Abstract
Summary
Ethnic differences in bone mineral density (BMD) between healthy adult black and white South African women were studied. Higher BMD was only noted at the femoral sites in black women. Body weight significantly impacted these findings. A lower fracture risk at all skeletal sites cannot be assumed in black South African (SA) women.
Purpose
Bone mineral density (BMD) varies amongst women of different ethnicities. African-Americans have higher BMD at all skeletal sites compared with whites. On the African continent, bone density studies suggest site-specific ethnic differences in BMD. To examine the contribution of body weight and lifestyle characteristics to ethnic differences in BMD between adult black and white South African women, we assessed lumbar spine (SBMD), femoral neck (FNBMD) and total femoral BMD (FTBMD) by dual-energy X-ray absorptiometry (DXA) in 184 black and 143 white women aged between 23 and 82 years.
Methods
BMDs were compared amongst pre- and postmenopausal blacks and whites before and after adjustment for covariates with significant univariate association with BMD. Volumetric bone mineral apparent density (BMAD) of the spine and femoral neck was also calculated to account for ethnic differences in bone size.
Results
Before adjustment, SBMD was lower (p < 0.05), FTBMD similar and FNBMD (p < 0.01) higher in premenopausal black women. Similar SBMD, but significantly higher BMD at the femoral sites (p < 0.01), was noted in postmenopausal blacks compared with whites. Amongst anthropometric measures and lifestyle factors, only adjustment for weight significantly altered these observed ethnic differences in bone density. After adjustment for weight, SBMD remained lower in premenopausal blacks and became lower in young postmenopausal blacks. Weight adjustment eliminated all ethnic differences in proximal femoral BMD measurements, with the exception of FNBMD that remained higher in younger postmenopausal blacks. Before adjustment, calculated SBMAD was similar and FNBMAD consistently higher in blacks in all the menstrual groups. Adjustment for weight did not alter these findings.
Conclusion
Most of the observed ethnic difference in BMD was explained by differences in body weight between black and white SA women. The higher femoral BMD in older blacks may explain, the lower hip fracture prevalence in black South African women. The lower SBMD in pre- and postmenopausal black women in this study suggests that factors other than BMD should be considered to explain a lower vertebral fracture prevalence in blacks, if a lower fracture prevalence does indeed exist.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ethnic differences in bone mineral density (BMD) and fracture risk are well recognized. People of African ancestry have a lower incidence of fragility fracture than Caucasians as shown by studies on the African continent [1–3] and in the USA [4–7]. Fracture data relating to populations on the African continent are, however, limited, old and mostly confined to reports on non-vertebral fracture prevalence. Recent radiological assessment of prevalent vertebral fractures has suggested that the difference in vertebral fracture prevalence between elderly African-Americans (AA) and Caucasians may be considerably smaller (only 1.3 times higher) than what is previously reported in population studies [7].
Higher BMD in both the axial and appendicular skeletons has been consistently and repeatedly documented in African-American women compared with their white counterparts [4, 8–12], and these differences may account for their lower incidence of osteoporotic fractures at all skeletal sites [4–7]. Some of the ethnic differences in BMD may be due to ethnic differences in bone size that produce a scale artefact when BMD is measured by two-dimensional areal absorptiometry [13, 14], but important ethnic differences in BMD remain after adjustment for such artefacts [8, 9, 12]. On the African continent, data on greater bone density in blacks compared with whites are not nearly as convincing. Limited studies conducted in West African populations [2, 15–17] and in selected South African female cohorts [18, 19] have reported similar lumbar spine BMD, but higher femoral bone density in black women compared with whites.
It is expected that the shared genetic phenotype of black populations in America and on the African continent [20] will ensure comparable bone mineral density in these populations and thus protect them against osteoporosis and fragility fractures in a similar fashion. Attainment of peak bone mass and subsequent bone loss is, however, the result of an interplay between genetics and the environment. Exposure to adverse environmental factors may, in part, explain why black populations on the African continent do not realize their genetic potential at all skeletal sites.
The aims of the present study were to study BMD in adult black and white pre- and postmenopausal South African women and to evaluate the impact of lifestyle characteristics and anthropometry, especially total body weight, on ethnic differences in bone density.
Materials and methods
Study population
The study was descriptive and cross sectional. The study population consisted of a convenience sample of 184 black and 142 white premenopausal and postmenopausal South African women between the ages of 23 and 82 years. Volunteer subjects were recruited by word of mouth and through local church and community centres from the geographical area normally supplied of medical care by the Tygerberg Academic Hospital near Cape Town. Black and white races were determined by self-declaration, and all women were residents in the Western Cape for the majority of their adult lives. Due to known socioeconomic and anthropometric differences between the two ethnic groups, recruitment aimed to include a representative sample of black and white SA females and did not specifically stratify subjects based on socioeconomic status or anthropometry.
Subjects were excluded if they had known metabolic bone diseases, suffered from diseases (e.g. endocrinopathies, malabsorption syndromes, malignancies, chronic alcoholism, renal or hepatic dysfunction), were taking medications (e.g. postmenopausal oestrogen therapy, glucocorticoids, anticonvulsants and any bone specific agent) known to affect bone metabolism or if they were pregnant or lactating. Subjects were classified as premenopausal (n = 163) if they reported monthly menstrual bleeding during each of the three months preceding study entry and were only eligible for study entry if they reported a regular menstrual cycle. Subjects with either a clinical menopause (cessation of menses for >1 year) and/or chemical menopause (FSH values greater than 40 mIU/l) were defined as postmenopausal (n = 163).
Written informed consent was obtained from each subject, the research complied with the World Medical Association Declaration of Helsinki—ethical principles for medical research involving human subjects—and the study was approved by the Ethical Review Board of the Faculty of Medicine, University of Stellenbosch.
Demographic data
A standardized interviewer-administered questionnaire was used to assess the following parameters with a potential impact on BMD: age (years), physical activity (a numerical score 0–5 based on active living, in-house and recreational physical activity), alcohol intake (units per week, a unit being equivalent to 28 g alcohol), cigarette smoking (expressed as ever, current or never and number of pack years), calcium intake (mg/day, dietary recall obtained by a qualified dietician during a personal interview) and a gynaecological history (age at menarche (years), number of prior pregnancies, breastfeeding, the use of oral or injectable hormonal contraception and menopausal status).
Anthropometry
All the anthropometric measurements were made by a single observer. All subjects were weighed on the same balanced beam scale. Height was measured with a stadiometer with a sliding headpiece to increase the accuracy of the reading. Waist circumference was determined in the erect position through a point one third of the distance between the xiphoid process and the umbilicus. Hip circumference was assessed in the erect position, through a point 4 cm below the superior anterior iliac spine, and elbow breadth was measured with a sliding calliper to the nearest 0.1 cm, at the point of the greatest breadth across the joint. Body mass index (BMI) was calculated as weight/(height)2 in kilogramme per metre squared [21].
Densitometry
Bone mineral content (BMC), bone area (BA) and bone mineral density (BMD) of the lumbar spine (L1–L4) and proximal femur were quantitated by employing dual-energy X-ray absorptiometry (Hologic DXA). A spine phantom was scanned weekly to determine the intrinsic coefficient of variation of the machine—this varied by less than 1 %. A single trained DXA technician performed scans on all study subjects, and the intra-operative variation was found to be less than 2.5 %
Bone mineral density was expressed as an absolute value (g/cm2) in all menstrual groups and as a deviation from the norm, defined as a T-score, in postmenopausal women only. We used the uniform NHANES III reference database for whites [22] to calculate T-scores for both ethnic groups. We used the WHO criteria [23], based on T-scores, to diagnose osteopenia and osteoporosis in postmenopausal women.
Areal BMD measurements by DXA introduce a scale artefact that causes small bones to have lower areal BMD than larger bones. When comparing people from different ethnic groups with potential differences in bone size, BMD differences may thus be more apparent than real. This scale artefact was reduced by expressing BMD as BMAD, a calculated three-dimensional variable that helps account for differences in bone size. BMAD at the lumbar spine (in g/cm3) was calculated as the mean BMC/(mean area)3/2 using the method of Carter et al. [13]. BMAD at the femoral neck (in g/cm3) was calculated as the BMC/(area)2 using the method of Katzman et al. [14].
In an attempt to assess ethnic differences in BMD at a time of expected peak BMD and following the impact of ageing, bone density was measured in premenopausal (aged 23–46 years), early postmenopausal (aged younger than 60 years with clinical or chemical menopauses) and late postmenopausal subjects (aged 60 years and older). To control for adiposity, data was also analyzed by dividing pre- and postmenopausal subjects into weight subgroups, i.e. a subgroup with normal-to-low body mass index (BMI < 25 kg/m2) and a subgroup defined as overweight (BMI ≥ 25 kg/m2) [21].
Statistical analysis
The statistical analysis was conducted by a qualified statistician (MK) using Statistica 7.1 software. Cross tabulation and the chi-square test were used to compare categorical variables. Spearman correlation was used for comparing continuous variables. One-way analysis of variance and analysis of covariance were used for comparing measurements between groups. A probability value (p) ≤0.05 was used as guideline for determining statistical significance. For all skeletal sites, BMDs and BMADs were first compared between the ethnic subgroups by ANOVA before adjustment for covariates. To determine whether observed ethnic differences in bone mineral status were due to ethnic factors, the differences were re-compared after adjustment for certain covariates. Analysis of covariance was performed to identify covariates with significant univariate association with lumbar and femoral BMD and BMAD. For the premenopausal subjects, covariates included ethnicity, age, weight, height, daily calcium intake, pack years of smoking, alcohol intake, physical activity, age at menarche, hormonal contraception and number of prior pregnancies. For the postmenopausal subjects, covariates included years since menopause in addition to the abovementioned. For post hoc testing, the Bonferroni test was used. To evaluate potential ethnic differences regarding the association of BMD parameters with age, a general regression model was used including age and race × age interactions.
Results
Clinical demographic characteristics
Table 1 shows baseline characteristics for the DXA cohort within the different ethnic and menstrual groups. Blacks were shorter and heavier with greater BMIs than whites. The weight difference was accentuated with ageing with an average 14-kg difference in weight between older black and white women. Blacks reached menarche at a later age and had greater number of pregnancies. A younger age at menopause and more years since menopause were only observed in the younger postmenopausal black women compared with whites. Blacks preferred progestogen-only injectable contraception, and ever use was mostly reported by the younger black females, whereas whites almost exclusively used oral oestrogen-containing contraception. Dietary calcium intake was significantly lower in blacks; they smoked less but were also less active post menopause. Mean alcohol consumption was low and comparable between the two ethnic groups.
The baseline clinical characteristics of the normal-low and overweight groups are shown in Table 2. The majority of black premenopausal females were overweight (74 %), whereas most white women had BMIs in the normal-to-low BMI range (62 %). In the normal-to-low BMI subgroup, there was no ethnic difference in mean BMI, but black females were significantly smaller with lower weight and height. The overweight premenopausal blacks were significantly heavier with greater BMIs than whites. The waist-hip ratio was similar in premenopausal normal weight and overweight blacks and whites. Based on BMI, the majority of both postmenopausal blacks (77 %) and postmenopausal whites (59 %) were categorized as overweight. In the normal-low weight postmenopausal women, the mean BMI was significantly higher in postmenopausal blacks. Although blacks tended to be heavier and shorter, the difference in weight and height between the two ethnic groups was not significant. All the anthropometric variables were significantly higher in the overweight postmenopausal blacks compared with whites.
Lumbar spine bone mineral density
Mean lumbar spine bone mineral content (SBMC), lumbar spine bone area (BA) and unadjusted lumbar spinal bone mineral density (SBMD) were significantly lower in premenopausal blacks compared with whites (Table 3). Univariate tests of significance identified ethnicity, body weight (p < 0.01) and height (p < 0.01) to be significantly associated with SBMD. After adjustment for weight as a covariate, mean SBMD remained significantly lower in the black cohort (p < 0.01).
In postmenopausal women, mean SBMC was similar in the blacks and whites, spine BA was significantly lower in the black females (p = 0.01) and unadjusted mean SBMD was similar in both the early and late postmenopausal black and white women. In the early and late postmenopausal groups, body weight (p < 0.01) was positively associated with SBMD. After adjustment for weight as a covariate, SBMD was significantly lower in the black females compared with whites in the early postmenopausal group (p = 0.01), whereas SBMD remained similar in the late postmenopausal cohorts (p = 0.18). Mean SBMD in the early and late postmenopausal black groups was near identical, but tended to be lower in the late postmenopausal white female group compared with the early postmenopausal white group (p = 0.07). This may suggest that, compared with blacks, more pronounced postmenopausal lumbar spine bone loss occurred in white females with ageing. SBMAD was similar between black and white women in all the menstrual groups, before and after adjustment for covariates.
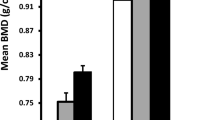
Weight was the only anthropometric variable that correlated significantly and positively with SBMD (Fig. 1) and SBMAD in all the menstrual subgroups. In the normal-low weight subgroup, SBMD was lower in the premenopausal and postmenopausal black females compared with whites (p ≤ 0.05), but similar in the overweight group (Table 4). Within the two ethnic groups, significantly lower SBMD was documented in premenopausal and postmenopausal black women of normal weight compared to their overweight counterparts (p ≤ 0.01). The mean SBMD of premenopausal and postmenopausal white women in the two weight subgroups was similar.
Femoral bone mineral density
The BMC of the femoral neck was similar in the premenopausal black and white subjects; the mean bone area (BA) of the femoral neck was significantly smaller in the black cohort, and this resulted in blacks having higher mean unadjusted femoral neck bone mineral density (FNBMD) than whites (Table 5). Weight and height were found to be significantly (p < 0.01) and positively associated with FNBMD. After adjustment for weight as a covariate, the difference in mean FNBMD between the two cohorts was non-significant. The BMC of the total femoral area tended to be lower; the mean total femoral BA was significantly smaller in blacks, with similar mean unadjusted total femoral bone mineral density (FTBMD) in the two cohorts. Weight and height (p < 0.01) were significantly associated with FTBMD. Adjustment for weight did not alter these findings.
Femoral neck and total femoral measurements of the postmenopausal cohorts are also shown in Table 5. The FNBMC was similar, the femoral neck BA significantly smaller and the mean unadjusted FNBMD higher in blacks in the early and late postmenopausal groups. Likewise, FTBMC was similar, total femoral BA smaller and mean unadjusted FTBMD statistically significantly higher in blacks compared with whites in the younger postmenopausal group. In older postmenopausal subjects, the FTBMC was, however, significantly higher and the total femoral BA similar. A significantly higher mean unadjusted FTBMD, in accordance with the younger postmenopausal cohort, was also documented in the older postmenopausal black women. Only weight (p < 0.01) was significantly associated with means FNBMD and FTBMD in the early postmenopausal subjects whereas age, weight, number of pregnancies and number of pack years smoked were significantly associated with proximal femoral bone density in older postmenopausal women. Only adjustment for weight significantly altered the ethnic differences in bone density (Table 5). Adjustment for weight diminished the ethnic difference in means FNBMD and FTBMD and resulted in similar mean FTBMD between the younger postmenopausal cohorts and similar means FNBMD and FTBMD between the older postmenopausal women.
Femoral neck BMAD unadjusted and adjusted for covariates with significant association (younger postmenopausal groups: weight only; older postmenopausal cohorts: weight and number of pregnancies) was consistently higher in blacks (Table 5).
Similar to our observations with regard to SBMD and SBMAD, weight was the only anthropometric variable that consistently correlated significantly and positively with BMD (Fig. 1) and BMAD at the proximal femoral sites in all the menstrual subgroups.
Within the different weight groups in the premenopausal women, ethnic differences in femoral BMD were confined to significantly higher FNBMD in blacks (Table 4). Both femoral measurements were significantly lower in the normal-low weight whites compared to the overweight white women (p < 0.01); this was not observed in blacks. In the postmenopausal women, femoral neck and total femoral BMD were higher in blacks compared with whites in the normal-low and overweight subgroups, although significance was not reached for FTBMD in the normal-low weight subgroup. This may be partially due to small numbers of both black and white women in this weight subgroup. Both femoral BMD measurements were significantly lower in normal-to-low weight blacks and whites compared to their respective overweight counterparts.
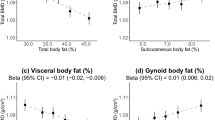
Comparison of bone density across age and menstrual groups
A statistically significant negative correlation between age and BMD at all skeletal sites was present in the total black and white cohorts. A general regression model including age and race × age interaction was employed to assess potential ethnic differences in the decline of BMD parameters with age. The race × age interaction was significant (p < 0.01), indicating that the association of BMD parameters with ageing differed between blacks and whites with a steeper decline present in ageing white women (Fig. 2). Despite the cross-sectional nature of our study, the pattern of bone loss with ageing appeared to differ between the two racial groups (Table 6). The percentage decline in SBMD between the premenopausal and early postmenopausal black and white cohorts was near identical (9 and 10 %, respectively), but the older black females maintained their SBMD better compared with whites. Similar SBMD was thus noted in the late postmenopausal black and white women despite the lower SBMD observed in premenopausal blacks. The percentage bone loss at the femoral neck and total femoral regions across the menopausal transition (i.e. between the premenopausal and early postmenopausal cohorts) was higher in whites (femoral neck region, 13 vs. 7 %; total femoral region, 8 vs. 2 %). Thereafter, a similar rate of decline in femoral BMD was noted in blacks and whites and ensured that black women maintained their significantly higher means FNBMD and FTBMD into old age.
Correlation between age and BMD in the black and white study cohorts. Significant negative correlation between age and BMD measurements at the lumbar spine (a), femoral neck (b) and total femoral (c) sites for blacks and whites (p ≤ 0.05). The interaction effect of race × age is significant for proximal femoral sites indicating a sharper decline in BMD measurements at the proximal femur in ageing whites compared with blacks (p < 0.001)
Osteopenia and osteoporosis in postmenopausal women
A similar percentage of black and white postmenopausal women had spinal osteopenia as measured against a uniform white reference population (53 % of postmenopausal blacks and 44 % of postmenopausal whites), while 14 % of both blacks and whites met the diagnostic criteria for osteoporosis. Although a higher percentage of postmenopausal whites were osteopenic at the proximal femoral sites, a significant percentage of postmenopausal blacks also presented with femoral neck (35 %) and total femoral (28 %) osteopenia. Osteoporosis as defined by WHO criteria, and measured against a uniform white reference population, was confined to the white group affecting 11 % of the postmenopausal population.
Discussion
This cross-sectional study which compared the spine and hip BMD of black and white South African women, concluded that spine BMD was either lower or similar in blacks compared with whites, that proximal femoral BMD was higher in blacks and that bone loss with ageing was attenuated in blacks. The ethnic differences in BMD observed in this study were fully accounted for by differences in total body weight between blacks and whites. Furthermore, the attenuated loss of bone in blacks appeared to relate largely to the progressive increase in body weight in ageing black women. The lower SBMD in blacks was due to a lower peak SBMD in premenopausal women and contests the idea of genetic protection against osteoporosis at all skeletal sites in black South African women.
Site-specific differences in BMD have been reported in other female populations on the African continent. Studies conducted in The Gambia and other West African populations have documented lower or similar SBMD in African women compared with European subjects [2, 15–17, 24]. In the only two previous studies employing DXA measurements of BMD in adult black and white South African women, similar SBMD, but significantly higher femoral BMD, has been reported [18, 19]. Although a similar trend in BMD measurements at different skeletal sites was reported in these studies compared to ours, significant differences were also observed, for example, SBMD was lower in our premenopausal blacks compared with whites, and the ethnic difference in femoral measurements was non-significant after adjustment for total body weight.
African-American women have higher BMD at all skeletal sites compared with whites [8–12, 25, 26], and most studies indicate that the higher BMD in adult African-American women is due to the attainment of a greater peak bone mass by early adulthood [8, 9, 11, 12, 25, 27]. It is thus generally accepted that the black skeleton is genetically protected against the development of OP and its consequences. South African blacks, similar to their American counterparts, may have a genetic tendency to greater BMD than whites, since both of these populations originated and migrated from West Africa [20]. The finding of lower SBMD in premenopausal blacks in the present study, however, argues against significant genetic protection in black South African women at all skeletal sites.
In this study, total body weight had a major impact on observed ethnic differences in peak BMD. The presence of a higher body weight eliminated ethnic differences in BMD at all skeletal sites, whereas a normal-low body weight unmasked site-specific ethnic differences in BMD in our study subjects. The finding of lower SBMD in premenopausal black women could be mainly attributed to lower SBMD in blacks with low-normal weight (p < 0.01). The SBMD of lower weight black women was also significantly lower than that of overweight blacks and suggests that a low body weight may serve as one of the most important risk factors for a low peak SBMD in blacks. A low body weight may, therefore, play a more important role than proposed genetic factors in determining ethnic differences in peak BMD at the spine in South African women. A significant association between spine BMD and other lifestyle factors such as a lower calcium intake and more frequent use of injectable contraception could not be demonstrated in our black study subjects, but this may be the result of a relatively small sample size.
Premenopausal blacks had greater proximal femoral neck BMD and similar total femoral BMD compared with whites. The higher femoral neck BMD was mostly accounted for by higher measurements in the low-normal weight subgroup, whereas no ethnic difference in proximal femoral BMD was noted in the overweight women. The higher femoral neck BMD in blacks in the low-normal weight group may suggest that genetic factors do play an important role at this specific skeletal site in blacks, affording protection despite adverse environmental factors. Higher BMD confined to the proximal femoral sites has been reported in black South African schoolchildren despite their lower socioeconomic status and exposure to numerous factors known to impact negatively on bone mass [28, 29]. This lends support to a protective genotype at the hip region in South African blacks similar to the African-American population.
Although this cross-sectional study was not designed to interpret longitudinal changes, apparent ethnic differences in the pattern of bone loss with ageing at both the hip and spine were observed. A steeper decline in BMD at all skeletal sites was noted in ageing white women, which reached statistical significance at the proximal femoral sites (p < 0.001) (Fig. 2). A slower decline in femoral BMD, especially during the menopausal transition period, and better-maintained spinal BMD in older blacks (Table 6) resulted in similar SBMD and progressively higher proximal femoral BMD in ageing black women.
Different patterns of bone loss in ageing black and white women, with a slower rate of cortical and trabecular bone loss in black women, have also been observed in previous multi-ethnic studies conducted in South Africa and the USA [18, 30–32]. The progressive increase in adiposity with ageing may be an important mechanism whereby black women maintained their BMD better into old age compared with whites. The ethnic difference in body weight was most pronounced in older women, and weight, similar to our finding in premenopausal women, was positively associated with BMD at all skeletal sites. The impact of body weight on BMD was further demonstrated by our finding of higher BMD, especially at the proximal femoral sites, in the overweight blacks and whites. Body weight may impact on patterns of bone loss via the mechanical loading effect of its lean mass component as well as the hormonal impact of its fat mass component [33–37]. Fat mass becomes the main determinant of endogenous oestrogen activity due to the increased conversion of androgens to estrogens after the menopause and may have a role in maintaining BMD in postmenopausal females as reported by others [34, 36, 37].
The higher proximal femoral BMD in our postmenopausal black women is in accordance with other South African and international studies [10, 18, 19, 26]. Differences in anthropometry, especially body weight or body mass index, have been reported to account for part of the difference in BMD between blacks and whites, both from South Africa and the USA [12, 18]. In the South African nurses’ study, proximal femoral BMD remained significantly higher in postmenopausal blacks after correction for weight [18]. Finkelstein et al. [12] reported that adjustment for anthropometric and lifestyle factors, particularly body weight, reduced the magnitude of the difference in lumbar and femoral neck BMD between African-American and Caucasian women (unadjusted difference SBMD 7–12 %, adjusted difference 3–6 %, unadjusted difference FNBMD 14–24 %, adjusted difference 6–9 %). Significant differences in BMD, however, remained, after correction for weight in all of these reports, whereas adjustment for body weight fully accounted for the ethnic differences in BMD between black and white women in the present study.
Clinical risk factors other than body weight may also impact on BMD and patterns of loss. The clinical risk profiles of black and white postmenopausal women differed, but a significant association was only noted between femoral BMD and parity (positive association) and pack years smoking (negative association) in older postmenopausal women. Correction for these clinical covariates did not significantly alter ethnic differences in femoral BMD. The mean calcium intake of postmenopausal blacks was lower compared with whites (p < 0.01), and physical activity was less well maintained amongst ageing blacks (p < 0.01). A significant association between calcium intake and physical inactivity and BMD could not be demonstrated in our postmenopausal cohorts. Again, this may be ascribed, at least in part, to the small sample size of our study, and a contribution of these lifestyle factors cannot be excluded.
Impact of bone size on BMD measurements
Lumbar spine and femoral neck bone area, as measured by DXA, were significantly smaller in black women compared with whites, a finding also reported in African-American women compared with Caucasian women [12]. Areal measurements may thus be inappropriately low in the black cohorts due to their smaller bone size. In the present study, partial corrections of bone size increased bone mineral measurements of the black women relative to whites and resulted in similar mean spinal BMAD and significantly higher mean femoral neck BMAD in premenopausal and postmenopausal black women before and after adjustments for covariates, including body weight.
Multi-ethnic studies in the USA reported that women with osteopenia or osteoporosis had an increased risk of fracture in every ethnic group, but the absolute risk of fracture at any given BMD differed between African-American women and white women [4, 5]. The estimated volumetric apparent bone density of the femoral neck is not regarded as superior to areal femoral BMD in the prediction of hip fracture in elderly postmenopausal white women [38]. Since women of different racial and ethnic groups have substantially different femoral neck sizes, BMAD might in fact be a better predictor than BMD of hip fracture in a more diverse population.
BMD and fracture risk in black and white postmenopausal females
Vertebral osteoporosis was present in 14 % of both black and white postmenopausal women, whereas femoral osteoporosis was confined to 11 % of the postmenopausal white population. The small/no ethnic difference in BMD at most measured sites cannot readily explain the apparent large difference in fracture risk previously reported in white and black South African women. Data pertaining to fracture prevalence in black South African females are very limited and old and may not truly represent current fracture risk [1, 3]. Prospective studies are clearly needed to assess the true prevalence of vertebral and hip fracture in black and white SA women.
Our study had limitations. Conclusions drawn from this study were limited by the small sample size of 326 women, but data obtained in this cohort nonetheless do contribute to the current small knowledge pool regarding ethnic differences in BMD on the African continent. Assessment of BMD measurements across age and menstrual groups in this cross-sectional study did allow us to observe different trends with regard to BMD measurements in premenopausal females and preservation of BMD with ageing in black and white SA women. The cross-sectional study design, however, limited our ability to truly assess and interpret longitudinal changes and bone loss patterns in both ethnic groups. The apparent ethnic differences in bone mineral changes with ageing observed and documented in this study therefore need to be verified in prospective population-based studies. As participation was voluntary, selection bias may have occurred. We furthermore did not stratify patients based on socioeconomic status or anthropometry due to inherent differences in this regard between the two ethnic groups. We do, however, feel that our BMD data was obtained in a study sample that accurately reflects the broader premenopausal and postmenopausal white and black SA female population.
To conclude, this study has shown that black South African women have lower spine BMD than whites, that the higher proximal femoral BMD in blacks is fully accounted for by marked ethnic differences in body weight and that the observed attenuated bone loss in black females is related to their significantly higher body weight. Black South African women should not be regarded as genetically protected against the development of osteoporosis and should not be excluded from strategies aimed at prevention and early detection of this potentially debilitating disease. The modern tendency towards a lower ideal body weight in urbanized black societies may further increase the likelihood of suboptimal attainment of peak BMD and may impact on bone loss rates with potentially lower BMD in later life in the black populations of South Africa. Prospective studies are clearly needed to better define patterns of bone loss and vertebral and hip fracture prevalence in postmenopausal black and white SA women.
References
Solomon L (1968) Osteoporosis and fracture of the femoral neck in the South African Bantu. J Bone Joint Surg 50(B):2–12
Aspray TJ, Prentice A, Cole TJ, Sawo Y, Reeve J, Francis RM (1996) Low bone mineral content is common, but osteoporotic fractures are rare in elderly rural Gambian women. J Bone Miner Res 11(7):1019–1025
Dent CE, Engelbrecht HE, Godfrey RC (1968) Osteoporosis at lumbar vertebrae and calcification of abdominal aorta in women living in Durban. BMJ 4:76–79
Cauley JA, Lui LY, Ensrud KE, Zmuda JM, Stone KL, Hochbeg MD, Cummings SR (2005) Bone mineral density and the risk of incident Non-spinal fractures in black and white women. JAMA 293(17):2102–2108
Barrett-Connor E, Siris ES, Wehren LE, Miller PD, Abbott TA, Berger ML, Santora AC, Sherwood LM (2005) Osteoporosis and fracture risk in women of different ethnic groups. J Bone Miner Res 20(2):185–194
Cauley JA, Palermo L, Vogt M, Ensrud KE, Ewing S, Hochberg M, Nevitt MC, Black DM (2008) Prevalent vertebral fractures in black women and white women. J Bone Miner Res 23(9):1458–1467
Lansdown D, Bennet B, Thiel S, Ahmed O, Dixon L, Vokes TJ (2011) Prevalence of vertebral fractures on chest radiographs of elderly African American and Caucasian women. Osteoporos Int 22(8):2365–2371
Henry YM, Eastell R (2000) Ethnic and gender differences in bone density and bone in young adults: effect of bone size. Osteoporos Int 11:512–517
Ettinger B, Sidney S, Cummings SR, Libanati C, Bikle DD, Tekawa IS, Tolan K, Steiger P (1997) Racial differences in bone density between young adult black and white subjects persist after adjustment for anthropometric, lifestyle and biochemical differences. J Clin Endocrinol Metab 82(2):429–434
Looker AC, Johnston CC Jr, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Lindsay RL (1995) Prevalence of low femoral bone density in older U.S. women from NHANES III. J Bone Miner Res 10(5):796–802
Liel Y, Edwards J, Shary J, Spicer KM, Gordon L, Bell NH (1988) The effects of race and body habitus on bone mineral density of the radius, hip and spine in premenopausal women. J Clin Endocrinol Metab 66(6):1247–1250
Finkelstein JS, Lee M-L T, Sowers M, Ettinger B, Neer RM, Kelsey JL, Cauley JA, Huang M, Greendale GA (2002) Ethnic variation in bone density in premenopausal and early perimenopausal women: effects of anthropometric and lifestyle factors. J Clin Endocrinol Metab 87(7):3057–3067
Carter DR, Bouxsein ML, Marcus R (1992) New approaches for interpreting projected bone densitometry data. J Bone Miner Res 7(2):137–145
Katzman DK, Bachrach LK, Carter DR, Marcus R (1991) Clinical and anthropometric correlates of bone mineral acquisition in healthy adolescent girls. J Clin Endocrinol Metab 73:1332–1339
Dibba B, Prentice A, Laskey MA, Stirling DM, Cole TJ (1999) An investigation of ethnic differences in bone mineral, hip axis length, calcium metabolism and bone turnover between West African and Caucasian adults living in the United Kingdom. Ann Human Biol 26(3):229–242
Melton LJ III, Marquez MA, Achenbach SJ, Riggs BL (2002) Variations in bone density among persons of African heritage. Osteoporos Int 13:551–559
Prentice A, Shaw J, Laskey AN, Cole TJ, Fraser DR (1991) Bone mineral content of British and rural Gambian women aged 18–80+ years. J Bone Miner Res 12:201–214
Daniels ED, Pettifor JM, Schnitzler CM, Russell SW, Patel DN (1995) Ethnic differences in bone density in female South African nurses. J Bone Miner Res 10(3):359–367
Chantler S, Dickie K, Goedecke JH, Levitt NS, Lambert EV, Evans J, Joffe Y, Micklesfield LK (2012) Site-specific differences in bone mineral density in black and white premenopausal South African women. Osteoporos Int 23:533–542
Excoffier L, Pelligrini B, Sanchez-Mazas A, Simon C, Langaney A (1987) Genetics and history of sub-Saharan Africa. Yearb Phys Anthropol 30:151–194
Kahn HS (1991) A major error in nomograms for estimating body mass index. Am J Clin Nutr 54:435–437
Binkley NC, Schmeer P, Wasnich RD, Lechnik L (2002) Position Statement. International Society for Clinical Densitometry Position Development Panel and Scientific Advisory Committee. What are the criteria by which a densitometric diagnosis of osteoporosis can be made in males and non-Caucasians? J Clin Densitom 5(3):19–27
Kanis JA (1997) Assessment of fracture risk and its application to screening for post-menopausal osteoporosis: Synopsis of a WHO-report. Osteoporos Int 1994; 4:368–381
Bererhi H, Constable A, Lindell AE, Coutino J, Kharousi W (1994) A study of bone mineral density versus age in Omani women—a comparison with normal British women. Nucl Med Commun 15:99–103
Luckey MM, Meier DE, Mandeli JP, DaCosta MC, Hubbard ML, Goldsmith SJ (1989) Radial and vertebral bone density in white and black women: evidence for racial differences in pre-menopausal bone homeostasis. J Clin Endocrinol Metab 69:762–770
DeSimone DP, Stevens J, Edwards J, Shary J, Gordon L, Bell NH (1989) Influence of body habitus and race on bone mineral density of the midradius, hip and spine in aging women. J Bone Miner Res 6(4):827–830
Gilsanz V, Roe TF, Mora S, Costin G, Goodman WG (1991) Changes in vertebral bone density in black girls and white girls during childhood and puberty. N Engl J Med 325(23):1597–1600
McVeigh JA, Norris SA, Cameron N, Pettifor JM (2004) Association between physical activity and bone mass in black and white South African children at age 9 yr. J Applied Physiol 97(3):1–11
Vidulich L, Norris SA, Cameron N, Pettifor JM (2006) Differences in bone size and bone mass between black and white 10-year-old South African children. Osteoporos Int 17:433–440
Solomon L (1979) Bone density in ageing Caucasian and African populations. Lancet 57(B):1326–1329
Cauley JA, Lui LY, Stone KL, Hillier TA, Zmuda JM, Hochberg M, Beck TJ, Ensrud KE (2005) Longitudinal study of changes in hip bone mineral density among Caucasian and African-American women. J Am Geriatr Soc 53:183–189
Luckey MM, Wallenstein S, Lapinski R, Meier DE (1996) A prospective study of bone loss in African-American and white women—a clinical research center study. J Clin Endocrinol Metab 81(3):2948–2956
Albala C, Yanez M, Devoto E, Sostin C, Zeballos C, Santos JL (1996) Obesity as a protective factor for postmenopausal osteoporosis. Int J Obes Relat Metab Disord 20(11):1027–1032
Glauber HS, Vollmer WM, Nevitt MC, Ensrud KE, Orwoll ES (1995) Body weight versus body fat distribution, adiposity, and frame size as predictors of bone density. J Clin Endocrinol Metab 80:1118–1123
Salamone LM, Glynn N, Black D, Epstein RS, Palermo L, Meilahn E, Kuller LH, Cauley JA (1995) Body composition and bone mineral density in premenopausal and early perimenopausal women. J Bone Miner Res 10(11):1762–1768
Reid IR, Ames R, Evans MC, Sharpe S, Cundy TF (1992) Determinants of total body and regional mineral density in normal postmenopausal women—a key role for fat mass. J Clin Endocrinol Metab 75:45–51
Meldrum DR, Davidson BJ, Taturyn IV, Judd HL (1981) Changes in circulating steroids with aging in postmenopausal women. Obstet Gynecol 57:624–629
Stewart A, Kumar V, Reid DM (2006) Long-term fracture prediction by DXA and QUS: a 10-year prospective study. J Bone Miner Res 21(3):413–418
Acknowledgements
This work was supported by grants from the Medical Research Council of South Africa and the Women’s Health Initiative Indianapolis. We thank Madele du Plessis for performing the dietary analyses.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Conradie, M., Conradie, M.M., Kidd, M. et al. Bone density in black and white South African women: contribution of ethnicity, body weight and lifestyle. Arch Osteoporos 9, 193 (2014). https://doi.org/10.1007/s11657-014-0193-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-014-0193-0