Abstract
Background
Intramedullary calcaneal nailing is used to treat displaced intra-articular calcaneal fractures.
The main goal of the study was to assess the reduction of tomography and secondary goals were patient functional scores and complication rates.
Methods
The functional outcome and restoration of the radiographic parameters were evaluated post-operatively, at three months, at one year, and at the last follow-up. The morphology of the posterior facet was evaluated post-operatively, at one year and at the last follow-up by CTs.
Results
Twenty-six patients were included. The mean follow-up was 2.8 years. The mean AOFAS-AHS was 79 at the last follow-up. The mean calcaneal height index and length rose respectively from 0.44 to 0.86 and 83 to 87 mm, and the width decreased from 50 to 46 mm.
Conclusion
The radiographic parameters were restored. The AOFAS-AHS was comparable with other series. This study confirms the efficiency of this procedure with lower rate of complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The treatment of displaced intra-articular calcaneal fractures (DIACF) is controversial [1,2,3,4,5]. Studies have shown surgical management for these fractures improves patient functional outcomes in comparison with non-operative treatment [6]. However, randomized prospective studies have reported no advantages for operative treatment [1, 7, 8]. Open reduction of the calcaneus is performed using an extended “L”-shaped lateral exposure. This surgical approach has been associated with a high rate of infection or delayed wound healing: respectively 20% and 37% [4, 9].
In 2010, an intramedullary calcaneal nail was developed. This system aims to restore the axis and height of the calcaneus, and allows reduction of the posterior facet articular facet through an intraosseous tunnel in calcaneal tuberosity [10].
This study aimed to assess calcaneal reduction, using the angles Bohler and Gissane, and hindfoot axis on plain radiographs. Furthermore, the post-operative morphology of the calcaneus (height, length, width) and the posterior facet reduction was assessed using computed tomography (CT) scans with three dimensional reconstructions. Secondary outcome measures were patient post-operative functional scores using the American Orthopedic Foot and Ankle Society–Ankle Hindfoot Score (AOFAS-AHS), and the incidence of complications.
Materials and methods
This was a prospective, mono-centric, and single-operator study to assess the radiological and patient functional outcomes for displaced intra-articular calcaneal fractures (DIACF) treated with the Calcanail implant between 2014 and 2016 and quote complications.
Inclusion criteria was calcaneal fractures with the presence of a DIACF with loss of congruence of the subtalar joint. Patients with a follow-up period shorter than two years, with open fracture or undisplaced fracture, were excluded.
Oral consent was obtained for all patients for all aspects of the study. Ethics approval was obtained for this study (review CE-GP 2017-11).
Operative technique
Patients are placed in the lateral decubitus position, with the affected limb highest. A guide pin is inserted centered within the calcaneal tuberosity in the coronal plane, and directed toward the centre of the posterior facet in the sagittal plane. Two pins are then placed from lateral to medial, one perpendicular to the first guide pin, in the calcaneal tuberosity, and one vertical, like a plumb line, in the body of the talus. Distraction of these two non-parallel pins creates a void within the subtalar joint for articular elevation, and, additionally, corrects calcaneal varus. A 10-mm bony tunnel is then created in the intact portion of the posterior tuberosity with a trephine placed over the guide pin. Posterior facet reduction is performed through this tunnel using a combination of three specifically designed elevators (straight plugger, curved plugger, and curved spatula) (Fig. 1). Being straight or curved, they allow to reach lateral or medial fragment, mobilize and push them to the talus facet, and also extricate the constant fragment if necessary. The reduction is maintained thanks to the distractor tool and also because it could be considered as a primary reduction, with fragments stable since they are reduced. A 10-mm-diameter nail of three available lengths (Calcanail®, FH Orthopedics, France) is inserted and locked in place with two 4.5-mm cannulated screws inserted from lateral to medial using a guide jig. Placement of the locked nail maintains articular reduction and the morphology of the calcaneus obtained by traction (Fig. 2). The locking screws can additionally provide interfragmentary fixation in the coronal plane.
Post-operatively, the foot and ankle are immobilized in a short leg plaster splint, and the patient kept non-weight-bearing for three weeks. Weight-bearing is allowed from three weeks in hindfoot off-loading shoe. Full weight-bearing in normal shoes is allowed at six weeks and physiotherapy commenced.
Clinical outcome measures
Pre-operative patient data was collected including age, gender, fracture side, trauma mechanism, other injuries, and time until surgery. Skin condition was graded according to the Tscherne classification.
Surgical outcomes included tourniquet use and time, surgical time, and irradiation. Post-operatively, all patients were evaluated at three and six weeks, three, six and 12 months, then annually. At each clinical follow-up, three clinical scores were collected the AOFAS-AHS, VAS (visual analogic scale), and SEFAS (self-reported foot and ankle score).
The early and late complications were recorded. Finally, of the time to return to work was collected for employed patients.
Radiological outcome measures
Data measurement bias was minimized by a double measurement taken by two assessors (with at least 1 month in between measurements). Values analyzed were means of the measurements. The single surgeon was not involved.
The Böhler and the Gissane angles, fracture consolidation, and the calcaneal height index (Goldzak index) were measured on the lateral view radiographs before and after procedure (Figs. 5 and 6). The hindfoot alignment was evaluated post-operatively, using a goniometer, based on Djian’s quadrangle on the Meary view [11]. The calcaneal height index (Goldzak index) is the ratio of the height of the posterior thalamic surface (HT) (depressed for DIACFs) over the height (HC) of the cuboid bone (Fig. 3). Fractures were grouped according to the Sanders’ classification using CT.
CT scans were repeated first immediately after the procedure to control the posterior facet reduction and calcaneus global shape, then one year later and at the final follow-up to control reduction remains stable. The calcaneal length was measured on sagittal slices as at the midpoint of the anterior process, defined as the distance between the most anterior point of the rostrum and the most posterior point of the tuberosity. Calcaneal width was measured similarly in axial slices, at the midpoint of the sustentaculum tali.
The post-operative reduction of the posterior articular facet was evaluated on 3D reconstruction CT scans, with pericalcaneal subtraction. The Goldzak’s global articular reduction assessment was used as follows:
Excellent (type A or B reduction and Böhler angle more than 20°),
Good (type D or E reduction and Böhler angle more than 20°),
Poor (type C reduction with a step more than 2 mm or Böhler angle less than 20°) (Fig .4) [12].
Pre- and post-operative anterior view on 3D CT scan, according to Goldzak classification: Green circle represent anterior view of posterior facet and simplify how reduction is assessed. Type A: intact surface. Extra-articular fracture but with subsidence like tongue type. Type B: anatomical reduction of the posterior facet. Type C: step more than 2 mm. Type D: postero-superior gap with rotation of one of the fragment. Type E: overall gap in between facet fragments but with no step
Data analysis
Statistical analysis was performed using the paired t test. The level of statistical significance, with numbers available, was set at a P value < .05.
Statistical analysis was performed using the XLstat software (Addinsoft, Paris, France). Radiographs and CT scan measurements were carried out using the Horos software (Horos Project).
Results
Patient series
We analyzed the prospectively collected data of 26 consecutive patients: 20 men and six women with an average age of 39 ± 16 years (range 21–90). Twelve fractures were on the left side and 14 on the right side. Ten patients were active smokers (39%). One case of calcaneal nailing was a revision procedure performed one day following a percutaneous pinning.
The mean follow-up was 2.8 years ± eight months (range 24–48 months). Two patients were lost to follow-up due to death or moving away. Two patients subsequently underwent secondary subtalar arthrodesis. Twenty-two patients with a calcaneal nail in situ were available to image at final follow-up.
Pre-operative data
All patients presented superficial skin contusions or blisters around the fracture site (Tscherne classification C1).
According to the Sanders’ classifications, five patients were IIA, seven IIB, four IIIAB, five IIIAC, and five IV. Sanders types III and IV represented 53.8% (Fig. 5).
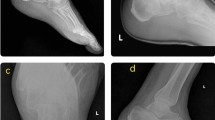
Patient 20: Measure of the Böhler angle and the calcaneal index pre-operatively A: Measure of the Böhler angle on the profile radiograph (11°). B: Measure of the calcaneal height index on the profile radiograph (0.61). C: Measure of the Böhler angle on the 3D CT scan profile view (11°). D: Measure of the calcaneal height index on the 3D CT scan profile view (0.61)
Operative data
The mean time before operative procedure was seven ± five days (range 0–15). The average duration of surgery was 69 ± 15 minutes (range 45–95). Mean fluoroscopy irradiation was 23 ± 17 cGy/cm. Twelve cases (45%) involved the use of the tourniquet.
Functional and clinical results
The post-operative functional results are summarized in Table 1. Podoscopic examination demonstrated that hindfoot varus was corrected in all patients. Footprints were corrected except two footprints that demonstrated first degree flat foot. Most patients reported gradual improvements in AOFAS-AHS over time. Two patients who did not improve required secondary subtalar fusion at 17 months and 24 months post-operatively. Their post-subtalar fusion AOFAS-AHS were 68 and 62 respectively for a maximal score of 92.
The mean time before return to work was 6.5 months (range 3 weeks to 24 months) in the 15 employed patients.
Plain radiographic and CT scan results
Radiological results are summarized in Table 2. All radiological findings stayed stable at the last follow-up (Figs. 6 and 7). The overall reduction was excellent in ten patients (39%), good in 11 patients (42%), and poor in five patients (19%) (Fig. 8). The mean post-operative hindfoot valgus, based on the Meary view radiograph, was 5° ± 1 (range 4–11) at the last follow-up. No residual hindfoot varus malalignment was found. Calcaneal fracture occurred within two months post-operatively in all patients.
Patient 20: Measure of the Böhler angle and the calcaneal index post-operatively A: Measure of the Böhler angle on the profile radiograph (35°). B: Measure of the calcaneal height index on the profile radiograph (1.0). C: Measure of the Böhler angle on the 3D CT scan profile view (35°). D: Measure of the calcaneal height index on the 3D CT scan profile view (1.0)
Complications
There was one high-grade complication in an active smoker who developed a skin necrosis with an early osteomyelitis of the calcaneal tuberosity. Removal of the device was required with a skin graft and prolonged dual intravenous (IV) antibiotic treatment administered with infection eradicated. The AOFAS-AHS at the last follow-up was 79 for this patient.
There were five lesser complications. One active smoker developed delayed wound healing, which resolved by local treatment within 45 days. One patient required implant removal at ten months post-operatively for prominence at the heel. The AOFAS-AHS after the removal was not available (lost to follow-up). Two patients required removal of the locking screws, due to pain and impingement on soft tissues. One patient developed complex regional painful syndrome, resolved within a year. His AOFAS-AHS was 85 at the last follow-up.
Two patients in our cohort required secondary subtalar fusion for post-traumatic subtalar osteoarthritis. Both cases demonstrated a type C, poor reduction on post-operative CT. One of these cases was of a Sanders’s III AB classification, developed painful calcaneofibular impingement, related to a lateral exostosis. For this patient, the AOFAS-AHS at final follow-up was 62.
We found no injury to the sural nerve or to the peroneal tendons.
Discussion
This study demonstrates that calcaneal nailing can benefit the reduction and fixation of the posterior facet and global shape in the surgical treatment of DIACF. The minimally invasive nature of this implant has many theoretical benefits. Our deep infection rate was low is comparison with other series of traditional open reductions [3, 5, 9].
Functional results
Our mean AOFAS-AHS is consistent with recent studies of long-term results on DIACF treated by open reduction and internal fixation (ORIF) utilizing an extensive lateral approach [13]. However, it is below that of Simon’s or Falis’, with 86.5 and 82 respectively with the same device (Table 3) [10, 14]. This difference might be explained by the younger age of our cohort, with higher functional demands.
No study has identified a statistically significant difference in the time before return to work among patients treated operatively and those treated non-operatively [2]. Our study reported a quick return to work and is a main asset.
Radiological outcomes
Few studies propose a clear evaluation of the reduction of the posterior facet of the calcaneus. Sanders’ evaluation is based on a single-section coronal CT scan of the thalamic surface. 3D CT scan reconstruction enabled a precise and very high demanding evaluation of both the posterior facet and overall calcaneal morphology, and the reduction maintenance over time [15]. Although Böhler angle and global shape were well restored, CT could identify a 2-mm step in the articular surface, enough to classify a type C (poor) reduction. We found no series in the literature which has submitted this kind of evaluation with a 2-mm step cut-off. In our study, Sanders types III and IV represented 53.8% but our patients with a residual step in the articular surface represented only 19% and with a good functional result [16, 17]. This rate might be only compared with other series if the same classification was applied. Some teams prefer to perform a primary fusion in these cases. We consider that, in Sanders III and IV, the posterior facet is severely affected and may lead to osteoarthritis with any surgical procedures. Nevertheless, the instrumentation of the device used allows a reduction or an improvement of the posterior facet and restore the global shape giving regularly good functional results. The procedure allows to prepare a possible secondary fusion, if needed, in good conditions with a correct axis of the hindfoot, no fibular impingement or tuberosity elevated.
In 2003, Kurozumi described a new CT classification to assess the reduction of the DIACF obtained by open reduction [18]. In his study, 12% of his patients retained a residual gap of the posterior thalamic facet post-ORIF. This highlights the fact that open fixation is also technically challenging, and despite its theoretical benefits for articular reduction, an anatomical result is not guaranteed.
Biomechanical perspectives
Goldzak and Simon demonstrated the biomechanical superiority of the intramedullary calcaneal nail over locking plate, in terms of load to failure and stiffness [12, 19]. Intramedullary nails offer better reduction stability and an early return to protected weight-bearing [20]. Our study supports the stability of the Böhler angle, calcaneal height index, length and width over time. A biomechanical study looked at the correlation between calcaneal height and the distribution of stress in the posterior surface of the subtalar joint [21]. It was reported that a 10-mm loss of calcaneal height resulted in a 15.6% maximal stress increase in the center of the posterior thalamic surface; for a height loss of 20 mm, this maximal stress increase was more than tripled (54.7%). Loss of calcaneal height and step-off is therefore an important parameter to be considered in the operative planning [22]. The standard calcaneal height index varies between 0.8 and 1 on radiographic lateral view, and between 0.8 and 1.1 on the frontal 3D CT scan.
Correction of calcaneal width is essential to prevent a calcaneofibular impingement or peroneal tendinopathy [23]. Correction of the length is also essential for the biomechanics of the achilleo-calcaneal-plantar complex. Accepted ranges for these data are uncertain. It is well established that a lack of posterior facet reduction gives poor results [24].
Complications
One infection and one case of delayed wound healing were observed in two patients who were active smokers. Recent experimental works and clinical observations have demonstrated that cigarette smoking impairs bone healing, wound healing and increases the risk of osteo-articular infections [25, 26]. The case of infection was observed on a psychiatric patient with a catatonic behavior. There is evidence that patients with psychiatric comorbidities have more complications and worse health-related quality of life than those without [27]. The case of delayed healing was of a patient with Sanders type III fracture. This represents a rate of 3.9% for each of these complications, compared with rates that can be as high as 20% and 37% respectively in ORIF procedures [4, 5, 9]. The intramedullary nail procedure, like other percutaneous procedure, is associated with a low risk of wound complications, particularly in the case of high-risk patients [28]. The good micro-circulation of the area of the main approach explains this low risk [29]. Moreover, Simon and Falis reported no wound complications or infections.
Operative treatment of DIACF lowers the risk of secondary subtalar fusion by 4.4 compared with non-operative treatment [30]. In our study, two patients (8.3%) required secondary subtalar fusion, which is similar to the data found in the literature, with rates between zero and 10 % for a mean follow-up between two and 12 years [1, 7, 8, 24].
Weaknesses of this study are there is no comparison group and the cohort lacks power to provide statistically significant measures of outcomes. Strength of this study are the monocentric prospective design with 2.8-year follow-up and a patient reported outcome (PROM) test, the inclusion of serial CT-scan analysis with 3D reconstruction, and the development of a new measure specific to fracture reduction.
Conclusion
This preliminary clinical study supports the effectiveness of the intramedullary nail procedure to restore the global shape and the articular posterior facet. This reduction was maintained over the short to medium term. Calcaneal nailing had a low rate of high-grade complications and enabled the patient to achieve a faster return to normal day-to-day life. Its design respects the principles of reduction, while incorporating the reduced complication rate of minimally invasive surgery.
References
Agren PH, Wretenberg P, Sayed-Noor AS (2013) Operative versus nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Jt Surg Am 95:1351–1357. https://doi.org/10.2106/JBJS.L.00759
Bruce J, Sutherland A (2013) Surgical versus conservative interventions for displaced intra-articular calcaneal fractures. Cochrane Database Syst Rev CD008628. https://doi.org/10.1002/14651858.CD008628.pub2
Buckley R, Leighton R, Sanders D et al (2014) Open reduction and internal fixation compared with ORIF and primary subtalar arthrodesis for treatment of Sanders type IV calcaneal fractures: a randomized multicenter trial. J Orthop Trauma 28:577–583. https://doi.org/10.1097/BOT.0000000000000191
Buckley RE, Tough S (2004) Displaced intra-articular calcaneal fractures. J Am Acad Orthop Surg 12:172–178
Gougoulias N, Khanna A, McBride DJ, Maffulli N (2009) Management of calcaneal fractures: systematic review of randomized trials. Br Med Bull 92:153–167. https://doi.org/10.1093/bmb/ldp030
Randle JA, Kreder HJ, Stephen D et al (2000) Should calcaneal fractures be treated surgically? A meta-analysis Clin Orthop Relat Res:217–227
Buckley R, Tough S, McCormack R et al (2002) Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Jt Surg Am 84-A:1733–1744
Griffin D, Parsons N, Shaw E et al (2014) Operative versus non-operative treatment for closed, displaced, intra-articular fractures of the calcaneus: randomised controlled trial. BMJ 349:g4483
Abidi NA, Dhawan S, Gruen GS et al (1998) Wound-healing risk factors after open reduction and internal fixation of calcaneal fractures. Foot Ankle Int 19:856–861. https://doi.org/10.1177/107110079801901211
Simon P, Goldzak M, Eschler A, Mittlmeier T (2015) Reduction and internal fixation of displaced intra-articular calcaneal fractures with a locking nail: a prospective study of sixty nine cases. Int Orthop 39:2061–2067. https://doi.org/10.1007/s00264-015-2816-5
Neri T, Barthelemy R, Tourne Y (2017) Radiologic analysis of hindfoot alignment: comparison of Meary, long axial, and hindfoot alignment views. Orthop Traumatol Surg Res 103:1211–1216. https://doi.org/10.1016/j.otsr.2017.08.014
Goldzak M, Simon P, Mittlmeier T et al (2014) Primary stability of an intramedullary calcaneal nail and an angular stable calcaneal plate in a biomechanical testing model of intraarticular calcaneal fracture. Injury 45(Suppl 1):S49–S53. https://doi.org/10.1016/j.injury.2013.10.031
Sanders R, Vaupel ZM, Erdogan M, Downes K (2014) Operative treatment of displaced intraarticular calcaneal fractures: long-term (10-20 years) results in 108 fractures using a prognostic CT classification. J Orthop Trauma 28:551–563. https://doi.org/10.1097/BOT.0000000000000169
Falis M, Pyszel K (2016) Treatment of displaced intra-articular calcaneal fractures by intramedullary nail. Preliminary report. Ortop Traumatol Rehabil 18:141–147. https://doi.org/10.5604/15093492.1205021
Roll C, Schirmbeck J, Muller F et al (2016) Value of 3D reconstructions of CT scans for calcaneal fracture assessment. Foot Ankle Int 37:1211–1217. https://doi.org/10.1177/1071100716660824
Qiang M, Chen Y, Jia X et al (2017) Post-operative radiological predictors of satisfying outcomes occurring after intra-articular calcaneal fractures: a three dimensional CT quantitative evaluation. Int Orthop 41:1945–1951. https://doi.org/10.1007/s00264-017-3577-0
Alexandridis G, Gunning AC, van Olden GDJ et al (2018) Association of pre-treatment radiographic characteristics of calcaneal fractures on patient-reported outcomes. Int Orthop 42:2231–2241. https://doi.org/10.1007/s00264-018-3852-8
Kurozumi T, Jinno Y, Sato T et al (2003) Open reduction for intra-articular calcaneal fractures: evaluation using computed tomography. Foot Ankle Int 24:942–948. https://doi.org/10.1177/107110070302401214
Eichinger M, Brunner A, Stofferin H et al (2018) Screw tip augmentation leads to improved primary stability in the minimally invasive treatment of displaced intra-articular fractures of the calcaneus: a biomechanical study. Int Orthop. https://doi.org/10.1007/s00264-018-4171-9
Nelson JD, McIff TE, Moodie PG et al (2010) Biomechanical stability of intramedullary technique for fixation of joint depressed calcaneus fracture. Foot Ankle Int 31:229–235. https://doi.org/10.3113/FAI.2010.0229
Wang Yi-min the 4th People’s Hospital of Shenzhen D of TO (2014) Finite element analysis of calcaneus stress distributions with variant heights. J Clin Rehabil Tissue Eng Res 6742_6746
Barrick B, Joyce DA, Werner FW, Iannolo M (2017) Effect of calcaneus fracture gap without step-off on stress distribution across the subtalar joint. Foot Ankle Int 38:298–303. https://doi.org/10.1177/1071100716678808
Rammelt S, Zwipp H (2004) Calcaneus fractures: facts, controversies and recent developments. Injury 35:443–461. https://doi.org/10.1016/j.injury.2003.10.006
Howard JL, Buckley R, McCormack R et al (2003) Complications following management of displaced intra-articular calcaneal fractures: a prospective randomized trial comparing open reduction internal fixation with nonoperative management. J Orthop Trauma 17:241–249
Krannitz KW, Fong HW, Fallat LM, Kish J (2009) The effect of cigarette smoking on radiographic bone healing after elective foot surgery. J Foot Ankle Surg 48:525–527. https://doi.org/10.1053/j.jfas.2009.04.008
Nasell H, Ottosson C, Tornqvist H et al (2011) The impact of smoking on complications after operatively treated ankle fractures--a follow-up study of 906 patients. J Orthop Trauma 25:748–755. https://doi.org/10.1097/BOT.0b013e318213f217
Renovell-Ferrer P, Berto-Marti X, Diranzo-Garcia J et al (2017) Functional outcome after calcaneus fractures: a comparison between polytrauma patients and isolated fractures. Injury 48(Suppl 6):S91–S95. https://doi.org/10.1016/S0020-1383(17)30801-X
Hammond AW, Crist BD (2013) Percutaneous treatment of high-risk patients with intra-articular calcaneus fractures: a case series. Injury 44:1483–1485. https://doi.org/10.1016/j.injury.2013.01.033
Carow JB, Carow J, Gueorguiev B et al (2018) Soft tissue micro-circulation in the healthy hindfoot: a cross-sectional study with focus on lateral surgical approaches to the calcaneus. Int Orthop 42:2705–2713. https://doi.org/10.1007/s00264-018-4031-7
Liu Y, Li Z, Li H et al (2015) Protective effect of surgery against early subtalar arthrodesis in displaced intra-articular calcaneal fractures: a meta-analysis. Med 94:e1984–e1980. https://doi.org/10.1097/MD.0000000000001984
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Fourgeaux, Dr. Estens, Pr Fabre, and Dr. Laffenetre declare that they have no conflict of interest.
Dr. Lucas y Hernandez reports consultancy for FH orthopedics during the conduct of the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of Evidence: Level III
Rights and permissions
About this article
Cite this article
Fourgeaux, A., Estens, J., Fabre, T. et al. Three-dimensional computed tomography analysis and functional results of calcaneal fractures treated by an intramedullary nail. International Orthopaedics (SICOT) 43, 2839–2847 (2019). https://doi.org/10.1007/s00264-019-04381-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-019-04381-3