Abstract
Diffuse infiltrative low grade gliomas (LGG) account for approximately 15 % of all gliomas. The prognosis of LGG differs between high-risk and low-risk patients notwithstanding varying definitions of what constitutes a high-risk patient. Maximal safe resection optimally is the initial treatment. Surgery that achieves a large volume resection improves both progression-free and overall survival. Based on results of three randomized clinical trials (RCT), radiotherapy (RT) may be deferred in patients with low-risk LGG (defined as age <40 years and having undergone a complete resection), although combined chemoradiotherapy has never been prospectively evaluated in the low-risk population. The recent RTOG 9802 RCT established a new standard of care in high-risk patients (defined as age >40 years or incomplete resection) by demonstrating a nearly twofold improvement in overall survival with the addition of PCV (procarbazine, CCNU, vincristine) chemotherapy following RT as compared to RT alone. Chemotherapy alone as a treatment of LGG may result in less toxicity than RT; however, this has only been prospectively studied once (EORTC 22033) in high-risk patients. A challenge remains to define when an aggressive treatment improves survival without impacting quality of life (QoL) or neurocognitive function and when an effective treatment can be delayed in order to preserve QoL without impacting survival. Current WHO histopathological classification is poorly predictive of outcome in patients with LGG. The integration of molecular biomarkers with histology will lead to an improved classification that more accurately reflects underlying tumor biology, prognosis, and hopefully best therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diffuse infiltrative low grade gliomas (LGG) account for approximately 5 % of all primary brain tumors and approximately 15 % of all gliomas [1•, 2]. Most LGG occur in patients 30 to 40 years of age [1•, 3]. According to the World Health Organization (WHO), diffuse infiltrative LGG (WHO grade II gliomas) include astrocytomas, oligodendrogliomas, and mixed oligoastrocytomas; all share a propensity to malignant transformation [3]. The majority of patients with LGG present with seizures that are often chronic and medication refractory. Following presentation with seizures or a focal neurological deficit, brain MRI demonstrates an intraparenchymal mass lesion that is non-contrast enhancing (only 15–20 % of LGG manifest contrast uptake) and most conspicuous with T2W or FLAIR MRI sequences. Surgery that achieves a large volume resection (>70 % tumor resection) improves progression-free (PFS) and overall survival (OS) [4–6]. The recent Radiation Therapy Treatment Group (RTOG) 9802 randomized clinical trial (RCT) established a new standard of care in high-risk patients by demonstrating an improvement in OS by the addition of PCV chemotherapy (procarbazine, lomustine {CCNU}, and vincristine) following RT as compared to RT alone. Based on results of three randomized clinical trials (RCT), radiotherapy (RT) may be deferred in patients with low-risk LGG (defined as age <40 years and having undergone a complete resection), although these trials preceded the definition of low- and high-risk LGG (Table 1). Another transformative finding has been the molecular characterization of both LGG and anaplastic gliomas (WHO grade III gliomas). The emergence of molecular biomarkers in LGG that are both prognostic and predictive will need to be integrated with morphology-based pathology and likely will fundamentally change both classification and management of LGG. Increasingly recognized as an important and clinically relevant outcome measure in patients with all grades of gliomas is the impact of treatment on quality of life (QoL) and neurocognitive function (NCF). These measures have been relatively unstudied in LGG and are particularly relevant given the long survival of patients with LGG.
Surgery
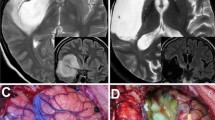
When possible, maximal safe resection is the first therapy to consider in treating patients with LGG [7••]. The objective of surgery is to confirm pathology of the lesion defied by the MRI and categorize as to histological and molecular classification. Resection may as well improve neurological function and decrease seizures, the most common symptom of LGG [7••, 8, 9].
There has been no RCT that assessed the extent of resection (EOR) in LGG impact on survival; however, numerous retrospective studies suggest improved survival in patients having undergone large volume resections [6]. Importantly, EOR as reported by the operating neurosurgeon without confirmation by imaging has not been found as prognostic [10]. Furthermore, large volume resection has been reported to improve time to malignant transformation as well as PFS and OS [1•, 6, 11]. A study conducted in Norway compared two differing treatment approaches in patients with LGG at two institutions: biopsy and observation in one institution and early maximal resection in the second institution [12]. Median OS was 5.6 years in the first institution versus 9.7 years in the second institution favoring early surgery in the management of LGG. A review of 17 retrospective studies analyzed the impact of the EOR on PFS and OS in LGG. A benefit in OS was observed in ten non-volumetric studies and in all four studies with volumetric determinations, whereas no benefit was observed in three non-volumetric studies [6]. In a cohort of 1509 patients with LGG, the EOR and post-surgical residual tumor volume were independent prognostic factors for PFS and OS [9]. In another cohort study of 216 patients, resection of >90 % of the tumor led to an improved 8-year OS rate compared to a tumor resection <60 % (91 vs. 60 %) [11].
Radiotherapy
Low dose of RT (45 Gy) was compared to high-dose of RT (59.4 Gy) in LGG after biopsy or surgery in the randomized phase III trial EORTC 22844 (Table 1). No difference in OS was observed; however, the quality of life (QOL) was more negatively impacted in the high-dose RT group [13]. These results were confirmed in another randomized phase III trial by the North Central Cancer Treatment Group (NCCTG) /RTOG/Eastern Cooperative Oncology Group (ECOG) study comparing low-dose RT (50.4 Gy) versus high dose (64.8 Gy) in adult LGG [14]. Additionally, a significant deterioration of mini-mental status score (MMSE) was observed in patients without tumor progression in the high-dose arm [15]. Thus, low-dose RT has been shown to confer similar PFS and OS outcomes as high-dose RT but with less toxicity. The EORTC 22845 randomized phase III trial compared early RT (54 Gy) versus delayed RT, i.e., administered at time of tumor progression. Median PFS was significantly better in the group with early RT (5.3 vs. 3.4 years) whereas OS was similar between both groups (7.4 vs. 7.2 years). Differences in neurocognition however were not studied [16]. Patients enrolled in the RCT RTOG 9802 were divided into two groups according to risk of disease recurrence. A total of 111 patients were included in the favorable group defined as <40 years of age and having undergone an image-verified complete resection and were observed with no further adjuvant therapy. In this group, PFS at 5 years was 48 % and a better PFS was correlated with a preoperative tumor diameter <4 cm, an oligodendroglioma subtype, and residual tumor <1 cm on MRI [17].
Chemotherapy
Administering chemotherapy as a first therapy in lieu of RT is attractive considering the delayed neurocognitive adverse consequences of RT particularly germane in patients with LGG in which OS is measured in years and the volume of brain irradiated is comparatively large [18–20]. Additionally, the efficacy of up-front chemotherapy in LGG has been demonstrated in several retrospective and small phase II studies [21–31].
The randomized phase III EORTC 22033–26033 trial investigated whether dose-dense temozolomide (TMZ) prolongs PFS as compared to RT (50.4 Gy) as primary treatment in high-risk non-1p19q codeleted LGG initially treated with surgery only (Table 1). High-risk was defined in this study as patients >40 years of age, symptomatic, or having evidence of radiographic progression following initial surgery. After a median follow-up of 45.5 months, PFS was similar in both groups (47 months in the RT arm and 40 months in the TMZ arm) albeit the protocol was designed to determine superiority of TMZ relative to RT. The median OS was not reached in the RT arm (74 months in the TMZ arm) implying the results are immature and therefore conclusions regarding effectiveness of a TMZ only initial therapy in high-risk LGG is premature. 1p deletion was a positive prognostic factor in both treatment groups [32]. In a subgroup analysis, PFS was longer in patients with IDH mutation and non-codeleted when treated with RT compared to TMZ [33].
PCV chemotherapy has been used in historically earlier trials in LGG however was replaced with TMZ in most centers and in later trials because of an improved toxicity profile and a perception these alkylating regimens were otherwise similar in efficacy [1•, 19, 34–36]. Notably, similar responses and survival have been documented with both chemotherapies. In patients with LGG treated with PCV, objective responses were observed in 27–80 %. Median PFS is reported as 21–46 months, 1-year PFS as 90 % and median time to maximum tumor size reduction range from 9–40.8 months in patients treated with PCV chemotherapy [21–27]. By comparison, in patients with LGG treated with TMZ, objective responses are observed in 31–61 %, median PFS range from 10.4–28 months, 1-year PFS was 39–70.5 % and median time to maximum tumor size reduction was 12 months [28–30, 37–39].
Whether TMZ and PCV are equi-efficacious is uncertain lacking a head-to-head comparator trial.
The amended design of the randomized phase III CODEL trial will compare three arms of treatment in 1p19q codeleted gliomas and will include both WHO grade II and III gliomas. The study compares RT followed by PCV to RT with concurrent and adjuvant TMZ. A small explorative third arm is treatment with TMZ only (a hypothesis generating substudy). The co-primary endpoints are PFS and neurocognition [35, 40–43]. The results of CODEL will clarify whether TMZ is equivalent to PCV.
Combined Radiotherapy and Chemotherapy
The single arm phase II RTOG 0424 trial evaluated concomitant RT (54 Gy) and TMZ followed by 12 cycles of TMZ in high-risk LGG. High-risk was defined by the presence of three or more risk factors including age ≥40 years, astrocytoma histology, midline involvement by tumor, preoperative tumor diameter of ≥6 cm, or a preoperative neurological deficit. The study met the primary endpoint as after a median follow-up of 4.1 years, the 3-year OS rate was 73.1 %, significantly higher as compared to 54 % in the historical control cohort. The 3-year PFS was 59.2 % [44].
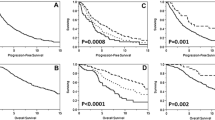
A new standard of care was established in adults with high-risk LGG by the RTOG 9802 trial that compared RT to RT followed by PCV (Table 1). The primary endpoint of the trial was OS. Patients defined as high-risk were >40 years of age or had less than complete resection regardless of age. Patients were randomly assigned to RT alone (54 Gy) or RT followed by 6 cycles of PCV. A total of 251 patients were enrolled. The long-term results were presented after a median follow-up of 11.9 years [45••]. A significant improvement in both PFS and OS was observed in the RT + PCV arm as compared to RT alone (Table 1). Multivariate analysis identified several favorable prognostic factors including treatment with PCV, oligodendroglioma histology, and female gender [45••]. The incidence of grade 3 hematologic toxicity was significantly higher in the RT + PCV arm as expected. The study reported a high level of compliance with treatment allocation for both treatment arms [46], which was higher than in the randomized trials of RT versus RT + PCV in anaplastic gliomas [47, 48]. At progression (73 and 39 %, respectively, in the RT only and RT + PCV arm) patients received salvage treatment that included surgical resection (26 % in the RT only arm, 14 % in the RT + PCV arm), salvage chemotherapy (56 vs. 23 %), and salvage RT (19 vs. 6 %). The study concluded that initial treatment with RT + PCV in patients with high-risk LGG is superior to initial RT alone followed by chemotherapy at progression [19].
Management of Recurrent Disease
No standard therapy has been established for the treatment of recurrent LGG. Therapeutic options include surgery, RT, and chemotherapy. The implementation of these therapies is primarily determined by prior therapy wherein low-risk LGG having been observed initially are treated with re-resection if possible followed by RT. By contrast in patients with high-risk LGG initially treated with RT + PCV, salvage chemotherapy with TMZ would most often be employed. Treatment after failure of alkylator-based chemotherapy (PCV or TMZ) is challenging and a wide divergence of opinion exists as to next best therapy as reflected in the National Comprehensive Cancer Network (NCCN) and European Association of Neuro-Oncology (EANO) guidelines [7••, 49].
Limitations of Current Therapy
Definition of High-Risk LGG
The definition of a high-risk LGG has variously been defined and not consistent across trials. For example, the definition of high-risk LGG used in RTOG 9802 results in the majority of LGG considered as high-risk and consequently treated with RT + PCV [50]. By contrast, an analysis of two RCT conducted by the EORTC concluded three of five risk factors, including an age > 40 years, astrocytoma histology, a tumor diameter > 6 cm, tumor crossing the midline, and the presence of a neurologic deficit before surgery, were necessary to define high-risk glioma and warrant up-front treatment with RT [51]. Furthermore, in the EORTC analysis the EOR was not found as prognostic. The recent EORTC trial, 22033, defined high-risk as patients with either recurrent or symptomatic disease.
The impact of the initial MMSE score, EOR, and 1p19q deletion status in addition to the prognostic factors reported by Pignatti were analyzed in 203 patients from the RCT NCCTG86-72-51 [52]. The median OS according to the prognostic factors defined by Pignatti was 10.8 years in low-risk patients and 3.9 years in the high-risk patients. Multivariate analysis showed that tumor size and MMSE were significantly correlated to OS and that tumor size, astrocytoma histology, and MMSE were significantly correlated with PFS. A tumor size >5 cm, astrocytoma histology, and a MMSE score < 27 led to a worse prognosis. The 1p19q status, available in only 66 patients, was associated with a better OS as well.
Prognostic models for PFS and OS were analyzed in 339 EORTC patients with LGG enrolled in the 22844 and 22845 trials and validated in 450 patients in two other studies (RTOG 9802 and NCCTG 86-72-51) [10]. PFS and OS were both negatively impacted by the presence of neurological deficits at baseline, a short interval (<30 weeks) between symptom onset and diagnosis, astrocytic histology, and tumors with a diameter >5 cm. Contrary to the initial report, age was not identified as a prognosis factor. Additionally, EOR did not influence either PFS or OS. Consequently the definition of high-risk in LGG appears study dependent, non-uniform across studies, and somewhat arbitrary.
Both rapid tumor growth rate (>8 mm/year) as defined by longitudinal imaging, increased cerebral blood volume, and a high-grade glioma-like MRI spectroscopic pattern have all been suggested as poor prognostic factors but have not been validated in prospective clinical trials [53, 54]. A major limitation in all of the abovementioned studies regarding prognostic factors is the absence of molecular data in determining these respective models.
Molecular Biomarkers
A high interobserver variability in classifying LGG is seen with the current WHO histological classification system [47, 48, 55–59, 60•]. In one study, a 40 % rate of disagreement with the original diagnosis was found after expert neuropathology review in which 9 % of all cases reviewed impacted therapy [61]. The WHO classification correlates only inconsistently with genetic markers and furthermore predicts prognosis poorly [56, 58, 60•]. Limited surgical sampling and omitting foci of higher grade histology may be another limitation of histological analysis [56–58, 61].
Molecular diagnosis permits an improvement in diagnosis and prognostication in LGG independent of morphologic criteria [60•, 62, 63]. The incorporation of molecular biomarkers in the next iteration of the WHO classification has been recently proposed (integrated ISN-Haarlem consensus) [64]. An integrated diagnosis combining molecular biomarkers with histological classification is currently recommended and increasingly used for therapeutic decisions [36, 60•, 65•] notwithstanding differing molecular classification systems (Table 2).
The most commonly utilized biomarkers in LGG include the expression of IDH1/2 (isocitrate dehydrogenase 1/2), the presence of G-CIMP (glioma-CpG island methylation phenotype), 1p/19q codeletion status, ATRX (alpha thalassemia mental retardation X-linked) expression, MGMT (methylguanine methyltransferase) promoter methylation, and TERT (telomerase reverse transcriptase) promoter mutation [59, 60•, 65•, 66•, 67•, 68•, 69–71] (Table 2). Other biomarkers, such as expression of CIC (capucia) and far upstream-binding protein 1 (FUBP1), N-myc downstream-regulated gene (NDRG)1, p53, alternative lengthening of telomeres (ALT) are of interest however require further validation [59, 71].
The Cancer Genome Atlas (TCGA) Research Network performed a genome-wide analyses of 293 grade II and III gliomas and compared the results from a multiplex molecular platform with both the WHO histologic classification and classification based on frequently used biomarkers in clinical practice: IDH1 and 1p/19q codeletion [60•] (Table 2). This molecular classification robustly stratified patient outcomes after adjustment for age and EOR.
The Mayo Clinic/University of California San Francisco (UCSF) model defined five glioma molecular groups using three biomarkers: mutation in the TERT promoter, IDH mutation, and 1p/19q codeletion [65•] (Table 2). A total of 1087 gliomas (615 WHO grade II or III gliomas) and 11,590 controls were assessed. The study concluded that the discrimination of five molecular groups according to the TERT promoter mutation, IDH mutation, and 1p/19q codeletion is highly correlated with age at diagnosis, clinical outcome, acquired genetic alterations, and germ line variants.
In a Japanese study, 332 WHO grade II and III gliomas were classified according to IDH mutation and 1p/19q codeletion status [66•] (Table 2). Type III gliomas had the poorest prognosis, with an OS similar to that of glioblastoma. Type III gliomas expressed other glioblastoma-like mutations such as amplification of EGFR, PDGFRA, CDK4, MDM2, and MDM4, deletion or mutation of PTEN, NF1, RB1, CDKN2A, and CDKN2B, del(10q), and amplification or mutation of class II phosphatidylinositol 3-kinase (PI3K) genes.
A German study of 405 adult glioma patients classified as 152 (37.5 %) astrocytomas, 61 (15 %) oligodendrogliomas, 63 (15.5 %) oligoastrocytomas, and 129 (32 %) glioblastomas according to the WHO 2007 classification was reanalyzed using ATRX expression, IDH1 mutation, and 1p/19q codeletion status [67•]. Gliomas were reclassified as astrocytomas in 155 cases (38 %), oligodendrogliomas in 100 cases (25 %) and glioblastomas in 150 cases (37 %). In 100 anaplastic gliomas from the NOA-4 trial with long-term follow-up data available, the diagnosis according to the integrated ISN-Haarlem consensus had significantly better prognostic power for both PFS and OS compared to the WHO 2007 classification. This model based on a stepwise analysis with initial immunohistochemistry for ATRX and IDH1 (R132H) followed by 1p/19q analysis and subsequent IDH sequencing, limits the number of molecular analysis and demonstrated a better association with patient outcome as compared to the WHO 2007 classification (Table 2).
In another German study of 137 patients including 61 WHO grade II and 76 WHO grade III gliomas, microarray-based genome- and transcriptome-wide analyses defined molecular subgroups related to histology, molecular markers (including IDH mutation, 1p/19q codeletion, and TERT promoter mutation), and patient outcome [68•]. The genomic profile identified five distinct glioma groups, three with an IDH mutation and two with IDH wild type. Expression profiling revealed eight transcriptionally different groups, five with IDH mutation, and three IDH wild type. Genomic profiling and expression profiling were only partially correlated. Correlation of DNA-based molecular stratification with clinical outcome defined three prognostic groups: the best prognosis was observed in IDH1/1 mutant and 1p/19q codeleted tumors and the worse outcome in patients with IDH non-mutated (wild type) tumors and glioblastoma-like genomic alteration such as gain of chromosome 7 arm, loss of chromosome arm 10q, TERT promoter mutation, and oncogene amplification. Patients with IDH1/2 mutation but no 1p19q codeletion had an intermediate prognosis.
The optimal combination of molecular biomarkers has not yet been validated or defined notwithstanding the multiplicity of proposed models illustrated in Table 2.
The similarities in outcome with comparable treatment between WHO grade II and grade III gliomas of the same lineage observed in the three trials of RT + PCV support the use of a common strategy for lower grade gliomas based on the presence of the 1p19q codeletion [19]. Nonetheless, an optimal therapy remains to be defined pending completion of CODEL, CATNON (a 4-arm RCT comparing RT alone to RT with three differing TMZ regimens in non-codeleted anaplastic gliomas), and a biomarker study of RTOG 9802. The molecular signature of LGG affects outcome regardless of treatment and the better outcome following large volume surgical resection reported may rather be a consequence of baseline molecular profile as opposed to EOR [18]. Based on the evolving significance of the molecular biomarker signature of LGG, the prognostic impact of the EOR and the molecular genotype has not been resolved. Additionally, the optimal RT dose based on the molecular classification of LGG merits consideration [19].
Neurocognitive Function
LGG most often occurs in young otherwise healthy adults. Late treatment-related toxicity and their impact on QoL must consequently be considered when deciding treatment. Neurocognitive function (NCF) at diagnosis has not been widely explored. Subtle deficits may be observed with pretreatment neuropsychological testing, although patients may still work and have an active social life [5]. At diagnosis, cognitive deficits are usually attributed to the tumor, tumor-related seizures, or use of antiepileptic drugs. Other factors, such as cognitive reserve and genetic susceptibility, likely influence cognition but have been rarely determined a priori [19, 72]. After treatment, the impact on NCF of tumor progression and toxicity of treatment has not been clearly defined. Worsening, most often transient, NCF can be observed especially after extensive resection [73, 74]. The RTOG 0925 trial is evaluating the natural history of NCF, QoL, and seizure control in patients with supratentorial low-risk LGG following surgery only will provide needed information on the cognitive impact of the tumor itself. A cohort of 160 LGG was studied to determine the cognitive impact of RT. Cognitive decline and leukoencephalopathy were significantly higher in the group with post-operative RT [75]. Neuropsychological evaluations were performed in a cohort of 65 long-term LGG survivors with stable disease after a mean of 12 years. Cognitive impairment was observed in 53 % of the patients treated with RT versus 27 % in the group of patients without RT. The deficits were more pronounced in attention, executive functioning, and processing speed [20]. These data support an approach in which a delay in the administration of RT as long as safely possible likely improves long-term neurocognitive outcome. Modern highly conformal RT such as proton-based RT may have less toxicity with respect to NCF however this hypothesis remains to be proven. A negative cognitive effect of chemotherapy only has been reported, particularly in breast cancer. So-called chemobrain usually impacts concentration and short-term memory, executive functioning, verbal ability, and visuospatial ability [76]. Whether a similar situation exists in gliomas, tumors that reside in and impact brain is more difficult to determine but likely contributes in part to neurocognitive injury [77].
In a neurocognitive evaluation, conducted in 352 patients enrolled in the RTOG 9802 trial, consisting of a MMSE at baseline and at 1, 2, 3, and 5 years, only a few patients experienced a significant decline in MMSE score. No significant difference was observed in the proportion of patients with MMSE score decline between arms and both arms experienced a significant similar gain over time [72]. The MMSE is however a relatively insensitive tool, and thus subtle changes in NCF after RT or RT + PCV cannot be excluded.
Conclusion
The prognosis of LGG differs between high-risk and low-risk patients notwithstanding varying definitions of what constitutes a high-risk patient. Concerns regarding therapy-associated cognitive impairment that impacts QoL and has in part limited the acceptance both by patients and providers of RT as initial treatment of LGG. Chemotherapy alone as a treatment of LGG may result in less toxicity however this has only once been prospectively evaluated in patients with high-risk LGG (EORTC 22033). EORTC 22033–26033 concluded that TMZ for progressing LGG not previously treated aside from initial surgery was not superior to RT in terms of PFS and with the caveat that OS results remain immature. Nonetheless and without a supportive RCT, there remain advocates of early chemotherapy with deferred RT as an option for patients with low-risk LGG either at diagnosis or at first progression.
The current standard of care for low-risk LGG is maximal safe resection followed by observation only based upon EORTC 22844 and 22845 and the NCCTG/RTOG/ECOG trials (Fig. 1). The RTOG 9802 trial defined RT + PCV as the new standard of care in high-risk LGG.
A challenge remains to define when an aggressive treatment improves OS without impacting QoL or NCF and when an effective treatment can be delayed in order to preserve QoL without impacting survival. Thus, improved definition of high-risk and low-risk LGG is of particular importance so as to define initial therapy.
Current WHO histopathological classification is poorly predictive of outcome in patients with LGG. The integration of molecular biomarkers into the histological classification will lead to an improved classification schema that more accurately reflects underlying tumor biology, prognosis, and hopefully best therapy. However, how molecular biomarker data impacts current therapies remains to be defined.
Yet to be explored are potential molecular targets in LGG including the BRAF serine/threonine kinase gene, the phosphatidyl inositol-3-kinase (PI3K)/AKT/mammalian target of rapamycin (mTOR) network, as well as IDH1 [42, 78]. Novel targeted therapies for LGG are an unmet need in neuro-oncology that hopefully will become increasingly relevant as the molecular definition of these tumors improves.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Tandon A, Schiff D. Therapeutic decision making in patients with newly diagnosed low grade glioma. Curr Treat Options Oncol. 2014;15:529–38. An overview on the role of surgery in the treatment of LGG.
Rees J. Temozolomide in low-grade gliomas: living longer and better. J Neurol Neurosurg Psychiatry. 2015;86:359–60.
Wen PY, DeAngelis LM. Chemotherapy for low-grade gliomas: emerging consensus on its benefits. Neurology. 2007;68:1762–3.
Ius T, Isola M, Budai R, Pauletto G, Tomasino B, Fadiga L, et al. Low-grade glioma surgery in eloquent areas: volumetric analysis of extent of resection and its impact on overall survival. A single-institution experience in 190 patients: clinical article. J Neurosurg. 2012;117:1039–52.
Duffau H, Taillandier L. New concepts in the management of diffuse low-grade glioma: proposal of a multistage and individualized therapeutic approach. Neuro-Oncology. 2015;17:332–42.
Hollon T, Hervey-Jumper SL, Sagher O, Orringer DA. Advances in the surgical management of low-grade glioma. Semin Radiat Oncol. 2015;25:181–8.
Soffietti R, Baumert BG, Bello L, von Deimling A, Duffau H, Frénay M, et al. Guidelines on management of low-grade gliomas: report of an EFNS-EANO Task Force. Eur J Neurol Off J Eur Fed Neurol Soc. 2010;17:1124–33. An excellent review of treatment of LGG.
Chang EF, Potts MB, Keles GE, Lamborn KR, Chang SM, Barbaro NM, et al. Seizure characteristics and control following resection in 332 patients with low-grade gliomas. J Neurosurg. 2008;108:227–35.
Pallud J, Audureau E, Blonski M, Sanai N, Bauchet L, Fontaine D, et al. Epileptic seizures in diffuse low-grade gliomas in adults. Brain J Neurol. 2014;137:449–62.
Gorlia T, Wu W, Wang M, Baumert BG, Mehta M, Buckner JC, et al. New validated prognostic models and prognostic calculators in patients with low-grade gliomas diagnosed by central pathology review: a pooled analysis of EORTC/RTOG/NCCTG phase III clinical trials. Neuro-Oncology. 2013;15:1568–79.
Smith JS, Chang EF, Lamborn KR, Chang SM, Prados MD, Cha S, et al. Role of extent of resection in the long-term outcome of low-grade hemispheric gliomas. J Clin Oncol Off J Am Soc Clin Oncol. 2008;26:1338–45.
Jakola AS, Unsgård G, Myrmel KS, Kloster R, Torp SH, Losvik OK, et al. Surgical strategy in grade II astrocytoma: a population-based analysis of survival and morbidity with a strategy of early resection as compared to watchful waiting. Acta Neurochir (Wien). 2013;155:2227–35.
Kiebert GM, Curran D, Aaronson NK, Bolla M, Menten J, Rutten EH, et al. Quality of life after radiation therapy of cerebral low-grade gliomas of the adult: results of a randomised phase III trial on dose response (EORTC trial 22844). EORTC Radiotherapy Co-operative Group. Eur J Cancer Oxf Engl 1990. 1998;34:1902–9.
Shaw E, Arusell R, Scheithauer B, O’Fallon J, O’Neill B, Dinapoli R, et al. Prospective randomized trial of low- versus high-dose radiation therapy in adults with supratentorial low-grade glioma: initial report of a North Central Cancer Treatment Group/Radiation Therapy Oncology Group/Eastern Cooperative Oncology Group study. J Clin Oncol Off J Am Soc Clin Oncol. 2002;20:2267–76.
Brown PD, Buckner JC, O’Fallon JR, Iturria NL, Brown CA, O’Neill BP, et al. Effects of radiotherapy on cognitive function in patients with low-grade glioma measured by the Folstein mini-mental state examination. J Clin Oncol Off J Am Soc Clin Oncol. 2003;21:2519–24.
van den Bent MJ, Afra D, de Witte O, Ben Hassel M, Schraub S, Hoang-Xuan K, et al. Long-term efficacy of early versus delayed radiotherapy for low-grade astrocytoma and oligodendroglioma in adults: the EORTC 22845 randomised trial. Lancet Lond Engl. 2005;366:985–90.
Shaw EG, Berkey B, Coons SW, Bullard D, Brachman D, Buckner JC, et al. Recurrence following neurosurgeon-determined gross-total resection of adult supratentorial low-grade glioma: results of a prospective clinical trial. J Neurosurg. 2008;109:835–41.
van den Bent MJ, Snijders TJ, Bromberg JEC. Current treatment of low grade gliomas. Memo. 2012;5:223–7.
van den Bent MJ. Practice changing mature results of RTOG study 9802: another positive PCV trial makes adjuvant chemotherapy part of standard of care in low-grade glioma. Neuro-Oncology. 2014;16:1570–4.
Douw L, Klein M, Fagel SS, van den Heuvel J, Taphoorn MJ, Aaronson NK, et al. Cognitive and radiological effects of radiotherapy in patients with low-grade glioma: long-term follow-up. Lancet Neurol. 2009;8:810–8.
Mason WP, Krol GS, DeAngelis LM. Low-grade oligodendroglioma responds to chemotherapy. Neurology. 1996;46:203–7.
Soffietti R, Rudà R, Bradac GB, Schiffer D. PCV chemotherapy for recurrent oligodendrogliomas and oligoastrocytomas. Neurosurgery. 1998;43:1066–73.
Buckner JC, Gesme D, O’Fallon JR, Hammack JE, Stafford S, Brown PD, et al. Phase II trial of procarbazine, lomustine, and vincristine as initial therapy for patients with low-grade oligodendroglioma or oligoastrocytoma: efficacy and associations with chromosomal abnormalities. J Clin Oncol Off J Am Soc Clin Oncol. 2003;21:251–5.
Stege EMB, Kros JM, de Bruin HG, Enting RH, van Heuvel I, Looijenga LHJ, et al. Successful treatment of low-grade oligodendroglial tumors with a chemotherapy regimen of procarbazine, lomustine, and vincristine. Cancer. 2005;103:802–9.
Lebrun C, Fontaine D, Bourg V, Ramaioli A, Chanalet S, Vandenbos F, et al. Treatment of newly diagnosed symptomatic pure low-grade oligodendrogliomas with PCV chemotherapy. Eur J Neurol Off J Eur Fed Neurol Soc. 2007;14:391–8.
Peyre M, Cartalat-Carel S, Meyronet D, Ricard D, Jouvet A, Pallud J, et al. Prolonged response without prolonged chemotherapy: a lesson from PCV chemotherapy in low-grade gliomas. Neuro-Oncology. 2010;12:1078–82.
Taal W, van der Rijt CCD, Dinjens WNM, Sillevis Smitt PAE, Wertenbroek AAACM, Bromberg JEC, et al. Treatment of large low-grade oligodendroglial tumors with upfront procarbazine, lomustine, and vincristine chemotherapy with long follow-up: a retrospective cohort study with growth kinetics. J Neurooncol. 2015;121:365–72.
Brada M, Hoang-Xuan K, Rampling R, Dietrich PY, Dirix LY, Macdonald D, et al. Multicenter phase II trial of temozolomide in patients with glioblastoma multiforme at first relapse. Ann Oncol Off J Eur Soc Med Oncol ESMO. 2001;12:259–66.
Hoang-Xuan K, Capelle L, Kujas M, Taillibert S, Duffau H, Lejeune J, et al. Temozolomide as initial treatment for adults with low-grade oligodendrogliomas or oligoastrocytomas and correlation with chromosome 1p deletions. J Clin Oncol Off J Am Soc Clin Oncol. 2004;22:3133–8.
Kaloshi G, Benouaich-Amiel A, Diakite F, Taillibert S, Lejeune J, Laigle-Donadey F, et al. Temozolomide for low-grade gliomas: predictive impact of 1p/19q loss on response and outcome. Neurology. 2007;68:1831–6.
Kaloshi G, Rroji A, Petrela M. Upfront chemotherapy with CCNU alone for adults’ low-grade gliomas: a clinical analysis. J Neurooncol. 2014;117:373–4.
Temozolomide chemotherapy versus radiotherapy in molecularly characterized (1p loss) low-grade glioma: a randomized phase III intergroup study by the EORTC/NCIC-CTG/TROG/MRC-CTU (EORTC 22033–26033). J. Clin. Oncol. [Internet]. [cited 2015 Aug 8]; Available from: http://meetinglibrary.asco.org/content/111001-132.
Radiotherapy in relation to temozolomide: Subgroup analysis of molecular markers of the randomized phase III study by the EORTC/NCIC-CTG/TROG/MRC-CTU (EORTC 22033–26033) in patients with a high risk low-grade glioma. J. Clin. Oncol. [Internet]. [cited 2015 Sep 27]; Available from: http://meetinglibrary.asco.org/content/147310-156.
Panageas KS, Iwamoto FM, Cloughesy TF, Aldape KD, Rivera AL, Eichler AF, et al. Initial treatment patterns over time for anaplastic oligodendroglial tumors. Neuro-Oncology. 2012;14:761–7.
Schaff LR, Lassman AB. Indications for treatment: is observation or chemotherapy alone a reasonable approach in the management of low-grade gliomas? Semin Radiat Oncol. 2015;25:203–9.
van den Bent MJ. Chemotherapy for low-grade glioma: when, for whom, which regimen? Curr. Opin. Neurol. 2015.
van den Bent MJ, Taphoorn MJB, Brandes AA, Menten J, Stupp R, Frenay M, et al. Phase II study of first-line chemotherapy with temozolomide in recurrent oligodendroglial tumors: the European Organization for Research and Treatment of Cancer Brain Tumor Group Study 26971. J Clin Oncol Off J Am Soc Clin Oncol. 2003;21:2525–8.
Pace A, Vidiri A, Galiè E, Carosi M, Telera S, Cianciulli AM, et al. Temozolomide chemotherapy for progressive low-grade glioma: clinical benefits and radiological response. Ann Oncol Off J Eur Soc Med Oncol ESMO. 2003;14:1722–6.
Quinn JA, Reardon DA, Friedman AH, Rich JN, Sampson JH, Provenzale JM, et al. Phase II trial of temozolomide in patients with progressive low-grade glioma. J Clin Oncol Off J Am Soc Clin Oncol. 2003;21:646–51.
Weller M, van den Bent M, Hopkins K, Tonn JC, Stupp R, Falini A, et al. EANO guideline for the diagnosis and treatment of anaplastic gliomas and glioblastoma. Lancet Oncol. 2014;15:e395–403.
Wick W, Wiestler B, Platten M. Treatment of anaplastic glioma. Cancer Treat Res. 2015;163:89–101.
Ahluwalia MS, Chang SM. Medical therapy of gliomas. J Neurooncol. 2014;119:503–12.
Laack NN, Sarkaria JN, Buckner JC. Radiation Therapy Oncology Group 9802: controversy or consensus in the treatment of newly diagnosed low-grade glioma? Semin Radiat Oncol. 2015;25:197–202.
Fisher BJ, Hu C, Macdonald DR, Lesser GJ, Coons SW, Brachman DG, et al. Phase 2 study of temozolomide-based chemoradiation therapy for high-risk low-grade gliomas: preliminary results of Radiation Therapy Oncology Group 0424. Int J Radiat Oncol Biol Phys. 2015;91:497–504.
Phase III study of radiation therapy (RT) with or without procarbazine, CCNU, and vincristine (PCV) in low-grade glioma: RTOG 9802 with Alliance, ECOG, and SWOG. J. Clin. Oncol. [Internet]. [cited 2015 Sep 27]; Available from: http://meetinglibrary.asco.org/content/127483-144. This phase III trial established a new standard of care in high-risk LLG patients.
Shaw EG, Wang M, Coons SW, Brachman DG, Buckner JC, Stelzer KJ, et al. Randomized trial of radiation therapy plus procarbazine, lomustine, and vincristine chemotherapy for supratentorial adult low-grade glioma: initial results of RTOG 9802. J Clin Oncol Off J Am Soc Clin Oncol. 2012;30:3065–70.
Intergroup Radiation Therapy Oncology Group Trial 9402, Cairncross G, Berkey B, Shaw E, Jenkins R, Scheithauer B, et al. Phase III trial of chemotherapy plus radiotherapy compared with radiotherapy alone for pure and mixed anaplastic oligodendroglioma: Intergroup Radiation Therapy Oncology Group Trial 9402. J Clin Oncol Off J Am Soc Clin Oncol. 2006;24:2707–14.
van den Bent MJ, Carpentier AF, Brandes AA, Sanson M, Taphoorn MJB, Bernsen HJJA, et al. Adjuvant procarbazine, lomustine, and vincristine improves progression-free survival but not overall survival in newly diagnosed anaplastic oligodendrogliomas and oligoastrocytomas: a randomized European Organisation for Research and Treatment of Cancer phase III trial. J Clin Oncol Off J Am Soc Clin Oncol. 2006;24:2715–22.
Nabors LB, Portnow J, Ammirati M, Brem H, Brown P, Butowski N, et al. Central nervous system cancers, version 2.2014. Featured updates to the NCCN Guidelines. J Natl Compr Cancer Netw JNCCN. 2014;12:1517–23.
Chamberlain MC. Does RTOG 9802 change practice with respect to newly diagnosed low-grade glioma? J Clin Oncol Off J Am Soc Clin Oncol. 2013;31:652–3.
Pignatti F, van den Bent M, Curran D, Debruyne C, Sylvester R, Therasse P, et al. Prognostic factors for survival in adult patients with cerebral low-grade glioma. J Clin Oncol Off J Am Soc Clin Oncol. 2002;20:2076–84.
Daniels TB, Brown PD, Felten SJ, Wu W, Buckner JC, Arusell RM, et al. Validation of EORTC prognostic factors for adults with low-grade glioma: a report using intergroup 86-72-51. Int J Radiat Oncol Biol Phys. 2011;81:218–24.
Gozé C, Blonski M, Le Maistre G, Bauchet L, Dezamis E, Page P, et al. Imaging growth and isocitrate dehydrogenase 1 mutation are independent predictors for diffuse low-grade gliomas. Neuro-Oncology. 2014;16:1100–9.
Guillevin R, Menuel C, Duffau H, Kujas M, Capelle L, Aubert A, et al. Proton magnetic resonance spectroscopy predicts proliferative activity in diffuse low-grade gliomas. J Neurooncol. 2008;87:181–7.
van den Bent MJ, Jaeckle K, Baumert B, Wick W. RTOG 9802: good wines need aging. J Clin Oncol Off J Am Soc Clin Oncol. 2013;31:653–4.
van den Bent MJ. Interobserver variation of the histopathological diagnosis in clinical trials on glioma: a clinician’s perspective. Acta Neuropathol (Berl). 2010;120:297–304.
Aldape K, Burger PC, Perry A. Clinicopathologic aspects of 1p/19q loss and the diagnosis of oligodendroglioma. Arch Pathol Lab Med. 2007;131:242–51.
Coons SW, Johnson PC, Scheithauer BW, Yates AJ, Pearl DK. Improving diagnostic accuracy and interobserver concordance in the classification and grading of primary gliomas. Cancer. 1997;79:1381–93.
Olar A, Sulman EP. Molecular markers in low-grade glioma-toward tumor reclassification. Semin Radiat Oncol. 2015;25:155–63.
Cancer Genome Atlas Research Network, Brat DJ, Verhaak RGW, Aldape KD, Yung WKA, Salama SR, et al. Comprehensive, integrative genomic analysis of diffuse lower-grade gliomas. N Engl J Med. 2015;372:2481–98. Proposal for a new classification of grade II and III gliomas.
Bruner JM, Inouye L, Fuller GN, Langford LA. Diagnostic discrepancies and their clinical impact in a neuropathology referral practice. Cancer. 1997;79:796–803.
Jiao Y, Killela PJ, Reitman ZJ, Rasheed AB, Heaphy CM, de Wilde RF, et al. Frequent ATRX, CIC, FUBP1 and IDH1 mutations refine the classification of malignant gliomas. Oncotarget. 2012;3:709–22.
Yan H, Parsons DW, Jin G, McLendon R, Rasheed BA, Yuan W, et al. IDH1 and IDH2 mutations in gliomas. N Engl J Med. 2009;360:765–73.
Louis DN, Perry A, Burger P, Ellison DW, Reifenberger G, von Deimling A, et al. International Society Of Neuropathology—Haarlem consensus guidelines for nervous system tumor classification and grading. Brain Pathol Zurich Switz. 2014;24:429–35.
Eckel-Passow JE, Lachance DH, Molinaro AM, Walsh KM, Decker PA, Sicotte H, et al. Glioma groups based on 1p/19q, IDH, and TERT promoter mutations in tumors. N Engl J Med. 2015;372:2499–508. Proposal for a new classification of grade II and III gliomas.
Suzuki H, Aoki K, Chiba K, Sato Y, Shiozawa Y, Shiraishi Y, et al. Mutational landscape and clonal architecture in grade II and III gliomas. Nat Genet. 2015;47:458–68. Proposal for a new classification of grade II and III gliomas.
Reuss DE, Sahm F, Schrimpf D, Wiestler B, Capper D, Koelsche C, et al. ATRX and IDH1-R132H immunohistochemistry with subsequent copy number analysis and IDH sequencing as a basis for an “integrated” diagnostic approach for adult astrocytoma, oligodendroglioma and glioblastoma. Acta Neuropathol (Berl). 2015;129:133–46. Proposal for a new classification of grade II and III gliomas.
Weller M, Weber RG, Willscher E, Riehmer V, Hentschel B, Kreuz M, et al. Molecular classification of diffuse cerebral WHO grade II/III gliomas using genome- and transcriptome-wide profiling improves stratification of prognostically distinct patient groups. Acta Neuropathol (Berl). 2015;129:679–93. Proposal for a new classification of grade II and III gliomas.
Dubbink HJ, Taal W, van Marion R, Kros JM, van Heuvel I, Bromberg JE, et al. IDH1 mutations in low-grade astrocytomas predict survival but not response to temozolomide. Neurology. 2009;73:1792–5.
Taylor JW, Chi AS, Cahill DP. Tailored therapy in diffuse gliomas: using molecular classifiers to optimize clinical management. Oncol Williston Park N. 2013;27:504–14.
Blaes J, Weiler M, Sahm F, Hentschel B, Osswald M, Czabanka M, et al. NDRG1 prognosticates the natural course of disease in WHO grade II glioma. J Neurooncol. 2014;117:25–32.
Prabhu RS, Won M, Shaw EG, Hu C, Brachman DG, Buckner JC, et al. Effect of the addition of chemotherapy to radiotherapy on cognitive function in patients with low-grade glioma: secondary analysis of RTOG 98–02. J Clin Oncol Off J Am Soc Clin Oncol. 2014;32:535–41.
Klein M, Duffau H, De Witt Hamer PC. Cognition and resective surgery for diffuse infiltrative glioma: an overview. J Neurooncol. 2012;108:309–18.
Duffau H. Cognitive assessment in glioma patients. J Neurosurg. 2013;119:1348–9.
Surma-aho O, Niemelä M, Vilkki J, Kouri M, Brander A, Salonen O, et al. Adverse long-term effects of brain radiotherapy in adult low-grade glioma patients. Neurology. 2001;56:1285–90.
Jim HSL, Phillips KM, Chait S, Faul LA, Popa MA, Lee Y-H, et al. Meta-analysis of cognitive functioning in breast cancer survivors previously treated with standard-dose chemotherapy. J Clin Oncol Off J Am Soc Clin Oncol. 2012;30:3578–87.
Pereira Dias G, Hollywood R, Bevilaqua MC do N, da Luz ACD da S, Hindges R, Nardi AE, et al. Consequences of cancer treatments on adult hippocampal neurogenesis: implications for cognitive function and depressive symptoms. Neuro-Oncology. 2014;16:476–92.
Schumacher T, Bunse L, Pusch S, Sahm F, Wiestler B, Quandt J, et al. A vaccine targeting mutant IDH1 induces antitumour immunity. Nature. 2014;512:324–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Emilie Le Rhun, Sophie Taillibert, and Marc C. Chamberlain each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Neuro-oncology
Rights and permissions
About this article
Cite this article
Le Rhun, E., Taillibert, S. & Chamberlain, M.C. Current Management of Adult Diffuse Infiltrative Low Grade Gliomas. Curr Neurol Neurosci Rep 16, 15 (2016). https://doi.org/10.1007/s11910-015-0615-4
Published:
DOI: https://doi.org/10.1007/s11910-015-0615-4