Abstract
Background
Despite studies showing superior results in terms of reduced stoma rate and higher primary anastomosis rate, the safety of bridge to surgery stenting (BTS stent) for left-sided malignant colonic obstruction, especially in oncological terms, remains a concern.
Aim
The aim of this meta-analysis was to evaluate whether BTS stent is a safe alternative to emergency surgery (EmS).
Methods
Randomized control trials (RCTs) comparing BTS stent and EmS for left-sided colonic obstruction caused by primary cancer of the colon, up to Sep 2018, were retrieved from the Pubmed, Embase database, clinical trials registry of U. S. National Library of Medicine and BMJ and Google Search.
Results
There were seven eligible RCTs, involving a total of 448 patients. Compared to EmS, BTS stent had a significantly lower risk of overall complications (RR = 0.605; 95% CI 0.382–0.958; p = 0.032). However, the overall recurrence rate was higher in the BTS stent group (37.0% vs. 25.9%; RR = 1.425; 95% CI 1.002–2.028; p = 0.049). BTS stent significantly increased the risk of systemic recurrence (RR = 1.627; 95% CI 1.009–2.621; p = 0.046). This did not translate into a significant difference in terms of 3-year disease-free survival or 3-year overall survival.
Conclusion
BTS stent is associated with a lower rate of overall morbidities than EmS. However, BTS stent was associated with a greater chance of recurrence, especially systemic recurrence. Clinicians ought to be aware of the pros and cons of different interventions and tailor treatments for patients suffering from left-sided obstructing cancer of the colon.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Up to 30% of patients suffering from colorectal cancer present with acute large bowel obstruction [1,2,3]. Emergency surgery (EmS) for acute obstruction at the left colon is associated with significant morbidity and mortality [4,5,6,7]. Self-expanding metallic stent (SEMS) can be used to relieve malignant colonic obstruction in patients with resectable disease, acting as a “bridge to surgery” [8]. Despite reports quoting high technical and clinical success rates, up to over 90% [9], there is a concern that the use of SEMS as a bridge to surgery might jeopardize oncological outcomes in patients with potentially curable disease [10]. A non-randomized comparative study demonstrated poorer survival in patients with SEMS compared to those with EmS [11]. The European Society of Gastrointestinal Endoscopy guideline stated that SEMS as a bridge to surgery is not recommended for left-sided malignant colonic obstruction, except in those with increased perioperative risks [12]. Nonetheless, the opposite view was proposed by a different consensus group, supporting the use of SEMS in such circumstances [13]. At present, the benefit of SEMS as a bridge to surgery remains unclear.
As new evidence has emerged [14], there is renewed interest in the above topic. Here, we aim to evaluate the updated evidence and attempted to answer the following question: is bridge to surgery stenting (BTS stent) a safe alternative to EmS in malignant left-sided colon obstruction? The primary objective was to compare the safety parameters between the two interventions: overall complications rates, mortality rates, locoregional recurrence, and systemic recurrence rates. The secondary objective was to compare the long-term outcomes, including the overall survival and disease-free survival rates.
Methods
Studies screening and selection
The methodology was adapted from the standard guidelines from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [15]. The search was carried out by Poon and Cheung, and included articles were reviewed by Poon, Cheung, and Chiu. All studies that compared the clinical outcomes of BTS stent with EmS in managing malignant colon obstruction were retrieved from Medline (PubMed), Embase (1980–), the clinical trials registry of U.S. National Library of Medicine and BMJ and Google Search. The search was carried out in September 2018. The MeSH terms “colon obstruction,” “stent,” “surgery,” and “malignant” were used as search terms. Only these four terms were used with the intention to include more literature for preliminary screening. In addition, “left sided,” “colonic stent,” and “malignant obstruction” was used for Google Search. Only randomized control trials (RCTs) with full articles in English and those that involved patients with potential curable disease were included. Editorials, case reports, expert opinions, letters to the editor, reviews without original data, conference abstract, and studies solely on the right-sided colon obstruction were excluded.
Data extractions and quality assessments
Data extractions and quality assessments were performed by Poon, which was then confirmed by Chiu. All data were captured from published literature except the locoregional and systemic recurrence rate of the study by Tung et al., for which the data were sought directly from the author [16].
Definitions of long-term outcomes
The measurement of long-term outcomes was made with reference to the time that the patients were enrolled in the trials. The local recurrence rate was known to be affected by its definition [17]. The definition of locoregional recurrence for colon cancer used in this review was adopted from Bowne et al., which included perianastomotic, mesenteric/nodal, retroperitoneal, and peritoneal [18].
Statistical analysis
Comprehensive meta-analysis (version 3, Biostat Inc, USA) was used for analyzing the results and constructing the forest and funnel plots. The risk ratio (RR) of adverse events occurring in patients treated with BTS stent compared to the EmS group was employed to evaluate the outcomes of the two interventions, except for survival outcomes, which odds ratio (OR) was used. 95% confidence intervals (95% CI) were used to evaluate the statistical significance of the RR and OR. An RR or OR value less than 1 indicates a superior outcome for BTS stent compared to EmS, and the value was considered statistically significant when p ≤ 0.05. Assessment of heterogeneity was done by the χ2 test and represented by the inconsistency index, I2. A fixed-effect model was used when I2 ≤ 50%. A random-effect model was used when I2 > 50%. The χ2 test was not employed to determine the heterogeneities of various analyses owing to its low power in detecting heterogeneity in a small-sample-sized analysis. Publication bias was evaluated by visual evaluation of the funnel plots. Results with asymmetrical funnel plots were further analyzed by Egger’s linear regression.
Results
Search result
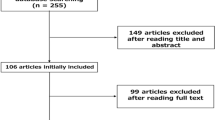
A total of 276 studies were identified. After removing duplicates, there were 274 studies remaining. After going through the titles and abstracts, 143 studies were excluded because of irrelevance or because the full articles were not available in English. A full review was performed for 131 full-text articles. A further 104 studies were excluded, and 27 studies were included for qualitative analysis. Seven trials were included for quantitative analysis (Fig. 1) [14, 16, 19,20,21,22,23,24,25].
Study characteristics
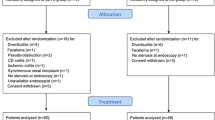
There were seven RCTs identified with a total of 448 patients (Table 1) [14, 19,20,21, 23,24,25]. There were 222 patients in the BTS stent group and 226 patients in the EmS group. The time from BTS stent to curative surgery ranged from 5 to 14 days. Two more publications reported the long-term follow-up results of previously published RCTs [16, 22]. There were four single-center trials [19, 23,24,25] and three multicenter trials [14, 20, 21]. Short-term outcomes were reported in seven publications [14, 19,20,21, 23,24,25]. Long-term outcomes were reported in five publications (Table 2) [14, 16, 22, 24, 25]. Three out of the seven RCTs were prematurely terminated. Two RCTs were stopped because of a high perforation rate in the BTS stent arm [20, 21] and one was stopped because of a high anastomotic leakage rate in the EmS arm [25].
Critical appraisal
All included studies reported random sequence generation and allocation concealment, resulting in a low risk of selection bias. The blinding of patients and personnel was considered impractical and was not assessed. The blinding of the assessor was unclear in two studies [19, 24] and not done in four trials [14, 16, 20, 23, 25]. There were four studies with high risk of performance bias due to variations in practices (e.g., choice of EmS, among different surgeons and different centers, some explained by their multi-center nature) [19,20,21,22]. Two trials were regarded as having high attrition bias due to a high dropout rate [21] and premature closure [25]. One study was considered at high risk of reporting bias as only the overall survival, without the disease-free survival, was reported [25]. The risk of bias assessment is summarized in Fig. 2. As the number of included studies was small, the funnel plots and Egger’s test did not show useful information.
Overall complications rate
The morbidities associated with the two interventions were reported in seven publications [14, 19,20,21, 23,24,25], with a total sample size of 447. Regarding the overall complications rate, the risk was significantly reduced by the BTS stent with a RR of 0.605 (p = 0.032; 95% CI 0.382–0.958). However, the results of individual studies on the occurrence of adverse events were quite heterogeneous with an I2 value of 72.8% (Fig. 3A).
The 30-day mortality rate
In total, five studies with 338 patients were included in the 30-day mortality rate analysis [14, 19,20,21, 25]. There were 166 and 172 patients in the BTS stent group and EmS group, respectively. The overall RR was 0.963 (95% CI 0.468–1.982; p = 0.918) (Fig. 3B). No significant difference was noted between the two interventions. The included studies were homogeneous (I2 = 0.0%), and the funnel plot was symmetrical.
Locoregional and systemic recurrences
Five studies with a total of 293 patients reported on the recurrence rate. The median follow-ups in the BTS stent and EmS groups were compared using a two-tailed Mann Whitney U test, and no significant difference was detected. The overall recurrence rates were 37.0% and 25.9% for BTS stent and EmS, respectively. A statistically significant RR of 1.425 (95% CI 1.002–2.028; p = 0.049) was detected, suggesting a higher risk of overall recurrence in the BTS stent group (Fig. 4A).
The analysis on the pattern of recurrence revealed a significantly greater chance of systemic recurrence with an RR of 1.627 (95% CI 1.009–2.621; p = 0.046) in the BTS stent group (Fig. 4B). 37 of 146 (25.3%) patients from the BTS stent group developed systemic recurrence, whereas 22 of 147 (15.0%) patients in the EmS group developed systemic recurrence. All RRs from individual RCTs (i.e., RR > 1) favored EmS, despite their lack of statistical significance individually, and the result was homogenous with I2 = 0.0%. The loco-regional recurrence rates were 11.60% and 10.9% for BTS stent and EmS, respectively. The RR was 1.110 (95% CI 0.593–2.078; p = 0.745), and the risk was not statistically significant (Fig. 4C).
Three-year disease-free survival and overall survival
There were three studies including a total of 206 patients that reported 3-year disease-free survival [14, 16, 22]. Pooled analysis showed comparable results between the two interventions (OR = 1.429; 95% CI 0.801–2.550; p = 0.227) (Fig. 5A). Four studies with a total of 233 patients reported on the 3-year overall survival [14, 16, 22, 25]. Pooled analysis showed no significant difference between the two interventions (OR = 1.659; 95% CI 0.930–2.962; p = 0.087) (Fig. 5B).
Sensitivity test
Sensitivity tests were performed on the 30-day mortality and overall complications. By alternatively removing individual studies, the 30-day mortality remained comparable between the BTS stent and EmS group. The RR was 0.834 (95% CI 0.360–1.932; p = 0.672) and 1.051 (95% CI 0.496–2.227; p = 0.897) after removing the largest and smallest study, respectively. The risk of overall complications remained significant after excluding the largest study (RR = 0.505; 95% CI 0.269–0.948; p = 0.034) but became insignificant after removing the smallest study (RR = 0.659, 95% CI 0.417–1.042; p = 0.074). The result also becomes insignificant when the study by Cheung et al. [23] was excluded. A sensitivity test was not performed for survival and recurrence rates due to the scarcity of studies included.
Discussion
The advantage of using SEMS to relieve obstruction in left-sided colon cancer is that it converts an emergency operation into a semi-elective one, with patients spared from the high operative risks and potential morbidities associated with emergency colorectal resections. A meta-analysis found that 78% of patients who underwent BTS stent were able to undergo a single-stage surgery with primary anastomosis [26]. Although not all studies favored BTS stent [27], multiple meta-analyses showed that BTS stent was associated with lower complication rates, higher primary anastomosis rate, and lower permanent stoma rate compared to EmS [28,29,30,31,32]. However, the majority of these meta-analyses focused only on the short-term outcomes. The concern that, despite having a superior short-term outcome, BTS stent may jeopardize the long-term oncological outcome of patients with potentially curable cancers was not addressed.
Part of the reason why earlier meta-analyses did not focus on long-term outcomes was because of a scarcity of data. In fact, few comparative studies reported long-term outcomes. Of those that did, many were retrospective non-randomized studies [33, 34]. The results from the ESCO trial, a multicenter randomized controlled trial published recently, provided more data in this regard and allowed better analysis of the long-term outcomes from BTS stent [14].
This meta-analysis shows lower complication for BTS stent than EmS. The overall and disease-free survival rates were comparable. These findings were in line with previous meta-analyses [29, 31, 32, 35, 36]. However, those with BTS stent were more prone to overall and systemic recurrences. Locoregional recurrence is primarily related to the failure of local control, which, in the case of cancer of the colon, is surgical resection. Systemic recurrence is, however, more related to the dissemination of cancer cells from the primary tumor before resection. The systemic recurrence rate is more relevant in the evaluation of whether BTS stent has an adverse impact on oncological outcomes. To date, this is the first meta-analysis that analyzed systemic and locoregional recurrence rates following BTS stents and EmS and showing an inferior oncological outcome in BTS stent from data derived from RCTs.
Sloothaak et al. performed a subgroup analysis for the Dutch Stent-in 2 trial and demonstrated that those who had perforation after BTS stent were at increased risk of recurrence, compared to those without perforation [22]. Three European multicenter trials were prematurely terminated due to a high perforation rate, 6.6%, 12.77%, and 54.44% [20, 21, 37]. It was noted that a high percentage of patients in these trials suffered from complete obstruction [20, 21]. It is reassuring to see that these high perforation rates were not seen in later studies [38]. But apart from clinical perforation, silent perforation could occur. Sloothaak et al. also reported that microperforation was noted in 10% of the resected specimens from patients who had prior stent insertion. Unlike clinical perforation, which is usually procedure- and technique-related, silent perforation is related to stent expansion and is highly unpredictable and, therefore, difficult to prevent.
However, perhaps stent-related perforation is not the only explanation of poorer oncological outcome in patients with BTS stent. Some postulated that forceful expansion of the gut lumen and tumor by SEMS, even in the absence of perforation, could introduce cancer cells into surrounding vessels and facilitate hematological tumor dissemination. Maruthachalam et al. detected an increase in the expression of CK20 micro RNA in the peripheral blood samples of patients after SEMS insertion [39]. Malgras et al. demonstrated a higher incidence of peritoneal carcinomatosis and poorer survival after colonic stenting in a mouse model [40]. Stenting itself might also have an impact on tumor biology. Two studies reported a higher incidence of perineural invasion in resected specimens after BTS stent, albeit not translating into poor survival in one of them [41, 42].
The overall survival and disease-free survival of BTS stent and EmS were comparable in this meta-analysis, despite a higher risk of systematic recurrence in the BTS stent group. The available data from the RCTs only allowed pooled analysis for 3-year survival outcomes. Therefore, it remains a possibility that the effect of systematic recurrence was not reflected in a relatively short period. Also, only three RCTs reported disease-free survival.
There are limitations to this meta-analysis. One of the major limitations of this analysis was that there are a limited number of long-term results from RCTs in the literature, and hence the sample size was somewhat inadequate to answer the question of whether BTS stent hurts long-term outcomes. It is unlikely that eligible studies were missed in this review. However, given the skepticism about BTS stent, conducting large-scale RCTs in the future would be extremely difficult [10]. Hopefully, the long-term follow-up results of some of the RCTs will be available in the future and help to address this issue. Another limitation was that EmS encompasses a wide variety of surgical procedures, each with a different clinical impact. Analyzing them as a single entity is far from ideal but often unavoidable.
Conclusion
BTS stent provided a favorable short-term outcome by reducing the overall complications in the treatment of malignant left-sided colonic obstruction. The 30-day mortality rate of BTS stent was comparable to EmS. In terms of long-term outcomes, both interventions have a similar 3-year disease-free survival and overall survival rate. However, BTS stent was associated with a higher incidence of systemic and overall recurrence. Therefore, this meta-analysis could not demonstrate that BTS stent is an oncologically safe alternative to EmS. Physicians should be aware of the pros and cons of BTS stent. The short-term advantages of BTS stent should be weighed against the potential long-term oncological hazards.
References
Kyllonen LE (1987) Obstruction and perforation complicating colorectal carcinoma. An epidemiologic and clinical study with special reference to incidence and survival. Acta Chir Scand 153:607–614
Waldron RP, Donovan IA, Drumm J, Mottram SN, Tedman S (1986) Emergency presentation and mortality from colorectal cancer in the elderly. Br J Surg 73:214–216
Deans GT, Krukowski ZH, Irwin ST (1994) Malignant obstruction of the left colon. Br J Surg 81:1270–1276
Lee YM, Law WL, Chu KW, Poon RT (2001) Emergency surgery for obstructing colorectal cancers: a comparison between right-sided and left-sided lesions. J Am Coll Surg 192:719–725
De Salvo GL, Gava C, Pucciarelli S, Lise M (2004) Curative surgery for obstruction from primary left colorectal carcinoma: primary or staged resection? Cochrane Database Syst Rev Cd002101
Sjo OH, Larsen S, Lunde OC, Nesbakken A (2009) Short term outcome after emergency and elective surgery for colon cancer. Colorectal Dis 11:733–739
Iversen LH, Bulow S, Christensen IJ, Laurberg S, Harling H (2008) Postoperative medical complications are the main cause of early death after emergency surgery for colonic cancer. Br J Surg 95:1012–1019
Foo CC, Poon JT, Law WL (2011) Self-expanding metallic stents for acute left-sided large-bowel obstruction: a review of 130 patients. Colorectal Dis 13:549–554
Watt AM, Faragher IG, Griffin TT, Rieger NA, Maddern GJ (2007) Self-expanding metallic stents for relieving malignant colorectal obstruction: a systematic review. Ann Surg 246:24–30
Suen MK, Zahid A, Young JM, Rodwell L, Solomon MJ, Young CJ (2015) How to decide to undertake a randomized, controlled trial of stent or surgery in colorectal obstruction. Surgery 157:1137–1141
Sabbagh C, Browet F, Diouf M, Cosse C, Brehant O, Bartoli E, Mauvais F, Chauffert B, Dupas JL, Nguyen-Khac E, Regimbeau JM (2013) Is stenting as “a bridge to surgery” an oncologically safe strategy for the management of acute, left-sided, malignant, colonic obstruction? A comparative study with a propensity score analysis. Ann Surg 258:107–115
van Hooft JE, van Halsema EE, Vanbiervliet G, Beets-Tan RG, DeWitt JM, Donnellan F, Dumonceau JM, Glynne-Jones RG, Hassan C, Jimenez-Perez J, Meisner S, Muthusamy VR, Parker MC, Regimbeau JM, Sabbagh C, Sagar J, Tanis PJ, Vandervoort J, Webster GJ, Manes G, Barthet MA, Repici A (2014) Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 46:990–1053
Ansaloni L, Andersson RE, Bazzoli F, Catena F, Cennamo V, Di Saverio S, Fuccio L, Jeekel H, Leppaniemi A, Moore E, Pinna AD, Pisano M, Repici A, Sugarbaker PH, Tuech JJ (2010) Guidelenines in the management of obstructing cancer of the left colon: consensus conference of the world society of emergency surgery (WSES) and peritoneum and surgery (PnS) society. World J Emerg Surg 5:29
Arezzo A, Balague C, Targarona E, Borghi F, Giraudo G, Ghezzo L, Arroyo A, Sola-Vera J, De Paolis P, Bossotti M, Bannone E, Forcignano E, Bonino MA, Passera R, Morino M (2017) Colonic stenting as a bridge to surgery versus emergency surgery for malignant colonic obstruction: results of a multicentre randomised controlled trial (ESCO trial). Surg Endosc 31:3297–3305
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6:e1000100
Tung KL, Cheung HY, Ng LW, Chung CC, Li MK (2013) Endo-laparoscopic approach versus conventional open surgery in the treatment of obstructing left-sided colon cancer: long-term follow-up of a randomized trial. Asian J Endosc Surg 6:78–81
Marsh PJ, James RD, Schofield PF (1995) Definition of local recurrence after surgery for rectal carcinoma. Br J Surg 82:465–468
Bowne WB, Lee B, Wong WD, Ben-Porat L, Shia J, Cohen AM, Enker WE, Guillem JG, Paty PB, Weiser MR (2005) Operative salvage for locoregional recurrent colon cancer after curative resection: an analysis of 100 cases. Dis Colon Rectum 48:897–909
Ho KS, Quah HM, Lim JF, Tang CL, Eu KW (2012) Endoscopic stenting and elective surgery versus emergency surgery for left-sided malignant colonic obstruction: a prospective randomized trial. Int J Colorectal Dis 27:355–362
Pirlet IA, Slim K, Kwiatkowski F, Michot F, Millat BL (2011) Emergency preoperative stenting versus surgery for acute left-sided malignant colonic obstruction: a multicenter randomized controlled trial. Surg Endosc 25:1814–1821
van Hooft JE, Bemelman WA, Oldenburg B, Marinelli AW, Lutke Holzik MF, Grubben MJ, Sprangers MA, Dijkgraaf MG, Fockens P (2011) Colonic stenting versus emergency surgery for acute left-sided malignant colonic obstruction: a multicentre randomised trial. Lancet Oncol 12:344–352
Sloothaak DA, van den Berg MW, Dijkgraaf MG, Fockens P, Tanis PJ, van Hooft JE, Bemelman WA (2014) Oncological outcome of malignant colonic obstruction in the Dutch Stent-In 2 trial. Br J Surg 101:1751–1757
Cheung HY, Chung CC, Tsang WW, Wong JC, Yau KK, Li MK (2009) Endolaparoscopic approach vs conventional open surgery in the treatment of obstructing left-sided colon cancer: a randomized controlled trial. Arch Surg 144:1127–1132
Ghazal AH, El-Shazly WG, Bessa SS, El-Riwini MT, Hussein AM (2013) Colonic endolumenal stenting devices and elective surgery versus emergency subtotal/total colectomy in the management of malignant obstructed left colon carcinoma. J Gastrointest Surg 17:1123–1129
Alcantara M, Serra-Aracil X, Falco J, Mora L, Bombardo J, Navarro S (2011) Prospective, controlled, randomized study of intraoperative colonic lavage versus stent placement in obstructive left-sided colonic cancer. World J Surg 35:1904–1910
Sebastian S, Johnston S, Geoghegan T, Torreggiani W, Buckley M (2004) Pooled analysis of the efficacy and safety of self-expanding metal stenting in malignant colorectal obstruction. Am J Gastroenterol 99:2051–2057
Kwak MS, Kim WS, Lee JM, Yang DH, Yoon YS, Yu CS, Kim JC, Byeon JS (2016) Does stenting as a bridge to surgery in left-sided colorectal cancer obstruction really worsen oncological outcomes? Dis Colon Rectum 59:725–732
Cirocchi R, Farinella E, Trastulli S, Desiderio J, Listorti C, Boselli C, Parisi A, Noya G, Sagar J (2013) Safety and efficacy of endoscopic colonic stenting as a bridge to surgery in the management of intestinal obstruction due to left colon and rectal cancer: a systematic review and meta-analysis. Surg Oncol 22:14–21
Huang X, Lv B, Zhang S, Meng L (2014) Preoperative colonic stents versus emergency surgery for acute left-sided malignant colonic obstruction: a meta-analysis. J Gastrointest Surg 18:584–591
Tan CJ, Dasari BV, Gardiner K (2012) Systematic review and meta-analysis of randomized clinical trials of self-expanding metallic stents as a bridge to surgery versus emergency surgery for malignant left-sided large bowel obstruction. Br J Surg 99:469–476
Allievi N, Ceresoli M, Fugazzola P, Montori G, Coccolini F, Ansaloni L (2017) Endoscopic stenting as bridge to surgery versus emergency resection for left-sided malignant colorectal obstruction: an updated meta-analysis. Int J Surg Oncol 2017:2863272
Wang X, He J, Chen X, Yang Q (2017) Stenting as a bridge to resection versus emergency surgery for left-sided colorectal cancer with malignant obstruction: a systematic review and meta-analysis. Int J Surg 48:64–68
Ho KM, Chan KM, Kwok SY, Lau PY (2017) Colonic self-expanding metal stent (SEMS) as a bridge to surgery in left-sided malignant colonic obstruction: an 8-year review. Surg Endosc 31:2255–2262
Quereshy FA, Poon JT, Law WL (2014) Long-term outcome of stenting as a bridge to surgery for acute left-sided malignant colonic obstruction. Colorectal Dis 16:788–793
Cennamo V, Luigiano C, Coccolini F, Fabbri C, Bassi M, De Caro G, Ceroni L, Maimone A, Ravelli P, Ansaloni L (2013) Meta-analysis of randomized trials comparing endoscopic stenting and surgical decompression for colorectal cancer obstruction. Int J Colorectal Dis 28:855–863
De Ceglie A, Filiberti R, Baron TH, Ceppi M, Conio M (2013) A meta-analysis of endoscopic stenting as bridge to surgery versus emergency surgery for left-sided colorectal cancer obstruction. Crit Rev Oncol Hematol 88:387–403
van Hooft JE, Fockens P, Marinelli AW, Timmer R, van Berkel AM, Bossuyt PM, Bemelman WA (2008) Early closure of a multicenter randomized clinical trial of endoscopic stenting versus surgery for stage IV left-sided colorectal cancer. Endoscopy 40:184–191
Matsuzawa T, Ishida H, Yoshida S, Isayama H, Kuwai T, Maetani I, Shimada M, Yamada T, Saito S, Tomita M, Koizumi K, Hirata N, Sasaki T, Enomoto T, Saida Y (2015) A Japanese prospective multicenter study of self-expandable metal stent placement for malignant colorectal obstruction: short-term safety and efficacy within 7 days of stent procedure in 513 cases. Gastrointest Endosc 82:697–7071
Maruthachalam K, Lash GE, Shenton BK, Horgan AF (2007) Tumour cell dissemination following endoscopic stent insertion. Br J Surg 94:1151–1154
Malgras B, Brulle L, Lo Dico R, El Marjou F, Robine S, Therwath A, Pocard M (2015) Insertion of a stent in obstructive colon cancer can induce a metastatic process in an experimental murine model. Ann Surg Oncol 22(Suppl 3):S1475–S1480
Sabbagh C, Chatelain D, Trouillet N, Mauvais F, Bendjaballah S, Browet F, Regimbeau JM (2013) Does use of a metallic colon stent as a bridge to surgery modify the pathology data in patients with colonic obstruction? A case-matched study. Surg Endosc 27:3622–3631
Kim HJ, Choi GS, Park JS, Park SY, Jun SH (2013) Higher rate of perineural invasion in stent-laparoscopic approach in comparison to emergent open resection for obstructing left-sided colon cancer. Int J Colorectal Dis 28:407–414
Acknowledgements
The authors thank Dr. Karen Tung, Pamela Youde Nethersole Eastern Hospital, Hong Kong, China for providing the additional information regarding the long-term results of the study conducted in her center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Chi Chung Foo, Samuel Ho Ting Poon, Rosemaire Hon Yiu Chiu, Wai Yiu Lam, and Lam Chi Cheung and Professor Wai Lun Law have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Foo, C.C., Poon, S.H.T., Chiu, R.H.Y. et al. Is bridge to surgery stenting a safe alternative to emergency surgery in malignant colonic obstruction: a meta-analysis of randomized control trials. Surg Endosc 33, 293–302 (2019). https://doi.org/10.1007/s00464-018-6487-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6487-3