Abstract
The aim of this study was to evaluate the relationship between historical height loss (HHL) and prevalent vertebral fractures (VF) in postmenopausal Moroccan women and to estimate its accuracy as a clinical test for detecting VF. Two hundred eighty-eight postmenopausal women were studied. All subjects had bone density measurements and spinal radiographs. Vertebral bodies (T4–L4) were graded using the semi-quantitative method of Genant. HHL was calculated as the difference between a patient’s tallest recalled height and the current measured height. The mean age was 58.4 ± 7.8 years. Thirty-one percent of patients were osteoporotic, and 46.5% had VF. Patients with VF had lost more height than those without VF (median, 2.0 cm (0.26–3.3) vs 0.96 cm (0.33–2.4), p < 0.05). In univariate analysis, HHL was positively correlated to both number and grade of prevalent VF (p < 0.05). The area under the receiver operating characteristics curve for the ability of HHL to detect VF was 0.60 (95% confidence interval (CI), 0.52, 0.69). Our HHL threshold for detecting VF was >1.5 cm, its sensitivity was 58%, and its specificity was 61%. The positive predictive value was 53%, and the negative predictive value was 65%. With HHL >1.5 cm, positive likelihood ratio was 1.49 with 95% CI, 1.07, 2.06. Our results demonstrate significant positive associations between HHL, VF, number of VF, and grade of VF. However, this relationship is not clinically pertinent. Consequently, HHL cannot be used as a reliable clinical test for detecting VF in postmenopausal Moroccan women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Osteoporosis is a disease of bone that leads to an increased risk of fracture. Typical fragility fractures occur in the vertebral column, hip, and wrist [1]. Vertebral fractures (VF) are the most common type of osteoporotic fracture, but more than two thirds remain undetected [2]. VFs resulting from osteoporosis often lead to loss of vertebral body height [3], in turn causing a decrease in stature [4, 5]. Consequently, height loss has long been assumed to be a marker of VFs [5–9]. Height loss can be evaluated in two ways. Determination of prospective height loss (PHL) employs sequential measurements of an individual’s height to determine if it is decreasing over time. This approach employs measurements that are under the control of a physician and may be able to identify the time period in which a fracture was sustained [6, 7]. A negative aspect of using PHL is that it detects only incident fractures and will not identify prevalent VFs at the start of monitoring. The second method to evaluating height loss is to determine historical height loss (HHL) [8, 10, 11]. In this method, HHL is calculated as the difference between current measured height and self-reported tallest recalled height (TRH) [10, 11]. This approach is compromised by error in patient recall and cannot identify when a fracture might have occurred. However, this technique has two important advantages. The first is that physician could detect fractures at the initial clinical contact by only one current height measurement. The second is that the use of HHL may allow the detection of prevalent fractures, which are one of the most common causes of disability and major contributor to medical care costs in many regions of the world. Prevalent VFs are also associated with elevated risk of further fractures [12, 13]. If the application of HHL to physical examination could improve the detection of patients with prevalent VFs, this will facilitate the targeting of treatment strategies to those at highest risk of future fracture [7]. The performance characteristics of HHL as a clinical test for the detection of VFs have been well described in only one study [11].
On the other hand, although the need for accurate anthropometric measurement has been repeatedly stressed, reports on height measurements in Moroccan populations never include estimates of measurement error. The lower is the variability between repeated measurements of the same subject by one (intra-observer differences) or two or more (inter-observer differences) observers, the greater is the precision. The most commonly used measure of precision is the technical error of measurement (TEM) [14–16].
The aim of this study was to evaluate the relationship between HHL and prevalent VFs in postmenopausal Moroccan women and to estimate its accuracy as a clinical test for detecting VFs. On the other hand, this study also calculated intra- and inter-observer errors of height measurement.
Subjects and methods
Subjects
The study involved 288 consecutive and ambulatory Moroccan postmenopausal women living in urban center of Morocco, who were sent to our outpatient Bone Densitometry Center. Recruitment was based on voluntary enrollment. All subjects were referred to this center for osteoporosis risk factors, including menopause. Informed consent was obtained from all subjects, and the study was approved by the ethics committee of our university hospital. We excluded from the study all patients with a history of (1) taking drugs known to influence bone metabolism in the past 2 years, such as vitamin D, calcium, corticosteroids, bisphosphonates, and hormone replacement therapy; (2) musculoskeletal, thyroid, parathyroid, adrenal, hepatic, or renal disease; (3) malignancy; and (4) hysterectomy.
Data collection and measurements
Each patient completed a questionnaire on sociodemographic parameters and osteoporosis risk factors. TRH was obtained from each patient. A subset of subjects was also asked to estimate the amount of height they had lost. HHL was calculated as the difference between TRH and measured height, which was determined using a wall-mounted mechanical stadiometer. Each subject was measured without shoes, with the heels, buttocks, and back to the stadiometer backboard. The subject’s head was maintained in the Frankfort plane, with the left orbital in the same horizontal plane as the left tragion. Heels were together and feet angled approximately 60° to each other. The patient was instructed to stretch to a fully erect position while keeping the feet flat on the floor. Height was recorded to the closest millimeter during normal respiration. Each subject was measured three times by the same observer, and the mean of these three values was considered as the current height measured. Between two measures, subjects went away from the stadiometer then replaced correctly again. Subjects were also measured by three other observers using the same stadiometer.
Height measurement error
Height measurement error was evaluated by calculating the TEM which is the square root of measurement error variance. The calculations for intra- and inter-observer error are broadly the same. Intra-observer TEM was estimated by the following equation:
where N is the number of subjects, K is the number of height determinations by the same observer, and M is the measurement. Inter-observer TEM was estimated by the same equation where K is the number of observers (assuming one determination per observer).
Other anthropometric data
Weight was measured without clothes or shoes at the time of bone densitometry measurements. The body mass index was calculated as body weight (kilogram)/height (meter square).
Bone mineral density measurements
Lumbar spine, trochanter, femoral neck, and total hip bone mineral density (BMD) were measured by dual-energy X-ray absorptiometry with a Lunar prodigy densitometer. Daily quality control was carried out by measurement of a Lunar phantom. At the time of the study, phantom measurements showed stable results. The phantom precision expressed as the coefficient of variation (percent) was 0.08. Both T and Z scores were obtained. In the T score calculations, the manufacturer’s ranges for European reference population were used because of the absence of a Moroccan database at the time of the study.
Vertebral morphometry
Lateral and anteroposterior radiographs of the thoracolumbar spine were obtained according to standardized procedures. The anterior, central, and posterior heights of each of the vertebral bodies from T4 to L5 were measured by expert radiologist and rheumatologist. VFs were diagnosed by the Genant semi-quantitative method [17], a visual radiographic approach which corresponds to the attribution of grades, ranging from 0 (no VF), 1 (20% decrease of vertebra height), 2 (between 20% and 40% decrease of vertebra height), to 3 (severe VF, more than 40% decrease of vertebra height).
Dietary calcium questionnaire
The frequential self-questionnaire of Fardellone has been modified, simplified, and adjusted to the Moroccan food habits. After translation and back translation, it was administered to 62 women volunteers, aged between 30 and 60 years. To test its validity, the questionnaire was compared to the weekly docket system, chosen as a reference method. To test its reproducibility, the questionnaire was administered again after a 1-week interval. The coefficient of correlation was 0.91. The questionnaire correctly classified women with daily calcium intake less than 800 mg with 76.9% specificity, while its sensitivity was 86.7%.
Statistical analysis
Statistical analysis was performed with Statistical Package for the Social Sciences (SPSS) for Windows 13.0 (SPSS Inc., Chicago, IL, USA). Population descriptions are expressed as mean ± standard deviation or medians for continuous variables and as percentage distributions for discrete variables. TEM was calculated. The subjects were separated into two groups (group 1 with fractures and group 2 without fractures). Means of the two groups were compared by t student and Mann–Whitney tests. Comparison of continuous variables was carried out by the Kruskal–Wallis test. Multiple linear regression models were used to determine the influence of total VFs, lumbar fractures, and thoracic fractures on HHL. Receiver operating characteristic (ROC) curves were generated, and the areas under the curves (AUC) were calculated to summarize the ability of height loss to predict fractures. The best cutoff value was chosen using Youndens’ index. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and positive likelihood ratio (with 95% confidence intervals (95% CI)) were calculated at the best cutoff value. p values of <0.05 were considered as statistically significant.
Results
Clinical characteristics
The characteristics of the patients are shown in Table 1. The mean age of the patients was 58.4 ± 7.8 years. All patients were residing in urban areas. Twenty-five percent of patients were illiterate, 17% had primary education, 38.9% had a secondary education, and 18.7% had received a university education. Thirty-one percent of patients were osteoporotic, and 46.5% had VF. Subjects had a median number of VF of 3 (2–5). Fifty-seven percent of patients remembered their TRH, and 36.8% could estimate the amount of height they had lost.
Determination of height measurement error
Intra-observer TEM was 0.12 cm, and inter-observer TEM was 0.25 cm.
Risk factors for vertebral fracture
In univariate analysis, VF risk was significantly associated to older age (p < 0.001), to higher number of pregnancies (p = 0.007), to longer duration of menopause (p < 0.001), and to lower BMD at all the sites (p < 0.05). Logistic regression showed that lumbar BMD (p < 0.001), age (p = 0.03), and level of instruction (p = 0.03) were all independent factors for VF.
Relationship between historical height loss and number of vertebral fractures
Patients with VF had lost more height than those without VF (2.0 cm (0.26–3.3) vs 0.9 cm (0.3–2.4); p < 0.05; Table 1). In univariate analysis, HHL and the number of prevalent VFs were positively correlated (p < 0.001). The height loss per fracture was 0.3 cm (95% CI, 0.1–0.4 cm). Incorporating age, the amount of height loss per fracture was 0.2 cm (95% CI, 0.1–0.4 cm; p < 0.05). The height loss per thoracic fracture (after correction for the presence of lumbar fractures and for age) was 0.2 cm (95% CI, 0.1–0.5 cm; p < 0.05). The height loss per lumbar fracture (after correction for the presence of thoracic fractures and for age) was greater at 0.4 cm (95% CI, 0.1–0.9 cm; p < 0.05).
Relationship between historical height loss and grade of vertebral fractures
Patients without prevalent VF (53.5%) had a median height loss of 0.9 cm (0.3–2.4). Grade 1 fractures were present in 88.8% of patients with VF, with a median HHL of 2 cm (0.1–3). Grade 2 fractures were found in 8.2% of subjects with VF who had a median HHL of 3.8 cm (0.25–12.2). HHL in grade 2 fractures was statistically higher than height loss for grade 1 fractures and for patients without fractures (p = 0.04). Grade 3 fractures were present only in four patients who did not remember their TRHs.
Accuracy of historical height loss as a clinical test for the detection of vertebral fracture
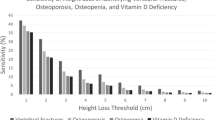
The area under the ROC curve for the ability of HHL to detect fracture was 0.60 (95% CI, 0.52, 0.69; Fig. 1). The best cutoff value chosen using Youndens’ index was 1.5 cm. At HHL >1.5 cm, sensitivity was 58% (95% CI, 45%, 69%), and specificity was 61% (95% CI, 51%, 71%). Predictive values were determined across a wide range of theoretical fracture prevalence that might be encountered in clinical practice by applying the sensitivity and specificity corresponding to HHL >1.5 cm (Table 2). For VF prevalence of 46.5%, PPV was 53% (95% CI, 41%, 64%), and NPV was 65% (95% CI, 54%, 75%). With HHL >1.5 cm, the positive likelihood ratio was 1.49 with a 95% CI from 1.07 to 2.06.
Discussion
The present study has identified significant positive associations between HHL, VF, number of VF, and grade of VF.
With emergence of effective osteoporosis treatments that markedly reduce fracture likelihood, it is essential to detect patients with VF so that appropriate diagnosis and therapy can be instituted [7]. Longitudinal studies reported that the decrease in stature with age among healthy people without VF was very slight, suggesting that in unselected population, some apparent stature loss with age is probably due to disease processes, such as VF [6, 18]. Consequently, some osteoporosis guidelines recommend that height loss assessment should be part of the evaluation of patients with osteoporosis and of those at risk of osteoporosis [19, 20]. Height loss can be evaluated by calculating HHL [11]. However, one difficulty was to determine a specific amount of HHL that should be used as a threshold for defining patients at high risk of having prevalent VFs.
Several studies demonstrated that HHL was strongly associated with VF [5, 8, 11, 21]. Nevertheless, only one study showed that HHL can serve as a test for assessing the presence of VFs and propose that the useful height loss threshold for postmenopausal women should be HHL >6.0 cm [11]. That threshold had a specificity of 94%, a sensitivity of 30%, and produced high NPVs across the range of VF prevalence encountered in clinical practice. HHL performed even better for certain subtypes of fracture patients: those with greater numbers of fractures, those with more severe fractures, and those with crush fractures. Besides, in the study of Siminoski et al. [11], the amount of height loss per fracture was 0.97 cm, after the correction for age. The HHL per thoracic fracture was 0.76 cm, and the HHL per lumbar fracture was greater at 1.5 cm. However, in the ROC curve which estimated the ability of HHL to predict one or more fractures, the AUC was only 0.66, and the positive likelihood ratio for fracture was relatively flat (2.8 for HHL >6 cm). These values indicated that there would be limitations to the application of HHL.
In our results, the most important finding was that HHL was significantly associated with VF and with number of VF. HHL was also significantly associated with number of thoracic VF, lumbar VF, and with grade of VF, confirming the findings of other investigators [5, 11]. However, this relationship was not clinically pertinent. Indeed, the average height loss per fracture after adjusting for age was only 0.2 cm with a 95% CI of 0.1 to 0.4 cm. This average height loss was close to the intra-observer TEM of height (0.12 cm). Indeed, height was recorded to the closest millimeter. So, a difference of 0.8 mm could not be detected by the stadiometer. This moderate average height loss may be explained by the great percentage of grade 1 VF in our patients (88.8%). Similarly, the amount of height loss per lumbar VF was 0.4 cm versus 0.2 cm for thoracic VF. Both values were less than those reported in other studies [11]. Nevertheless, the area under the ROC curve for the ability of HHL to detect fracture was only 0.60. Besides, our threshold (HHL >1.5 cm) was smaller than that reported in another study [11]. At HHL >1.5 cm, positive likelihood ratio was 1.49, and PPV was only 53%. So, while a prevalent fracture is suggested, it cannot be ruled in by height measurements with sufficient certainty to be applied clinically as a definitive test for VF. In brief, using HHL >1.5 cm could be a major source of inaccuracy to detect prevalent fractures in Moroccan women.
HHL is calculated from two variables: current measured height and TRH. Each has potential sources of error. TRH is based on patient memory of height attained in young adulthood. So, TRH is subjected to the error due to the patient’s recall [11]. In fact, 25.4% of our patients were illiterate, and only 56.9% could remember their TRH. Nobody had documentation about TRH. Furthermore, for eight patients, TRH were smaller than current measured heights.
Besides, current height will vary with the time of day, physical exertion prior to measurement, variation in posture, and disease states [22–24]. In our study, the intra- and inter-observer TEMs for height measurement were very similar to those observed by other investigators [13, 14]. Anthropometric measurement error is unavoidable and should be minimized by paying close attention to every aspect of the data collection process. In this study, height measurement errors were minimized to acceptable ranges.
There were two main limitations of this study. First, the subjects were not recruited from the community at large but were selected from patients who underwent bone density determinations. This selection bias likely explains the relatively high prevalence of osteoporosis in the subjects studied. However, we have already shown that 31% to 39% of postmenopausal Moroccan women had osteoporosis [25–27]. On the other hand, using HHL for assessment of height loss was not easy because more than half of patients did not remember their TRH. Therefore, it could be interesting in our population to use a marker of TRH such as arm span. Indeed, arm span is very close to stature in young adults and may thus produce a more accurate HHL determination and improved detection of VF. Furthermore, studies suggest that a minimum 3-cm difference between arm span and current height makes up one of the criteria for suspecting osteoporosis [28–31].
Conclusion
In brief, our results showed significant positive associations between HHL, VF, number of VF, and grade of VF. However, this relationship was not clinically pertinent. So, HHL cannot be used as a reliable clinical test for detecting VFs in postmenopausal Moroccan women.
References
Roux C (2006) Osteoporosis. Rev Prat 56:673–677
Cooper C, Atkinson EJ, O’ Fallon WM, Melton LJ (1992) Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985–1989. J Bone Miner Res 7:221–227
Genant HK, Wu CY, van Kuikj C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Spector TD, McCloskey EV, Doyle DV, Kanis JA (1993) Prevalence of vertebral fracture in women and the relationship with bone density and symptoms: the Chingford Study. J Bone Miner Res 8:817–822
Gunnes M, Lehmann EH, Mellstrom D, Johnell O (1996) The relationship between anthropometric measurements and fractures in women. Bone 19:407–413
Huang C, Ross PD, Lydick E, Davis JW, Wasnich RD (1996) Contributions of vertebral fractures to stature loss among elderly Japanese-American women in Hawaii. J Bone Miner Res 11:408–411
Siminoski K, Jiang G, Adachi JD, Hanley DA, Cline G, Ioannidis G, Hodsman A, Josse RG, Kendler D, Olszynski WP, Ste Marie LG, Eastell R (2006) The accuracy of height loss during prospective monitoring for detection of incident vertebral fractures. Osteoporos Int 16:403–410
Ismail AA, Cooper C, Felsenberg D, Varlow J, Kanis JA, Silman AJ, O’Neill TW (1999) Number and type of vertebral deformities: epidemiological characteristics and relation to back pain and height loss. Osteoporos Int 9:206–213
Ettinger B, Black DM, Nevitt MC, Rundle AC, Cauley JA, Cummings SR, Genant HK (1992) Contribution of vertebral deformities to chronic back pain and disability. J Bone Miner Res 7:449–456
Kaptoge S, Armbrecht G, Felsenberg D, Lunt M, O’Neill TW, Silman AJ, Reeve J, EPOS study Group (2004) When should the doctor order a spine X-ray? Identifying vertebral fractures for osteoporosis care: results from the European Prospective Osteoporosis Study (EPOS). J Bone Miner Res 19:1982–1993
Siminoski K, Warshawski RS, Jen H, Lee K (2006) The accuracy of historical height loss for the detection of vertebral fractures in postmenopausal women. Osteoporos Int 17:290–296
Delmas PD, Genant HK, Crans GG, Stock JL, Wong M, Siris E, Adachi JD (2003) Severity of prevalent vertebral fractures and the risk of subsequent vertebral and nonvertebral fractures: results from the MORE trial. Bone 33:522–532
Yoshimura N, Kinoshita H, Takijiri T, Oka H, Muraki S, Mabuchi A, Kawaguchi H, Nakamura K, Nakamura T (2008) Association between height loss and bone loss, cumulative incidence of vertebral fractures and future quality of life: the Miyama study. Osteoporos Int 19:21–28
Moreno LA, Joyanes M, Mesana MI, González-Gross M, Gil CM, Sarría A, Gutierrez A, Garaulet M, Perez-Prieto R, Bueno M, Marcos A, AVENA Study Group (2003) Harmonization of anthropometric measurements for a multicenter nutrition survey in Spanish adolescents. Nutrition 19:481–486
Ulijaszek SJ, Kerr DA (1999) Anthropometric measurement error and the assessment of nutritional status. Br J Nutr 82:165–177
Norton K, Whittingham N, Carter L, Kerr D, Gore C, Marfell-Jones M (1996) Measurement techniques in anthropometry. In: Norton K, Olds T (eds) Anthropometrica. University of New South Wales Press, Sydney, pp 25–75
Grados F, Roux C, De Vernejoul MC, Utard G, Sebert JL, Fardellone P (2001) Comparison of four morphometric definitions and a semiquantitative consensus reading for assessing prevalent vertebral fractures. Osteoporos Int 12:716–722
Davies KM, Recker RR, Stegman MR, Heaney RP (1991) Tallness versus shrinkage: do women shrink with age or grow taller with recent birth date? J Bone Miner Res 6:1115–1120
AACE Osteoporosis Task Force (2003) Association of Clinical Endocrinologists medical guidelines for clinical practice for the prevention and management of postmenopausal osteoporosis. Endocr Pract 9:544–564
Brown JP, Josse RG, Scientific Advisory Council of the Osteoporosis Society of Canada (2002) Clinical practice guidelines for the diagnosis and management of osteoporosis in Canada. Can Med Assoc J 167:S1–S34
Roux C, Priol G, Fechtenbaum J, Cortet B, Liu-Léage S, Audran M (2007) A clinical tool to determine the necessity of spine radiography in postmenopausal women with osteoporosis presenting with back pain. Ann Rheum Dis 66:81–85
Manonai J, Khanacharoen A, Theppisai U, Chittacharoen A (2001) Relationship between height and arm span in women of different age groups. J Obstet Gynaecol Res 27:325–327
Chandler PJ, Bock RD (1991) Age changes in adult stature: trend estimation from mixed longitudinal data. Ann Hum Biol 18:433–440
Friedlaender JS, Costa PT, Bosse R, Ellis E, Rhoads JG, Stoudt HW (1977) Longitudinal physique changes among healthy white veterans at Boston. Hum Biol 49:541–558
Noppa H, Andersson M, Bengtsson C, Bruce A, Isaksson B (1980) Longitudinal studies of anthropometric data and body composition: the population study of women in Goteborg, Sweden. Am J Clin Nutr 33:155–162
Allali F, Maaroufi H, Aichaoui S, Khazani H, Saoud B, Benyahya B, Abouqal R, Hajjaj-Hassouni N (2007) Influence of parity on bone mineral density and peripheral fracture risk in Moroccan postmenopausal women. Maturitas 57:392–398
Allali F, El Aichaoui S, Saoud B, Maaroufi H, Abouqal R, Hajjaj-Hassouni N (2006) The impact of clothing style on bone mineral density among post menopausal women in Morocco: a case-control study. BMC Public Health 6:135
Allali F, El Aichaoui S, Khazani H, Benyahia B, Saoud B, El Kabbaj S, Bahiri R, Abouqal R, Hajjaj-Hassouni N (2008) High prevalence of hypovitaminosis D in Morocco: relationship to lifestyle, physical performance, bone markers, and bone mineral density. Semin Arthritis Rheum. doi:10.1016/j.semarthrit.2008.01.009
Versluis RG, Petri H, Van de Ven CM, Scholtes AB, Broerse ER, Springer MP, Papapoulos SE (1999) Usefulness of arm span and height comparison in detecting vertebral deformities in women. Osteoporos Int 9:129–133
Wang XF, Duan Y, Henry M, Kin BT, Seeman M (2004) Body segment lengths and arm span in healthy men and women and patients with vertebral fractures. Osteoporos Int 15:43–48
Uoglu D, Unlu F, Akyuz G (2008) Relationship between arm span and height in postmenopausal osteoporotic women. Rheumatol Int 28:737–741
Acknowledgements
This work was supported by grants from the University Mohammed V, Souissi, Rabat-Morocco and by the University Hospital of Rabat-Sale, Morocco.
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors’ contributions
We declare that we participated at the study as following:
F. Allali and N. Hajjaj-Hassouni conceived the study and supervised its design, execution, and analysis and participated in the drafting and critical review of the manuscript. F. Allali, I. Hmamouchi, and R. Abouqal did data management and statistical analyses. All other authors enrolled patients and participated in data acquisition and critical revision of the manuscript. L. Bennani wrote the paper with input from all investigators.
Rights and permissions
About this article
Cite this article
Bennani, L., Allali, F., Rostom, S. et al. Relationship between historical height loss and vertebral fractures in postmenopausal women. Clin Rheumatol 28, 1283–1289 (2009). https://doi.org/10.1007/s10067-009-1236-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-009-1236-6