Abstract
Background
Traditionally, left-sided acute bowel obstruction is treated by a staged procedure because immediate resection and anastomosis in a massive distended and unprepared colon carries a high complication rate. Total abdominal colectomy is a one-stage procedure that will remove synchronous proximal neoplasms, reduce the risk of subsequent metachronous tumor, and avoid stoma. Colorectal stents are being used for palliation and as a bridge to surgery in obstructing colorectal carcinoma, making elective surgery straightforward, enabling easily mobilization and resection of the colon with a possible trend toward reduction in postoperative complication rates compared to emergency surgery. The purpose of this work was to compare the procedures of endoscopic stenting followed by elective colectomy versus total abdominal colectomy and ileorectal anastomosis in the management of acute obstructed carcinoma of the left colon as regards feasibility, safety, and clinical outcomes
Methods
From January 2009 through May 2012, 60 patients were randomized to either emergency stenting followed by elective resection (ESER group) or total abdominal colectomy and ileorectal anastomosis (TACIR group).
Results
Twenty nine patients (96.7 %) had successful stenting and underwent elective surgery 7–10 days later (ESER group). Postoperative complications were encountered in four patients in the ESER group compared to 15 patients in the TACIR group (p = 0.012). Anastomotic leakage was encountered in one patient (3.3 %) in the TACIR group. There were no operative mortalities in the present study. Within the first three postoperative months, the TACIR group patients had significantly more frequent bowel motions per day compared to the ESER group patients although (p = 0.013). In both study groups, the follow-up duration ranged from 6 to 40 months with a median of 18 months. Recurrent disease was encountered in five patients (17.2 %) in the ESER group compared to four patients (13.3 %) in the TACIR group (p = 0.228).
Conclusion
Both techniques are feasible, safe, and produce comparable oncological outcomes. However, endoscopic stenting followed by elective resection was associated with significantly less postoperative complications and bowel motions per day.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute malignant colonic obstruction is a common surgical emergency that is associated with significant morbidity and mortality.1,2 Despite widespread colorectal cancer screening programs, approximately a fourth of patients with colorectal malignancy present with acute colonic obstruction.2–4 Traditionally, left-sided acute colonic obstruction is treated by a staged procedure because immediate resection and anastomosis in a massively distended and unprepared colon carries high morbidity and mortality rates.5–8 Patients undergoing a one-stage emergency curative operation for obstructing tumors will have a lower survival probability than patients with non-obstructing lesions.9 In some patients, improved outcome after emergency surgery for colorectal cancer has been reported.10 This improvement was hypothesized to be due to more aggressive emergency surgery and the increase in primary resections.10 A two-stage procedure, involving segmental resection of obstructed bowel followed by either Hartmann’s closure of the distal stump or exteriorization of the stump as a mucous fistula with proximal bowel exteriorized as an end stoma is a popular approach because it is quick, does not risk anastomotic leakage and is technically less demanding than a single-stage operation. After the initial surgery, patients must wait at least 8 weeks before the colostomy can be safely reversed, and they often are required to wait much longer for adequate bowel continuity to be restored.11,12 Furthermore, many patients cannot undergo reversal of the colostomy because of advanced age and comorbid conditions and thus must be content with a permanent stoma.3,13 In addition to the increased costs associated with stoma care, these patients report a significantly lower mean health-related quality of life than similar patients without a colostomy.14–17 Therefore, the main disadvantages are that up to 60 % of stomas are never reversed, the expense and morbidity of the takedown procedure are significant, and patients have to make physical and psychological adjustments to live with a stoma.12 Primary resection and anastomosis with a proximal diverting stoma is an alternative to two-stage procedure that may be adopted in high risk anastomosis; on the other hand, the classic three-stage operation is usually challenged because of its high cumulative mortality and morbidity rates and compromised long-term survival resulting from delay in resection of the tumor.18,19 This procedure is rarely performed any more except in very poor risk patients.
In evaluating risk factors for patients presenting as surgical emergencies due to colorectal cancer, emergency patients had more advanced tumors, were older, and were much more likely to be widowed.20 Emergency bowel surgery in the elderly is significantly affected by delayed admission, nature and extent of bowel disease, pre-existing cardiopulmonary disease, presence of generalized peritonitis, requirement of bowel resection, and procedure choice.21 Increasingly, studies have been published advocating the advantages of primary resection with immediate anastomosis, the potential benefits include shorter hospital stay, reduced mortality and morbidity rates, and avoidance of stoma.22–25 One of the arguments for subtotal colectomy is that this procedure will remove synchronous proximal neoplasms and reduce the risk of subsequent metachronous tumor development compared with segmental resection.26–28 However, when the obstructed tumor is located at the recto-sigmoid junction and removal of the upper rectum is mandatory, a small rectal stump with reduced capacity usually result in increased daily bowel motions and possibility of fecal incontinence.29 Moreover, it is recognized that emergency abdominal surgery is associated with higher risks of death and complications than the same operation performed on an elective basis.4 In this setting, therefore, a technique that alleviates obstruction, while allowing for surgery to be delayed, may be useful. Endoscopic colonic stent insertion is advocated as a “bridge to surgery” in patients with potentially resectable malignant disease.30–32 An endoscopically placed stent relieves symptoms of colonic obstruction and allows for medical resuscitation, optimization of co-morbid disorders, bowel preparation, and staging.33,34 The colonic tumor can then be resected electively, thereby, in theory, decreasing surgical risk of complications and death.35 Self-expanding metallic stents have been used previously for palliative treatment of obstructed advanced unresectable colorectal cancer. Recently, there have been reports of colonic stents to relieve colonic obstruction temporarily, followed by elective definitive resection of the tumor at a later date.11 Colonic stent placement may not be technically possible or clinically successful, and the procedure is associated with risks of bleeding, stent migration, and bowel perforation. In addition, self-expanding metallic stents are expensive and can be placed only by physicians with specialized training.
The purpose of this work was to compare the procedures of endoscopic stenting for relief of obstruction followed by elective colectomy versus total abdominal colectomy and ileorectal anastomosis (TACIR) in the management of acute obstructed carcinoma of the left colon as regards feasibility, safety, and clinical outcomes.
Patients and Methods
The study was approved by the ethics committees of both the General Surgery Department and the Faculty of Medicine of the University of Alexandria, Alexandria, Egypt. An informed consent was obtained from all patients who agreed to participate in the study. Eligible participants were patients presenting with acute left colonic obstruction confirmed by a computed tomography of the abdomen. Exclusion criteria included patients with distal rectal cancer less than 8 cm from the anal verge, patients with signs of peritonitis, and the presence of metastatic disease and/or carcinomatosis. Following preoperative evaluation, patients were randomly assigned to undergo either emergency stenting followed by elective resection within the following 7–10 days (ESER group) or total abdominal colectomy and ileorectal anastomosis (TACIR group). Randomization was performed using a pseudorandom number generator with individual assignments concealed in sequentially numbered sealed envelopes that were opened in order when assignments were made. Randomization and patients’ allocation in either group were managed by an independent observer.
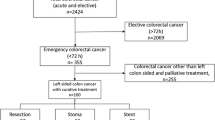
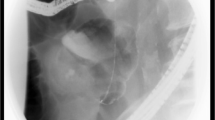
In the ESER group, patients had upfront endoscopic placement, under fluoroscopic guidance, of a colonic stent across the obstruction according to the standard technique described elsewhere.36–38 Following successful stent placement (Fig. 1), the patient was admitted to a general surgical ward, received a colonic purge, and subsequently underwent elective tumor resection and primary anastomosis within 7–10 days of stent placement. Resection options included either a left hemicolectomy or an anterior resection (Fig. 2). Full colonoscopy to exclude synchronous lesions was attempted in all patients prior to start of surgery.
In the TACIR group, total abdominal colectomy and ileorectal anastomosis was performed for every patient regardless of age or gender. Laparotomy was performed through a midline incision. The site and nature of left colon obstruction was confirmed, and when necessary, obstructed large bowel was decompressed by insertion of a needle attached to a suction apparatus. Gaseous decompression of colon allowed through examination of the liver and the peritoneum to exclude the presence of metastases and/or peritoneal carcinomatosis.
The patients’ demographic characteristics, associated comorbidities, operative data, postoperative complications, and duration of hospital stay were recorded. Follow-up was performed on three-monthly basis in the first postoperative year, six-monthly basis in the second postoperative year, and yearly thereafter. Follow-up regimen in the first 2 postoperative years included serum carcinoembryonic antigen measurement every 3 months, abdominal ultrasonography every 6 months, and an abdominal computed tomography and plain X-ray of the chest yearly.
Statistical Analysis
Because there were no previous studies comparing the surgical outcomes of emergency colonic stenting followed by elective resection to emergency TAC and ileorectal anastomosis, no effect size could be calculated and consequently no sample size could be determined. Having 30 patients per group seemed reasonable as it approximates the sample size in other analogous studies. It was therefore intended to end the study when 30 patients allocated to each treatment group completed the study. All data analysis was performed with the Statistical Package for the Social Sciences version 17 software (SPSS, Chicago, IL, USA). The Mann–Whitney U test and the Student’s t test were used for continuous variables. The chi-squared and the Fisher's exact test were used for categorical variables. All P values were two-sided. A P < 0.05 was considered statistically significant. Values are expressed as mean ± SD unless otherwise stated.
Results
From January 2009 through May 2012, 60 patients presenting with acute left-sided colonic obstruction matched the eligibility criteria. They were 37 females (61.7 %) and 23 males (38.3 %). Their age ranged from 35 to 68, with a median of 44 years. Following initial evaluation and preparation, patients were randomly assigned to either the ESER group (30 patients) or the TACIR group (30 patients). The patients’ demographic characteristics, associated co-morbidities, location of the tumor, and TNM stage are shown in Table 1.
Endoscopic colonic stenting was attempted in all patients of ESER group and was successful in 29 patients (96.7 %). Stent placement was technically unsuccessful in one patient (3.3 %) who had a rectosigmoid cancer due to failure of passage of the guide-wire through the obstructing lumen and fear of inducing perforation. This patient underwent emergency total abdominal colectomy and ileorectal anastomosis and was excluded from further analysis. A 10-cm stent was inserted in 24 patients while a 12-cm stent was inserted in the remaining five patients. Bowel function was restored at a median of 6 h (range; 2–12) in all patients. No complications were encountered during stent placement or after insertion till the time of definitive surgery.
Table 2 illustrates the operative details of both study groups: significantly less mean operative time, mean intraoperative blood loss, and less patients requiring whole blood and/or fresh frozen plasma (p < 0.001). Postoperative complications were encountered in four patients in the ESER group compared to 15 patients in the TACIR group (p = 0.012). Table 3 illustrates the postoperative complications encountered in both study groups. Anastomotic leakage was encountered in one patient (3.3 %) in the TACIR group. This was female patient who developed discharge of intestinal content from the drain site after discharge on the 15th postoperative day. The patient was re-admitted to the hospital where ultrasound abdomen was done and revealed no intra-abdominal collection. Non-operative measures including correction of serum albumin level were followed by complete cessation of the discharge. No statistically significant difference was found between both study groups as regards the median hospital stay. There were no operative mortalities in the present study.
Within the first three postoperative months, the TACIR group patients had significantly more frequent bowel motions per day compared to the ESER group patients although (p = 0.013). This difference tended to disappear after the sixth postoperative month.
In both study groups, the follow-up duration ranged from 6 to 40 months with a median of 18 months. Recurrent disease was encountered in five patients (17.2 %) in the ESER group compared to four patients (13.3 %) in the TACIR group (p = 0.228). In the ESER group, two patient (6.9 %) developed local recurrence while three patients (10.3 %) developed multiple liver metastases that were not amenable to surgical resection. In the TACIR group, one patient (3.3 %) developed local recurrence while three patients (10 %) developed distant metastases. One patient (3.3 %) developed a single right lobe liver metastasis that was managed by radiofrequency ablation while the other two patients (6.9 %) developed both liver and brain metastases. The three patients who developed local recurrence in the present study had bulky circumferential stage III tumors. Adjuvant chemotherapy was given to all stage II and III patients.
Discussion
Acute malignant colonic obstruction is a common surgical emergency. Despite widespread colorectal cancer screening, approximately a fourth of patients with colorectal malignancy present with acute colonic obstruction.1,2 Up to 85 % of acute colonic obstruction is due to malignancy and between 10 and 30 % of patients with colonic cancer present with obstructive symptoms. Emergency operation is associated with high morbidity and mortality rates and often results in temporary or permanent colostomy. Surgery on the unprepared bowel carries high morbidity (10–36 %) and high mortality (6–30 %) rates compared to elective procedures which have lower morbidity (4–14 %) and mortality (1–7 %) rates.39,40
Self-expanding metal stents have been used in esophageal, biliary, hepatic, and vascular obstruction. Technological advances and the introduction of flexible stents with larger lumen have facilitated their use in colonic obstruction. Endoscopic colonic stent insertion is advocated as a “bridge to surgery” in patients with potentially resectable malignant disease.30,32 An endoscopically placed stent relieves symptoms of colonic obstruction and allows for medical resuscitation, optimization of co-morbid conditions, bowel preparation, and staging.33,34 The colonic tumor can then be resected electively, thereby, in theory, decreasing surgical risk of complications and death.35 This was evident in the present study by the lower incidence of both wound infection and chest infection in the ESER group. Furthermore, bowel decompression and preparation increases the likelihood of successful primary anastomosis and minimizes the need for colostomy. This was also evident in the present study by the significantly lower operative time and operative blood loss in the ESER group which reflects the easier handling, manipulation, and dissection of the non-obstructed non-distended colon.
There was no significant difference between both groups as regards anastomotic leakage. Although minor leakage was encountered in one patient of the TACIR group, however, this leakage stopped spontaneously on conservative measures reflecting that bowel preparation is an important item before surgery to avoid such complication. On the other hand, no post-operative mortality was encountered in both groups denoting the effectiveness and safety of both techniques in the management of acute left-sided colonic obstruction despite of the minor complications encountered. Neither perforation nor other complications related to stent placement were encountered in the present study. Only in one patient, we failed to insert the stent safely due to failure of passage of the guide wire.
One-stage resection and anastomosis (TACIR) have several advantages including saving of time and reduction in hospital costs, avoidance of the risk of a second operation, elimination of the waiting period because of a second operation, avoidance of the trouble and embarrassment resulting from a temporary colostomy, and finally offering a better quality for patients.27 This was evident in the present study as the median hospital stay was significantly lower in the TACIR group compared to the ESER group which can be explained by the fact that after successful placement of stent, the patient was admitted to a general surgical ward and subsequently underwent elective tumor resection and primary anastomosis within 7–10 days of stent placement. Based on this initial experience, the authors speculate that it might be possible to wait less than 7–10 days depending on the general condition of the patient and the time required for correction of fluid and electrolyte imbalance
The other rationale for TACIR is based on the fact that there may be synchronous lesions of colorectal cancer at the time of presentation. In a series by Arnaud et al., there were 6.8 % synchronous colorectal cancers at the time of acute presentation, and this was evident in one patient in the TACIR group.41 Thus, another advantage of this procedure is that the operation deals with any synchronous tumors and minimizes metachronous colonic tumors.
A major functional issue with TACIR has been the increased frequency of bowel movements, which averaged two to four bowel movements per day in some studies.42,43 In the present study, patients with TACIR experienced a median of six bowel motions per day within the first three postoperative months compared to a median of two bowel motions per day in the ESER group during the same period. Although the difference in the frequency of bowel motions per day between both study groups was statistically significant (p = 0.013), however, this difference was temporary and tended to disappear after the sixth postoperative month.
In the ESER group, two patient (6.9 %) developed local recurrence compared to one patient (3.3 %) in the TACIR group. All three patients had stage III cancers and presented in obstruction. This may explain the relatively early local recurrence. Small sample size probably explains why the local recurrence rate in the ESER group is double that in the TACIR group in the present study. Larger numbers of patient are required to confirm whether this difference truly exists.
The present study had shown that patients who present with acute left-sided colonic obstruction may be treated by either technique. Both techniques are feasible, safe, and produce comparable oncological outcomes. Although endoscopic stent placement followed by elective resection was associated with significantly less postoperative complications and bowel motions per day, however, its high price precludes its routine use at least in our country (the cost averages about 7,000 Egyptian pounds).
References
Boyle P. Some recent developments in the epidemiology of colorectal cancer. In: Bleiberg HRP, Wilke H-J, editors. Management of colorectal cancer. London: Martin Dunitz; 1998. p. 19–34.
Ohman U. Prognosis in patients with obstructing colorectal carcinoma. Am J Surg 1982;143:742–7.
Deans GT, Krukowski ZH, Irwin ST. Malignant obstruction of the left colon. Br J Surg 1994;81:1270–6.
Riedl S, Wiebelt H, Bergmann U, Hermanek P Jr. Postoperative complications and fatalities in surgical therapy of colon carcinoma. Results of the German multicenter study by the Colorectal Carcinoma Study Group. Chirurg 1995;66:597–606.
Clark J, Hall A, Mussa AR . Treatment of obstructing cancer of the colon and rectum. Surg Gynec Obstet. 1975; 141: 541–544.
Carson SN, Poticha SM, Shields TW. Carcinoma obstructing the left side of the colon. Arch Surg. 1977; 122: 523–526.
Deutsh AA, Zelikovski A, Strenberg A, Reiss R. One-stage subtotal-colectomy with anastomosis for obstructing carcinoma of the left colon. Dis. Colon rectum 1983; 26: 227–230.
McArdle CS, Hole DJ. Emergency presentation of colorectal cancer is associated with poor 5 year survival. British Journal of Surgery 2004;91(5):605–9.
Setti Carraro P, Segala M, Cesana B, Tiberio G. Obstructing colonic cancer: failure and survival over a ten-year follow-up after one-stage curative surgery. Diseases of the Colon and Rectum 2001;44(2):243–50.
Runkel NS, Hinz U, Lehnert T, Buhr HJ, Herfarth Ch. Improved outcome after emergency surgery for cancer of the large intestine. British Journal of Surgery 1988;85(9):1260–5.
Mitry E, Barthod F, Penna C, Nordlinger B. Surgery for colon and rectal cancer. Best Pract Res Clin Gastroenterol 2002;16:253–65.
Pearce NW, Scott SD, Karran SJ. Timing and method of reversal of Hartmann’s procedure. Br J Surg 1992;79:839–41
Wong RW, Rappaport WD, Witzke DB, Putnam CW, Hunter GC. Factors influencing the safety of colostomy closure in the elderly. J Surg Res 1994;57:289–92.
Nugent KP, Daniels P, Stewart B, Patankar R, Johnson CD. Quality of life in stoma patients. Dis Colon Rectum 1999;42: 1569–74.
Sprangers MA, Taal BG, Aaronson NK, te Velde A. Quality of life in colorectal cancer. Stoma vs. nonstoma patients. Dis Colon Rectum 1995;38:361–9.
Londono-Schimmer EE, Leong AP, Phillips RK. Life table analysis of stomal complications following colostomy. Dis Colon Rectum 1994;37:916–20.
Park JJ, Del Pino A, Orsay CP, Nelson RL, Pearl RK, Cintron JR, et al. Stoma complications: the Cook County Hospital experience. Dis Colon Rectum 1999;42:1575–80.
Fielding LP, Stewart-Brown S, Blesovsky L. Large-bowel obstruction caused by cancer: a prospective study. BMJ 1979;2: 515–17.
Carson SN, Poticha SM, Shields TW. Carcinoma obstructing the left side of the colon. Arch Surg 1977;112: 523–26.
Scott NA, Jeacock J, Kingston RD. Risk factors in patients presenting as an emergency with colorectal cancer. British Journal of Surgery 1995;82(3):321–3.
Kulah B, Gulgez B, Ozmen M, Ozer M, Coskun F. Emergency bowel surgery in the elderly. Turkish Journal of Gastroenterology 2003;14(3):189–93.
Phillips RKS, Hittinger R, Fry Js, Fielding LP. Malignant large bowel obstruction. Br. J. Surg. 1985; 72: 296–302.
Deans GT, Krukowski ZH, Irwin ST. Malignant obstruction of the left colon Br. J. Surg. 1994; 81: 1270–1276.
Naraynsingh V, Rampaul R, Maharaj D, Kuruvilla T, Ramcharan K, Pouchet B. Prospective study of primary anastomosis without colonic lavage for patients with an obstructed left colon. Br. J. Surg. 1999; 86: 1341–1343.
Hsu TC. One-stage resection and anastomosis for acute obstruction of the left colon. Dis. Colon Rectum 1998; 42 : 28–32.
Mucci SH, Tuech JJ, Brehant O, Lermite E, Bergamaschi R, Pessaux P, Arnaud JP. Emergency subtotal/total colectomy in the management of obstructed left colon carcinoma. Int J Colorectal Dis 2006; 21: 538–541.
Hsu TC. Comparison of one stage resection and anastomosis of acute complete obstruction of left and right colon. Am. J. Surg 2005; 189: 384–387.
Lim JF, Tang CL, Seow-Choen F, Heah SM. Prospective, randomized trial comparing intraoperative colonic irrigation with manual decompression only for obstructed left-sided colorectal cancer. Dis Colon Rectum 2005; 48: 205–209.
The SCOTIA Study group. Single-stage treatment for malignant left-sided colonic obstruction: a prospective randomized clinical trial comparing subtotal colectomy with segmental resection following intra-operative irrigation. Br. J. Surg. 1995; 82: 1622–7.
Dohmoto M. New method: endoscopic implantation of rectal stent in palliative treatment of malignant stenosis. Endoscopia Digestiva 1991;3:1507–12.
Mainar A, Tejero E, Maynar M, Ferral H, Castaneda- Zuniga W. Colorectal obstruction: treatment with metallic stents. Radiology 1996;198:761–4.
Farrell JJ, Carr-Locke DC. Metal enteral stents: an endoscopist’s perspective. Seminars in Interventional Radiology 2001;18:327–37.
Baron TH, Dean PA, Yates MR 3rd, Canon C, Koehler RE. Expandable metal stents for the treatment of colonic obstruction: techniques and outcomes. Gastrointest Endosc 1998;47:277–86.
Mainar A, De Gregorio Ariza MA, Tejero E, Tobio R, Alfonso E, Pinto I, et al. Acute colorectal obstruction: treatment with self expandable metallic stents before scheduled surgery—results of a multicenter study. Radiology 1999;210:65–9.
Keymling M. Colorectal stenting. Endoscopy 2003;35:234–8.
Baron TH. Colorectal stents. Tech Gastrointestinal Endosc 2003; 5: 183–90
Tiemey W, Chuttani R, Croffie J, et al. Enteral stents. Gastrointestinal Endosc 2006; 63: 920–6
Baron TH. Minimizing endoscopic complications: endoluminal stents. Gastrointestinal Endosc Clin N Am 2007;17: 83–104.
Riedl S, Wiebelt H, Bergmann U, Hermanek P Jr. Post-operative komplikationen und letalitat in der chirurgishen Therapies des Coloncarcinoms. Cbirurg 1995; 66: 597–606.
Khot UP, Wenk Lang A, Muraliu K, Parker MC. Systematic review of the efficacy and safety of colorectal stents. Br J Surg 2002;89:1096–1102.
Arnaud J, Bergamaschi R. Emergency subtotal/total colectomy with anastomosis for acutely obstructed carcinoma of the left colon. Diseases of the Colon and Rectum 1994; 37(7): 685–8.
Halevy A, Levi J, Orda R. Emergency subtotal colectomy. A new trend for treatment of obstructing carcinoma of the left colon. Annals of Surgery 1989; 210(2):220–3.
Reemst P, Kulipers H, Wobbes T. Management of left-sided colonic obstruction by subtotal colectomy and ileocolic anastomosis. European Journal of Surgery 1998; 164(7): 537–40.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ghazal, AH.A., El-Shazly, W.G., Bessa, S.S. et al. Colonic Endolumenal Stenting Devices and Elective Surgery Versus Emergency Subtotal/Total Colectomy in the Management of Malignant Obstructed Left Colon Carcinoma. J Gastrointest Surg 17, 1123–1129 (2013). https://doi.org/10.1007/s11605-013-2152-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-013-2152-2