60:2126–2132
Winn MD, Murshudov GN, Papiz MZ (2003) Macromolecular TLS refinement in REFMAC at moderate resolutions. Methods Enzymol 374:300–321
Suven Life Sciences Ltd, Hyderabad, India. Contact: gopi@suven.com
Sumika Chemical Analysis Services, Ltd, Osaka, Japan. Contact: hashimoto@scas.co.jp
Sershen H, Hashim A, Dunlop DS, Suckow RF, Cooper TB, Javitt DC (2016) Modulating NMDA receptor function with D-amino acid oxidase inhibitors: understanding functional activity in PCP-treated mouse model. Neurochem Res 41:398–408
Matsuura A, Fujita Y, Iyo M, Hashimoto K (2015) Effects of sodium benzoate on pre-pulse inhibition deficits ad hyperlocomotion in mice after administration of phencyclidine. Acta Neuropsychiatrica 27:159–167
Zhu S, Paoletti P (2015) Allosteric modulators of NMDA receptors: multiple sites and mechanisms. Curr Op Pharm 20:14–23
Yu SY, Wu DC, Liu L, Ge Y, Wang YT (2008) Role of AMPA receptor trafficking in through the δ 2 glutamate receptor. Nat Neurosci 14(5):603–611
Cook D, Brown D, Alexander R, March R, Morgan P, Satterthwaite G, Pangalos MN (2014) Lessons learned from the fate of AstraZeneca’s drug pipeline: a five dimensional framework. Nat Rev Drug Discovery 13:419–431
Morgan P, van der Graaf P, Arrowsmith J, Feltner DE, Drummond KS, Wegner CD, Street SD (2012) Can the flow of medicines be improved? Fundamental pharmacokinetic and pharmacological principles towards improving phase II survival. Drug Disc Today 17:419–424
Strick CA, Li C, Scott L, Harvey B, Hajós M, Steyn SJ, Piotrowski MA, James LC, Downs JT, Rago B, Becker SL, El-Kattan A, Xu Y, Ganong AH, Tingley FD III, Ramirez AD, Seymour PA, Guanowsky V, Majchrzak MJ, Fox CB, Schmidt CJ, Duplantier AJ (2011) Modulation of NMDA receptor function by inhibition of D-amino acid oxidase in rodent brain. Neuropharmacology 61:1001–1015
Horiike K, Tojo H, Arai R, Yamano T, Nozaki M, Maeda T (1987) Localisation of D-amino acid oxidase in Bergman glial cells and astrocytes of rat cerebellum. Brain Res Bull 19:587–596
Horiike K, Tojo H, Arai R, Nozaki M, Maeda T (1994) D-Amino acid oxidase is confined to the lower brain stem and cerebellum in rat brain: regional differences in astrocytes. Brain Res 652:297–303
Matsuura A, Fujita Y, Iyo M, Hashimoto K (2015) Effects of sodium benzoate on pre-pulse inhibition deficits and hyperlocomtion in mice after administration of phencyclidine. Acta Neuropsychiatrica 27(3):159–167
Rojas C, Alt J, Ator N, Thomas AG, Wu Y, Hin N, Wozniak K, Ferraris D, Rais R, Tsukamoto T, Slusher BS (2016) D-amino-acid oxidase inhibition increases D-serine plasma levels in mouse but not in monkey or dog. Neuropsychopharmacology 41:1610–1619
Acknowledgements
The authors would like to gratefully thank Sarah Almond, Shyam Bechar, Richard Newman, Kamal Lalgi, Dhruval Patel, Stuart Stafford and John Robinson (Takeda Cambridge Ltd), Sean Gay (Takeda California,) and Ranjev Savopoulos (Assay Advantage Ltd). Whilst not contributing directly to the data presented within this paper each of those named above played important roles in identifying either the compounds synthesised or the methods by which to test them.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Howley, E., Bestwick, M., Fradley, R. et al. Assessment of the Target Engagement and d-Serine Biomarker Profiles of the d-Amino Acid Oxidase Inhibitors Sodium Benzoate and PGM030756. Neurochem Res 42, 3279–3288 (2017). https://doi.org/10.1007/s11064-017-2367-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-017-2367-9