Abstract
Purpose
Post-operative wound infections (PWI) following calcaneal fracture surgery can lead to prolonged hospital stay and additional treatment with antibiotics, surgical debridement or implant removal. Our aim was to determine the incidence of superficial and deep PWI and to identify risk factors (RF).
Methods
This study is a retrospective case series. All consecutive patients from 2000 to 2010 with a closed unilateral calcaneal fracture treated with open reduction and internal fixation (ORIF) by an extended lateral approach were included. Patient, fracture, trauma and peri-operative characteristics were collected, including RF such as smoking, diabetes mellitus, time to operation, pre-operative in- or outpatient management and wound closure technique. The primary end point was a PWI as defined by the US Centers for Disease Control and Prevention.
Results
A total of 191 patients were included of which 47 patients (24.6 %) had a PWI; 21 (11.0 %) and 26 (13.6 %) patients had a superficial and deep wound infection, respectively. American Society of Anesthesiologists (ASA) classification higher than ASA 1 was associated with an increased risk. Placement of a closed suction drain at the end of surgery was associated with less PWI (35 % vs 15 %, p = 0.002). In this study, none of the previously reported RF were associated with an increased risk for PWI.
Conclusions
ORIF of displaced calcaneal fractures is associated with a high rate of PWI of 25 %. Factors that were associated with an increased risk were ASA classification other than 1 and absence of a closed suction drain placement. A closed suction drain may be a protective measure to avoid wound complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Calcaneal fractures account for less than 2 % of all fractures [1, 2]. Treatment may consist of operative or conservative management. Patients treated with open reduction and internal fixation (ORIF) are more likely to develop wound complications. However, surgery correlates with better patient-related outcome [3, 4].
Calcaneal surgery is infamous for its post-operative infection rate leading to prolonged hospital stay and secondary operations. The incidence of a wound infection following operative treatment of closed calcaneal fractures varies between 2 % and 25 % and rates of complications requiring surgery are up to 21 % [5–19] (Table 1).
Some studies identified covariates associated with an increased risk of wound complications such as a higher body mass index (BMI), smoking [5, 20] and drug abuse [12]. In addition, the incidence of wound infections increased in patients who were managed as outpatients pre-operatively or underwent surgery more than five or 14 days following trauma [5, 20, 21]. However, another recent retrospective study showed no correlation with surgical timing [22]. Intra-operative risk factors were surgical experience [12, 23] and a single layered closure technique [20].
In the decision to treat patients operatively or conservatively it is important to consider risk factors for wound complications. The main drawback of previous research is that many risk factors were identified in small case series. The aim of this study was to assess the relation between wound infections and associated risk factors in a large series of patients with unilateral closed displaced calcaneal fractures treated with ORIF through an extended lateral approach (ELA) at an academic level 1 trauma centre.
Patients and methods
All consecutive patients over a 12-year period (January 2000 until December 2011) with a unilateral calcaneal fracture treated with ORIF through an ELA were included in this retrospective study. Patients with open fractures and/or treatment with an external fixator prior to ORIF were excluded because of the increased risk of post-operative wound complications [9, 11, 12]. Patients with bilateral calcaneal fractures were excluded because of the unfeasibility of performing an independent analysis of two fractures in the same patient. Other exclusion criteria were patients who were operated with a different approach than the ELA (including patients with a primary arthrodesis through an ELA), referred patients with a pre-existing wound infection, reconstructive surgery following conservative treatment for calcaneal fracture and patients with incomplete follow-up. Polytrauma patients who underwent surgery on other extremities or body parts in the same operative session as calcaneal fracture surgery were excluded from analysis considering operation time. Minimal follow-up was one year. To prevent observer bias, the treating surgeons were not part of the review team. The Institutional Review Board approved the study.
Clinical data
Data were obtained from the hospital’s electronic and paper medical records: patient characteristics were gender, age at the time of trauma, insurance status, BMI, past medical history (psychiatric/cardiac/pulmonary/peripheral vascular disease/diabetes mellitus), known substance abuse and American Society of Anesthesiologists (ASA) classification. Duration of post-operative hospital stay and type of management were also recorded. Following trauma, patients were either hospitalised (inpatient management) or admitted to the hospital a day prior to surgery (outpatient management).
The following trauma characteristics were documented: polytrauma patient (defined as Injury Severity Score ≥16) and trauma mechanism, classified as low- and high-energy trauma (LET and HET) and subdivided in fall from height, fall from stairs, motor vehicle accident (MVA), direct trauma or other mechanism. Fracture characteristics were: side of injury, presence of ipsilateral foot or lower extremity fractures and fracture type. All fractures were classified according to the Sanders and the Essex-Lopresti classifications by a specialised trauma surgeon and a radiologist, and radiographic analysis for Böhler’s angles was performed on pre- and direct post-operative lateral images [24, 25]. The increase in Böhler’s angle was measured to analyse a possible association with wound infections due to increased tension on the wound edges in intra-operative adjustment to a normal angle. Finally, preoperative and intra-operative characteristics were collected such as time to surgery, the surgeon’s experience, duration of surgery, tourniquet use and duration, closed suction drain placement and wound closure technique.
The primary outcome, post-operative wound infection, was classified as superficial or deep infection by applying the criteria of the US Centers for Disease Control and Prevention for defining a surgical site infection [26]. Superficial wound infections were defined as wound dehiscence or signs of infections (confirmed with a positive culture) amenable to conservative treatment with antibiotics. Deep wound infections were confirmed with a positive culture and defined as osteomyelitis, infected hardware or a plate fistula needing hardware removal, (readmission with) intravenous antibiotics or wound debridement with or without local antibiotic treatment with gentamicin beads or vacuum-assisted closure.
Surgical procedure
All patients were advised to strictly elevate the foot and ankle in between trauma (no cast) and surgery and intravenous antibiotics were administered to all patients 30 minutes prior to surgery (1,500 mg cefuroxime). The patient was placed in the contralateral decubitus position of the injured leg on a radiolucent operating table. The ELA (Seattle/modified Kocher) was used [10, 24] (Fig. 1) in which the full-thickness flap was retracted according to the no-touch technique, with temporary K-wires in the talus to facilitate operative exposure [10]. A non-locking stainless steel AO/Synthes calcaneal plate with stainless steel 3.5-mm screws (Synthes, West Chester, PA, USA) was used. A tourniquet was not used routinely.
a Pre-surgical demarcation: the inverted C line is the base of the fifth metatarsal, the dotted line is the head of the fibula, the upper line is the wrong approach and the lower line is the ELA. b Surgical view in which the full-thickness flap is retracted according to the no-touch technique, with temporary K-wires in the talus to facilitate operative exposure. c Post-operative view with Donati Ethilon® sutures and a closed suction drain
The goal of surgery was restoration of articular surfaces, calcaneal height, width and length, and correction of varus. Intra-operatively the positions of the fragments, plate and screws were evaluated by the surgeon with fluoroscopy. Wound closure was either performed with subcuticular inverted Vicryl sutures combined with Steri-Strips (3M, St. Paul, MN, USA) and/or (Allgöwer-)Donati Ethilon (Ethicon, Division of Johnson & Johnson, Somerville, NJ, USA) sutures depending on the preference of the surgeon as well as placement of a closed suction drain (8 F). Post-operatively the drain was removed when production was less than 30 cc in the last 24 hours or after 48 hours. All patients were hospitalised following surgery and none were treated in day care. Post-operative antibiotics were not prescribed routinely. Patients were kept non-weight-bearing for a period of 12 weeks and were instructed to perform flexion and extension exercises of the ankle.
Statistical analyses
Data were analysed using the Statistical Package for the Social Sciences (SPSS) version 19.0 (SPSS Inc., Chicago, IL, USA). Normality of continuous data was tested with the Kolmogorov-Smirnov test and by inspecting the frequency distributions (histograms). Descriptive analysis was performed to compare baseline characteristics between patients with and without an infection. For continuous data, mean SD (parametric data) or medians and interquartile ranges (non-parametric data) were calculated. Differences were assessed using Student’s t test (parametric data) or the Mann-Whitney U test (non-parametric data).
Categorical data were compared using the chi-square test. A p value <0.05 was taken as the threshold of statistical significance. Firstly, a univariate analysis was performed followed by a multivariate logistic regression analysis to model the relationship between different covariates and wound infection. Covariates with a p < 0.2 and expected associated risk factors were selected for the multivariate regression. This was done for the total population of patients with a wound infection and for a subgroup of patients with a deep wound infection.
Results
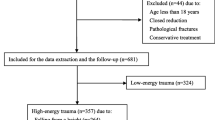
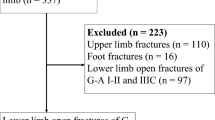
There were 260 patients with 279 calcaneal fractures treated operatively during the 12-year study period. A total of 191 patients were included (Fig. 2). Patient characteristics are found in Table 2.
Forty-seven patients (24.6 %) had a post-operative wound infection confirmed with a positive culture. Of these patients, 21 (11.0 %) had a superficial and 26 (13.6 %) had a deep wound infection. In 20 (42.6 %) of the 47 patients with a wound infection, the infection was treated with oral antibiotics. In one patient (2.1 %) the infection resolved spontaneously with local wound care without the use of antibiotics. In 18 patients (38.3 %) with a deep wound infection intravenous antibiotics were administered. In general, the indication for operative debridement was a wound infection without clinical improvement with intravenous antibiotics (ongoing drainage, septic signs). This decision was left to the discretion of the attending surgeon. In eight patients (20 %) intravenous antibiotic treatment and surgical debridement were not successful and the implant had to be removed because of an ongoing infection. No amputations were performed.
In the univariate analysis, ASA classification other than 1 (p = 0.001) showed an increased risk of a post-operative wound infection. Patients with a wound infection were hospitalised two days longer on average compared to the group without a wound infection (seven vs five days, p < 0.001). Patients with a deep wound infection were hospitalised for an average of an extra four days compared to patients without a deep wound infection (nine vs five days, p < 0.001). In 83.2 % the operation was performed by a single senior surgeon. In 99 patients (53.6 %) a closed suction drain was placed and this was associated with less post-operative wound infections (35 vs 15 %, p = 0.002). This association was not seen when looking at the deep infections only. In the 86 patients without drain placement there were 34.9 % wound infections of which 16.3 % were deep infections. Finally, multivariate analysis of six possible risk factors was performed based on results in the univariate analysis of this study and previously reported risk factors from the literature. This also showed a decreased risk of post-operative wound infections after placement of a closed suction drain at the end of surgery (p = 0.003) (Table 3).
Discussion
In this case series of 191 unilateral calcaneal fractures the post-operative wound infection rate was 25 % of which 13.6 % were deep infections. Factors that were associated with an increased risk for wound infections were ASA classification other than 1 and absence of a closed suction drain placement at the end of surgery. None of the previously reported risk factors (higher BMI, drug abuse, smoking, outpatient management and surgery after more than five or 14 days) showed a relation with a post-operative wound infection in our study [5, 12, 20, 21] (Table 3). As there was no difference in wound infections between pre-operative in- or outpatients we find that pre-operative outpatient management is acceptable. As could be expected, hospital stay for the index fracture was longer in patients with a wound infection.
In the literature on drain placement in surgery of the musculoskeletal system no significant differences were found in incidence of wound infections, dehiscence or re-operation [27]. Unfortunately no specific data on calcaneal fracture surgery were available in this study. Closed suction drain placement has previously not been shown to reduce wound healing complications [20]. However, in our study placement of a closed suction drain during surgery resulted in a significant decrease of post-operative wound infections. As 83 % of surgeries were performed by a single senior surgeon who decided on drain placement in 85 patients (54 %) vs no drain placement in 69 (43 %) with missing data in five patients we cannot exclude selection bias. Because of the retrospective character of the study we do not have information about haemostasis before wound closure. Surprisingly, the effect of a closed suction drain on post-operative wound infections was only found for the total population of patients with wound infections. In the subgroup of patients with deep infections this effect could not be detected. We suspect this is due to the small number of patients in this group (n = 26).
Our study shows a considerable percentage of wound infections. As previously noted, infection rates in the literature vary between 2 % and 25 % [5–19] (Table 1). The policy at our facility is to treat the vast majority of dislocated intra-articular calcaneus fracture patients operatively, irrespective of any unfavourable factors for wound healing, which could contribute to the high rate of infections. This considerable rate of wound infections is more likely the result of our type of surgical approach. As we recently started performing calcaneal surgery more often by an even more extended lateral approach according to Freeman et al. [28] and (in less complex fractures) via the sinus tarsi approach [29, 30], the severe wound complication rates appear to have decreased. In the latter type of approach a wound complication rate of 29 % in the ELA versus 6 % in the less invasive sinus tarsi approach was described [31].
In summary, we present a large series of consecutive patients with closed displaced calcaneal fractures treated with ORIF. A post-operative wound complication rate of 25 % was detected and ASA classification other than 1 and no closed suction drain placement at the end of surgery were identified as risk factors for wound infection. We therefore conclude that a closed suction drain may be a protective measure to avoid wound complications. Future studies are required to further investigate the long-term clinical outcome in patients with a post-operative wound infection.
References
Mitchell MJ, McKinley JC, Robinson CM (2009) The epidemiology of calcaneal fractures. Foot (Edinb) 19(4):197–200. doi:10.1016/j.foot.2009.05.001
Schepers T, van Lieshout EM, van Ginhoven TM, Heetveld MJ, Patka P (2008) Current concepts in the treatment of intra-articular calcaneal fractures: results of a nationwide survey. Int Orthop 32(5):711–715. doi:10.1007/s00264-007-0385-y
Howard JL, Buckley R, McCormack R et al (2003) Complications following management of displaced intra-articular calcaneal fractures: a prospective randomized trial comparing open reduction internal fixation with nonoperative management. J Orthop Trauma 17(4):241–249
Jiang N, Lin QR, Diao XC, Wu L, Yu B (2012) Surgical versus nonsurgical treatment of displaced intra-articular calcaneal fracture: a meta-analysis of current evidence base. Int Orthop 36(8):1615–1622. doi:10.1007/s00264-012-1563-0
Folk JW, Starr AJ, Early JS (1999) Early wound complications of operative treatment of calcaneus fractures: analysis of 190 fractures. J Orthop Trauma 13(5):369–372
Harvey EJ, Grujic L, Early JS, Benirschke SK, Sangeorzan BJ (2001) Morbidity associated with ORIF of intra-articular calcaneus fractures using a lateral approach. Foot Ankle Int 22(11):868–873
Naovaratanophas P, Thepchatri A (2001) The long term results of internal fixation of displaced intra-articular calcaneal fractures. J Med Assoc Thai 84(1):36–44
Buckley R, Tough S, McCormack R et al (2002) Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am 84-A(10):1733–1744
Benirschke SK, Kramer PA (2004) Wound healing complications in closed and open calcaneal fractures. J Orthop Trauma 18(1):1–6
Zwipp H, Rammelt S, Barthel S (2004) Calcaneal fractures–open reduction and internal fixation (ORIF). Injury 35(Suppl 2):SB46–SB54. doi:10.1016/j.injury.2004.07.011
Koski A, Kuokkanen H, Tukiainen E (2005) Postoperative wound complications after internal fixation of closed calcaneal fractures: a retrospective analysis of 126 consecutive patients with 148 fractures. Scand J Surg 94(3):243–245
Court-Brown CM, Schmied M, Schutte BG (2009) Factors affecting infection after calcaneal fracture fixation. Injury 40(12):1313–1315. doi:10.1016/j.injury.2009.03.044
Demcoe AR, Verhulsdonk M, Buckley RE (2009) Complications when using threaded K-wire fixation for displaced intra-articular calcaneal fractures. Injury 40(12):1297–1301. doi:10.1016/j.injury.2009.03.017
Kienast B, Gille J, Queitsch C et al (2009) Early weight bearing of calcaneal fractures treated by intraoperative 3D-fluoroscopy and locked-screw plate fixation. Open Orthop J 3:69–74. doi:10.2174/1874325000903010069
Gaskill T, Schweitzer K, Nunley J (2010) Comparison of surgical outcomes of intra-articular calcaneal fractures by age. J Bone Joint Surg Am 92(18):2884–2889. doi:10.2106/JBJS.J.00089
Bergin PF, Psaradellis T, Krosin MT et al (2012) Inpatient soft tissue protocol and wound complications in calcaneus fractures. Foot Ankle Int 33(6):492–497. doi:10.3113/FAI.2012.0492
Wu Z, Su Y, Chen W et al (2012) Functional outcome of displaced intra-articular calcaneal fractures: a comparison between open reduction/internal fixation and a minimally invasive approach featured an anatomical plate and compression bolts. J Trauma Acute Care Surg 73(3):743–751. doi:10.1097/TA.0b013e318253b5f1
Ding L, He Z, Xiao H, Chai L, Xue F (2013) Risk factors for postoperative wound complications of calcaneal fractures following plate fixation. Foot Ankle Int 34(9):1238–1244. doi:10.1177/1071100713484718
Rammelt S, Zwipp H, Schneiders W, Dürr C (2013) Severity of injury predicts subsequent function in surgically treated displaced intraarticular calcaneal fractures. Clin Orthop Relat Res 471(9):2885–2898. doi:10.1007/s11999-013-3062-z
Abidi NA, Dhawan S, Gruen GS, Vogt MT, Conti SF (1998) Wound-healing risk factors after open reduction and internal fixation of calcaneal fractures. Foot Ankle Int 19(12):856–861
Tennent TD, Calder PR, Salisbury RD, Allen PW, Eastwood DM (2001) The operative management of displaced intra-articular fractures of the calcaneum: a two-centre study using a defined protocol. Injury 32(6):491–496
Ho CJ, Huang HT, Chen CH, Chen JC, Cheng YM, Huang PJ (2013) Open reduction and internal fixation of acute intra-articular displaced calcaneal fractures: a retrospective analysis of surgical timing and infection rates. Injury 44(7):1007–1010. doi:10.1016/j.injury.2013.03.014
Schepers T, Den Hartog D, Vogels LM, Van Lieshout EM (2013) Extended lateral approach for intra-articular calcaneal fractures: an inverse relationship between surgeon experience and wound complications. J Foot Ankle Surg 52(2):167–171. doi:10.1053/j.jfas.2012.11.009
Sanders R, Fortin P, DiPasquale T, Walling A (1993) Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop Relat Res 290:87–95
Essex-Lopresti P (1952) The mechanism, reduction technique, and results in fractures of the os calcis. Br J Surg 39(157):395–419
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 20(4):250–278. doi:10.1086/501620, quiz 279–80
Parker MJ, Livingstone V, Clifton R, McKee A (2007) Closed suction surgical wound drainage after orthopaedic surgery. Cochrane Database Syst Rev 3:CD001825. doi:10.1002/14651858
Freeman BJ, Duff S, Allen PE, Nicholson HD, Atkins RM (1998) The extended lateral approach to the hindfoot. Anatomical basis and surgical implications. J Bone Joint Surg Br 80(1):139–142
Schepers T (2011) The sinus tarsi approach in displaced intra-articular calcaneal fractures: a systematic review. Int Orthop 35(5):697–703. doi:10.1007/s00264-011-1223-9
Nosewicz T, Knupp M, Barg A et al (2012) Mini-open sinus tarsi approach with percutaneous screw fixation of displaced calcaneal fractures: a prospective computed tomography-based study. Foot Ankle Int 33(11):925–933. doi:10.3113/FAI.2012.0925
Kline AJ, Anderson RB, Davis WH, Jones CP, Cohen BE (2013) Minimally invasive technique versus an extensile lateral approach for intra-articular calcaneal fractures. Foot Ankle Int 34(6):773–780. doi:10.1177/1071100713477607
Acknowledgments
The authors kindly thank R. Wouters, M.D. for his aid in data collection during this study. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Backes, M., Schepers, T., Beerekamp, M.S.H. et al. Wound infections following open reduction and internal fixation of calcaneal fractures with an extended lateral approach. International Orthopaedics (SICOT) 38, 767–773 (2014). https://doi.org/10.1007/s00264-013-2181-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-013-2181-1