Abstract
Introduction
Calcaneal fractures account for 60–75% of all tarsal fractures and represent surgical challenges because of their frequency and complexity. Despite standardized procedures and new implants, literature reports high revision rates and unsatisfactory results. The study aims to describe the role of the surgeon with respect to the clinical outcome.
Methods
Between 2014 and 2017, 94 calcaneal fractures (all type AO C1-3) were re-examined in 86 patients (67 male and 19 female; mean age: 51 years). The treatment was always carried out by means of locking compression plate via the extensile lateral approach. A comparison was made between treatment by an experienced (ES) and less experienced surgeon (LES). Annually, the ES performed at least 30 procedures for calcaneus fracture treatment as compared to < 10 operations performed by the LES.
Results
The mean AOFAS, VAS FA, and Kiel Score in the ES group were 77.0 (SD 15.9), 69.0 (SD 18.8), and 65.0 (SD 20.6), respectively. The corresponding values in the LES group were 68.1 (SD 21.0), 60.3 (SD 22.4), and 53.0 (SD 21.9) (p < 0.05). The operation time was on average 14 min shorter in the ES group than the LES group (p < 0.05).
Conclusion
The significantly better scores, along with shorter operation time, shorter duration of incapacity to work, and lower complication rate prove the importance of having an experienced surgeon perform complex intra-articular calcaneal fracture repairs. The extensile lateral approach is still considered the standard method.
Level of evidence
Level III, comparative series.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Calcaneal fractures account for only 2% of all fractures, but they represent 60–75% of all tarsal fractures. About 10% are bilateral calcaneal fractures. For the patient, this injury represents a life-changing event with questionable return to work [1,2,3].
Calcaneal fractures are usually accompanied by varus malalignment, plantar widening and, above all, a reduction or even negation of the Böhler angle. The last-mentioned factor represents an essential success control and is one of the measured outcome parameters.
Owing to its complexity, surgical treatment still remains a challenge in calcaneal fractures; the extensile lateral approach is still one of the most frequently used methods for treatment [4,5,6,7,8,9].
However, given the high complication rates reported, this approach has become increasingly less popular. The demand for minimally invasive approaches as well as the comparative results with conservative therapy has regained popularity [10, 11].
Despite critical examination of the choice of approach and constant improvement of surgical instruments and osteosynthesis material, it is not always possible to achieve a satisfactory outcome. The possible causes include material failure, implant loosening, early and late infections, malunion, nonunion, and posttraumatic arthrosis [12]. On the patient side, nicotine abuse, being overweight, diseases such as diabetes mellitus, and lack of compliance are contributing factors [13,14,15].
In this study, we evaluated the role of the surgeon in the treatment of displaced intra-articular calcaneal fractures.
Patients and methods
Population
In this retrospective study, all calcaneal fractures treated in the study center between 2014 and 2017 were recorded. A total of 192 fractures were identified from the clinic's internal database. Taking into account the inclusion and exclusion criteria (Fig. 1), 120 patients were considered eligible, of which 86 patients with 94 fractures (74 male, 78.7%; 20 female, 21.3%) were finally included in the study. The remaining patients refused to participate in the study or could not be contacted. The mean age at surgery was 51 (range: 22–76) years (Table 1, Fig. 1). The patients included in the study were invited, in writing, to a follow-up examination. The mean follow-up time was 3.2 (range: 2.6–3.9) years.
Inclusion and exclusion criteria
The inclusion criteria were: only displaced intra-articular calcaneal fractures (AO C1-3 classification) in patients who underwent surgery exclusively at our study center; treatment using locking compression plate via the extensile lateral approach (ELA); and a minimum age of 18 years and a written declaration of consent to participate in the study. The exclusion criteria were patients with concomitant or previous injuries and those with non-displaced or extraarticular calcaneal fractures.
Assessments methods
In this study, fractures were classified according to Sanders and the modified AO classification [16, 17]. Demographic data, body mass index (BMI), and nicotine abuse were recorded.
The AOFAS-Score (American Orthopedic Foot and Ankle Society), the Kiel score for calcaneus fractures, and the VAS FA (Visual-Analogue-Scale Foot and Ankle) were used to assess quality of life and performance. Furthermore, the duration of surgery and time of incapacity to work were recorded.
In addition, the documentation of possible complications such as infections, revision procedures, material removal, and subtalar arthrodesis was carried out during the course of the procedure. In addition, an assessment of the preoperative and current Böhler angle was performed in the radiographic control.
All results were classified into treatment by particularly experienced surgeons (ES, n = 2) and less experienced surgeons (LES, n = 2). The term “experienced surgeon” was derived based on the number of calcaneus fracture treatments that were performed independently. Regardless of the study, the average number was 30 per year. In the LES group, less than 10 per year calcaneus fracture treatments were performed by the surgeon. In the present study, 60 and 34 fractures were treated by particularly experienced and less experienced surgeons, respectively. Furthermore, the scores of all surgeons were compared over time (“treatment in early half of the study” and “late half of the study”).
All procedures performed in this study were in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The ethics committee of the institutional review board approved this study (FF 92/2016). Informed consent was obtained from all patients. None of the authors have any conflict of interest to declare.
Surgical procedure
The treatment of complex intra-articular calcaneal fractures (AO C1-3) was performed routinely by means of locking compression plate via the ELA with closed femoral blood vessels. Intra-operative fluoroscopic 3D-imaging for reduction control was used routinely [18]. All operations were performed according to a standardized procedure at the specialist level (Figs. 2, 3a, b) [19]. In two cases, 2–3° open fractures were initially treated with an external fixator [20]. The definitive treatment of all fractures took place on average after 7 days.
The goal of any treatment is always preservation of the subtalar joint. To avoid overloading the neighboring joints with resulting arthrosis of the upper ankle and Chopart' joints, the authors felt the need to preserve the lower ankle joint [21]. An arthrodesis was considered the ultima ratio.
Rehabilitation protocol
The post-treatment recovery provided for wearing an orthotic boot for 12 weeks on forearm crutches for 6 weeks, 24 h/day with sole contact. Removal of the boot for personal hygiene and physiotherapy was permitted. Six weeks postoperatively, radiography was followed by subsequent load build-up over the next 6 weeks. During the load build-up, the boot could be removed at night. At 12 weeks postoperatively, computed tomographic (CT) imaging was carried out before granting permission to wear normal street shoes.
An exception to this scheme was made for the nine bilateral fractures. After the 6-week relief, the weight was alternately applied in the wheelchair and on the anti-gravity treadmill (AlterG®). In addition to gait training, the accompanying physiotherapy included lymphatic drainage, toe mobilization, and active-assistive exercise of the upper ankle joint.
Statistical analysis
It is a monocentric comparative case study with data collection averaging 3.2 (2.6–3.9) years postoperatively. Case number calculation was omitted in the sense of the retrospective design. The statistical analysis was conducted using IBM SPSS Statistics version 23 (IBM Dtl. GmbH, Ehningen, Germany) and JASP 0.12.1 (2013–2020 University of Amsterdam, Netherlands). Mean values from the ES and LES groups were compared using the Student's t-test for independent samples. The significance level was set at p < 0.05.
Results
As shown in Table 1, there was an equal distribution of demographic data; risk profile (age, nicotine abuse, BMI); and fracture type in both groups.
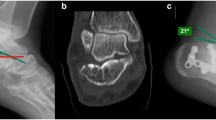
The fractures were always displaced intra-articular calcaneal fractures of Sanders type 3 and 4 (Sanders 3: 57.4%, Sanders 4: 42.6%) or AO C1-3 (Table 1, Fig. 4a–c). All patients were treated by locking compression plate via the extensile lateral approach.
Scores
The mean AOFAS, VAS FA, and Kiel scores of all patients was 73.6 (range: 27–100), 65.8 (range: 20–100), and 60.7 (range: 12–99), respectively. The comparison of the results from the LES and ES groups showed significantly better results for the experienced surgeon in all presented scores (p < 0.05) (Table 2).
Times
The mean duration of surgery was significantly longer in the LES group (128.4 min) than in the ES group (114.6 min, p = 0.047). The overall mean time of incapacity of all patients was 28.5 weeks (31.3 (SD: 27.4) vs. 26.8 (SD: 27.4) weeks, in the LES and ES groups, respectively (p > 0.05) (Table 2).
Radiological results
The radiographically determined Böhler angle improved from preoperative 11.5° to postoperative 32.8° in the Les group and from preoperative 8.1° to postoperative 31.8° in the ES group. Thus, the LES and ES groups achieved a mean improvement of 20.8° and 23.8°, respectively. The difference between LES and ES was not significant (p > 0.05).
Implant removal and complications
In 38 cases (40.4%), metal removal was carried out in the meantime because of local irritation. The frequency was quite similar in the two groups (23 [38.3%] vs. 15 [44.1%] in the ES and LES groups, respectively).
Regardless of group affiliation, 32 (84%) patients reported a subjective relief of symptoms after metal removal.
Five relevant complications with wound conditions required revision. Two cases could be treated by irrigation, superficial debridement. In the remaining three cases, a deep wound infection was detected, and the implant was removed prematurely. In two cases, a 3° open fracture was the cause.
Overall, one and four complications occurred in the ES and LES groups, respectively. The results of patients with bilateral fractures did not differ significantly from those with unilateral fractures in the 3-year study with regard to the parameters mentioned above and were therefore not listed separately.
In cases of advanced arthrosis of the subtalar joint, six subtalar arthrodesis (LES: 2, ES: 4) were performed in the further course of the procedure. Their results too did not differ significantly from the rest of the patients and are also not listed separately owing to the small number of cases.
Discussion
The results of our study confirm that surgeon’s experience is a particularly relevant influencing variable. We were able to show significant differences between the LES and ES groups.
As early as 1993, Sanders et al. published a paper on the outcome of osteosynthetically treated calcaneal fractures and observed the learning curve in the treatment. In the years 1987–1990, an improvement in the radiographic reduction result of type II and III fractures n. Sanders, but surprisingly not for type IV fractures.
However, the study at that time also included non-displaced type II fractures. And even a conservative treatment was part of the study.
In addition, the study was conducted before the advent of today's common use of locking compression plates [22]. The question regarding the role of the surgeon remained of unrestricted importance [23].
Recent studies have emphasized the need for exact anatomical reduction using locking plates [24]. Significant surgical expertise is required to achieve such a result. As reported by Persson et al., the Böhler angle was also used in the present study to assess the success of the procedure [25]. In the present study, the reconstruction of the Böhler angle, an important radiological feature, tended to be better for experienced surgeons, but this was not statistically significant. Irrespective of the frequent mentions, the actual significance of the Böhler angle must therefore be questioned. Furthermore, no positive correlation could be found between Böhler angles and the clinical scores discussed below.
A uniform recommendation for the radiological evaluation of the reduction result is missing in the literature so far [26]. The work of Keizer et al. in 2017, who initiated a uniform scoring protocol for radiological assessment, seems promising [27].
Ahn et al. 2019 proposed a trend-setting assessment of the surgeon’s learning curve. In all, 45 cases were CT-morphologically examined for the reduction result and Böhler and Gissane angles were compared. They concluded that a minimum of 20 fracture treatments of the calcaneus lead to significantly better results. This is consistent with the mean value between the ES and LES groups in the present study. Moreover, the mean surgery time was almost identical, at 117 min. However, the heterogeneous fracture classification (Sanders type 2–4) should be noted [23].
To reduce approach morbidity and the associated wound complications, the demand for less invasive approaches have been made in recent years. Stabilization of the calcaneus fracture is achieved either by minimally invasive plate osteosynthesis (MIPO) or treated by an intramedullary nail. The present study lacks a direct comparison of the bony reconstruction of the calcaneus using a locking compression plate versus the intramedullary nail. However, based on the clinical scores and complication rates, the locking compression plate shows comparably good results in a previously published study [28]. The present study with a large number of cases thus confirms that ELA remains a safe approach in the surgical treatment of complex intra-articular calcaneal fractures [4, 6, 29]. The alarming revision rates of over 25% due to wound infections and wound margin necrosis in the literature can, in the authors' view, be significantly reduced by careful soft tissue management [30,31,32,33].
The clinical results presented in the present manuscript are consistent with studies in the literature [34, 35]. The complication rate was remarkably lower than with the sinus-tarsi approach or a minimally invasive procedure [37]. The results of the present study confirm the surgeon himself as an important influencing factor [38]. In the authors' view, the low complication rate and comparably good results mean that the need for newer implants and minimally invasive approaches is secondary.
We agree with Rammelt et al. that an optimal result in surgical restoration can only be achieved with anatomically correct reduction. This ability is because of experience and the growing expertise of the surgeon.
If the reduction is insufficient, the disadvantages of surgical and non-operative treatment are combined [24]. Even though four of the five relevant complications occurred in the LES group, the overall acceptably low infection rate of 5.3% must be emphasized, especially with regard to the exclusively displaced fractures type AO C1-3.
It is noteworthy that nicotine abuse did not have a significant influence on the clinical scores in the present study. However, the aforementioned five complications all occurred in smokers, which likely confirms the known negative influence of nicotine abuse on soft tissue and bone healing [39,40,41,42].
In both groups, implant removal was performed with the same frequency in about 40% of patients, mainly owing to local irritation. The question of the benefit of a planned implant removal from the calcaneus after bony consolidation is still debatable [43], with a prospective comparison missing in published literature. In the present study, the majority of patients reported a significant reduction in symptoms after implant removal, but there was no objectifiable assessment of the symptoms prior to removal. The 10% wound infections reported by Backes et al. [44] after removal of material from the lower leg were not observed in our study.
The significantly shorter duration of operations in the ES group and the tendency towards a shorter period of incapacity to work after treatment by an experienced surgeon leads to expectations of cost efficiency from an economic perspective. For further proof of this assumption, subsequent studies would require an additional cost breakdown of reintegration measures and outpatient and inpatient rehabilitation.
Our study has some limitations. First is the retrospective design and the difference in group size between the ES and LES groups. Second is the lack of a uniform protocol for the evaluation of postoperative CT. The results of the present study show that the much-cited Böhler angle correlates only insufficiently with the clinical outcome. Therefore, the evaluation of the calcaneal height, arch collapse, and varus or valgus deformity of the calcaneus would be interesting in further studies.
The term “experienced surgeon” was derived from an observation of the annual fracture treatments performed on the calcaneus. The number of interventions after which this effect becomes significant should be compared in a prospective study based on the available results.
The use of the AOFAS score should be viewed critically, as it has not been validated for the German-speaking countries, and the quality of pain is of comparatively high importance. Nonetheless, the AOFAS score was used in this study because it is one of the best-known scores in literature, is used internationally, and is easily understood by patients. The Kiel Score is less common in international literature, but it has been validated for German-speaking countries and is highly specific for the injury pattern and, in the authors' view, is clearly underrepresented.
The strengths of the study are the high number of cases and the homogeneous injury pattern (AO C1-3) that were exclusively treated by means of locking compression plate via the extensile lateral approach.
Conclusion
We were able to show significant differences between the LES and ES groups especially in the clinical results. The high value of the Böhler angle as the most important radiological parameter could not be proven.
The significantly better clinical scores in ES with shorter duration of surgery, shorter time of incapacity, and lower complication rate prove the necessity to have displaced intra-articular calcaneal fractures operated upon by an experienced surgeon.
The overall low complication rate and comparably good results emphasize the need for surgical expertise and obscure the demand for minimally invasive approaches.
References
Sampath Kumar V, Marimuthu K, Subramani S et al (2014) Prospective randomized trial comparing open reduction and internal fixation with minimally invasive reduction and percutaneous fixation in managing displaced intra-articular calcaneal fractures. Int Orthop 38:2505–2512. https://doi.org/10.1007/s00264-014-2501-0
Schepers T, Patka P (2009) Treatment of displaced intra-articular calcaneal fractures by ligamentotaxis: current concepts’ review. Arch Orthop Trauma Surg 129:1677–1683. https://doi.org/10.1007/s00402-009-0915-8
Wei N, Yuwen P, Liu W et al (2017) Operative versus nonoperative treatment of displaced intra-articular calcaneal fractures: a meta-analysis of current evidence base. Medicine (Baltimore) 96:e9027. https://doi.org/10.1097/MD.0000000000009027
Zhuang L, Wang L, Xu D et al (2019) Same wound complications between extensile lateral approach and sinus tarsi approach for displaced intra-articular calcaneal fractures with the same locking compression plates fixation: a 9-year follow-up of 384 patients. Eur J Trauma Emerg Surg 17:2–9. https://doi.org/10.1007/s00068-019-01221-2
Buzzi R, Sermi N, Soviero F et al (2019) Displaced intra-articular fractures of the calcaneus: ORIF through an extended lateral approach. Injury 50(Suppl 2):S2–S7. https://doi.org/10.1016/j.injury.2019.01.037
Jansen SCP, Bransen J, van Montfort G et al (2018) Should the extended lateral approach remain part of standard treatment in displaced intra-articular calcaneal fractures? J Foot Ankle Surg 57:1120–1124. https://doi.org/10.1053/j.jfas.2018.05.015
Backes M, Spierings KE, Dingemans SA et al (2017) Evaluation and quantification of geographical differences in wound complication rates following the extended lateral approach in displaced intra-articular calcaneal fractures—a systematic review of the literature. Injury 48:2329–2335. https://doi.org/10.1016/j.injury.2017.08.015
Zwipp H, Rammelt S, Barthel S (2004) Calcaneal fractures—open reduction and internal fixation (ORIF). Injury 35(Suppl 2):SB46-54. https://doi.org/10.1016/j.injury.2004.07.011
Gusic N, Fedel I, Darabos N et al (2015) Operative treatment of intraarticular calcaneal fractures: anatomical and functional outcome of three different operative techniques. Injury 46(Suppl 6):S130–S133. https://doi.org/10.1016/j.injury.2015.10.061
Eckstein C, Kottmann T, Füchtmeier B, Müller F (2016) Long-term results of surgically treated calcaneal fractures: an analysis with a minimum follow-up period of twenty years. Int Orthop 40:365–370. https://doi.org/10.1007/s00264-015-3042-x
Pastor T, Gradl G, Klos K et al (2016) Displaced intra-articular calcaneal fractures: is there a consensus on treatment in Germany? Int Orthop 40:2181–2190. https://doi.org/10.1007/s00264-016-3134-2
Schepers T, Patka P (2008) Calcaneal nonunion: three cases and a review of the literature. Arch Orthop Trauma Surg 128:735–738. https://doi.org/10.1007/s00402-007-0516-3
Court-Brown CM, Duckworth AD, Ralston S, McQueen MM (2019) The relationship between obesity and fractures. Injury 50:1423–1428. https://doi.org/10.1016/j.injury.2019.06.016
Zhang Z, Wang Z, Zhang Y et al (2018) Risk factors for increased postoperative drainage of calcaneal fractures after open reduction and internal fixation: an observational study. Medicine (Baltimore) 97:e11818. https://doi.org/10.1097/MD.0000000000011818
Lin S, Xie J, Yao X et al (2018) The use of cryotherapy for the prevention of wound complications in the treatment of calcaneal fractures. J Foot Ankle Surg 57:436–439. https://doi.org/10.1053/j.jfas.2017.08.002
Harnroongroj T, Harnroongroj T, Suntharapa T, Arunakul M (2016) The new intra-articular calcaneal fracture classification system in term of sustentacular fragment configurations and incorporation of posterior calcaneal facet fractures with fracture components of the calcaneal body. Acta Orthop Traumatol Turc 50:519–526. https://doi.org/10.1016/j.aott.2016.08.007
Rubino R, Valderrabano V, Sutter PM, Regazzoni P (2009) Prognostic value of four classifications of calcaneal fractures. Foot Ankle Int 30:229–238. https://doi.org/10.3113/FAI.2009.0229
Beerekamp MSH, Backes M, Schep NWL et al (2017) Effects of intra-operative fluoroscopic 3D-imaging on peri-operative imaging strategy in calcaneal fracture surgery. Arch Orthop Trauma Surg 137:1667–1675. https://doi.org/10.1007/s00402-017-2787-7
Eckardt H, Lind M (2015) Effect of intraoperative three-dimensional imaging during the reduction and fixation of displaced calcaneal fractures on articular congruence and implant fixation. Foot Ankle Int 36:764–773. https://doi.org/10.1177/1071100715576518
Gupta A, Ghalambor N, Nihal A, Trepman E (2003) The modified Palmer lateral approach for calcaneal fractures: wound healing and postoperative computed tomographic evaluation of fracture reduction. Foot Ankle Int 24:744–753. https://doi.org/10.1177/107110070302401003
Yang C, Xu X, Zhu Y et al (2016) A long-term study of the effect of subtalar arthrodesis on the ankle and hindfoot joints. J Am Podiatr Med Assoc 106:47–53. https://doi.org/10.7547/14-002
Sanders R, Fortin P, DiPasquale T, Walling A (1993) Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-199305000-00012
Ahn J, Kim TY, Kim TW, Jeong BO (2019) Learning curve for open reduction and internal fixation of displaced intra-articular calcaneal fracture by extensile lateral approach using the cumulative summation control chart. Foot Ankle Int 40:1052–1059. https://doi.org/10.1177/1071100719850149
Rammelt S, Sangeorzan BJ, Swords MP (2018) Calcaneal fractures—should we or should we not operate? Indian J Orthop 52:220–230. https://doi.org/10.4103/ortho.IJOrtho_555_17
Persson J, Peters S, Haddadin S et al (2015) The prognostic value of radiologic parameters for long-term outcome assessment after an isolated unilateral calcaneus fracture. Technol Health Care 23:285–298. https://doi.org/10.3233/THC-140890
Beerekamp MSH, Luitse JSK, Ubbink DT et al (2013) Evaluation of reduction and fixation of calcaneal fractures: a Delphi consensus. Arch Orthop Trauma Surg 133:1377–1384. https://doi.org/10.1007/s00402-013-1823-5
de Muinck Keizer RJO, Beerekamp MSH, Ubbink DT et al (2017) Systematic CT evaluation of reduction and hardware positioning of surgically treated calcaneal fractures: a reliability analysis. Arch Orthop Trauma Surg 137:1261–1267. https://doi.org/10.1007/s00402-017-2744-5
Zwipp H, Rammelt S, Amlang M et al (2013) Operative treatment of displaced intra-articular calcaneal fractures. Oper Orthop Traumatol 25:554–568. https://doi.org/10.1007/s00064-013-0246-3
De Groot R, Frima AJ, Schepers T, Roerdink WH (2013) Complications following the extended lateral approach for calcaneal fractures do not influence mid- to long-term outcome. Injury 44:1596–1600. https://doi.org/10.1016/j.injury.2013.06.014
Li S (2018) Wound and sural nerve complications of the sinus tarsi approach for calcaneus fractures. Foot Ankle Int 39:1106–1112. https://doi.org/10.1177/1071100718774808
Backes M, Schepers T, Beerekamp MSH et al (2014) Wound infections following open reduction and internal fixation of calcaneal fractures with an extended lateral approach. Int Orthop 38:767–773. https://doi.org/10.1007/s00264-013-2181-1
Backes M, Spijkerman IJ, de Muinck-Keizer R-JO et al (2018) Determination of pathogens in postoperative wound infection after surgically reduced calcaneal fractures and implications for prophylaxis and treatment. J Foot Ankle Surg 57:100–103. https://doi.org/10.1053/j.jfas.2017.08.016
Backes M, Schep NWL, Luitse JSK et al (2015) The effect of postoperative wound infections on functional outcome following intra-articular calcaneal fractures. Arch Orthop Trauma Surg 135:1045–1052. https://doi.org/10.1007/s00402-015-2219-5
Yao H, Lu H, Zhao H et al (2017) Open reduction assisted with an external fixator and internal fixation with calcaneal locking plate for intra-articular calcaneal fractures. Foot Ankle Int 38:1107–1114. https://doi.org/10.1177/1071100717715908
Fascione F, Di Mauro M, Guelfi M et al (2019) Surgical treatment of displaced intraarticular calcaneal fractures by a minimally invasive technique using a locking nail: a preliminary study. Foot Ankle Surg 25:679–683. https://doi.org/10.1016/j.fas.2018.08.004
Spierings KE, Min M, Nooijen LE et al (2019) Managing the open calcaneal fracture: a systematic review. Foot Ankle Surg 25:707–713. https://doi.org/10.1016/j.fas.2018.10.005
Lin J, Xie C, Chen K et al (2019) Comparison of sinus tarsi approach versus extensile lateral approach for displaced intra-articular calcaneal fractures Sanders type IV. Int Orthop 43:2141–2149. https://doi.org/10.1007/s00264-019-04318-w
Park J, Che JH (2017) The sinus tarsi approach in displaced intra-articular calcaneal fractures. Arch Orthop Trauma Surg 137:1055–1065. https://doi.org/10.1007/s00402-017-2714-y
van der Vliet QMJ, Hietbrink F, Casari F et al (2018) Factors influencing functional outcomes of subtalar fusion for posttraumatic arthritis after calcaneal fracture. Foot Ankle Int 39:1062–1069. https://doi.org/10.1177/1071100718777492
Backes M, Dorr MC, Luitse JSK et al (2016) Predicting loss of height in surgically treated displaced intra-articular fractures of the calcaneus. Int Orthop 40:513–518. https://doi.org/10.1007/s00264-015-2982-5
Zeman J, Matějka T, Zeman P et al (2019) Outcomes of treatment of calcaneal fractures using locking compression plate with or without augmentation. Acta Chir Orthop Traumatol Cech 86:413–418
Soni A, Vollans S, Malhotra K, Mann C (2014) Association between smoking and wound infection rates following calcaneal fracture fixation. Foot Ankle Spec 7:266–270. https://doi.org/10.1177/1938640014537301
Backes M, Dingemans SA, Dijkgraaf MGW et al (2017) Effect of antibiotic prophylaxis on surgical site infections following removal of orthopedic implants used for treatment of foot, ankle, and lower leg fractures: a randomized clinical trial. JAMA 318:2438–2445. https://doi.org/10.1001/jama.2017.19343
Backes M, Dingemans SA, Schep NWL et al (2015) Wound infections following implant removal below the knee: the effect of antibiotic prophylaxis; the WIFI-trial, a multi-centre randomized controlled trial. BMC Surg 15:12–16. https://doi.org/10.1186/1471-2482-15-12
Acknowledgements
We thank OPED© for providing the survey platform for data collection. A separate declaration was issued.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fischer, S., Meinert, M., Neun, O. et al. Surgical experience as a decisive factor for the outcome of calcaneal fractures using locking compression plate: results of 3 years. Arch Orthop Trauma Surg 141, 1691–1699 (2021). https://doi.org/10.1007/s00402-020-03649-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03649-3