Abstract
Purpose
This study aims to evaluate the role of colonic stenting as a bridge to surgery in acutely obstructed left-sided colon cancer.
Methods
Patients with acute left-sided malignant colonic obstruction with no evidence of peritonitis were recruited. After informed consent, patients were randomized to colonic stenting followed by elective surgery or immediate emergency surgery. Patients who had successful colonic stenting underwent elective surgery 1 to 2 weeks later, while the other group had emergency surgery. Patients in whom stenting was unsuccessful also underwent emergency surgery.
Results
Twenty patients were randomized to stenting and 19 to emergency surgery. Fourteen patients (70%) had successful stenting and underwent elective surgery at a median of 10 days later; the rest underwent emergency surgery. Technical stent failure occurred in five patients (25%). One patient failed to decompress after successful stent deployment. All patients underwent definitive colonic resection with primary anastomosis. Two of 20 patients in the stenting group required defunctioning stomas compared to 6 of 19 in emergency surgery group, p = 0.127. Overall complication rate was 35% versus 58% (p = 0.152) and mortality was 0% versus 16% (p = 0.106) in the stenting group and emergency surgery group, respectively. Postoperatively, the stenting group was discharged from hospital earlier (median of 6 versus 8 days, p = 0.028) than the emergency surgery group.
Conclusion
Colonic stenting followed by interval elective surgery may be safer, with a trend towards lower morbidity and mortality when compared with the current practice of emergency surgery for left-sided malignant colonic obstruction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer is the most common cancer in men and the second most common in women in Singapore [1]. About 7% to 29% of colorectal cancers presents as acute intestinal obstruction [2]. Intestinal obstruction is a surgical emergency that requires surgery to relieve the obstruction as soon as possible.
However, emergency surgery for obstructing lesion is associated with high mortality rate of between 10% and 30% compared to <5% for elective surgery for colorectal cancer [3, 4]. This includes increased anesthetic risk because of inadequate time to optimize patients before operation. Emergency surgery is associated with a higher requirement for critical care as well as with a prolonged hospital stay. Surgery on unprepared bowel also results in need for on-table decompression or washout and possible defunctioning stoma formation. This would result in the patient requiring another surgery for stoma closure in the future. In addition, acutely obstructed patients are more likely to require a subtotal colectomy [4] and may result in poorer bowel function in the future.
Stage for stage, patients treated by emergency resection should have similar long-term survival compared to the elective setting after they recovered from the operation. However, patients with obstructed colorectal cancer operated in the emergency setting often have their adjuvant chemotherapy delayed or omitted because of postoperative complications or prolonged recovery process, resulting in compromised oncologic therapy and outcome.
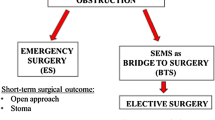
Self-expanding metallic stents (SEMS) have been used for palliative treatment of obstructed advanced unresectable colorectal cancer. Recently, there have been reports of colonic stents to relieve colonic obstruction temporarily, followed by elective definitive resection of the tumor at a later date, with the stents used as a “bridge to surgery” [5, 6]. This brings about the benefit of operating on an elective basis, on a properly assessed patient with prepared bowel, and possibly lower perioperative complications and improved survival. While the use of SEMS are becoming popular, no randomized study has been published to clarify whether stenting as a bridge to surgery represent a safe and effective option to emergency surgical resection for the treatment of malignant colorectal obstruction.
We proposed to conduct a prospective randomized controlled trial comparing endoscopic stenting for relief of obstruction followed by elective colectomy versus emergency colectomy for patients with acute colonic obstruction secondary to left-sided colorectal cancer.
Material and methods
Eligibility for enrollment
Patients who presented to our institution with acute intestinal obstruction secondary to left-sided colonic cancer were offered participation in the trial. Left-sided colonic cancer was defined as that distal to and including the splenic flexure of the colon up to and including the rectosigmoid colon. Patients with distal rectal cancers <8 cm from the anal verge were excluded. Diagnosis of acute colonic obstruction was made clinically, based on symptoms of vomiting, abdominal distension, abdominal pain, and inability to pass stools, and confirmed radiologically on plain abdominal films demonstrating dilated colon. The diagnosis of the colonic tumor causing the obstruction and the site of tumor was confirmed by flexible sigmoidoscopy or computer tomography scan of the abdomen and pelvis. Patients with signs of peritonitis suggestive of bowel perforation or sepsis demanding urgent surgery were excluded. Obstruction due to noncolonic malignancy was excluded. The trial was approved by our hospital’s institutional review board.
Randomization
After written informed consent was obtained, eligible patients were randomly assigned to one of two groups by consecutive opening of sequentially numbered, opaque, sealed envelopes. Envelope randomization was performed by a computer-generated code. Patients were randomized to emergency endoscopic colonic stenting, followed by elective surgery at a later date or to emergency surgery (current standard treatment). Patients who had successful stenting were discharged and readmitted for elective surgery. Patients in whom stenting was unsuccessful underwent emergency surgery. The choice of surgery performed was up to the individual consultant colorectal surgeon.
SEMS placement procedure
Gentle flexible sigmoidoscopy after a rectal enema was performed to confirm the diagnosis of left-sided colonic cancer. The stenosing lesion was stented by a combined endoscopic and fluoroscopic approach performed by or supervised by a consultant colorectal surgeon. Using a double-channel therapeutic endoscope, a guide wire was introduced across the stenosis and beyond the obstruction; subsequently, water-soluble contrast was injected via a catheter over the guide wire to confirm the intraluminal placement of the guide wire as well as to assess the length of the stenosis. The SEMS was inserted through the endoscope over the guide wire and deployed in place. We use either the 22 × 90- or 25 × 90-mm stents (WallFlex® colonic stent; Boston Scientific, Natick, MA, USA) for our procedures. Correct positioning of the stent was confirmed using both fluoroscopy and endoscopy. Stenting procedures were all carried out with conscious sedation. We did not perform balloon predilatation because this was reported to be associated with a higher incidence of perforation [7]. Technical success was defined as successful SEMS placement and deployment. Clinical success was defined as the colonic decompression within 96 h after successful placement of the stent, with passage of stools and resolution of nausea and vomiting, and confirmed on plain abdominal radiograph.
Surgical procedure
Patients who had successful stenting and decompression were discharged and readmitted for elective surgery. Elective surgery should preferably take place about 1 to 2 weeks after stenting. Standard preoperative bowel preparation, prophylactic low-molecular-weight heparin, and intravenous antibiotics were administrated as per usual in elective surgery. Patients randomized to emergency surgery and patients who failed stenting underwent surgery as soon as the operating theaters were available after initial stabilization. In both elective and emergency cases, tumor resection followed standard oncologic principles. Surgical options at the discretion of the individual consultant colorectal surgeon included resection and primary anastomosis, Hartmann’s procedure, subtotal or total colectomy, diverting stoma formation, and laparoscopic colectomy.
Objectives and hypothesis
The objective of this study was to evaluate the role of colonic SEMS placement as a bridge to surgery in patients with acute malignant left-sided colonic obstruction. The study was designed to test the hypothesis that SEMS placement could be effectively and safely used in this group of patients to relieve colonic obstruction thereby allowing safe recovery and medical stabilization before proceeding to elective surgery.
Statistical analysis
The primary endpoint was 60 days postoperative complication rates. Postoperative complication was defined as any event leading to hospital readmission or prolonging current hospital stay. Secondary outcomes evaluated included type of surgery performed, bowel preservation, presence of a stoma, postoperative bowel function, length of hospital stay, length of stay in critical care, and hospitalization costs. Based on the results of previous studies [5, 6, 8], this study was designed to have 80% power to detect a 40% difference in complication rates between the stenting group and emergency surgery group, with a two-sided alpha error of 5%. A sample size of 20 patients in each group was required.
Data on patient demographics, stenting details, operative details, histopathological details, postoperative recovery, complications, and outcome, as well as financial costs were entered into a statistical software package (SPSS version 16.0, Chicago, IL, USA) and analyzed using the Mann–Whitney U test for continuous variables and the chi-squared test or Fisher’s exact test for categorical variables. Two-sided statistical significance was accepted at the 5% level.
Financial cost analysis
Cost-effectiveness was examined by comparing the health care costs generated for endoscopic stenting with elective surgery versus costs for emergency surgery. Only direct health care costs were considered. Costs of hospital admission, readmissions for complications, and readmissions for closures of stomas included inpatient hospitalization costs, costs of critical care, endoscopy costs, costs of stents, operation costs, and surgical expendables costs. Hospitalization costs were calculated according to the “private” rates before government public hospital subsidies in Singapore dollars (S$ 1.00, approximately US$ 0.65), obtained from information from the hospital’s finance department.
Results
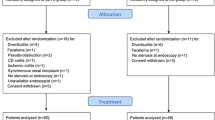
Between October 2004 and February 2008, a total of 40 patients admitted with acute left-sided malignant colonic obstruction were recruited. After written informed consent, 21 were randomized to the stenting group and 19 were randomized to the emergency surgery group. One patient who was randomized to the stenting group developed signs and symptoms of peritonitis before his stenting procedure and required immediate surgery and, therefore, was excluded from the trial. There were no significant difference in the age, sex, and distribution of the site of the tumor between the two groups (see Table 1).
Stenting outcome
Placement of SEMS took a median time of 35 min (range, 20–80 min). Fourteen patients out of 20 (70%) had successful stenting and bowel decompression. They resumed soft diet after a median of 2 days (range, 1–4 days) and were discharged a median of 4 days (range, 2–6 days) later. They returned for elective surgery at a median of 10 days (range, 9–38 days) after stenting. Six out of 20 patients failed stenting, of which technical failure occurred in 5 patients (25%). The main cause was the inability to pass the guide wire across the stenotic cancer (in four cases). In the fifth patient, we were unable to visualize the tumor lumen at all as it was behind a tight bend and hence unable to pass the guide wire across. The sixth patient had a stent successfully placed and deployed across the tumor but failed to decompress and required emergency surgery; this patient was considered to have clinical failure. There were no instances of inability to deploy the stent or stent-related problems after deployment. There were also no instances of guide wire or stent perforation in this study. Hence, 14 patients who had successful endoscopic stenting underwent elective surgery, while 6 patients who failed stenting underwent emergency surgery. The results were analyzed on an intention-to-treat basis. See the trial flow diagram in Fig. 1.
Operative details
All patients underwent definitive resection of the colonic tumor with primary anastomosis (Table 2). Among the 20 patients randomized to the stenting group, 12 had open surgery and 8 underwent elective laparoscopic colectomies, 3 of which were converted to open. All 19 patients who were randomized to the emergency surgery group had open surgery.
The length of incision was shorter in the stenting group compared to the emergency surgery group (15 versus 20 cm, p = 0.003). Patients who had successful stenting were able to have full bowel preparation before elective surgery, whereas 4 patients in the stenting group (who failed stenting) and 12 patients in the emergency surgery group required on-table bowel decompression. Two of the 20 patients in the stenting group required a defunctioning stoma compared to 6 out of 19 patients in the emergency surgery group, but this was not statistically significant. One stoma in the stenting group and two in the emergency surgery group were not closed at 1 year post-operation because of progressive disease. Tumor-specific segmental resection was possible in 18 patients (90%) in the stenting group compared to only 12 (63%) in the emergency surgery group, with the rest undergoing subtotal colectomy (see Table 2).
Postoperative recovery, complications, and outcome
There were no mortality in the stenting group; on the other hand, there were three mortalities (16%) in the emergency surgery group, but this was not statistically significant. The overall complication rate in the stenting group compared to the emergency surgery group was 35% versus 58%, respectively, but this was not statistically significant (see Table 3). One patient in the stenting group developed intra-abdominal abscess requiring intravenous antibiotics therapy and full thickness wound dehiscence requiring operative repair. Another patient in the stenting group developed a leak from small bowel anastomosis requiring relaparotomy. In the emergency surgery group, two patients required reoperation: one patient developed acute left femoral embolism requiring operative embolectomy, one patient developed massive bleeding from right-sided diverticulosis requiring total colectomy and end ileostomy.
Bowel function returned after a median of 4 days in the stenting group compared to 5 days after emergency surgery, but this was not statistically significant. Patients were fit for discharge earlier in the stenting group at a median of 6 days (range, 4–28 days) postoperatively than in the emergency surgery group, 8 days (range, 6–39 days), p = 0.028. Median postoperative bowel frequency per day was similar in both groups.
Length of hospital stay and financial cost
The total length of hospital stay (including stoma closure for two-stage operative procedure) and the length of stay in critical care were similar for the two groups. The cost of treatment between the two groups was also similar (see Table 4).
Subgroup analyses
Subgroup analysis comparing the group who failed stenting requiring immediate surgery with the group randomized to emergency surgery from the outset showed no differences in terms of patients’ age, tumor location, tumor stage, stoma rate, and postoperative complication rate (see Table 5). The group of 14 patients who had successful stenting followed by elective surgery had statistically significantly better outcomes compared with the group randomized to emergency surgery in a subgroup analysis in terms of higher tumor-specific segmental resection rate, lower stoma rate, lower postoperative complication rate, earlier return of bowel function, and shorter length of stay in critical care (see Table 6).
Discussion
Malignant left-sided colonic obstruction is a difficult clinical problem and requires urgent surgical treatment. The options for surgery include proximal diversion only, primary resection without anastomosis, and primary resection with primary anastomosis with or without defunctioning stoma. In our institution, we adopt an aggressive approach for patients with left-sided colonic obstruction, striving to achieve primary resection and primary anastomosis [8–10]. However, depending on the hemodynamic stability of the patient and concomitant medical conditions, one-stage resection and anastomosis may not be possible and defunctioning stoma formation after anastomosis may often be necessary. The associated morbidity and mortality of this group of patients were well known [3, 11].
SEMS were initially attempted in patients with incurable disease. Recently, stents became popular as a “bridge to surgery” in patients with obstructed but resectable colorectal cancer. Martinez-Santos et al. [5] showed that SEMS placement before elective surgery was associated with a higher incidence of primary anastomosis, fewer complications, a shorter hospital stay, and a shorter stay in the intensive care unit than emergency surgical resection.
In the present trial, clinical success was achieved in 14 out of 20 patients (70%) that were randomized to stenting. In this subgroup of patients, colonic decompression by stenting allowed time for correction of dehydration and electrolyte imbalance and institution of nutritional therapy. In fact, the patients recovered so well that they were fit for discharge at a median of 4 days post-stenting.
In this study, our technical success rate in the placement of the stent was 75%, which was lower than some published reports. In a pooled analysis by Sebastian et al. [12] of 1,198 patients from 54 heterogeneous cohort studies, the reported technical success rates in individual series varied from 64% to 100%. This lower technical success rate might due to the fact that all patients recruited in this trial were in complete clinical obstruction, rather than in case series, which included partially obstructing tumors and palliative stenting where there was still a clear lumen channel. All five cases of our technical stent failures were due to the inability to find the lumen for passage of the guide wire. And this was also noted in the pooled analysis that the technical success in the bridge to surgery group was slightly lower at 91.9% compared to the overall technical success rate of 94%. In the same analysis, failure rate on attempted placement of the rectosigmoid stents was 5.8%, while the failure rates for descending colon and more proximal colon stent placement were higher at 14.5% and 15.4%, respectively.
We did not experience any perforation or other complications related to stent placement in this trial. Avoidance of excessive manipulation of the guide wire and too much air insufflation was important. We also did not practice balloon predilatation, as it was significantly associated with perforation [7]. The average reported rate of perforation caused by the guide wire or stent was about 4% [12]. Risk of stent migration or need for reintervention to maintain patency was not a problem in this current trial setting because the stent was required to remain in the colon for a short period of time till elective surgery.
This trial found that stenting as a bridge to surgery showed a possible trend towards reduction in postoperative complication rates compared to emergency surgery. There were no mortality in the stenting group; on the other hand, there were 16% mortality in the emergency surgery group, although it was not statistically significant. It might be attributed to the time window created after successful stenting to allow emergency surgery to be deferred, permitting adequate assessment of patient, preparation, and optimization of patient’s condition before definitive surgery. In contrast with the usual stormy postoperative course we were familiar with in the emergency surgery group, patients in the successfully stented subgroup seemed to sail through surgery rather uneventfully.
There was earlier hospital discharge post-surgery in the stenting group, although the total length of hospital stay was similar between the two groups. The costs between the two groups were similar in this randomized trial, although a study in UK estimated that the cost reduction was 12% [13], and was more impressive at 28.8% in a study conducted in Switzerland by Binkert et al. [14]. We would still consider stenting as a bridge to surgery cost-effective in this study because, for similar costs, stent placement may result in improved clinical outcome including fewer complications despite the high individual cost of the stents.
In the subgroup of patients who had successful stenting, we found that elective surgery was straightforward. Preoperative bowel preparation was possible, enabling easily mobilization of the colon and avoided the need for on-table decompression during resection. The use of left iliac fossa skin crease incision was also possible during elective surgery for open resection in this subgroup, in contrast to the use of standard long midline incision for the emergency surgery group. Skin crease incisions were associated with less postoperative pain and faster recovery in a previous study at our institution [15]. The median interval to surgery after stenting was 10 days. We felt that the optimal interval to proceed with elective surgery was between 9 and 14 days post-stenting, when there was usually only mild peritumor inflammation and adhesions due to the presence of the stent in situ [16]. In our experience, increased likelihood of dense fibrotic adhesions might be encountered after 14 days, which might increase difficulty during surgery. Towards the later part in the conduct of this trial, we also found that laparoscopic colectomy may be feasible in this subgroup of patients, although we accepted that our conversion rate was high at three out of eight cases. Conversions were due to dense adhesions from peritumor inflammation with stent in situ. We recommended early conversion if dense adhesions were encountered. The incision wound for tumor extraction was required to be 1 to 2 cm longer than usual to accommodate the delivery of the often-bulky tumor with the stent in situ. Nonetheless, the fact that laparoscopic surgery was potentially feasible in obstructed colorectal cancer after stenting was very satisfying and encouraging [17].
Result from this randomized trial adds to accumulated data including the findings from three recent large systematic reviews [7, 12, 18] that colonic stent placement as a bridge to surgery may be safe and effective and may be associated with lower mortality and morbidity.
Our sample size calculation was based on our initial successful experience in colonic stenting as well as results from previous published studies with the technical success rate of stent placement at 90% to 95% [5, 12]. Our somewhat lower technical success rate in stent placement in this trial may have lessened the overall difference between the two groups and, therefore, the trial failed to reach statistical significance. Nevertheless, the results still showed a trend towards lower complication rates for the stenting group. Subgroup analysis showed that the group of patients who had failed stenting did not fare worse than the group randomized initially to emergency surgery. This may be due to the fact that we did not encounter any complications related to the stenting procedure and that the attempted stenting procedure did not result in significant delays in arrangement for emergency surgery for patients in whom stenting failed. We accept that this may not always be the case, and stent-related complications will affect the overall effectiveness of choosing stenting for patient with obstructed left-sided colon cancer.
Conclusion
Colonic stenting for acute left-sided malignant colonic obstruction can be safely attempted. After successful stenting, when possible, interval elective surgery may be safer, with less morbidity and mortality when compared with the current practice of emergency surgery. The stoma rate tended to be lower, and the requirement for critical care may be shorter in comparison with emergency surgery.
References
National Registry of Diseases Office (2008) Singapore Cancer Registry interim report—trends in cancer incidence in Singapore 2002–2006. National Registry of Diseases Office, Singapore
Deans GT, Krukowski ZH, Irwin ST (1994) Malignant obstruction of the left colon. Br J Surg 81(9):1270–1276
Smith JJ, Cornish J, Tekkis P, Thompson MR (2007) The National Bowel Cancer Audit Project 2007: quality improvement and open reporting. Association of Coloproctology of Great Britain and Ireland, London
Hennekinne-Mucci S, Tuech JJ, Brehant O, Lermite E, Bergamaschi R, Pessaux P, Arnaud JP (2006) Emergency subtotal/total colectomy in the management of obstructed left colon carcinoma. Int J Colorectal Dis 21(6):538–541. doi:10.1007/s00384-005-0048-7
Martinez-Santos C, Lobato RF, Fradejas JM, Pinto I, Ortega-Deballon P, Moreno-Azcoita M (2002) Self-expandable stent before elective surgery vs. emergency surgery for the treatment of malignant colorectal obstructions: comparison of primary anastomosis and morbidity rates. Dis Colon Rectum 45(3):401–406
Saida Y, Sumiyama Y, Nagao J, Uramatsu M (2003) Long-term prognosis of preoperative “bridge to surgery” expandable metallic stent insertion for obstructive colorectal cancer: comparison with emergency operation. Dis Colon Rectum 46(10 Suppl):S44–S49
Khot UP, Lang AW, Murali K, Parker MC (2002) Systematic review of the efficacy and safety of colorectal stents. Br J Surg 89(9):1096–1102
Lim JF, Tang CL, Seow-Choen F, Heah SM (2005) Prospective, randomized trial comparing intraoperative colonic irrigation with manual decompression only for obstructed left-sided colorectal cancer. Dis Colon Rectum 48(2):205–209
Nyam DC, Leong AF, Ho YH, Seow-Choen F (1996) Comparison between segmental left and extended right colectomies for obstructing left-sided colonic carcinomas. Dis Colon Rectum 39(9):1000–1003
Nyam DC, Seow-Choen F, Leong AF, Ho YH (1996) Colonic decompression without on-table irrigation for obstructing left-sided colorectal tumours. Br J Surg 83(6):786–787
Poon RT, Law WL, Chu KW, Wong J (1998) Emergency resection and primary anastomosis for left-sided obstructing colorectal carcinoma in the elderly. Br J Surg 85(11):1539–1542
Sebastian S, Johnston S, Geoghegan T, Torreggiani W, Buckley M (2004) Pooled analysis of the efficacy and safety of self-expanding metal stenting in malignant colorectal obstruction. Am J Gastroenterol 99(10):2051–2057
Osman HS, Rashid HI, Sathananthan N, Parker MC (2000) The cost effectiveness of self-expanding metal stents in the management of malignant left-sided large bowel obstruction. Colorectal Dis 2(4):233–237
Binkert CA, Ledermann H, Jost R, Saurenmann P, Decurtins M, Zollikofer CL (1998) Acute colonic obstruction: clinical aspects and cost-effectiveness of preoperative and palliative treatment with self-expanding metallic stents—a preliminary report. Radiology 206(1):199–204
Kam MH, Seow-Choen F, Peng XH, Eu KW, Tang CL, Heah SM, Ooi BS (2004) Minilaparotomy left iliac fossa skin crease incision vs. midline incision for left-sided colorectal cancer. Tech Coloproctol 8(2):85–88
Bethge N, Sommer A, Gross U, von Kleist D, Vakil N (1996) Human tissue responses to metal stents implanted in vivo for the palliation of malignant stenoses. Gastrointest Endosc 43(6):596–602
Chung TS, Lim SB, Sohn DK, Hong CW, Han KS, Choi HS, Jeong SY (2008) Feasibility of single-stage laparoscopic resection after placement of a self-expandable metallic stent for obstructive left colorectal cancer. World J Surg 32(10):2275–2280
Watt AM, Faragher IG, Griffin TT, Rieger NA, Maddern GJ (2007) Self-expanding metallic stents for relieving malignant colorectal obstruction: a systematic review. Ann Surg 246(1):24–30
Author information
Authors and Affiliations
Corresponding author
Additional information
Category of paper
Randomized controlled trial.
Rights and permissions
About this article
Cite this article
Ho, KS., Quah, HM., Lim, JF. et al. Endoscopic stenting and elective surgery versus emergency surgery for left-sided malignant colonic obstruction: a prospective randomized trial. Int J Colorectal Dis 27, 355–362 (2012). https://doi.org/10.1007/s00384-011-1331-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-011-1331-4