Abstract
Africa is experiencing an exponential increase in the number of older persons. The number of persons surviving with human immunodeficiency virus is simultaneously increasing due to improved availability of anti-retroviral therapy. The burden of non-communicable diseases, in particular, osteoporosis and its consequent fragility fractures, is also predicted to increase. Osteoporosis, however, remains a neglected disease and there are no age-standardized reference data available to accurately screen and diagnose individuals with osteoporosis. Epidemiological studies reporting the incidence of hip fracture or vertebral fractures are limited from Africa, especially Sub-Saharan Africa. The studies are usually limited as they are based on a retrospective data and small study numbers and often from a single study site. However, compared with early initial studies, the more recent studies show that osteoporosis and fractures are increasing across the continent. The overall incidence rates for osteoporosis and fractures still vary greatly between different regions in Africa and ethnic groups. Predisposing factors are similar with those in developed countries, but awareness of osteoporosis is sorely lacking. There is a lack of awareness among the population as well as health authorities, making it extremely difficult to quantify the burden of disease. There is great potential for research into the need and availability of preventive strategies. The FRAX® tool needs to be developed for African populations and may circumvent the shortage of bone densitometry.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Osteoporosis (OP) has been neglected as a health priority in Africa, especially Sub-Saharan Africa, for several reasons. Health authorities are overwhelmed by the burden of communicable diseases such as tuberculosis (TB) and human immunodeficiency virus (HIV), among others. There is a perception that OP and its consequent fragility fractures are rare among Black Africans [1]. Dual x-ray absorptiometry (DXA) equipment for measurement of bone mineral density (BMD) is not widely available, hampering early diagnosis and treatment [1]. Life expectancy in Africa has increased significantly in the last two decades. The population of people aged 60 years and over is expected to triple across the continent, from 46 million in 2015 to 147 million by the year 2050 [2]. The combination of an expected increase in the aged population, rapid urbanization, and changes in secular trends in Africa is anticipated to lead to a proportional rise in non-communicable diseases (NCD) including OP [2]. Despite this, health care policies towards ageing populations remain a low priority within African countries [1]. The challenges and opportunities relating to OP in developing countries, including several African countries, were last reviewed in 2008 [3].
The pathogenesis of OP is complex and the aetiology is multifactorial rendering reasonable grounds to suggest probable need for multimodal approaches to combat OP. Age and menopause play a major role in its development and the impact may be worsened by associated calcium deficiency, vitamin D deficiency, comorbid diseases like rheumatoid arthritis (RA), concomitant medications such as glucocorticoids, and reduced physical activity, to name a few [4]. Genetic factors are also implicated, but no candidate genes have yet been identified among several that have been studied [5]. Studies from the United States of America (USA) have shown differences in BMD between American Blacks and Whites [6, 7], suggesting importance of ethnic differences. This justifies implementation of local studies, especially in a continent with diverse cultures and ethnicities like Africa.
The most devastating consequence of OP is a hip fracture (HF). Experts predict that the number of HF, which are a surrogate marker for osteoporosis, will increase from the 1.26 million per year seen in 1990 to 4.5 million cases by the year 2050 [8]. Age-standardized rates for OP hip fractures are almost 200-fold and 140-fold higher in women and men respectively in developed countries than in developing countries [9]. Lower rates of HF are seen in Asia, Middle East, Oceania, Latin America, and Africa, but it is expected that by the year 2050, the highest proportionate increase in the number of hip fractures will occur in Africa [1]. Vertebral fractures (VF), on the other hand, are more common but often asymptomatic and probably under-reported [10, 11].
Epidemiology of osteoporosis and hip fractures in Africa
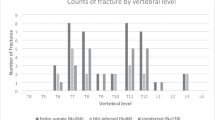
Whilst the incidence of OP is well established in developed countries, there are virtually no large population-based studies from Africa, especially from Sub-Saharan Africa [12] (Fig. 1). The major studies are summarized in Table 1. The incidence of OP in Egypt is estimated to be 21.9% in men and 28.4% in post-menopausal women (PMW) with 53.9% of woman having osteopaenia [13]. A subsequent study found a higher prevalence in rural PMW at 47.8% [14]. In Morocco, it is estimated that 13.4% of men aged 50 years and over and 44.6% of PMW have OP [15, 16]. The prevalence varies from 21 to 31% in other studies among PMW [17, 18]. The age-adjusted annual incidence for HF was 52.1/100,000 in women and 43.7/100,000 in men in a study in 2002 [19]. A study between 2006 and 2009 found a higher age-adjusted incidence of 85.9/100,000 in women and 72.7/100,000 in men [20]. Rates of OP are lower in Tunisia with 25% of PMW and 23.3% in healthy women [1, 21]. In 2002, a national study estimated that the incidence rate (IR) of HF was 213.5 per 100,000 per year [1]. Vertebral fractures were the commonest OP fractures and accounted for 60% of all fractures in PMW followed by wrist fractures (32%) [22]. The IR of OP in Algerian women is similar to that in Moroccan women at 35.8% [23]. In a retrospective study, 115 HFs were documented in an 18-month period out of a total of 486 fractures (16.8%) [24].
There are fewer studies from East and West Africa and geographic differences are observed between East and West Africa. Early studies from Gambia showed no HFs, despite Gambian women having a lower BMD and BMC at the lumbar spine and radius compared with White women from the United Kingdom (UK) [25]. Studies show that OP is 80 times more common among East Africans with higher levels of lactase persistence than lactase non-persistence among West Africans [26]. In the first prospective longitudinal study from Gambia in patients aged > 40 years in 2012, self-reported HF rates were still low and between 0.4 and 3% only. Using the Lunar DXA machine, VF prevalence was found to be 9%, with 6% in men and 3% in women [27].
An early study from Kenya (2004) found OP in 24.3% and osteopaenia in 32% of PMW, respectively [28]. A later study confirmed an OP incidence rate of 243 per 100,000 in women aged 50 years and over, leading to a call to treat all patients aged 75 years and over with fragility fractures with OP medications . However, HF rates were low and only 15 HFs were documented in the period 1998–2007 in a single hospital study [28, 29]. In a 5-year retrospective study from Tanzania, 222 patients sustained HF, of which 55.8% met the criteria for fragility fracture. The authors noted a 2.34% increase in fragility fractures per year over the 5-year period [31].
Initial studies from Nigeria reported a very low incidence of HF at 1.9 per 100,000 in women and 2.3 per 100,000 in men over 50 years in 1990 [32]. A subsequent study over the period 2002–2008 found a higher rate at 57.8 and 46.3 for men and women, respectively, in persons greater than 50 years old, especially in the > 80-year age group. The study documented 42 HFs, of which 68% occurred in women and men with a mean age of 67.5 years and 69.0 years, respectively [33]. An early study in pre- and post-menopausal women using broadband ultrasound (US) found that 24% of the women had T-scores indicative of osteopenia and 9% had T-scores indicative of OP, despite low fracture rates, based on US reference data [34]. In comparison, in a more recent study, Alonge et al. found a higher point prevalence of OP in persons aged 60 years and older at 56.9% (men [43.7%] and women [65.8%]) [35].
A small cross-sectional study from Cameroon in women 50 years and older found low rates of OP at 17.9%, which increased to 55.8% in women 70 years and older [36]. Fractures due to OP are uncommon in Cameroon with an IR of 4.1 in women, 2.2 in men for HF, and 1.2 in women and 0.2 in men for wrist fractures per 100,000 persons aged 35 years and older. The IR increased with age to 24.4 per 100,000 in persons aged 65 years or more. The mean age at fracture was lower than that of developed countries and this is partly due to decreased lifespan, as only 1.1% of women and 0.7% of men survived beyond the age of 65 years [37].
A retrospective study from Ethiopia in all fracture subjects found that 9.3% of all fractures were secondary to OP and the sex-specific prevalence rate was 9.5 and 8.9% for men and women, respectively [38]. In the single study from Senegal in 43 patients, only 35% of patients had osteopaenia and 26% had osteoporosis [39]. A study in 51 Zimbabwean men using DXA Hologic QDR found OP at the lumbar spine (LS) in 24% of subjects and in 6% at the proximal femur (PF) using the White NHANES III reference range compared with 29% and 6% using African American reference data. [40]. In a cross-sectional study in 518 healthy pre-menopausal Black Ugandan and Zimbabwean women, BMD findings were similar to US reference population with osteopaenia in 35.3% for LS and 9.7% for total hip (TH) and OP in only 1.5% for LS and 0.2% for TH [41].
In the first South African study of normative BMD data, Kalla et al. showed a prevalence of osteopenia of 16% in the lumbar region and a prevalence of 24% at Ward’s area. There were no significant differences in LS or PF BMD between White and Coloured women, but there were significant differences from US reference values, especially in women aged 50 years and over [42]. In another study, Black women were found to have a higher PF BMD than White women in the pre-menopausal, perimenopausal, and post-menopausal groups of 7, 10, and 13%, respectively [43]. Additional studies highlight that using White or African American reference ranges may not be appropriate in African Blacks as there are differences, including genetics and hip geometry, among other factors [43, 44]. Daniels et al. also showed that bone mineral apparent density (BMAD) was higher at the femoral neck (FN) and LS in Black women than in White women [43]. Similarly, Conradie et al. found FN and PF BMD were higher in Black women than in White women but that the LS BMD was lower in Black women than in White women, after adjusting for differences in body size [45]. The ethnic differences in BMD findings are thought to be due to differences in bone turnover, body fat composition, diet, socioeconomic status, contraceptive use, load bearing, and lifestyle (smoking, alcohol consumption) [46, 47].
In 1968, a historical study showed a 10 times lower fracture rate in urban Black men than in Whites with an IR of 5.2/100,000 persons [48]. Surprisingly, a parallel epidemiological metacarpal BMD study in 1969 showed age-matched Whites had better BMD than Blacks [49]. A second small study, which excluded persons with OP, found a higher IR of HF at 12.0 per 100,000 among Blacks (72 patients) [50]. In a HF study in 2011, Paruk et al. found an IR of 77.1 per 100,000 in Blacks in the public sector in eThekwini [51]. In a more recent study in both the public and private sectors in 2018, Dela et al. found an IR for HF of 68·6 per 100,000 for the total population and 87·5 and 46·2 per 100,000 for women and men, respectively. The highest HF IR was seen in White women of 176·0 per 100,000, followed by Indian women at 147·7 per 100,000 and Coloured women at 73·2 per 100,000 and the lowest in African women at 43·6 per 100,000. A similar pattern was observed in men, but at much lower rates with White men having the highest IR at 76·5 per 100,000. Men fractured at a younger age in the total group and in each ethnic group and HF IR increased with age in all ethnic groups [52]. Postulated factors responsible for differences in HF rates include differences in BMD, hip geometry, and bone morphology (thicker trabeculae, greater osteoid surface, volume and thickness, larger erosion surface) [46, 53, 54].
Whilst Dent et al. found a low rate of vertebral fracture (VF) in urban and rural Blacks compared with Whites in their study in 1968, which was based on lumbar radiographs [55], a recent study in woman aged 40 years and over by Conradie et al. showed a similar VF rate in Black (9.1%) and White (5.0%) women [56]. Risk factors for VF in Black women were a lower body weight and lower areal and volumetric BMD at all sites whilst older age, physical inactivity, decreased muscle strength, and low femoral BMD were risk factors in Whites. In addition, Basu et al. showed that 38% of Black women aged 60 years and over developed new vertebral deformities over a 5-year period [57].
Risk factors for osteoporosis
In Egyptian women aged 60 years and over, OP was associated with female gender, older age, a low body mass index, higher fall risk, and vitamin D deficiency in 60.9% of persons (vitamin D < 20 ng/mL) [58]. A Nigerian study confirmed that increasing age, female gender, lack of formal education, unemployment, sedentary lifestyle, peptic ulcer disease medication, and asthenic build contributed to HF risk [35]. In a Cameroon study, BMD findings were affected by menopause, inactivity, low calcium intake, and cigarette smoking [36]. In a comparative study, lower BMD was found in Ugandan people with lower BMI, physical inactivity, lactation, and contraceptive use [41]. In Algeria, the OP risk factors identified were female sex, advanced age, corticosteroid therapy, and sedentary lifestyle [24]
Studies show that after age and gender, body weight is one of the most important contributors to BMD. In pre-menopausal African and White women, fat-free soft tissue mass, although lower in African women, was the most significant contributor to BMD at all sites in African women but only the hip in White women [47]. Other risk factors identified in South African studies include greater than three pregnancies, physical exercise, load bearing, socioeconomic factors, type of contraceptive use, calcium and fat intake, and differences in bone geometry and genetics [45, 47, 56, 59, 60]
Role of HIV in Africa
The human immunodeficiency virus (HIV) epidemic has played a fundamental role in changing the landscape of Africa’s health issues in the last few decades. HIV is a multisystem disease and adversely affects bone and endocrine metabolism leading to a low BMD. Mechanisms include HIV effects on leptin, pro-inflammatory cytokines, and oestrogen. The low BMD in HIV patients is exacerbated by menopause and anti-retroviral treatment (ART) [61].
Studies show that in people living with HIV (PLWHIV), osteopenia is seen in 67% and osteoporosis in 15% of HIV-positive patients. In addition, BMD reduction is 6.4-fold higher and osteoporosis 3.7-fold higher in HIV-positive patients [62, 63]. The use of specific ART is associated with OP and increased fracture risk [62,63,64]. Several longitudinal studies in ART-naïve individuals showed that BMD decreases by 2–6% within 24–48 weeks after initiation of ART, after which BMD values remain stable or even increase slightly [64, 65]. The prevalence of OP is approximately three times higher in HIV-infected patients receiving ART than uninfected patients.
A study from Botswana in healthy persons aged 18–29 years old using pre-exposure prophylaxis (PrEP) found a high prevalence of low BMD (defined as a Z-score of more than 2.0 SD below the mean at any anatomic site: hip, spine, or forearm) of 6.8%. Men, interestingly, had a lower BMD compared with women (11.3% vs. 2.6%, p = 0.02), with 22% of women and 50% of men having osteopenia in the wrist, and 39% and 40% respectively in the LS. Hip osteopenia was less common, at 9% in women and 5% in men. The reasons for the lower BMD are not clear and possibly include biological factors or comparison with inappropriate reference ranges [66].
The prevalence of a low BMD was higher in healthy Malawian men compared with women who had been on ART for at least 1 year. The BMD was lower at LS than PF and a lower BMD was associated with decreased physical activity [67]. Among Nigerian PLWHIV, OP was found in 31.9% and osteopenia in 46.6% [68]. A higher prevalence of OP based on quantitative ultrasound (QUS) diagnosis was observed in Kenya in PLWHIV on an ART regimen in the 18–40-year age group (56.5%) compared with ART-naïve PLWHIV (32.6%) [65]. The prevalence was only 9.3% in HIV-negative persons. A lower BMD was associated with increasing age, and persons using ART also had a lower BMI and BMD than ART-naïve and HIV-negative patients (23.6%, 24.8%, and 26.1% respectively). This study failed to show a relationship between BMD and ART duration, lifestyle factors, steroid use, or level of physical activity. In pre-menopausal South African women with HIV, significant bone loss (2–3% annually), exceeding post-menopausal losses, has been reported [69]. The World Health Organization (WHO), however, acknowledges that despite the widespread use of ART among PLWHIV [70], there is no consensus opinion on effective strategies to manage the reduced BMD secondary to the use of ART [71].
Role of vitamin D in osteoporosis
Vitamin D deficiency is thought to be common in Africa, with approximately 50–90% of persons on the continent having hypovitaminosis D [1]. Vitamin D plays a pivotal role in regulation and metabolism of calcium, phosphorus, and bone formation and mineralization. Vitamin D deficiency is associated with low bone mass and osteoporosis [72]. Predictors for low vitamin D were older age, female gender, multiparity, type of clothing, low socioeconomic status, and urbanization [1]. A recent meta-analysis found a pooled prevalence of hypovitaminosis D status to be 18–46% (95% CI 10.66–27.78) using a cutoff of serum 25(OH)D concentration less than 30 nmol/L; 34–22% (95% CI 26.22–43.68) for a cutoff of less than 50 nmol/L; and 59–54% (95% CI 51.32–67.50) for a cutoff of less than 75 nmol/L. The study found that lower levels were more common in North and South Africa, urban areas, and women [73]. George et al., in a cross-sectional analysis of adult Black and Indian subjects in Johannesburg, South Africa (SA), found the prevalence of vitamin D deficiency (≤ 30 nmol/L) to be 3.0% in the Black and 15.0% in the Indian population [74]. In contrast, vitamin D deficiency and insufficiency was found in 65% of HF and matched control subjects aged 60 years in a recent study from Durban [75]. Whilst HIV is well associated with low vitamin D levels and OP, a study from Cape Town found that HIV-positive women did not have lower BMD or vitamin D levels than HIV-negative controls [76]. These studies show that vitamin D deficiency is associated with OP and HF, but there are several complex factors which influence vitamin D levels.
Glucocorticoid-induced osteoporosis
Glucocorticoid-induced bone loss is well described and the mechanisms are complex. Most studies include post-menopausal patients with underlying inflammatory diseases which may contribute to bone loss. Studies have been reported from a few African countries. Kalla et al., in a few studies in patients with RA and systemic lupus erythematosus (SLE), showed that the underlying disease may be more important than the use of glucocorticoids [77,78,79]. Menopause and reduced physical function may be contributory factors to the bone loss. Patients with SLE were found to have higher BMD than patients with RA, despite higher glucocorticoid doses. A study from Senegal failed to show a relationship between the prolonged use of glucocorticoids and OP [39], whilst other studies, in keeping with the literature, showed that glucocorticoids increase the risk of OP [14, 30].
Awareness, availability of testing and treatment, and national treatment guidelines for osteoporosis
The International Osteoporosis Foundation (IOF) audit of Africa and Middle East in 2011 found that generally in Africa, there is a limited awareness of OP and few countries have national guidelines or OP societies. Osteoporosis is usually not part of the undergraduate medical curriculum in medical schools across Africa [1].
The direct and indirect burden of OP in an African setting is also not quantified. There has been a slight shift in the last decade however, with several countries recognizing the need to address musculoskeletal health issues, especially with the impact of ageing and HIV on bone [27, 80]. As a result, several countries such as SA, Nigeria, Uganda, Gambia, and Kenya are among those who now have an osteoporosis society.
There are few studies on awareness in the general population, and they show that OP awareness varied substantially and tends to increase with age, gender, and employment status. The main source of information was often the media. Awareness among health care workers also varied, and effective training and promotion strategies are required [81,82,83]
Most countries have limited access to DXA machines, which are usually located in urban centres and in the private health care. The cost of DXA also varies in the public sector and usually it is not reimbursed by funders. Physicians usually follow international guidelines, and apart from SA, which has well-established OP guidelines, other countries do not have defined guidelines [1, 84]. There is an urgent need for African countries to develop awareness campaigns and introduce cost-effective screening and treatment algorithms for OP to address the projected increase in the disease burden. There is, however, the fear of over mobilization of demand through adequate awareness at population level, and failure to deliver on the intended services by relatively poor governments particularly in Africa.
Some of the limiting factors hindering uptake by end users (prescribers and patients) are drug availability, affordability, and lack of knowledge on current OP drugs regarding their safety profiles in the target age group which often has other medical comorbidities. This is a minimum required necessity to justify any effort to screen patients for OP, that is, assurance to treat.
Screening and fracture risk assessment
The DXA scan is recommended by the WHO as a gold standard for diagnosing OP. Because of its availability, related minimal radiation exposure, and simplicity of use, DXA is the most commonly used quantitative radiologic method to assess bone mass. However, routine measuring of BMD for all post-menopausal women is not feasible in some developed and many developing countries due to either lack of availability of the technology, deficiency of financial resources, or failure of medical aids to reimburse the test [85]. Bone mineral density alone without clinical risk factors is a poor predictor for fragility fractures [86], and DXA use is limited in different ethnic and age groups [87, 88]. There are several alternative imaging tools including quantitative computed tomography (pQCT) which can measure volumetric BMD, cortical and trabecular compartments separately which are useful options in determining bone strength [88]. These may be more feasible options in resource-limited settings [89].
Several screening tools using clinical risk factors which have been extensively validated have been developed. The ORAI, OSIRIS, SCORE, OPERA, OST, ABONE, and BWC were used in Egyptian elderly women and showed that 54.3% of elderly women had OP and 36.7% had osteopenia using DXA scan. This was higher than findings by Taha et al. [13] and the SCORE technique was superior to the other tools [90].
The WHO developed the Fracture Risk Assessment Tool (FRAX®) which determines the 10-year probability of the potential risk for future HF or major osteoporotic fractures in women and men between the ages of 40 and 90 years, by using different risk factors related to BMD [91]. The FRAX® tool is recommended as a validated screening tool and it has been validated in over 26 studies [89]. The use of FRAX® tool is dependent on a country having their own epidemiological data on HF incidence or the country should adopt another country as a surrogate marker. The limitations include, inter alia, that it does not take into account all clinical risk factors such as falls, cannot be used in patients already on treatment, and does not take into account subjects that that have multiple risk factors [92]. It also does not take into account the heterogeneous genetic and environmental exposures in African communities even within the same country. Ideally, we need to develop a FRAX® predictive tool specific for the African continent. This kind of study would need to first define the incidence of confirmed HFs in a target population. Such a study is currently underway in SA and some preliminary information has recently been published [52]. Presently, Tunisia and Morocco are the only two African countries that have their own FRAX® models [1].
Mortality and morbidity and health care costs
Osteoporosis, on its own, is not a direct cause of increased morbidity and mortality. However, the subsequent fractures result in significant mortality, morbidity, and loss of disability-adjusted life years (DALYs). In assessing the global burden of disease, OP itself was not considered a disease, but rather a low BMD which is a risk factor for fractures was included, as it contributes to the health burden of falls which was assessed. The study found that compared with the 1990 results, the 2010 estimates for global DALYs and deaths attributable to a low BMD had increased slightly from 12.1% and 29.6% to 14.8% and 34.7% for all fall-related DALYs and deaths, respectively. This confirmed that a low BMD and indirectly OP are a growing global health burden. Of concern is that there were only three studies from Sub-Saharan Africa that were available to be included in the analysis, suggesting a lack of research on the burden of chronic disease from this region [93].
The mortality associated with HF is still significantly high, even in developed countries like the UK, where, whilst the 30-day mortality has decreased to 6% due to intensive interventions, the 1-year mortality remains high at 30% [94, 95]. Mortality rates (MR) post-HF in Africa are postulated to be 2–3-fold higher than the reported rates of 25–30% in developed countries [1, 80]. There are only two small retrospective published studies from SA on HF morality showing a higher 30-day mortality rate than the UK. The first in 57 patients reported a MR of 14% and 32% at 30 days and 1 year respectively, which increased to 39% in the second year in patients aged 65 years and over [96]. Similar results were seen at 12.5% and 34.3%, at 30 days and 1 year respectively in patients who underwent cemented hemiarthroplasty for hip fracture [97].
There are no published studies on the long-term outcomes post-HF or health care costs associated with HF. Studies addressing these areas and determining available resources are urgently required.
Conclusion
An audit by the IOF in 2011 found a lack of large population studies, national registries, and an absence of clear terms of reference to assess osteoporosis outcomes in Africa and the Middle East. The audit noted that OP was a “neglected but highly prevalent disease” in Africa [1]. Genetics, ethnicity, lifestyle, comorbid diseases, concomitant medications, and differences in longevity may explain some of the apparent differences in IR across regions in the African continent. DXA machines are not widely available, and there is an urgent need to improve awareness among the general public as well as health authorities and to institute cost-effective preventive screening and treatment guidelines, to control this silent killer. The burden of HIV bone disease may contribute to the underlying burden of OP in the African continent, especially since the bone loss seems to be worse among men and at a younger age. Development of a country-specific FRAX® tool would be ideal, but would need large-scale epidemiological studies on HF incidence. The burden of OP on the African continent is currently unknown. Further studies on IR of HF and the concomitant morbidity and mortality will contribute to an understanding of the extent of the disease burden due to OP in Africa.
Data availability
Not applicable
References
Fuleihan GEH, Adib G, Itani N, Nauroy L, Arabi A, Baddoura R (2011) The Middle East & Africa regional audit. Osteoporos Int 22:S677–S678
World Health Organization: Africa: the time to ensure a healthy and dignified ageing for Africans is now. Available at https://www.afro.who.int/regional-director/regional-director-commentaries/time-ensure-healthy-and-dignified-ageing-africans. Accessed 4 Feb 2020
Handa R, Kalla AA, Maalouf G (2008) Osteoporosis in developing countries. Baillieres Best Pract Res Clin Rheumatol 22(4):693–708
Seeman E (2003) Pathogenesis of osteoporosis. J Appl Physiol 95:2142–2151. https://doi.org/10.1152/japplphysiol.00564.2003
Zmuda JM, Sheu YT, Moffett SP (2006) The search for human osteoporosis genes. J Musculoskelet Neuronal Interact 6(1):3–15
Araujo AB, Travison TG, Harris SS, Holick MF, Turner AK, McKinlay JB (2007) Race/ethnic differences in bone mineral density in men. Osteoporos Int 18:943–953. https://doi.org/10.1007/s00198-006-0321
Melton LJ (2001) The prevalence of osteoporosis: gender and racial comparison. Calcif Tissue Int:179–181. https://doi.org/10.1007/s00223-001-1043
Gullberg B, Johnell O, Kanis JA (1997) World-wide projections for hip fracture. Osteoporos Int 7(5):407–413
Cauley JA, Chalhoub D, Kassem AM, Fuleihan GEH (2014) Geographic and ethnic disparities in osteoporotic fractures. Nat Rev Endocrinol 10(6):338–351. https://doi.org/10.1038/nrendo.2014.51
Ensrud KE, Schousboe JT (2011) Vertebral fractures. N Engl J Med 364(17):1634–1642
Kanis JA, McCloskey EV (1994) Epidemiology of vertebral osteoporosis. Bone 13(Supple 2):S1–S10. ISSN 8756–3282. https://doi.org/10.1016/8756-3282(92)90189-4
Atiase Y, Quard A (2020) A call to action for osteoporosis research in sub-Saharan Africa. Ghana Med J 54(1):58–67. https://doi.org/10.4314/gmj.v54i1.9
Taha M (2011) Prevalence of osteoporosis in Middle East systemic literature review. In: Proceedings of the 10th ECOO. Cairo, Egypt. Available at http://www.scribd.com/doc/53103901/Osteopoorosis-Cairo-April-2011-v1. Accessed Jan 2020
Gheita TA, Hammam H (2018) Epidemiology and awareness of osteoporosis: a viewpoint from the Middle East and North Africa. Int J Clin Rheumatol 13(3):134–147. https://doi.org/10.4172/1758-4272.1000177
El Maghraoui A, Guerboub AA, Achemlal L, Mounach A, Nouijai A, Ghazi M, Bezza A, Tazi MA (2006) Bone mineral density of the spine and femur in healthy Moroccan women. J Clin Densitom 9(4):454–460
El Maghraoui A, Ghazi M, Gassim S, Mounach A, Ghozlani I, Nouijai A, Achemlal L, Bezza A, Dehhaoui M (2009) Bone mineral density of the spine and femur in a group of healthy Moroccan men. Bone 44(5):965–969
El Maghraoui A, Sadni S, El Maataoui A et al (2015) Influence of obesity on vertebral fracture prevalence and vitamin D status in postmenopausal women. Nutr Metab (Lond) 12:44
Bennani L, Allali F, Rostom S, Hmamouchi I, Khazzani H, El Manouri L, Ichchou L, Abourazzak FZ, Abouqal R, Hajjaj-Hassouni N (2009) Relationship between historical height loss and vertebral fractures in postmenopausal women. Clin Rheumatol 28:1283–1289
El Maghraoui A, Koumba BA, Jroundi I, Achemlal L, Bezza A, Tazi MA (2005) Epidemiology of hip fractures in 2002 in Rabat, Morocco. Osteoporos Int 16:597–602
El Maghraoui A, Ngbanda AR, Bensaoud N, Bensaoud M, Rezqi A, Tazi MA (2013) Age-adjusted incidence rates of hip fractures between 2006 and 2009 in Rabat, Morocco. Osteoporos Int 24(4):1267–1273. https://doi.org/10.1007/s00198-012-2061-3
Sahli H, Testouri N, Ben CM et al (2009) Bone mineral density in healthy Tunisian women. Maturitas. 63(3):227–232
Sellami S, Sahli H, Meddeb N, Hamza S, Chahed M, Ben M’Barek R, Zouari B, Ladab F (2006) Prevalence of osteoporotic fractures in Tunisian women. Rev Chir Orthop Reparatrice Appar Mot 92:490–494. https://doi.org/10.1016/s0035-1040(06)75836-6. Abstract in English
Haouichat C, Hammoumraoui N, Lehtihet S et al (2014) SAT0461 Prevalence of postmenopausal osteoporosis in Algerian women. Ann Rheum Dis 73:760
Zehraoui N, Saidi N, Hafirassou H et al (2019) AB0834 Frequency of osteoporotic hip fracture in an Algerian hospital. Ann Rheum Dis 78:1887
Asprey TJ, Prentice A, Cole TJ et al (1996) Low bone mineral content is common but osteoporotic fractures are rare in elderly rural Gambian women. J Bone Miner Res 11(7):1019–1025
Hilliard CB (2016) High osteoporosis risk among East Africans linked to lactase persistence genotype. Bone Key Rep 5:803. https://doi.org/10.1038/bonekey.2016.30
Zengin A, Fulford AJ, Sawo Y, Jarjou LM, Schoenmakers I, Goldberg G, Prentice A, Ward KA (2017) The Gambian bone and muscle ageing study: baseline data from a prospective observational African Sub-Saharan study. Front Endocrinol 8:219. https://doi.org/10.3389/fendo.2017.00219
Odawa F, Ojwang S, Muia N (2004) The prevalence of post-menopausal osteoporosis in black Kenyan women. J Obstet Gynaecol 17(Supp 1):45–46
Gakuu LN (2010) The challenge of fracture management in osteoporotic bones. East Afr Orthopaed J 4(1). https://doi.org/10.4314/eaoj.v4i1.63606
Oyoo GO, Kariuki JG (2008) Osteoporosis-from hormonal replacement therapy to bisphosphonates and beyond: a review. East Afr Med J 84:535
Tsabasvi M, Davey S, Temu R (2017) Hip fracture pattern at a major Tanzanian referral hospital: focus on fragility hip fractures. Arch Osteoporos 12:47. https://doi.org/10.1007/s11657-017-0338-
Adebajo AO, Cooper C, Grimley EJ (1997) Fractures of the hip and distal forearm in West Africa and the United Kingdom. Age Ageing 20(43):438. https://doi.org/10.1093/ageing/20.6.435
Jervas E, Onwukamuche CK, Anyanwu GE, Ugochukwu AI (2011) Incidence of Fall related hip fractures among the elderly persons in Owerri, Nigeria. Asian Journal of Med. Science. 3(3):110–114
VanderJagt DJ, Bond B, Dulai R et al (2001) Assessment of the bone status of Nigerian women by ultrasound and biochemical markers. Calcif Tissue Int 68:277–284. https://doi.org/10.1007/BF02390834
Alonge TO, Adebusoye LA, Ogunbode AM, Olowookere OO, Ladipo MM-A, Balogun WO, Okoje-Adesomoju V (2017) Factors associated with osteoporosis among older patients at the Geriatric Centre in Nigeria: a cross-sectional study. S Afr Fam Pract 59(3):87–93. https://doi.org/10.1080/20786190.2016.1272248
Singwe-Ngandeu M, Nko’o AS (2008) Bone mineral density in Cameroon women in Yaounde: an echographic study. Mali Med 23(1):21–26
Zebaze RM, Seeman E (2003) Epidemiology of hip and wrist fractures in Cameroon, Africa. Osteoporos Int 14:301–305
Bayray A, Enquselassie F, Gebreegziabher Z (2012) Magnitude and pattern of osteoporotic fractures among adults in Tigiray, Ethiopia; a retrospective hospital based study. Ethiop Med J 50:297–305
Diagne-Gueye NM, Soko TO, Diedhiou I, Ndiaye A (2016) DEXA contribution in bone densitometry evaluation on osteoporosis in Senegal: results of a study realized in African Black populations. Open J Rheumatol Autoimmune Dis 06:85–95. https://doi.org/10.4236/ojra.2016.64014
Mukwasi C, Dube S, Chingarande G, Majonga E, Karera A (2014) Bone mineral density in elderly black men attending parirenyatwa hospitalin harare. World J Med Sci 10:82–88. https://doi.org/10.5829/idosi.wjms.2014.10.1.81125
Mgodi NM, Kelly C, Gati B, Greenspan S, Dai JY, Bragg V, Livant E, Piper JM, Nakabiito C, Magure T, Marrazzo JM, Chirenje ZM, Riddler SA, MTN-003B Protocol Team (2015) Factors associated with bone mineral density in healthy African women. Arch Osteoporos 10:206. https://doi.org/10.1007/s11657-015-0206-7
Kalla A, Fataar A, Bewerunge L (1994) Assessment of age related bone loss in normal South African women by means of the Hologic QDR 1000 system. S Afr Med J 84:398–404
Daniels ED, Pettifor JM, Schnitzler CM, Russell SW, Patel DN (1995) Ethnic differences in bone density in female South African nurses. J Bone Miner Res 10(3):359–367
Mcveigh JA, Norris SA, Cameron N, Pettifor JM (2010) Associations between physical activity and bone mass in black and white South African children at age 9 yr. J Appl Physiol 97(3):1006–1012. https://doi.org/10.1152/japplphysiol.00068.2004
Conradie M, Conradie MM, Kidd M, Hough S (2014) Bone density in black and white South African women: contribution of ethnicity, body weight and lifestyle. Arch Osteoporos 9:193. https://doi.org/10.1007/s11657-014-0193-0
Schnitzler CM, Mesquita JM (2006) Cortical bone histomorphometry of the iliac crest in normal black and white South African adults. Calcif Tissue Int 79:373–382. https://doi.org/10.1007/s00223-006-0053
Chantler S, Dickie K, Goedecke JH, Levitt NS, Lambert EV, Evans J, Joffe Y, Micklesfield LK (2012) Site-specific differences in bone mineral density in black and white premenopausal South African women. Osteoporos Int 23(2):533–542. https://doi.org/10.1007/s00198-011-1570-9
Solomon L (1968) Osteoporosis and fracture of femoral neck in the South African Bantu. J Bone Surg 50B:2–13
Solomon L (1979) Bone density in ageing Caucasians and African populations. Lancet 1979:5
Schnaid E, MacPhail A, Sweet MB (2000) Fractured neck of femur in Black patients. J Bone Joint Surg (Br) 82(B):872–875
Paruk F, Matthews G, Cassim B (2017) Osteoporotic hip fractures in Black South Africans: a regional study. Arch Osteoporos 12(1):107. https://doi.org/10.1007/s11657-017-0409-1
Dela SS, Paruk F, Brown SL, Lukhele M, Kalla AA, Jordaan JD, Conradie M, Mohamed O, Chutterpaul P, Cassim B (2020) Ethnic and gender-specific incidence rates for hip fractures in South Africa: a multi-centre study. Bone 133:115253. https://doi.org/10.1016/j.bone.2020.115253
Micklesfield L, Norris S, Pettifor J (2011) Ethnicity and bone: a South African perspective. J Bone Miner Metab 29:257–267. https://doi.org/10.1007/s00774-011-0269-5
Cumming RG, Cauley JA, Palermo L et al (1994) Racial differences in hip axis lengths, might explain racial differences in hip fractures. Osteoporos Int 4:226–229
Dent CE, Engelbrecht HE, Godfrey RC (1968) Osteoporosis of lumbar vertebrae and calcification of abdominal aorta in women living in Durban. BMJ 4:76–79
Conradie M, Conradie MM, Scher AT, Kidd M, Hough S (2015) Vertebral fracture prevalence in black and white South African women. Arch Osteoporos 10:203. https://doi.org/10.1007/s11657-015-0203-x
Basu D (2010) Determination of bone mass and prevalence of vertebral deformities in postmenopausal black women in South Africa. PhD dissertation, University of the Witwatersrand, South Africa.
Farouk O, Mahran DG, Said HG, Alaa MM, Eisa AA, Said GZ, Rashed H, Ez-Eldeen A (2016) Hypovitaminosis D among patients admitted with hip fracture to a level-1 trauma center in the Sunny Upper Egypt: prevalence and associated correlates. Geriatr Orthop Surg Rehabil 7(3):148–152. https://doi.org/10.1177/2151458516655436
Lloyd R, Hind K, Micklesfield A, Lisa K, Sean C, Truscott JG, Parr B et al (2010) A pilot investigation of load-carrying on the head and bone mineral density in premenopausal, black African women. J Bone Miner Metab 28:185–190
Nelson DA, Pettifor JM, Barondess DA, Cody DD, Uusi-Rasi K, Beck TJ (2004) Comparison of cross-sectional geometry of the proximal femur in white and black women from Detroit and Johannesburg. J Bone Miner Res 19(4):560–565
Gennari L, Merlotti D, De Paola V, Calabro A, Becherini L, Martini G et al (2005) Estrogen receptor gene polymorphisms and the genetics of osteoporosis: a huge review. Am J Epidemiol 161:307–320
Kruger MJ, Nell TA (2017) Bone mineral density in people living with HIV: a narrative review of the literature. AIDS Res Ther 14:35. https://doi.org/10.1186/s12981-017-0162-y
Brown TT, Qaqish RB (2006) Antiretroviral therapy and the prevalence of osteopenia and osteoporosis: a meta-analytical review. AIDS 20:2165–2174
Stellbrink HJ, Orkin C, Arribas JR, Compston J, Gerstoft J, Van Wijngaerden E et al (2010) Comparison of changes in bone density and turnover with abacavir-lamivudine versus tenofovir-emtricitabine in HIV infected adults: 48-week results from ASSERT study. Clin Infect Dis 51:963–972
Abdullahi AM, Oyoo GO, Sheikh AM, Maritim MC, Kwasa JK (2016) Bone mineral density abnormalities in HIV infected patients and HIV negative respondents at Mbagathi Hospital using calcaneal quantitative ultrasound. Afr J Rheumatol 4(2):47–53
Kasonde M, Niska RW, Rose C, Henderson FL, Segolodi TM, Turner K, Smith DK, Thigpen MC, Paxton LA (2014) Bone mineral density changes among HIV-uninfected young adults in a randomised trial of pre-exposure prophylaxis with tenofovir-emtricitabine or placebo in Botswana. PLoS One 9(3):e90111
Chisati EM, Constantinou D, Lampiao F (2020) Reduced bone mineral density among HIV infected patients on anti-retroviral therapy in Blantyre, Malawi: prevalence and associated factors. PLoS One 15(1):e0227893. https://doi.org/10.1371/journal.pone.0227893
Alonge TO, Okoje-Adesomoju VN, Atalabi OM et al (2013) Prevalence of abnormal bone mineral density in HIV-positive patients in Ibadan, Nigeria. J West Afr Coll Surg 3(4):1–14
Hamill MM, Pettifor JM, Ward KA, Norris SA, Prentice A (2017) Changes in bone mineral density, body composition, vitamin D status, and mineral metabolism in urban HIV-positive South African women over 12 months. J Bone Miner Res 32(8):1615–1624
World Health Organization (2015) Global health sector response to HIV, 2000 – 2015: focus on innovations. Progress Report Available at https://www.who.int/hiv/pub/progressreports/2015-progress-report/en/. Accessed 3 Mar 2020
Matovu FK, Wattanachanya L, Beksinska M, Pettifor JM, Ruxrungtham K (2016) Bone health and HIV in resource-limited settings: a scoping review. Curr Opin HIV AIDS 11(3):306–325. https://doi.org/10.1097/COH.0000000000000274
Bishof-Ferrari HA (2007) How to select the doses of vitamin D in the management of osteoporosis. Osteoporos Int 18:401–407
Mogire RM, Mutua A, Kimita W, Kamau A et al (2020) Prevalence of vitamin D deficiency in Africa: a systematic review and meta-analysis. Lancet Glob Health 8:e134–e142. https://doi.org/10.1016/S2214-109X(19)30457-7
George JA, Norris SA, van Deventer HE, Crowther NJ (2013) The association of 25 hydroxyvitamin D and parathyroid hormone with metabolic syndrome in two ethnic groups in South Africa. PLoS One 8(4):e61282. https://doi.org/10.1371/journal.pone.0061282
Chutterpaul P, Paruk F, Cassim B (2019) Prevalence of vitamin D deficiency in older South Africans with and without hip fractures and the effects of age, body weight, ethnicity and functional status. J Endocrinol Metab Diabetes S Afr 24(1):10–15. https://doi.org/10.1080/16089677.2018.1534360
Hamill MM, Ward KA, Pettifor JM, Norris SA, Prentice A (2013) Bone mass, body composition and vitamin D status of ARV-naive, urban, black South African women with HIV infection, stratified by CD 4 count. Osteoporos Int 24(11):2855–2861
Kalla AA, Fataar AB, Jessop SJ, Bewerunge L (1993) Loss of trabecular bone mineral density in systemic lupus erythematosus. Arthritis Rheum 36:1726–1734
Kalla AA, Meyers OL, van Wyk Kotze TJ, Laubscher R (1995) Corticosteroid therapy and bone mass - comparison of systemic lupus erythematosus and rheumatoid arthritis. S Afr Med J 84(7):404–409
Kalla AA, Bewerunge L, Langley A, Meyers OL, Fataar AB (2002) Trabecular bone density in premenopausal rheumatoid arthritis patients. S Afr Med J 92(1):62–68
Gregson CL, Cassim B, Micklesfield LK, Lukhele M, Ferrand RA, Ward KA, on behalf of the SAMSON Collaborative Working Group et al (2019) Fragility fractures in sub-Saharan Africa: time to break the myth. Lancet Glob Health 7(1):26–E 27
Njeze Ngozi R, Ikechukwu O, Miriam A et al (2017) Awareness of osteoporosis in a polytechnic in Enugu, South East Nigeria VL. Arch Osteoporos 12(1):51. https://doi.org/10.1007/s11657-017-0342-3
El-Tawab SS, Saba EKA, Elweshahi HMT et al (2016) Knowledge of osteoporosis among women in Alexandria (Egypt): a community based survey. Egypt Rheumatol 38(3):225–231
Hassan NE, Shebini SME, El-Masry SA et al (2019) Inter-relationship of awareness, knowledge, attitude, some socio-economic variables and osteoporosis in sample of Egyptian women. Open Access Maced J Med Sci 7(15):2538–2544. https://doi.org/10.3889/oamjms.2019.707
Hough S, Ascott-Evans BH, Brown SL, Cassim B, de Villiers TJ, Lipschitz S, Pettifor JM, Sonnendecker EWW (2010) NOFSA guideline for the diagnosis and management of osteoporosis. J Endocrinol Metab Diabetes S Afr 15(3):107–108. https://doi.org/10.1080/22201009.2010.10872239
Richy F, Ethgen O, Bruyere O, Mawet A, Reginster JY (2004) Primary prevention of osteoporosis: mass screening scenario or prescreening with questionnaires? An economic perspective. J Bone Miner Res 19:1955–1960. https://doi.org/10.1359/jbmr.040903
Sornay-Rendu E, Munoz F, Garnero P (2005) Identification of osteopaenic women at high risk of fracture: the OFELY study. J Bone Miner Res 20(10):1813–1819
Prentice A (2004) Diet, nutrition and the prevention of osteoporosis. Public Health Nutr 7(1A):227–243. https://doi.org/10.1079/PHN2003590
Zengin A, Prentice A, Ward KA (2015) Ethnic differences in bone health. Front Endocrinol 6:24. https://doi.org/10.3389/fendo.2015.00024
Marques A, Ferreira RJ, Santos E et al (2015) The accuracy of osteoporotic fracture risk prediction tools: a systematic review and meta-analysis. Ann Rhem Dis 74:1958–1967. https://doi.org/10.1136/annrheumdis-2015-207907
Abou-Hashem RM, Abd-El-Gawad WA, Abouseif HA (2019) Modified SCORE tool for prediction of bone mineral density in Egyptian elderly women. Comparison of seven osteoporosis screening tools. Health Care Women Int 40(10):1084–1100. https://doi.org/10.1080/07399332.2018.1542433
Kanis JA, Oden A, Johansson H, Borgström F, Ström O, Mccloskey E (2009) FRAX and its application in clinical practice. Bone. 44:734–743
Dawson-Hughes B, Tosteson AN, Melton L, Baim S, Favus MJ, Khosla S et al (2008) Implications of absolute fracture risk assessment for osteoporosis practice guidelines in the USA. Osteoporos Int 19(4):449–458
Sànchez-Riera L, Carnahan E, Vos T, Veerman L, Norman RE, Lim SS, Hoy DG, Smith E, Wilson N, Nolla JM, Chen JS, Macara M, Kamalaraj N, Li Y, Kok C, Santos-Hernández C, March L (2014) The global burden attributable to low bone mineral density. Ann Rheum Dis 73(9):1635–1645
National Hip Fracture Database (NHFD) Annual Report (2018) Available online at https://www.nhfd.co.uk/. Accessed Feb 2020
Neuburger J, Currie C, Wakeman R, Tsang C, Plant F, De Stavola B et al (2015) The impact of a national clinician-led audit initiative on care and mortality after hip fracture in England: an external evaluation using time trends in non-audit data. Med Care 53(8):686–691
Ngobeni RS (2010) Mortality in elderly patients with intertrochanteric fractures: three years’ experience. SAOJ 9(1):55–60
Du Toit AL, Van der Merwe JF (2018) Mortality following hip fractures managed with hemiarthroplasty in the elderly in South Africa. SAOJ 17(3):30–34
Map of Africa; available at https://mapchart.net/world.html. Accessed 15 May 2020
Author information
Authors and Affiliations
Contributions
FP, AAK, and MT: literature review and manuscript preparation
Corresponding author
Ethics declarations
Disclosures
None.
Ethics approval
Not applicable
Consent to participate
Not applicable
Consent for publication
Not applicable
Code availability
Not applicable
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Rheumatology in Africa
Rights and permissions
About this article
Cite this article
Paruk, F., Tsabasvi, M. & Kalla, A.A. Osteoporosis in Africa—where are we now. Clin Rheumatol 40, 3419–3428 (2021). https://doi.org/10.1007/s10067-020-05335-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05335-6