Abstract
Introduction
Intramedullary locking devices (ILDs) have recently been advocated as a minimally invasive approach to manage displaced intraarticular calcaneal fractures (DIACFs), to minimise complications and improve outcomes. We reviewed clinical and biomechanical studies dealing with commercially available devices to identify their characteristics, efficacy and safety.
Methods
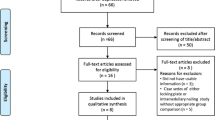
Following a PRISMA checklist, Medline, Scopus and EMBASE databases were searched to identify studies reporting the use of ILDs for treating DIACFs. Biomechanical studies were first evaluated. Cohort studies were then reviewed for demographics, surgical technique, postoperative protocol, clinical and radiographic scores, complications and reoperations. The modified Coleman Methodology Score (CMS) was used to assess the quality of studies.
Results
Eleven studies were identified which investigated two devices (Calcanail®, C-Nail®). Three biomechanical studies proved they offered adequate primary stability, stiffness, interfragmentary motion and load to failure. Eight clinical studies (321 feet, 308 patients) demonstrated a positive clinical and radiographic outcome at 16-months average follow-up. Metalware irritation (up to 20%) and temporary nerve entrapment symptoms (up to 30%) were the most common complications, while soft tissue issues (wound necrosis, delayed healing, infection) were reported in 3–5% of cases. Conversion to subtalar fusion was necessary in up to 6% of cases. Four (50%) out of 8 studies were authored by implant designers and in 5 (62%) relevant conflicts of interest were disclosed. Mean (± standard deviation) CMS was 59 ± 9.8, indicating moderate quality.
Conclusions
Treating DIAFCs with ILDs leads to satisfactory clinical outcomes at short-term follow-up, enabling restoration of calcaneal height and improved subtalar joint congruency. Metalware irritation and temporary nerve entrapment symptoms are common complications although wound complications are less frequent than after open lateral approaches. The quality of evidence provided so far is moderate and potentially biased by the conflict of interest, raising concerns about the generalisability of results.
Level of evidence
Level V – Review of Level III to V studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Calcaneal fractures are the most frequent tarsal bony injury and account for 1% to 4% of all adult fractures [1, 2]. Intra-articular extension is present in 60% to 80% of cases with joint incongruity associated with functional impairment [1, 2]. Adequate restoration of the articular surface can lead to satisfactory long-term clinical results [3,4,5,6] and surgical goals are thus focused on re-establishing the height and length of the calcaneus and reconstructing the posterior articular facet in particular [7]. The best treatment of the displaced intraarticular calcaneal fracture (DIACF) is still debated [1, 8,9,10]. Lateral approaches are associated with complications including hematoma, skin necrosis, soft tissue infection, and osteitis in up to 35% of cases [5, 11,12,13,14,15]. This has generated interest in percutaneous reduction and fixation techniques [16,17,18,19], which may reduce these risks.
Gussenbauer reported the use of an intramedullary nail to fix calcaneal fractures as early as 1888 although no outcomes are available for review [20]. No published reports exist concerning intramedullary locking devices (ILDs) until 2012 when Goldzak et al. described their technique for treating DIACFs [21]. There have subsequently been a few studies showing encouraging results of ILDs for DIACFs which theoretically combine the advantages of minimally invasive surgery with stable fixation [22,23,24,25,26,27,28,29,30,31].
With this background, we performed a systematic review of the literature to identify the current level of evidence supporting the adoption of calcaneal ILDs in the treatment of DIACFs. Our aims were (i) to report the biomechanical background for ILDs and (ii) to investigate the efficacy and safety of ILDs through the analysis of clinical studies published in modern literature.
Methods
This systematic review was designed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The project was prospectively registered with the PROSPERO database of systematic reviews (CRD42019147815).
Eligibility criteria
We included studies reporting the use of ILD for treating DIACF designed as biomechanical study (in-vitro study) and prospective or retrospective clinical study (randomised clinical trials, controlled clinical trials, observational cohort prospective and retrospective studies, case series) in English, French, Spanish, German and Italian. We excluded studies reporting redundant data with previous publications and case reports.
Data sources and search
A comprehensive electronic search of the current literature was performed using Medline, Scopus and EMBASE databases, from the earliest records through November 06, 2020. Additional studies were identified by checking the bibliographies of the articles selected. Reviews were excluded. If full texts were not available, authors were contacted. Using Boolean operators, the following search terms were used: calcane* AND fractur* AND fixat* AND nail*.
Study selection
Results were managed using Endnote. Duplicates and studies without abstracts were excluded. Titles and abstracts were screened by two authors (AB and MA) at different places and times. After applying exclusion criteria, eligible studies were selected. Disagreements were solved through discussion and consensus.
Studies were categorised into two groups: 1) biomechanical studies and 2) clinical studies. Studies in the first group were critically analysed. From studies in the second group, data were extracted regarding conflict of interest, study design (and the Level of Evidence), demographics (sample size, sex, age), surgical procedure (mean time between injury and surgery, type of device, technique, fracture classification, postoperative protocol) follow-up, clinical and radiographic scores, patient satisfaction, intraoperative and postoperative complications, reoperations, and time to return to work and sport activities. All values for the aforementioned variables were reported as per the primary authors’ description. Whenever an outcome was reported at more than one point in time during follow-up, values of the last recorded follow-up were used.
Quality assessment
The modified Coleman methodological score (CMS) was used, ranging from 0 to 100 [32]. Two investigators performed the CMS assessment twice (AB and YG), with an interval of 10 days, then discussed the scores when a difference of more than two points was present until consensus was reached. A score higher than 85 was considered excellent, good from 70 to 84, moderate from 50 to 69 and poor when less than 50, as previously reported in foot and ankle literature [33].
Summary measures and synthesis of results
Summarised data are presented as mean value ± standard deviation, ranges and frequency. All analyses were performed using STATA statistical software package (Version 14.0, StataCorp, 2015). A critical analysis was provided for each outcome even if a systematic pooling of data (weighted means) was not possible, therefore, a formal meta-analysis was not performed due to the lack of data in primary studies.
Results
Biomechanical studies
Three biomechanical studies about ILD were retrieved for this review [27,28,29] (Fig. 1). They were all published in the English language.
Goldzak et al. compared the Calcanail® (FH Orthopedics, Heimsbrunn, France) against an angular stable AO locking plate (Synthes Inc., Paoli, PA 19301-1222, USA) in artificially generated Sanders type IIB fractures on 7 pairs of corroded (dry) human calcaneal and talar bones. The first breakage under compressive load occurred under similar forces for both nail and plate constructs, although nail-fixed specimens exhibited threefold higher stiffness (190 N/mm vs. 60 N/mm) and significantly higher load to failure (350 N vs. 280 N) [27]. Although the authors concluded that intramedullary nails offered superior primary stability and that this may reduce the risk of secondary displacement during weight bearing [27], the limitations included the use of dry bones that did not tolerate the load applicable to frozen bones [27].
Reinhardt et al. subsequently compared three devices: Calcanail®, C-Nail® (Medin, Nov. Město n. Moravě, Czech Republic) and a polyaxial locking plate (Rimbus®; Intercus GmbH; Rudolstadt, Germany) in artificially reproduced Sanders type IIB fractures in 21 fresh-frozen cadavers [29]. Load to failure was greatest with C-Nail® (2800 N) than Rimbus® plate (2000 N) than Calcanail® (1740 N) although the difference was not statistically significant. Conversely, stiffness was significantly greater for Calcanail® (600 N/mm) than locking plate (530 N/mm) and C-Nail® (500 N/mm). In that study, changes in Bohler’s angle after failure in any testing sequence was lower for Calcanail® than C-Nail® and Rimbus plate (3.6° vs 8° vs 15°, respectively). Interfragmentary motion and specifically motion of subtalar joint fragment were not dissimilar for the three implants whilst both nails allowed more movement of the anterior process of the calcaneus, as would be expected considering their design.
Ni et al. compared a Calcanail® fixed in a standard manner, locking plate fixed with 3.5 mm screws (Synthes, Solothurn, Switzerland) and a modified Calcanail® technique that adds a 3.5 mm lag screw entering postero-anterior to the anterior process through the channel in the middle of the nail thereby transfixing it [28]. Finite element analysis was performed on a model mimicking a Sanders type IIIAB fracture in a simulated single stance which was then validated in a cadaveric model. The modified Calcanail® technique provided more stiffness than the standard technique or locking plate (552 N/mm vs. 522 N/mm vs. 454 N/mm respectively). The additional lag screw reduced micromotion between fracture fragments which increased fracture stability (0.07 mm vs. 0.1 mm vs. 0.09 mm respectively) with stress forces better distributed which was theorised to reduce the risk of hardware failure [28].
Clinical studies
Characteristics of studies
Eight clinical studies involving 321 feet (308 patients) were included in the analysis (Fig. 1), of which six (75%) investigated the Calcanail® implant [22,23,24, 26, 30, 31] and two investigated the C-Nail® [25, 34]. Four (50%) out of 8 were authored by implant designers and in 5 (62%) relevant conflicts of interest were disclosed. All studies were published in the English language or with an English translation included. Six out of 8 were level IV studies [22,23,24,25,26, 30] whilst two were level III [31, 34]. Five of 8 (62%) were prospective studies [22, 25, 26, 30, 31]. The mean cohort size was 40 ± 25 feet (range 17 to 103) with a mean age of 48.2 ± 5.6 years (range 21 to 90) that were followed-up to a mean 15.7 ± 5.5 months (range 11 to 33) (Table 1). The mean CMS of all studies was only 59 ± 9.8 (range 47 to 77) with most studies having methodological limitations, and only 2 (25%) showing good methodological quality [25, 30] (Table 2).
Indications and technique
The indication for ILD was DIACF with loss of subtalar joint congruency on plain radiographs or CT scans in all studies [21, 23,24,25,26, 30, 31, 34,35,36].
All studies reporting outcomes of the Calcanail® [22,23,24, 26, 30, 31] broadly adopted the basic surgical technique described by Goldzak et al. [21], although in 3 (50%) studies the prone position was preferred over the lateral decubitus position [23, 24, 31]. All authors reduced the depressed posterior facet articular surface through a combination of talocalcaneal distraction (which restored height) and the insertion of specialised bone tamps that elevated the calcaneal side of the joint. Fixation was performed by introducing of the ILD via the same channel created through the posterior tuberosity and two locking screws. Two studies documented augmentation by additional lag screws [24, 31] and sinus tarsi approach in some cases [31].
The two studies reporting clinical outcomes of the C-Nail® [25, 34] reproduced the technique described in the literature [37]. Reduction was achieved through a sinus tarsi approach and the implant was introduced from the posterior tuberosity and locked by means of 5 or 6 screws.
Postoperative protocol
Variability existed in post-operative casting and mobilisation protocols. Most surgeons advised partial weight bearing for 6 to 10 weeks after surgery [23,24,25,26, 30] (Table 3). In 2 (28%) studies, 3 weeks of cast immobilisation was recommended [23, 30], whereas other authors (42%) suggested early physiotherapy to prevent stiffness [24,25,26]. In 2 (28%) studies, non-weight bearing was suggested for 3 weeks, followed by partial bearing for other 3 weeks [23, 30], whilst in 2 (28%) studies postoperative instructions were unclear [22, 31].
Clinical outcome
The American Orthopaedic Foot and Ankle Society score for ankle and hindfoot (AOFAS-AHS) was the most common clinical outcome measure (used in 7 (87%) studies [22, 23, 25, 26, 30, 31, 34]), followed by the visual analogue scale for pain (VAS) in 3 (37%) studies [26, 30, 31]. At latest follow-up, AOFAS-AHS (on 239 feet) averaged 82.7 ± 47.1 points (range 61 to 100) and VAS (on 63 feet) averaged 3 ± 0.5 points (range 0 to 9). A mean postoperative stay in hospital of 9.6 days was documented in 3 (37%) studies [24, 31, 34]. Other questionnaires used in single studies are depicted in Table 3.
Radiographic outcome
Böhler angle was the most common measurement to assess reduction, being documented in 7 studies (87%) [21, 23, 25, 26, 30, 31, 34,35,36]. Other radiographic parameters were Gissane angle (reported in 2 (28%) studies [30, 31]), Goldzak index or calcaneal height index (in 3 (42%) [22, 23, 30]) and posterior facet step off (in 2 (28%) [25, 31]) (Table 4).
Pre and postoperative radiographs showed the mean Böhler angle improved from 4° ± 4 (range -50 to 28) to 29° ± 2.7 (range 22 to 50) and mean Gissane angle from 117° ± 7 (range 80 to 151) to 104° ± 5.6 (range 85 to 133). Computerised tomography (CT) revealed the Goldzak index increased from 0.5 ± 0.1 (range 0.1 to 0.8) preoperatively to 0.8 ± 0.1 (range 0.4 to 1.1) postoperatively whilst the posterior facet step off reduced from 3.6 mm ± 2.3 (range 0 to 6) preoperatively to 0.8 mm ± 0.2 (range 0 to 3) postoperatively (Table 4).
Of note, a combined assessment of reduction based on both radiographs and CTs (rated as excellent if Sanders type A or B and Böhler angle > 20°, good if type D or E and Böhler angle > 20° and poor if type C or Böhler angle < 20°) was reported in 2 (28%) studies [22, 30], where good or excellent reduction was achieved in 75% [22] and 81% [30], respectively (Table 4).
Failure and complications
Complication rates ranged between 5 and 30% [21, 23,24,25,26, 30, 31, 34,35,36] (Table 5), with metalware irritation reported in 0–20% of cases and leading (in all cases) to implant removal. Conversion to fusion was necessary in 4–6% (except for one study where it was never required [34]), generally at 11 to 24 months from surgery (Table 5). Soft tissue complications (wound necrosis, delayed healing and infection) were reported in 3–5% of feet [25, 30, 31] and nerve entrapment symptoms (up to 30% of cases) were generally self-resolving [22, 31]. Two cases of complex regional pain syndrome (CRPS) were documented in 2 studies [23, 30] (Table 5).
Discussion
The ideal treatment for DIACF is still a matter of debate with no single method being suitable for all types of fractures and a patient-centered approach is advocated by authors [9, 10]. Indeed the choice of operative or non-operative management continues to be controversial amongst foot and ankle surgeons and divides opinion [38, 39]. Some authors have recommended operative management for DIACFs, reporting better results albeit with a higher complication rate [3,4,5,6, 8, 13, 40, 41]. Conversely, the UKHeFT study reported that surgery did not improve outcomes at two-year follow-up (in closed injuries) [38]. Interestingly this UK-based randomised trial did not influence the practice of surgeons in the UK with the percentage of calcaneal fractures treated operatively remaining constant at 7% [42]. There was however an increase in minimally invasive techniques although this is probably part of a wider trend [42].
Direct visualisation of the lateral calcaneal wall and fracture has been regarded as the standard surgical method for DIACFs since it facilitates anatomical reduction of the fracture and restoration of Bohler’s angle. Despite advancements in surgical fixation devices such as locking plates, risks remain including wound infection, haematoma, sural nerve injury, failure of fixation [43,44,45,46] and need for revision surgery in up to 35% of patients [5, 11, 13, 47,48,49,50].
It is with this in mind that devices that rely upon minimally invasive techniques have been developed. Whilst both commercially available ILDs provide on-axis fixation, they differ in the means by which fracture reduction is achieved. The C-Nail® implant cannot be used as a fracture reduction tool and anatomical fracture reduction has to be achieved with dedicated screws through a mini-lateral incision prior to nail insertion [24]. This, together with the horizontal positioning of the nail and the use of more than 3 multidirectional locking screws (as compared to the oblique position with 2 parallel locking screws for Calcanail®) constitute significant differences that should be taken into account by surgeons before using these devices. In contrast, the Calcanail® utilises an intra-focal reduction technique of the articular surface [21]. The possibility to restore and maintain the correct articular height to convert to arthrodesis in case of the severely damaged posterior facet is another relevant advantage of this approach [21, 24].
From the biomechanical standpoint, both commercially available ILDs achieve satisfactory primary stability in absolute values and when compared to locking plates [27, 29]. ILDs have successfully been used to allow partial weight bearing at an average of 3 weeks although it is not known if this confers any long-term benefit, and AOFAS-AHS and VAS scores are similar to more ‘traditional’ surgery at short term follow-up [38, 51]. From the radiographic viewpoint, surgery utilising ILDs restore Bohler angle close to reference values (between 22° and 50°) [21, 23, 25, 26, 30, 31, 35, 36], comparing well with values obtained after extensile lateral approach (between 24° and 31°) [51]. Despite less invasive approaches, residual step-off of the posterior facet is reported as low as 0.8 – 1 mm (measured on CT scans), although this has only been assessed in two studies [25, 31]. Of note, only 2 studies reported the Gissane angle, which according to the recent literature may widely vary according to ethnicity and lead to misinterpretation of imaging [52].
Thus, whilst it can be considered that fracture reduction, fixation and patient-reported outcome scores are comparable with more extensile surgery, the question arises of whether complications are lower? This review established the complication rate of ILDs between 6 and 30% [22, 24,25,26,27, 31, 32, 35, 36] with metalware irritation (including implant protrusion on the plantar aspect of the foot and lateral prominence of locking screw head causing either skin or peroneal tendon irritation) nerve entrapment symptoms (usually self-limiting) reported up to 20% and 30% of cases, respectively. Whilst 4% to 6% of patients underwent subtalar arthrodesis at approximately 1-year follow-up, it cannot be identified whether this is due to surgery or to cartilage damage related to the original injury and whether this rate will increase in the long term (Table 5). The overall rate of complications relating to soft tissues was lower than traditional operative techniques (3–5% vs. 12–35% respectively), which may be a result of the reduced stress on tissues achieved by minimally invasive technique [51] (Table 5). This would also be in accordance with the encouraging mid- to long-term results reported for other minimally-invasive approaches to the calcaneus such as the sinus tarsi one, which seems related to a very low risk of wound and neuropathic complications with clinical results not inferior to the extensile lateral approach [19, 53].
The methodology of the studies analysed in this review was overall only of moderate quality, mainly due to the small sample size, short follow-up, poor assessment of the outcome and lack of subgroup analysis in cohorts of patients presenting with a different pattern of injury. Furthermore, the majority of studies were co-authored by the respective implant designers, which raises concern about whether other surgeons may be able to reliably reproduce the reported outcomes. Small sample sizes, short follow-up and low levels of evidence are other relevant factors to consider when interpreting results. Some studies are retrospective and only one prospective comparative study (Level III) [31] is available. Out of 6 studies on Calcanail®, two authors report the use of additional screws [24, 31], which while provide further mechanical stability [28] also increase the heterogeneity of the studies. For these reasons, according to the ABCI system (where A represents good evidence, B fair evidence, C conflicting or poor-quality evidence and I insufficient evidence) [54], ILDs for DIACFs should be assigned a grade C recommendation. We encourage further comparative studies to verify the hypothesis that using ILDs in a minimally invasive approach leads to stable fracture fixation and better clinical outcomes in the mid and long term.
We acknowledge the limitations of this study. The sample size is relatively small and no formal meta-analysis was performed. In this analysis, we were able to provide only average values rather than weighted means, which would have enabled us to obtain more powerful results. It would also have been useful to consider the surgical time and the experience of the surgeon [15] as variables influencing the outcome after ILDs, but this was not doable either due to the paucity and quality of studies available in the literature. Furthermore, sub-group assessment of outcomes based on fracture classification was not possible to perform. Although most authors used the Sanders classification to describe fractures in their cohort, sufficient follow-up data relevant to each type was not provided. It is our belief that the complexity of the initial injury affects the outcome and future work should establish if ILD are better indicated in some fractures type more than others. Finally, as overmentioned, the amount of implant designers as authors might have skewed the results of primary studies and subsequently of our review. This being said, we believe that the opportunity to raise awareness about this type of bias among studies dealing with ILDs for DIACFs is a further merit of this study.
Conclusion
Using ILDs to treat DIACFs can lead to encouraging short-term clinical and radiological outcomes. Complications include metalware irritation and temporary nerve entrapment symptoms although wound complications are less common than after traditional more invasive techniques. Published results on ILDs scores only moderate for quality of evidence and this is potentially biased by the conflict of interest by implant designers. Grade C recommendation in favour of ILDs can be established, therefore further adequately powered comparative studies with long-term follow-up is advocated.
References
Epstein N, Chandran S, Chou L (2012) Current concepts review: intra-articular fractures of the calcaneus. Foot Ankle Int 33:79–86. https://doi.org/10.3113/FAI.2012.0079
Wei N, Zhou Y, Chang W, Zhang Y, Chen W (2017) Displaced intra-articular calcaneal fractures: classification and treatment. Orthopedics 40:e921–e929. https://doi.org/10.3928/01477447-20170907-02
Potter MQ, Nunley JA (2009) Long-term functional outcomes after operative treatment for intra-articular fractures of the calcaneus. J Bone Jt Surg Am 91:1854–1860. https://doi.org/10.2106/JBJS.H.01475
Makki D, Alnajjar HM, Walkay S, Ramkumar U, Watson AJ, Allen PW (2010) Osteosynthesis of displaced intra-articular fractures of the calcaneum: a long-term review of 47 cases. J Bone Joint Surg Br 92:693–700. https://doi.org/10.1302/0301-620X.92B5.23542
Rammelt S, Zwipp H, Schneiders W, Dürr C (2013) Severity of injury predicts subsequent function in surgically treated displaced intraarticular calcaneal fractures. Clin Orthop Relat Res 471:2885–2898. https://doi.org/10.1007/s11999-013-3062-z
Sanders R, Vaupel ZM, Erdogan M, Downes K (2014) Operative treatment of displaced intraarticular calcaneal fractures. J Orthop Trauma 28:551–563. https://doi.org/10.1097/BOT.0000000000000169
Thermann H, Krettek C, Huffner T, Schratt H-E, Albrecht K, Tscherne H (1998) Management of calcaneal fractures in adults. Clin Orthop Relat Res 353:107–124. https://doi.org/10.1097/00003086-199808000-00013
Thordarson DB, Krieger LE (1996) Operative vs. nonoperative treatment of intra-articular. Fractures of the calcaneus: a prospective randomized trial. Foot Ankle Int 17:2–9. https://doi.org/10.1177/107110079601700102
Sanders R (2000) Displaced intra-articular fractures of the calcaneus. J Bone Jt Surg Am 82:225–250. https://doi.org/10.2106/00004623-200002000-00009
Rammelt S (2014) An update on the treatment of calcaneal fractures. J Orthop Trauma 28:549–550. https://doi.org/10.1097/BOT.0000000000000227
Abidi NA, Dhawan S, Gruen GS, Vogt MT, Conti SF (1998) Wound-healing risk factors after open reduction and internal fixation of calcaneal fractures. Foot Ankle Int 19:856–861. https://doi.org/10.1177/107110079801901211
Folk JW, Starr AJ, Early JS (1999) Early wound complications of operative treatment of calcaneus fractures: analysis of 190 fractures. J Orthop Trauma 13:369–372
Buckley R, Tough S, Mccormack R, Pate G, Leighton R, Petrie D et al (2002) Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures. J Bone Jt Surg Am 84:1733–1744. https://doi.org/10.2106/00004623-200210000-00001
Howard JL, Buckley R, McCormack R, Pate G, Leighton R, Petrie D et al (2003) Complications following management of displaced intra-articular calcaneal fractures: a prospective randomized trial comparing open reduction internal fixation with nonoperative management. J Orthop Trauma 17:241–249
Fischer S, Meinert M, Neun O, Colcuc C, Gramlich Y, Hoffmann R et al (2020) Surgical experience as a decisive factor for the outcome of calcaneal fractures using locking compression plate: results of 3 years. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03649-3
Stulik J, Stehlik J, Rysavy M, Wozniak A (2006) Minimally-invasive treatment of intra-articular fractures of the calcaneum. J Bone Joint Surg Br 88:1634–1641. https://doi.org/10.1302/0301-620X.88B12.17379
Weber M, Lehmann O, Sägesser D, Krause F (2008) Limited open reduction and internal fixation of displaced intra-articular fractures of the calcaneum. J Bone Joint Surg Br 90:1608–1616. https://doi.org/10.1302/0301-620X.90B12.20638
Nosewicz T, Knupp M, Barg A, Maas M, Bolliger L, Goslings JC et al (2012) Mini-open sinus tarsi approach with percutaneous screw fixation of displaced calcaneal fractures: a prospective computed tomograph-based study. Foot Ankle Int 33:925–933. https://doi.org/10.3113/FAI.2012.0925
Richter I, Krähenbühl N, Ruiz R, Susdorf R, Horn Lang T, Hintermann B (2020) Mid- to long-term outcome in patients treated with a mini-open sinus-tarsi approach for calcaneal fractures. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03530-3
Gussenbauer C (1888) Ueber die Behandlung der Rissfracturen des Fersenbeines. Prag Med Wochenschr 13:161–162
Goldzak M, Mittlmeier T, Simon P (2012) Locked nailing for the treatment of displaced articular fractures of the calcaneus: description of a new procedure with calcanail®. Eur J Orthop Surg Traumatol 22:345–349. https://doi.org/10.1007/s00590-012-0968-1
Simon P, Goldzak M, Eschler A, Mittlmeier T (2015) Reduction and internal fixation of displaced intra-articular calcaneal fractures with a locking nail: a prospective study of sixty nine cases. Int Orthop 39:2061–2067. https://doi.org/10.1007/s00264-015-2816-5
Fascione F, Di Mauro M, Guelfi M, Malagelada F, Pantalone A, Salini V (2018) Surgical treatment of displaced intraarticular calcaneal fractures by a minimally invasive technique using a locking nail: a preliminary study. Foot Ankle Surg. https://doi.org/10.1016/j.fas.2018.08.004
Saß M, Rotter R, Mittlmeier T (2019) Minimally invasive internal fixation of calcaneal fractures or subtalar joint arthrodesis using the Calcanail®. Oper Orthop Traumatol 31:149–164. https://doi.org/10.1007/s00064-018-0576-2
Zwipp H, Paša L, Žilka L, Amlang M, Rammelt S, Pompach M (2016) Introduction of a new locking nail for treatment of intraarticular calcaneal fractures. J Orthop Trauma 30:e88-92. https://doi.org/10.1097/BOT.0000000000000482
Falis M, Pyszel K (2016) Treatment of displaced intra-articular calcaneal fractures by intramedullary nail: preliminary report. Ortop Traumatol Rehabil 18:141–147. https://doi.org/10.5604/15093492.1205021
Goldzak M, Simon P, Mittlmeier T, Chaussemier M, Chiergatti R (2014) Primary stability of an intramedullary calcaneal nail and an angular stable calcaneal plate in a biomechanical testing model of intraarticular calcaneal fracture. Injury 45:S49-53. https://doi.org/10.1016/j.injury.2013.10.031
Ni M, Wong DW-C, Niu W, Wang Y, Mei J, Zhang M (2019) Biomechanical comparison of modified Calcanail system with plating fixation in intra-articular calcaneal fracture: a finite element analysis. Med Eng Phys. https://doi.org/10.1016/j.medengphy.2019.06.004
Reinhardt S, Martin H, Ulmar B, Döbele S, Zwipp H, Rammelt S et al (2016) Interlocking nailing versus interlocking plating in intra-articular calcaneal fractures. Foot Ankle Int 37:891–897. https://doi.org/10.1177/1071100716643586
Fourgeaux A, Estens J, Fabre T, Laffenetre O, Lucasy Hernandez J (2019) Three-dimensional computed tomography analysis and functional results of calcaneal fractures treated by an intramedullary nail. Int Orthop. https://doi.org/10.1007/s00264-019-04381-3
Herlyn A, Brakelmann A, Herlyn PK, Gradl G, Mittlmeier T (2019) Calcaneal fracture fixation using a new interlocking nail reduces complications compared to standard locking plates-preliminary results after 1.6 years. Injury. https://doi.org/10.1016/j.injury.2019.07.015
Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD (2000) Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports 10:2–11
Bernasconi A, Sadile F, Smeraglia F, Mehdi N, Laborde J, Lintz F (2017) Tendoscopy of Achilles, peroneal and tibialis posterior tendons: an evidence-based update. Foot Ankle Surg 24:374–382. https://doi.org/10.1016/j.fas.2017.06.004
Zeman J, Zeman P, Matejka T, Belatka J, Matejka J (2019) Comparison of lcp and intramedullary nail osteosynthesis in calcaneal fractures. Acta Ortop Bras 27:288–293. https://doi.org/10.1590/1413-785220192706223193
Sturbois-Nachef N, Allart E, Grauwin M-Y, Rousseaux M, Thévenon A, Fontaine C (2019) Tibialis posterior transfer for foot drop due to central causes: long-term hindfoot alignment. Orthop Traumatol Surg Res 105:153–158. https://doi.org/10.1016/j.otsr.2018.11.013
Burssens A, Van Herzele E, Leenders T, Clockaerts S, Buedts K, Vandeputte G et al (2017) Weightbearing CT in normal hindfoot alignment: presence of a constitutional valgus? Foot Ankle Surg. https://doi.org/10.1016/j.fas.2017.02.006
Zwipp H, Rammelt S, Amlang M, Pompach M, Dürr C (2013) Osteosynthese dislozierter intraartikulärer Kalkaneusfrakturen. Oper Orthop Traumatol 25:554–568. https://doi.org/10.1007/s00064-013-0246-3
Griffin D, Parsons N, Shaw E, Kulikov Y, Hutchinson C, Thorogood M et al (2014) Operative versus non-operative treatment for closed, displaced, intra-articular fractures of the calcaneus: randomised controlled trial. BMJ 349:g4483. https://doi.org/10.1136/bmj.g4483
Cheung GC, Kumar G (2014) The BMJ’s cover line on calcaneal fractures is misleading. BMJ 349:5208–5208. https://doi.org/10.1136/bmj.g5208
Agren P-H, Mukka S, Tullberg T, Wretenberg P, Sayed-Noor AS (2014) Factors affecting long-term treatment results of displaced intraarticular calcaneal fractures: a post hoc analysis of a prospective, randomized, controlled multicenter trial. J Orthop Trauma 28:564–568. https://doi.org/10.1097/BOT.0000000000000149
Rodriguez-Merchan EC, Galindo E (1999) Intra-articular displaced fractures of the calcaneus. Int Orthop 23:63–65. https://doi.org/10.1007/s002640050307
Humphrey JA, Woods A, Robinson AHN (2019) The epidemiology and trends in the surgical management of calcaneal fractures in England between 2000 and 2017. Bone Joint J 101:140–146. https://doi.org/10.1302/0301-620X.101B2.BJJ-2018-0289.R3
Rammelt S, Amlang M, Barthel S, Zwipp H (2004) Minimally-invasive treatment of calcaneal fractures. Injury 35(2):55–63. https://doi.org/10.1016/j.injury.2004.07.012
Zwipp H, Rammelt S, Barthel S (2004) Calcaneal fractures–open reduction and internal fixation (ORIF). Injury 35(2):46–54. https://doi.org/10.1016/j.injury.2004.07.011
Chen L, Zhang G, Hong J, Lu X, Yuan W (2011) Comparison of percutaneous screw fixation and calcium sulfate cement grafting versus open treatment of displaced intra-articular calcaneal fractures. Foot Ankle Int 32:979–985. https://doi.org/10.3113/FAI.2011.0979
Backes M, Schepers T, Beerekamp MSH, Luitse JSK, Goslings JC, Schep NWL (2014) Wound infections following open reduction and internal fixation of calcaneal fractures with an extended lateral approach. Int Orthop 38:767–773. https://doi.org/10.1007/s00264-013-2181-1
Benirschke SK, Sangeorzan BJ (1993) Extensive intraarticular fractures of the foot. Surgical management of calcaneal fractures. Clin Orthop Relat Res 1993:128–134
Zwipp H, Tscherne H, Thermann H, Weber T (1993) Osteosynthesis of displaced intraarticular fractures of the calcaneus. Results in 123 cases. Clin Orthop Relat Res 1993:76–86
Ding L, He Z, Xiao H, Chai L, Xue F (2013) Risk factors for postoperative wound complications of calcaneal fractures following plate fixation. Foot Ankle Int 34:1238–1244. https://doi.org/10.1177/1071100713484718
Sanders R, Fortin P, DiPasquale T, Walling A (1993) Operative treatment in 120 displaced intraarticular calcaneal fractures: results using a prognostic computed tomography scan classification. Clin Orthop Relat Res 1993:87–95
Bai L, Hou Y-L, Lin G-H, Zhang X, Liu G-Q, Yu B (2018) Sinus tarsi approach (STA) versus extensile lateral approach (ELA) for treatment of closed displaced intra-articular calcaneal fractures (DIACF): a meta-analysis. Orthop Traumatol Surg Res 104:239–244. https://doi.org/10.1016/j.otsr.2017.12.015
Schmutz B, Lüthi M, Schmutz-Leong YK, Shulman R, Platt S (2020) Morphological analysis of Gissane’s angle utilising a statistical shape model of the calcaneus. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03566-5
Khazen G, Rassi CK (2020) Sinus tarsi approach for calcaneal fractures: the new gold standard? Foot Ankle Clin 25:667–681. https://doi.org/10.1016/j.fcl.2020.08.003
Wright JG, Einhorn TA, Heckman JD (2005) Grades of recommendation. J Bone Joint Surg Am 87:1909–1910. https://doi.org/10.2106/JBJS.8709.edit
Funding
No funding has been provided for the current work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflict if interest directly of indirectly related to this work.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was not needed for this literature review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bernasconi, A., Iorio, P., Ghani, Y. et al. Use of intramedullary locking nail for displaced intraarticular fractures of the calcaneus: what is the evidence?. Arch Orthop Trauma Surg 142, 1911–1922 (2022). https://doi.org/10.1007/s00402-021-03944-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03944-7