Abstract
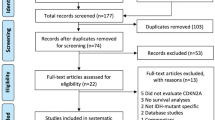
There is a lack of relevant prognostic and predictive factors in neurooncology besides mutation of isocitrate dehydrogenase 1, codeletion of 1p/19q and promoter hypermethylation of O 6 -methylguanine-DNA-methyltransferase. More importantly, there is limited translation of these factors into clinical practice. The cancer genome atlas data and also clinical correlative analyses suggest a pivotal role for the epidermal growth factor receptor /protein kinase B/mammalian target of rapamycin (mTOR) pathway in both biology and the clinical course of gliomas. However, attempts to stratify gliomas by activating alterations in this pathway have failed thus far. The tumors of 40 patients with WHO grade II gliomas without immediate postoperative genotoxic treatment and known progression and survival status at a median follow-up of 12.2 years were analyzed for expression of the mTOR complex 2 downstream target N-myc downstream regulated gene (NDRG)1 using immunohistochemistry. Baseline characteristics for NDRG1 absent/low versus moderate/high patients were similar. Time to reintervention was significantly longer in the NDRG1 group (P = 0.026). NDRG1 may become a novel biomarker to guide the decision which WHO°II glioma patients may be followed without postsurgical intervention and which patients should receive genotoxic treatment early on. Validation of this hypothesis will be possible with the observational arm of the RTOG 9802 and the pretreatment step of the EORTC 22033/26032 trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
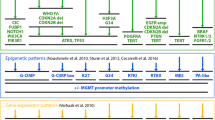
Mutations of the isocitrate dehydrogenase (IDH) gene 1 were first identified in human gliomas as a result of a large-scale genomic sequencing approach [1]. This has been confirmed across gliomas of World Health Organization (WHO) grades II–IV, including both astrocytic and oligodendroglial tumors [2–4]. However, most studies have failed to link IDH1 mutations to better responsiveness to specific types of treatment, neither in glioblastoma [5], anaplastic glioma [2, 6] nor low-grade glioma [7].
Although diagnoses of gliomas are based on histology, molecular abnormalities known to occur in these tumors have been evolving as supportive markers to assist diagnostics and patient management. Besides IDH1 mutations, these markers in WHO grade II gliomas are O 6-methylguanine-DNA methyltransferase (MGMT) promoter methylation status, deletions involving chromosomes 1p and 19q, and mutations in the v-raf murine sarcoma viral oncogene homolog B1 (BRAF) oncogene have moved into the focus of scientific interest and are already implemented in routine diagnostic workup. To evaluate the clinical relevance of these markers, it is crucial to distinguish the prognostic significance, defined as overall better outcome irrespective of management, from the predictive significance, defined as a better outcome given a specific treatment is administered [8].
Hypermethylation of the MGMT gene promoter for malignant gliomas and codeletion of 1p/19q for anaplastic oligodendroglial tumors are the only biomarkers linked to sensitivity to a specific treatment, that is, alkylating chemotherapy, specifically temozolomide (TMZ) for MGMT [9, 10] and the combination of procarbazine, 1-(2-chlorethyl)-3-cyclohexyl-1-nitrosourea (CCNU) and vincristine (PCV) for 1p/19q codeletion [11, 12]. Until recently, it was believed that the predictive value of MGMT promoter methylation may be limited to glioblastoma since anaplastic gliomas showed a more favorable course of disease with a hypermethylated MGMT promoter in both alkylator- and also radiotherapy-treated patients [2, 11]. Interaction analyses between IDH1 and MGMT, however, have revealed that MGMT promoter methylation is probably a predictive biomarker for response to chemotherapy in patients with IDH1 wild-type, but not IDH1 mutant gliomas, irrespective of WHO grade [13]. All currently known biomarkers unravel their prognostic properties only if genotoxic treatment is used and none of the biomarkers discussed so far, including IDH or TP53 status, MGMT promoter hypermethylation or 1p/19q codeletion, show a good relation to the natural course of disease [8, 14]. In low-grade gliomas, guidance whether a patient with a newly diagnosed tumor needs early genotoxic treatment or not is pivotal, as the most commonly used treatment, radiotherapy of the involved part of the brain [15], is not associated with an overall survival (OS) benefit but possibly with long-term adverse sequelae especially in patients with a favorable prognosis [16].
The mTORC2-pathway effector, N-myc downstream regulated gene (NDRG)1, has been proposed as a prognostic factor in tumors including gliomas [17], although prognostic relevance in either direction has been described. Most recently, recurrent translocations of the oncogene plasmocytoma variant translocation (PVT)1, including PVT1–MYC and PVT1–NDRG1, have been described as potential targets in group 3 medulloblastoma [18].
Initial experiments assessing the role of NDRG1 in basic in vitro and in vivo proliferation paradigms surprisingly revealed growth-limiting properties of NDRG1 expression [19]. From that, we hypothesized that World Health Organization (WHO) grade II gliomas with a differential postoperative course of disease can be separated on the basis of the expression of the mTORC2 downstream target, NDRG1, which then may serve as a biomarker for the decision to treat or to perform a watch-and-wait strategy.
Materials and methods
Patients and evaluations: German glioma network (GGN) cohort
The GGN is a prospective cohort study that enrolled newly diagnosed patients with various types of glioma and frozen tissue asservation from October 2004 to October 2010. From this cohort, we identified 40 patients with a diagnosis of a supratentorial WHO grade II astrocytoma or oligodendroglial tumor confirmed by history taking and central pathology review [20], as well as adequate follow-up at least until progression, who were followed by a watch-and-scan policy according to investigators’ discretion supported by risk factor profiles [21]. Some of these patients were included in previous publications addressing the same clinical correlative question, but assessing different markers [8, 14]. Clinical data were prospectively assembled as outlined before (http://www.gliomnetzwerk.de) [5]. All patients gave written informed consent. All activities of the GGN have been approved by the review boards of the participating institutions.
Molecular methods
1p/19q deletion status, MGMT promoter methylation as well as IDH and TP53 mutational status have been determined as described previously [8, 14].
Immunohistochemistry
Formalin-fixed paraffin-embedded tissue of 40 human grade II gliomas from the GGN [8, 14] was employed for immunohistochemical analysis for NDRG1 (goat anti-NDRG1 at 1:1,000, Abcam, Cambridge, England, UK) on 3 μm sections. For quantitative analysis of the staining pattern by an independent neuropathologist blinded to the clinical data, the Histo-Score by Bruna et al. [22] was applied. The score ranges from 0 to 300 and is calculated as the percentage of weakly stained cells plus the percentage of moderately stained cells multiplied by two plus the percentage of strongly stained cells multiplied by three. The entire tumor section was assessed except for areas not distinguishable from reactive tissue (Fig. 1). Ki67 immunostaining was done with an anti-Ki67 (MIB-1, mouse monoclonal antibody, Flex TRS low, 1:200 dilution, Dako, Glostrup, Denmark). For assessment of the proliferation index, anti-Ki67 immunostained tumors sections were scanned at low magnification to identify an area with high labelling density. In this area, 500 tumor cell nuclei were evaluated. The fraction of labelled nuclei per 500 tumor cell nuclei was determined by manual counting and is expressed as a percentage.
Histoscore for NDRG1 a NDRG1 immunohistochemistry in a case of moderate staining (histo score group >10, left) and a case with absence of NDRG1 expression (histo score group <10). Note staining of the tumor cell processes (arrows) and the decreasing staining of tumor matrix apart from strongly positive areas (arrowheads). b Representative cases illustrating the application of an adapted histo score [22] for evaluation of NDRG1 staining on paraffin-embedded glioma sections. The score ranges from 0 to 300 and is calculated as the percentage of weakly stained cells plus the percentage of moderately stained cells multiplied by two plus the percentage of strongly stained cells multiplied by three (positive cells are stained red and an isotype control c is provided). The entire tumor section was assessed except for areas not distinguishable from reactive tissue
Statistical analysis
Survival data for NDRG1 low (0–10) or intermediate/high (>10–300) were plotted by the Kaplan–Meier method and analyzed by the log-rank test. Multivariate analysis of progression-free survival (PFS) used Cox proportional hazards models to adjust for the following clinical data and molecular markers: histological tumor type, resection status, age in years, IDH1 status and MGMT promoter methylation status. Survival analyses were performed by B.H. using IBM SPSS Statistics Version 20.
Results
Baseline clinical and molecular characteristics and NDGR1 expression
To assess whether the postoperative course of disease in WHO grade II glioma patients shows an association with NDRG1 expression, we took advantage of a series of patients who received no immediate radiotherapy or chemotherapy after the diagnosis had been established as part of a surgical intervention. The patients were assigned to two different groups: NDRG1 absent/low versus NDRG1 moderate/high as illustrated in Fig. 1. The two groups were well balanced with respect to age, post-operative KPS, histological subtype, Ki67 labelling, 1p/19q status, IDH status, TP53 status, but there was an overrepresentation of gross total resections and MGMT promoter hypermethylation in the NDRG1 absent/low group (Table 1).
High NDRG1 levels are associated with longer time to intervention, but not overall survival
After a median follow-up of 146 months, 40 patients have progressed (100 %) and 26 patients (65 %) have died. At progression, 24 patients were treated with radiotherapy, 10 patients with chemotherapy, and 6 patients with combined modality treatment.
In the univariate analysis oligodendroglial histology and moderate/high NDRG1 expression were associated with a strong risk reduction for progression (Table 2). Moderate/high NDRG1 expression was associated with superior PFS [NDRG1 low: median PFS 30 months (95 % confidence interval 12–48 months)] versus [NDRG1 medium/high: median PFS 54 months (95 % confidence interval 24–84 months)] (Fig. 2a). Of note, the effect of NDRG1 was present also in analyses separated for astrocytic and oligodendroglial histologies without differential impact. On multivariate analysis, oligodendroglial histology (HR 0.3, 95 % CI 0.1–0.6, P = 0.001) and moderate/high NDRG1 expression (HR 0.4, 95 % CI 0.2–0.8, P = 0.01) persisted as strong prognostic factors (Table 2).
NDRG1 expression prognosticates superior PFS in postsurgically untreated WHO grade II gliomas a PFS and b OS data of 40 patients with a WHO grade II glioma without postsurgical treatment until further progression are plotted in the group no/low or moderate/high expression of NDRG1 in the tumor tissue. Scoring and grouping was done by an independent neuropathologist (FS) blinded to PFS or OS data. c NDRG1 expression relative to patient survival in glioblastoma (REMBRANDT)
For OS, however, i.e. after one or more genotoxic treatments, which included sequential radiotherapy and alkylating chemotherapy in either order in all patients, only age was prognostic (<40 years versus ≥40 years, P < 0.05) and the two NDRG1 groups did not differ anymore (Fig. 2b). Due to the lack of archival data to confirm our findings, we just took the opportunity to check for the potential negative impact on OS in patients that had undergone radiochemotherapy. Analysis of the repository for molecular brain neoplasia data (REMBRANDT) database revealed that the OS of glioblastoma patients with intratumoral upregulation of NDRG1 was reduced compared to patients with intermediate or downregulated expression of this gene (Fig. 2c).
These data indicate that moderate/high NDRG1 expression is an independent prognostic factor for favorable outcome in patients with WHO grade II gliomas not exposed to postsurgical treatment.
Discussion
Despite relevant progress in the field of molecular classification of malignant gliomas, all attempts to define a parameter, which predicts the natural course of disease in low-grade gliomas, have failed thus far. Patients with these tumors are currently treated or followed based on the set of prognostic parameters developed from the EORTC 22844 trial [21], but still a lot of uncertainty for individual treatment decisions remains. From this set of parameters, oligodendroglial histology has been confirmed here as prognostic for PFS without postsurgical intervention (Table 2).
Analyses of the prognostic potential of 1p/19q codeletion, IDH1 mutation and MGMT promoter hypermethylation revealed a prognostic or predictive potential of these markers only when radio- or chemotherapy were used [5, 8, 14]. In addition, there are molecular alterations like duplications or mutations of the v-raf murine sarcoma viral oncogene homolog B1 (BRAF) that not only define a specific glioma entity, but may also be linked to a specific therapy [23]. There is an unmet need for molecular markers with prognostic impact in the immediate postsurgical situation [24] that facilitate daily decision-making in the clinic.
Despite its name, NDRG1 is neither regulated by nor correlated to N-Myc in glioma [19]. NDRG1 has been described as a hypoxia-inducible protein in glioblastoma, whose expression is associated with increasing malignancy in gliomas, peaking out in relapsed glioblastomas following radiochemotherapy [19]. Our survival analysis on postsurgically untreated WHO°II gliomas demonstrate an NDRG1-associated growth delay and thus an improved PFS in a multivariate analysis (Fig. 2a), which was not visible any more at OS when genotoxic treatments had been applied (Fig. 2b). Due to a lack of a confirmatory data set, we only confirmed the negative prognostic impact of NDRG1 mRNA expression when treatments are applied (Fig. 2c). These data allow a separation of disease- and treatment-modifying effects and support a tumor-suppressing function of NDRG1, which is limiting tumorigenicity in the natural course of the disease. Further, the other biomarkers discussed in glioma, 1p/19q, IDH1, MGMT, Ki67 labelling [8, 14], hot spot mutations in the promoter region of telomerase reverse transcriptase (TERT) [25] and mutation/loss of alpha-thalassemia/mental retardation syndrome X-linked (ATRX) expression [26] show a good relation to the natural course of disease, but unravel their prognostic properties only if cytotoxic treatment is applied. This prevents their use to categorize tumors and also to determine more favorable subgroups of tumors, in which a wait-and-scan strategy after surgery might be better than immediate cytotoxic treatment. The size of our patient cohort prevents further subgroup analyses. In this cohort, no interaction between tumor type, 1p/19q codeletion, IDH1 mutation or MGMT promoter methylation and NDRG1 expression was found. Of note, although no significant differences are found between the two NDRG1 expression groups, positive risk factors, specifically gross total resection, are numerically higher represented in the NDRG1 no/low group, and therefore bias against our finding (Table 1).
Outside the brain tumor field, the relevance of NDRG1 depends on the tumor entity. NDRG1 suppresses the proliferation of breast cancer cells in vitro [27] and the tumor growth of pancreatic and bladder cancer in vivo [27, 28], whereas survival and proliferation of hepatocellular carcinoma cells are promoted [29]. In line with these preclinical findings NDRG1 expression is associated with a favorable prognosis in patients with breast, colon or pancreatic cancer [28, 30, 31], but associated with more aggressive disease in cervical or liver cancer [32, 33]. In these studies, effects on tumor growth and therapy-modifying properties of NDRG1 are not separable.
In summary, NDRG1 may serve as the first prognostic biomarker for the natural course of disease in WHO grade II gliomas that awaits validation in the analyses of the observational arm of RTOG 9802 and the registration step of the EORTC 22033/26032 WHO grade II glioma trials.
References
Parsons DW, Jones S, Zhang X et al (2008) An integrated genomic analysis of human glioblastoma multiforme. Science 321:1807–1812
Wick W, Hartmann C, Engel C et al (2009) NOA-04 randomized phase III trial of sequential radiochemotherapy of anaplastic glioma with PCV or temozolomide. J Clin Oncol 27:5874–5880
Sanson M, Marie Y, Paris S et al (2009) Isocitrate dehydrogenase 1 codon 132 mutation is an important prognostic biomarker in gliomas. J Clin Oncol 27:4150–4154
Hartmann C, Hentschel B, Wick W et al (2010) Patients with IDH1 wild type anaplastic astrocytomas exhibit worse prognosis than IDH1-mutated glioblastomas, and IDH1 mutation status accounts for the unfavorable prognostic effect of higher age: implications for classification of gliomas. Acta Neuropathol 120:707–718
Weller M, Felsberg J, Hartmann C et al (2009) Molecular predictors of progression-free and overall survival in patients with newly diagnosed glioblastoma: a prospective translational study of the German Glioma Network. J Clin Oncol 27:5743–5750
Van den Bent MJ, Dubbink HJ, Marie Y et al (2010) IDH1 and IDH2 mutations are prognostic but not predictive for outcome in anaplastic oligodendroglial tumors: a report of the European organization for Research and Treatment of Cancer Brain Tumor Group. Clin Cancer Res 16:1597–1604
Dubbink HJ, Taal W, van Marion R et al (2009) IDH1 mutations in low-grade astrocytomas predict survival but not response to temozolomide. Neurology 73:1792–1795
Hartmann C, Hentschel B, Tatagiba M et al (2011) Molecular markers in low-grade gliomas: predictive or prognostic? Clin Cancer Res 17:4588–4599
Hegi ME, Diserens AC, Gorlia T et al (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 352:997–1003
Wick W, Platten M, Meisner C et al (2012) Temozolomide chemotherapy alone versus radiotherapy alone for malignant astrocytoma in the elderly: the NOA-08 randomised, phase 3 trial. Lancet Oncol 13:707–715
van den Bent MJ, Brandes AA, Taphoorn MJ et al (2013) Adjuvant procarbazine, lomustine, and vincristine chemotherapy in newly diagnosed anaplastic oligodendroglioma: long-term follow-up of EORTC Brain Tumor Group Study 26951. J Clin Oncol 31:344–350
Cairncross G, Wang M, Shaw E et al (2013) Phase III trial of chemoradiotherapy for anaplastic oligodendroglioma: long-term results of RTOG 9402. J Clin Oncol 31:337–343
Wick W, Meisner C, Hentschel B et al (2013) Prognostic or predictive value of MGMT promoter methylation in malignant gliomas depends on IDH1 mutation. Neurology 81:1515–1522
Weller M, Berger H, Hartmann C et al (2007) Combined 1p/19q loss in oligodendroglial tumors: predictive or prognostic biomarker? Clin Cancer Res 13:6933–6937
van den Bent MJ, Afra D, de Witte O et al (2005) Long-term efficacy of early versus delayed radiotherapy for low-grade astrocytoma and oligodendroglioma in adults: the EORTC 22845 randomised trial. Lancet 366:985–990
Shaw EG, Wang M, Coons SW et al (2012) Randomized trial of radiation therapy plus procarbazine, lomustine, and vincristine chemotherapy for supratentorial adult low-grade glioma: initial results of RTOG 9802. J Clin Oncol 30:3065–3070
Sun B, Chu D, Li W, Chu X, Li Y, Wei D, Li H (2009) Decreased expression of NDRG1 in glioma is related to tumor progression and survival of patients. J Neurooncol 94:213–219
Northcott PA, Shih DJ, Peacock J et al (2012) Subgroup-specific structural variation across 1,000 medulloblastoma genomes. Nature 488:49–56
Weiler M, Blaes J, Sahm F et al (2013) mTOR target NDRG1 confers MGMT-dependent resistance to alkylating chemotherapy. Proc Natl Acad Sci USA. doi:10.1073/pnas.1314469111
Louis DN, Ohgaki H, Wiestler OD et al (2007) The 2007 WHO classification of tumors of the central nervous system. Acta Neuropathol 114:97–109
Pignatti F, van den Bent M, Curran D et al (2002) Prognostic factors for survival in adult patients with cerebral low-grade glioma. J Clin Oncol 20:2076–2084
Bruna A, Darken RS, Rojo F et al (2007) High TGFbeta-Smad activity confers poor prognosis in glioma patients and promotes cell proliferation depending on the methylation of the PDGF-B gene. Cancer Cell 11:147–160
Riemenschneider MJ, Jeuken JW, Wesseling P, Reifenberger G (2010) Molecular diagnostics of gliomas: state of the art. Acta Neuropathol 120:567–584
Tabatabai G, Stupp R, van den Bent MJ et al (2010) Molecular diagnostics of gliomas: the clinical perspective. Acta Neuropathol 120:585–592
Koelsche C, Sahm F, Capper D et al (2013) Distribution of TERT promoter mutations in pediatric and adult tumors of the nervous system. Acta Neuropathol 126:907–915
Wiestler B, Capper D, Holland-Letz T et al (2013) ATRX loss refines the classification of anaplastic gliomas and identifies a subgroup of IDH mutant astrocytic tumors with better prognosis. Acta Neuropathol 126:443–451
Kurdistani SK, Arizti P, Reimer CL, Sugrue MM, Aaronson SA, Lee SW (1998) Inhibition of tumor cell growth by RTP/rit42 and its responsiveness to p53 and DNA damage. Cancer Res 58:4439–4444
Maruyama Y, Ono M, Kawahara A et al (2006) Tumor growth suppression in pancreatic cancer by a putative metastasis suppressor gene Cap43/NDRG1/Drg-1 through modulation of angiogenesis. Cancer Res 66:6233–6242
Yan X, Chua MS, Sun H, So S (2008) N-Myc down-regulated gene 1 mediates proliferation, invasion, and apoptosis of hepatocellular carcinoma cells. Cancer Lett 262:133–142
Bandyopadhyay S, Pai SK, Hirota S et al (2004) Role of the putative tumor metastasis suppressor gene Drg-1 in breast cancer progression. Oncogene 23:5675–5681
Koshiji M, Kumamoto K, Morimura K et al (2007) Correlation of N-myc downstream-regulated gene 1 expression with clinical outcomes of colorectal cancer patients of different race/ethnicity. World J Gastroenterol 13:2803–2810
Chua MS, Sun H, Cheung ST et al (2007) Overexpression of NDRG1 is an indicator of poor prognosis in hepatocellular carcinoma. Mod Pathol 20:76–83
Nishio S, Ushijima K, Tsuda N et al (2008) Cap43/NDRG1/Drg-1 is a molecular target for angiogenesis and a prognostic indicator in cervical adenocarcinoma. Cancer Lett 264:36–43
Acknowledgments
This work was supported by the German Cancer Aid with a program project grant for the German Glioma Network, within the Brain Tumor Network (BTNplus; Subproject 6) of the National Genome Research Network (NGFNplus) by the Federal Ministry of Education and Research (BMBF), and the Hertie Foundation. J.B., C.T. and M.S. are doctoral students in the PhD Program of the DKFZ.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
J. Blaes, M. Weiler, and F. Sahm have contributed equally to this study.
Rights and permissions
About this article
Cite this article
Blaes, J., Weiler, M., Sahm, F. et al. NDRG1 prognosticates the natural course of disease in WHO grade II glioma. J Neurooncol 117, 25–32 (2014). https://doi.org/10.1007/s11060-013-1357-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-013-1357-2