Abstract
Purpose
No consensus exists on the optimal treatment of acute malignant right-sided colonic obstruction (RSCO). This systematic review aims to compare procedure-related mortality and morbidity rates between primary resection and stent placement as a bridge to surgery followed by elective resection for patients with acute RSCO.
Methods
PubMed, Embase and Cochrane library were searched for all relevant literature. Primary endpoints were procedure-related mortality and morbidity. Methodological quality of the included studies was assessed using the MINORS criteria.
Results
Fourteen cohort studies were eligible for analysis. A total of 2873 patients were included in the acute resection group and 155 patients in the stent group. Mean mortality rate for patients who underwent acute resection with primary anastomosis was 10.8 % (8.1–18.5 %). Overall mortality for patients initially treated with a colonic stent followed with elective resection was 0 %. Major morbidity was 23.9 % (9.3–35.6 %) and 0.8 % (0–4.8 %), respectively. Both mortality and major morbidity were significantly different. In addition, stent placement shows lower rates of anastomotic leakages (0 vs 9.1 %) and fewer permanent ileostomies (0 vs 1.0 %).
Conclusion
Primary resection for patients with acute RSCO seems to be associated with higher mortality and major morbidity rates than stent placement and elective resection. In addition, stent placement resulted in fewer anastomotic leakages and permanent ileostomies. However, as no high-level studies are available on the optimal treatment of RSCO and proximal stenting is considered technically challenging, future comparative studies are warranted for the development of an evidence-based clinical decision guideline.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Approximately 15 % of patients with colon cancer present with colonic obstruction as a first symptom [1]. This potentially life-threatening condition generally requires emergency intervention, and 32.5–54 % of emergency surgeries for colonic obstruction are performed for tumours located in the proximal colon [2, 3]. Traditionally, malignant obstruction of the right colon has been treated with resection and primary anastomosis, which was deemed safe after prospective data showed no difference in mortality between emergency and elective surgery for right colonic obstruction [4]. However, recent studies found significantly higher operative risks for emergency resection compared to elective surgery [5, 6].
Indeed, patients presenting with right-sided colonic obstruction (RSCO) are generally older and have a more advanced tumour stage than electively treated patients [3]. Added to this poor general condition, patients commonly have a distended bowel and often a period of reduced intake and weight loss, which likely will lead to high mortality and morbidity rates following emergency surgery. This prompted the search for valid alternatives for these frail patients, in whom the benefits of surgery might not outweigh the risks. Colonic stents can be used to address the immediate problem of a colonic obstruction and yet allow time for careful preparation for an extensive operation, thus serving as a ‘bridge to surgery’. This time can be used to optimise the patient’s condition and allows for better staging of cancer, which could prevent unnecessary operations in inoperable patients [6]. However, only limited data are available regarding stent placement in the proximal colon. Likewise, a staged approach with initial creation of a deviating ileostomy followed by elective tumour resection could theoretically be of benefit for patients who are in poor preoperative condition at the time of presentation. This approach is not uncommon for left-sided colon obstruction but very rarely used for right-sided obstructions.
Through a systematic review of available literature, this study aims to provide an overview of procedure-related mortality and morbidity rates of both primary resection and bridge to surgery with a colonic stent followed by elective resection in patients with acute malignant RSCO and to identify possible preoperative risk factors associated with worse outcomes after emergency intervention.
Methods
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [7]. Inclusion criteria for article selection were all studies containing information on treatment for acute right-sided colon obstruction.
Search strategy
A systematic search was performed in MEDLINE (PubMed), EMBASE (Ovid) and the Cochrane Database of Systematic Reviews. The search was restricted to publications in English and Dutch. Studies involving animal experiments were also excluded. The final search was performed on March 26, 2015. The search strategy for PubMed included colon obstruction[tiab] OR colonic obstruction[tiab] OR obstructed colon[tiab] OR malignant obstruction[tiab] OR proximal obstruction[tiab] OR right sided obstruction[tiab] OR colonic ileus[tiab] AND (surgery[tiab] OR colectomy[tiab] OR hemicolectomy[tiab] OR resection[tiab] OR colostomy[tiab] OR ostomy[tiab] OR stoma[tiab] OR stent[tiab] OR stents[tiab]). In addition, EMBASE and Cochrane databases were searched for relevant literature using the same search terms for domain and determinant. The reference lists of included articles were screened to identify additional studies.
Study selection and quality assessment
Two reviewers (FA and HB) independently selected all relevant studies based on title and abstract. Studies were included when the location of obstruction was proximal, when the intervention was performed in an emergency setting and when data on post-intervention morbidity and/or mortality were provided. Conference abstracts without subsequent publication were excluded. In addition, studies in which outcome measures were not reported specifically for proximal obstruction or emergency intervention, <10 patients included, <80 % of the colonic obstruction caused by colon cancer or studies with a solely palliative approach were excluded from analysis. Both reviewers read the full text of the remaining articles. Final inclusion was based on consensus. All included studies were critically and independently appraised by both reviewers, using the MINORS criteria [8]. Studies containing the following variables were included: age, gender, location of the obstruction, morbidity and mortality. For stent studies, technical success, defined as deployment of the stent in the planned location, and clinical success, defined as decompression leading to relief of symptoms, were also mandatory variables.
Data extraction
Two reviewers (FA and HB) extracted all data from the original articles. Baseline characteristics including age, gender, American Society of Anesthesiologists (ASA) score and location of the obstruction were obtained from included studies, as well as procedure-related mortality and morbidity. Mortality was defined as death within 30 days of the intervention or death within 3 months of the intervention without having been discharged from the hospital. Morbidity was subdivided in major and minor morbidity according to the Clavien-Dindo classification of surgical complications [9]. Minor morbidity was defined as grade IIIa or lower, major as grade IIIb or higher.
Statistical analysis
Continuous variables were described as mean with range. Categorical variables were described as counts and percentages. Fisher’s exact test was used for data analysis where necessary.
Results
Study selection, study characteristics and methodological quality
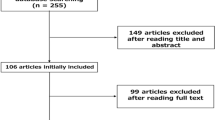
In total, 1384 studies were identified by the search, and after removal of duplicates, 1038 remained. All articles were screened for eligibility based on title and abstract, leading to exclusion of 1372 studies. The remaining 18 studies were analysed in detail. Full-text investigation led to exclusion of an additional eight studies. Five were excluded because they did not report outcomes for treatment of proximal obstruction specifically. Two were excluded because the number of patients with right-sided obstruction was very small (<10 patients). One study was excluded because it included the same patients as another study; the excluded study had the smallest number of patients. Eventually, ten studies were included. Cross-reference searching yielded another four articles relevant for this review. In total, 14 studies were included in this systematic review [3, 5, 10–21] (Fig. 1).
Included articles were published between 2001 and 2013 and reported outcomes on a total of 2992 patients. Outcomes for primary resection were reported in ten articles (2837 patients) and for stent placement in four (155 patients). No studies reporting on deviating ileostomy creation as a treatment option were identified. All included studies are non-comparative cohort studies; ten describe retrospective data and the other four have a prospective design. The mean MINORS criteria score was 8.8 (range 6 to 11) out of a maximum possible score of 16 (Table 1). Since no comparative studies were included, a meta-analysis of the data was not possible.
Details on demographics and patient characteristics are shown in Tables 2 and 3. For patients undergoing primary resection (n = 2873), mean age was 63.1 years (59–75), 48.8 % were male and 40.2 % were ASA class III–IV. One hundred fifty-five patients underwent stent placement; mean age was 68.4 years (66.2–73), and 58.7 % were male. Unfortunately, ASA classification and tumour stage were not reported for patients undergoing stent placement. Of the 155 patients in the stent group, 95 patients had the stent placed as a bridge to surgery; in 60 patients, stent placement was as a palliative approach (Fig. 2). All 95 patients, who received stent placement as a bridge to surgery, eventually underwent elective resection. Reasons for a palliative approach were the presence of metastatic disease in three studies [10, 21], poor preoperative condition or metastatic disease in one [18], and not stated in one study [13].
Mortality
All 14 studies reported on mortality rates (Tables 4 and 5) [3, 5, 10–21]. Mean overall mortality was 10.8 % (8.1–18.5 %) in the primary resection group (n = 2873) and 0 % in the stent group (n = 155). This difference was found to be statistically significant (p = 0.009).
Morbidity
Morbidity rates were reported in 11 out of 14 included studies [3, 10–15, 17–19, 21]. Mean overall complication rate was 63.0 % (22.2–77.8 %) for the primary resection group (n = 841) and 12.3 % (3.8–24.0 %) for the stent group (n = 155). This difference was not statistically significant (p = 0.079), although borderline.
Morbidity rates could be classified further into major or minor morbidity in 8 of 14 studies [11, 14, 15, 17–19, 21], reporting on 535 patients in the primary resection group and 108 in the stent group. Minor morbidity, grade IIIa or lower, was not significantly different for the primary resection group 26.5 % (16.3–51.2 %) compared with the stent group 3.4 % (0–7.1 %) (p = 0.77). Major morbidity, grade IIIb or higher, was 23.9 % (9.3–35.6 %) for the resection group, which is significantly higher than a 0.8 % (0–4.8 %) major morbidity rate for the stent group (p = 0.049).
The occurrence of anastomotic leakage was reported in four studies and was 9.1 % (4.3–16.4 %) following primary resection (n = 465) and 0 % for those patients in the stent group who subsequently underwent elective resection (n = 95) [11, 14–16]. All cases of stenting as a bridge to surgery to an operation were clinically successful. Median time from stent to operation was 19 days (range 7–42). No major surgical complications occurred, and none required temporary stoma formation. Three out of 95 patients (3.4 %) had minor morbidity after elective resection [11, 14–16].
Six studies reported on the creation of a protective ileostomy following primary resection [11, 14–17, 19]. In total, 38 patients (7.6 %, 0–23.2 %) were treated with an ileostomy; ultimately, four patients (1.0 %, 0–1.9 %) ended up with a permanent ileostomy. No permanent ileostomies were created in the stent group.
Specific outcomes for the stent group are shown in Table 5. Technical success was achieved in 95.5 % (86.0–100 %) of patients, and mean clinical success rate was 89.0 % (78.0–96.3 %). Stent-related perforation occurred in 1.3 % (0–5 %), stent migration in 2.0 % (0–8.0 %) and stent re-occlusion in 3.2 % (0–11.0 %) of patients.
In addition to mortality and morbidity, we tried to identify preoperative risk factors for mortality. However, due to the lack of reporting on the different variables such as age, ASA score and tumour location in the included studies, specific analysis was not possible.
Discussion
This systematic review was performed to provide an overview of the current literature on outcome of acute malignant right-sided colonic obstruction. To our knowledge, this is the first systematic review regarding treatment options specifically for acute malignant RSCO. The results suggest that a bridge to surgery approach using stent placement with subsequent elective resection is accompanied by significantly lower mortality and major morbidity when compared with primary resection (p = 0.009 and p = 0.049, respectively). In addition, a tendency to a lower percentage of anastomotic leakage (0.0 %) and permanent ileostomy creation (0.0 %) in the patients treated with stent is demonstrated when compared to primary resection (9.1 and 1.0 %, respectively).
Primary resection and anastomosis are the current treatment of choice for acute RSCO, and the great majority (94.8 %) of patients included in this review received this treatment. The overall mortality of around 10 % seems to be an improvement compared to 21 % seen in older studies [22] and might be due to advances in critical care, antibiotic use and CT-guided abscess drainage. Nevertheless, mortality after emergency resection is much higher than after elective resection, which confirms that emergency right hemicolectomy is a high-risk procedure [2, 3, 5]. This stresses the need for alternative treatment strategies leading to bowel decompression and preventing perforation before definitive treatment of the obstructing tumour.
Stenting as a bridge to surgery has been proposed as an attractive alternative to primary resection [23]. In this review, clinical success of stent placement, with decompression of the colon and relief of symptoms, was achieved in 89.0 % (78.0–96.3 %), and perforation was found in 1.3 % (0–5 %) of patients. These observations are similar to those found in retrospective studies of stenting for left-sided colonic obstructions [23–25]. However, prospective studies have shown clinical success rates of only 40.0–71.7 % and perforation rates as high as 19–34 % in left-sided obstruction [26–28]. The discrepancy between retrospective and prospective data has been attributed to selection bias. Attempts for stent placement were generally not undertaken in patients with total obstructions in retrospective studies, because complete obstruction makes deployment technically difficult and increases the risk of perforations [29]. Perforation is a feared complication, since it is associated with higher risks of mortality due to abscess formation. Additionally, there are concerns about tumour spread and worsened long-term survival after perforation [27]. Most studies reporting on stent placement are performed in left-sided obstructions, and less than 4 % of the reported cases involve stent placement in the proximal colon [30]. It is important to realize that stent placement in the right side of the colon is technically challenging [13, 31, 32].
Despite the usual technical difficulty of proximal stent placement, technical and clinical success rates in all included retrospective studies are as high as 95.5 and 89.0 %, respectively. We tried to examine whether this might be due to patient selection. In the stent group, 55.2 % had a subtotal obstruction, making stent placement easier. However, no data are available on the number of (sub)total obstructions in the acute resection group, making it impossible to determine whether patient selection occurred. In addition, we identified by whom the stents were placed, since experience has been shown to be important and determines technical and clinical success in stent placement [25]. Only Dronamraju et al. and Repici et al. reported on this, and in these two studies, the stents were placed by a single endoscopist or gastroenterologist in each institution. How many stents they placed annually or their initial experience with stents was not stated [10, 18]. In 50 % of the patients, a WALLSTENT was used, 40.5 % received a Hanaro stent and 9.5 % a Bona stent. The diameter of these stents ranged from 20 to 24 mm and the length from 6 to 16 cm. Whether these different stent designs or measures influenced the outcomes is unknown. Finally, tumour location did differ between the acute resection group and the stent group, i.e. 39.5 % had the tumour located at the hepatic flexure in the acute resection group versus 7.7 % in the stent group. However, tumour location is not a known risk factor for complications in colonic stent placement [25].
We tried to identify risk factors associated with a higher mortality and morbidity following surgery. Identification of these risk factors might help in clinical decision-making. However, the reported data were too inconsistent to allow for analysis. The individual findings in some of the included studies showed increasing mortality and morbidity with increasing age [3, 11, 20]. However, in all studies except for the study by Aslar et al., these ratios were calculated for left-sided and right-sided resections in elective and emergency settings combined. Kobayashi et al. found an odds ratio of 3.99 (2.209–7.208) for patients with ASA class IV + V and an odds ratio of 2.317 (1.564–3.431) for patients with ASA class III in a cohort of 15,275 patients who underwent emergency or elective right hemicolectomy [5]. In addition, multiple other studies, both retrospective and prospective, associated ASA class III or higher with increased risks of mortality and/or major morbidity [3, 11, 19, 20, 33]. Advanced age and ASA class III or higher are therefore likely to be independent risk factors for mortality, and those patients may have most benefit from other treatment alternatives.
An important question currently is whether stent placement might have a negative influence on the oncologic long-term results, due to tumour manipulation and/or micro-perforations. None of the included studies report on long-term outcomes. For left-sided colonic obstructions, stent placement is currently only recommended in palliative patients or as a bridge to surgery when the patient is deemed unfit for major surgery since no consensus has been reached on the influence of stent placement on survival and recurrence rates [34, 35].
A systematic review such as this has several limitations that should be taken into account. First, due to lack of high-level evidence on acute RSCO, none of the included studies were comparative or blinded, and most included studies were retrospective, increasing the risk of possible bias and confounding. Furthermore, in only one out of the four studies reporting on stent placement, more than half of the included patients received stent as a bridge to surgery. Second, morbidity appeared to have been assessed differently in the various studies included in this study. Therefore, all complications were scored according to the surgical complication classification according to Clavien and Dindo [9]. Although this classification is validated, it remains liable to subjective bias. Finally, the included studies did not all report on the different outcome measures, resulting in varying numbers of group sizes for the different outcomes.
To our knowledge, this is the first systematic review reporting on alternative treatment options for right-sided colonic obstructions. Taking into consideration that literature reporting on this subject is scarce, this systematic review shows that stent placement seems to lead to significantly lower mortality and major morbidity rates when compared to primary resection. In addition, a lower percentage of patients with anastomotic leakage and a permanent ileostomy after eventual resection were seen when first treated with stent placement. Furthermore, stent placement can also be used as a palliative modality and could prevent unnecessary large abdominal surgery when further oncologic staging shows inoperable disease. The favourable results reported after stenting as a bridge to surgery are an indication that this could be a viable alternative for primary acute resection. However, the concerns over technical and clinical success, stent-related complications and long-term oncologic outcomes should be taken into account. Therefore, stent placement as a bridge to surgery could be a viable alternative for acute resection in curable patients with a high operative risk. In addition, it should only be applied when executed by a skilled and experienced endoscopist. Keeping the limitations of this study in mind, it is time for a prospective, comparative study between primary resection and stenting for malignant RSCO which will aid future clinical decision-making and may offer a suitable treatment for the individual patient.
References
Phillips RK, Hittinger R, Fry JS, Fielding LP (1985) Malignant large bowel obstruction. Br J Surg 72:296–302
McArdle CS, Hole DJ (2004) Emergency presentation of colorectal cancer is associated with poor 5-year survival. Br J Surg 91:605–609
Sjo OH, Larsen S, Lunde OC, Nesbakken A (2009) Short term outcome after emergency and elective surgery for colon cancer. Color Dis 11:733–739
Smithers BM, Theile DE, Cohen JR, Evans EB, Davis NC (1986) Emergency right hemicolectomy in colon carcinoma: a prospective study. Aust N Z J Surg 56:749–752
Kobayashi H, Miyata H, Gotoh M, Baba H, Kimura W, Kitagawa Y, et al. (2013) Risk model for right hemicolectomy based on 19,070 Japanese patients in the National Clinical Database. J Gastroenterol. epub
Smothers L, Hynan L, Fleming J, Turnage R, Simmang C, Anthony T (2003) Emergency surgery for colon carcinoma. Dis Colon Rectum 46:24–30
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62(10):1006–1012
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196
Dronamraju SS, Ramamurthy S, Kellu SB, Hayat M (2009) Role of Self-Expanding Metallic Stents in the Management of Malignant Obstruction of the Proximal Colon. Dis Colon Rectum 52:1657–1661
Aslar AK, Özdemir S, Mahmoudi H, Kuzu MA (2011) Analysis of 230 cases of emergent surgery for obstructing colon cancer – lessons learned. J Gastrointest Surg 15:110–119
Chin CC, Wang JY, Changchien CR, Huang WS, Tang R (2010) Carcinoma obstruction fo the proximal colon cancer and long-term prognosis – obstruction is a predictor of worse outcome in TNM stage II tumor. Int J Color Dis 25:817–822
Cho YK, Kim SW, Lee BI, Lee KM, Lim DH, Kim JS et al (2011) Clinical outcome of self-expandable metal stent placement in the management of malignant proximal colon obstruction. Gut Liver 5:165–170
Frago R, Biondo S, Millan M, Kreisler E, Golda T, Fraccalvieri D (2011) Differences between proximal and distal obstructing colonic cancer after curative surgery. Color Dis 13:e116–e122
Hsu TC (2005) Comparison of one-stage resection and anastomosis of acute complete obstruction of left and right colon. Am J Surg 189:384–387
Lee YM, Law WL, Chu KW, Poon RT (2001) Emergency surgery for obstructing colorectal cancers: a comparison between right-sided and left-sided lesions. J Am Coll Surg 192:719–725
Ng SS, Lee JF, Yiu RY, Li JC, Leung WW, Leung KL (2008) Emergency laparoscopic-assisted versus open right hemicolectomy for obstructing right-sided colonic carcinoma: a comparative study of short-term clinical outcomes. World J Surg 32:454–458
Repici A, Adler DG, Gibbs CM, Malesci A, Preatoni P, Baron TH (2007) Stenting of the proximal colon in patients with malignant large bowel obstruction: techniques and outcomes. Gastrointest Endosc 66(5):940–944
Tan KK, Sim R (2010) Surgery for obstructed colorectal malignancy in an Asian population: predictors of morbidity and comparison between left- and right-sided cancers. J Gastrointest Surg 14:295
Tekkis PP, Kinsman R, Thompson MR, Stamatakis JD (2004) The association of coloproctology of Great Britain and Ireland Study of large bowel obstruction caused by colorectal cancer. Ann Surg 240:76–81
Yao LQ, Zhong YS, Xu MD, Xu JM, Zhou PH, Cai XL (2011) Self-expanding metallic stents drainage for acute proximal colon obstruction. World J Gastroenterol 17:3342–3346
Miller FB, Nikolov NR, Garrison RN (1987) Emergency right colon resection. Arch Surg 122(3):339–343
Tilney HS, Lovegrove RE, Purkayastha S, Sains PS, Weston-Petrides GK, Darzi AW et al (2007) Comparison of colonic stenting and open surgery for malignant large bowel obstruction. Surg Endosc 21(2):225–233
Watt AM, Faragher IG, Griffin TT, Rieger NA, Maddern GJ (2007) Self-expanding metallic stents for relieving malignant colorectal obstruction: a systematic review. Ann Surg 246(1):24–30
Small AJ, Coelho-Prabhu N, Baron TH (2010) Endoscopic placement of self-expandable metal stents for malignant colonic obstruction: long-term outcomes and complication factors. Gastrointest Endosc 71(3):560–572
Sebastian S, Johnston S, Geoghegan T, Torreggiani W, Buckley M (2004) Pooled analysis of the effi cacy and safety of self-expanding metal stenting in malignant colorectal obstruction. Am J Gastroenterol 99:2051–2057
Pirlet IA, Slim K, Kwiatkowski F, Michot F, Millat BL (2011) Emergency preoperative stenting versus surgery for acute left-sided malignant colonic obstruction: a multicenter randomized controlled trial. Surg Endosc 25(6):1814–1821
van Hooft JE, Bemelman WA, Oldenburg B, Marinelli AW, Holzik MF, Grubben MJ, Sprangers MA, Dijkgraaf MG, Fockens P (2011) collaborative Dutch Stent-In study group. Colonic stenting versus emergency surgery for acute left-sided malignant colonic obstruction: a multicentre randomised trial. Lancet Oncol 12(4):344–352
Ansaloni L, Andersson RE, Bazzoli F, Catena F, Cennamo V, Di Saverio S et al (2010) Guidelines in the management of obstructing cancer of the left colon: consensus conference of the world society of emergency surgery (WSES) and peritoneum and surgery (PnS) society. World J Emerg Surg 28(5):29
Khot UP, Lang AW, Murali K, Parker MC (2002) Systematic review if the efficacy and safety of colorectal stents. Br J Surg 89:1096–1102
Bonin EA, Baron TH (2010) Update on the Indications and Use of Colonic Stents. Curr Gastroenterol Rep 12(5):374–382
Keymling M (2003) Colorectal stenting. Endoscopy 35(3):234–238
Tan KK, Liu JZ, Yeow Y, Gunasekaran S, Tan JJ (2011) Is emergency right hemicolectomy still associated with significant morbidity and mortality rates? An institution’s experience of 207 cases over 6 years. Int J Color Dis 26:1157–1161
van Hooft JE, van Halsema EE, Vanbiervliet G, Beets-Tan RG, DeWitt JM, Donnellan F, Dumonceau JM, Glynne-Jones RG, Hassan C, Jiménez-Perez J, Meisner S, Muthusamy VR, Parker MC, Regimbeau JM, Sabbagh C, Sagar J, Tanis PJ, Vandervoort J, Webster GJ, Manes G, Barthet MA, Repici A (2014) Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Gastrointest Endosc 80(5):747–761. doi:10.1016/j.gie.2014.09.018, e1-75
Erichsen R, Horváth-Puhó E, Jacobsen JB, Nilsson T, Baron JA, Sørensen HT (2015) Long-term mortality and recurrence after colorectal cancer surgery with preoperative stenting: a Danish nationwide cohort study. Endoscopy
Conflict of interest
F.J. Amelung, H.W.L. de Beaufort, P.D. Siersema, P.M. Verheijen and E.C.J. Consten have no conflicts of interests or financial ties to disclose.
Sources of funding for research and/or publication
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Amelung, F.J., de Beaufort, H.W.L., Siersema, P.D. et al. Emergency resection versus bridge to surgery with stenting in patients with acute right-sided colonic obstruction: a systematic review focusing on mortality and morbidity rates. Int J Colorectal Dis 30, 1147–1155 (2015). https://doi.org/10.1007/s00384-015-2216-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-015-2216-8