Abstract
MicroRNAs (miRNAs) are small noncoding RNAs, which play a complex role in posttranscriptional gene expression and can theoretically be used as a diagnostic or prognostic tool, or therapeutic target for neoplasia. Despite advances in the diagnosis and treatment of skeletal sarcomas, including osteosarcoma and chondrosarcoma, much remains unknown regarding their underpinning molecular mechanisms. Given the recent increasing knowledge base of miRNA roles in neoplasia, both as oncogenes and tumor suppressor genes, this review will focus on the available literature regarding the expression profiles and potential roles of miRNA in skeletal sarcomas. Although this is an emerging field, miRNA profiling may be of use in clarifying competing diagnoses of skeletal sarcomas and possibly indicate patient risk of resistance to traditional chemotherapeutic agents. While detecting and targeting miRNAs is currently limited to experimental investigations, miRNA may be utilized for future clinical management of skeletal sarcomas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
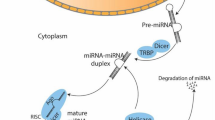
Small noncoding RNAs, such as microRNAs (miRNA), are 21–25 nucleotides in length and since their discovery in 1993 have emerged as disease-associated biomarkers. MiRNAs are stable in biological fluids and thus, in theory, represent good targets for diagnostic and prognostic assays. Detection of miRNA polymorphisms and miRNA variants has been identified in patients with a predisposition to cancer development [1]. MiRNAs are well established as regulators of tumorigenesis and have different stages of expression during neoplasia. MiRNA is generated from long primary RNA polymerase II-derived transcripts through two processing reactions: nuclear Drosha cleavage and cytoplasmic Dicer cleavage, which forms mature miRNA [2]. Broadly, they control gene expression by binding to the 3′ untranslated region of target messenger RNAs (mRNAs) resulting in changes such as mRNA destabilization or translational repression. Recent studies have found the mechanism to be localized during the initiation step of mRNA translation. See [2] for an in-depth review of miRNA processing and regulation.
MiRNA expression can be altered in malignancy and plays a significant role in tumor progression, including tumorigenesis, invasion, metastasis and angiogenesis. Depending on its method of action toward a targeted protein, miRNAs may act as oncogenes when overexpressed or upregulate oncogenes by downregulating tumor suppressor genes [3]. The increasing importance of understanding the functional significance of miRNAs has made its role in gene expression a well-studied field (Tables 1, 2). Additionally, miRNAs may be tissue specific and thus have the potential to serve as unique identifiers of tumor type and origin [4]. In addition, miRNA polymorphisms have strong implications in understanding the prognosis and progression of disease. MiRNA polymorphisms can include SNPs, chromosomal variation and epigenetic defects that may interfere with miRNA-mediated regulation and can be found not only in the miRNA target gene, but also in primary, precursor and mature miRNA sequences as well as the genes involved in miRNA biogenesis and miRNA promoters [5].
Osteosarcoma (OS) is a leading cause of cancer-related death in adolescents, most commonly arising in the metaphyses of long bones [6]. The histologic appearance of OS can be quite diverse, including various lineages of differentiation and unusual variants (Fig. 1). Nevertheless, OS is a very aggressive tumor, which left untreated is universally fatal. With modern multimodal treatment, the 5-year survival rate of OS patients has improved to 60–70 % [7, 8]. However, for patients with metastatic disease outcomes remain poor [7, 8]. Deregulation of miRNA sequences has been recognized to have a role in osteosarcomagenesis. The implications for treatment, prognosis and the basic biology of OS will be discussed below as well as a comparison to chondrosarcoma (the second most common primary bone malignancy).
Histopathologic diversity of osteosarcoma. Although the majority of osteosarcoma variants have a similar prognosis, OS tumors have significant anatomic and histologic diversity. a Typical appearance of osteoblastic OS, with filigree type neoplastic bone. b Typical appearance of chondroblastic OS, with large areas of predominant chondroid matrix. c Typical appearance of fibroblastic OS, often demonstrating large areas of fibroblastic differentiation with inconspicuous osteoid. d Giant cell-rich OS, an unusual histologic appearance with numerous giant cells. e Parosteal OS, demonstrating typical dual fibro-osseous differentiation. f Telangiectatic OS, demonstrating areas of hemorrhage, fibrin and markedly pleomorphic tumor cells
MiRNA and the tumor suppressor p53 in osteosarcoma
The p53 tumor suppressor lies at the nexus of cellular pathways that sense DNA damage, cellular stress and improper cell proliferation (see [9] for a review). Sporadic osteosarcoma demonstrates deletions or loss of heterozygosity in the p53 locus (17p13.1) in ~40 % of tumors [10–12]. Moreover, p53 heterozygote mice are well known to spontaneously develop OS in ~25 % of cases (see [13] for a review). He et al. [14] identified the miR-34 family as direct transcriptional targets of p53, via the use of p53-deficient cell types. Moreover, they found that ectopic expression of miR-34 induces cell cycle arrest across primary tumor cells and cell lines. Concordant with this, miR-34 downregulates a group of genes associated with the promotion of cell cycle progression. Collectively, these findings indicated that the miR-34 family acts as tumor suppressors in concert with p53 [14]. See also [15, 16] for a more detailed discussion of the miR-34 family in cancer development.
Another investigator examined the specific function of miR-34s in OS cell biology [17]. Here, He et al. examined the expression of miR-34 in 117 primary osteosarcoma samples and the in vitro roles of miR-34. Consistent with its presumed role as a tumor suppressor, miR-34 expression was decreased across tumor samples, although minimal deletions or epigenetic inactivations were observed. Consistent with the known induction of miR-34 expression by p53, those OS cell lines without p53 expression did not show miR-34 induction in the context of genotoxic stress (such as the p53 null SAOS2 cell line). Moreover, miR-34 target gene expression appeared to be partially dependent on p53 expression. Finally, miR-34 was found to induce cell cycle arrest in OS cells in vitro [17]. Thus, the miR-34 appears to have tumor suppressor properties in OS as well as other malignancies, in accordance with p53.
MiRNA and oncogenes in osteosarcoma
Another area of importance in miRNA regulation is the expression of oncogenes, which may affect tumor progression and the metastatic dissemination of sarcoma cells. Many osteosarcoma miRNAs regulate transcription factors that have been identified as inducers of pro- or anti-metastasis in steps of metastatic dissemination by the gain of migratory capacity and invasiveness or angiogenesis and resistance to apoptosis. The transcription factor TWIST promotes cell migration and invasion in synovial sarcoma and OS patients with resistance to chemotherapy [18, 19]. TWIST has been found to decrease OS cell survival against cisplatin by inhibition of the β-catenin and endothelin-1/endothelin-A receptor pathways [20, 21]. Zhou et al. [18] found that miR-33a correlated with clinical progression of OS, via downregulation of TWIST and reduced cisplatin-induced OS cell apoptosis in vitro.
MiRNA oncogenes have also been differentially expressed in OS as compared to other malignancies. Among these, using miRNA expression profiling of human OS cells, Maire et al. [22] found that miR-126 is overexpressed in human OS specimens. miR-126 has been reported to repress SPRED-1 (Sprouty-related, EVH1 domain-containing protein-1) expression, an inhibitor of MAPK (mitogen-activated protein kinase) signaling, and stimulate VEGF (vascular endothelial growth factor)-induced angiogenesis, thereby enhancing cell migration, proliferation and survival [23]. Other miRNAs known to have inhibitory effects on VEGF expression were conversely found to be downregulated among human OS samples [24, 25]. For example, miR-410 and miR-29b, known to repress VEGF expression [26], were downregulated in OS [24, 25]. In line with these observations, forced overexpression of either miR-140 or miR-29b led to reduced VEGF expression in SAOS-2 and MG-63 OS cell lines [24, 25]. Therefore, miRNAs may have a role not only in initiation of tumorigenesis but also in tumor vascularity and metastatic spread.
BCL-2 (B cell lymphoma 2) is a proto-oncogene that regulates the apoptosis pathway and increases survival by increasing resistance to apoptosis [27]. Multiple miRNAs have been found to regulate BCL-2 expression in osteosarcoma as well as other neoplasms; however, BCL-2 expression alone has not been found to correlate with osteosarcoma prognosis [28, 29]. The miR-16 family (miR-16 and miR-195) has been found to target BCL-2, and reduced expression of these miRNA correlates with resistance to chemotherapy [30, 31]. Other tumor suppressors of BCL-2 include miR-143, which was downregulated in OS cells lines and primary tumor samples, where BCL-2 was found to be the direct target of miR-143. When miR-143 expression was restored in MG-63 and U2OS OS cell lines, investigators found that the anti-tumorigenic effect of miR143 was validated in vitro through reduction in cell viability, promotion of cell apoptosis and tumor suppression [32].
MiRNA expression in osteosarcoma versus chondrosarcoma
Chondrosarcoma is the second most common primary malignant tumor of the bone. Unlike OS, chondrosarcoma is a malignancy of adulthood and older age and occurs most commonly in the pelvis (although any bone formed by endochondral ossification may be involved) [33]. Much like OS, differential expression and regulation of miRNA in chondrosarcoma is an area of recent investigation [34]. Studies have identified multiple similarities in the expression profiles of miRNA in chondrosarcoma and OS (summarized in Table 3). Probably the best example is the tumor suppressor miR-100, which is downregulated in both chondrosarcoma and OS tumors. This was determined from both primary human tissues of chondrosarcoma [35] and OS [36, 37], as well as multiple chondrosarcoma cell lines including SW1353 and OUMS-27 [38]. In addition, the forced downregulation of miR-100 was found to result in highly aggressive cell lines and cisplatin resistance, in vitro using cisplatin-resistant chondrocyte clones (CDDP CR1, CR2 and CDDP RP) [35] and in OS cell lines (HOS, MHM, OHS and OSA) [37]. In aggregate, miR-100 seems to have similar functional properties in OS and chondrosarcoma biology, although the secondary molecular mechanisms are not well understood. In fact, miR-100 may have tumor suppressor properties in various carcinomas as well, as low miR-100 expression has been observed to be a negative prognostic factor across breast, pancreatic and esophageal carcinomas [39–41]. Multiple other miRNAs are similarly dysregulated between chondrosarcoma and OS, including miR-134, miR-377 and miR-497 [38, 42–44]. However, their functional significance and/or distinct targets of gene expression have not been well defined.
Interestingly, several miRNAs show distinct transcriptional targets or even dichotomous changes between chondrosarcoma and OS. For example, even though miR-145 is upregulated in both chondrosarcoma and OS specimens, the target genes for the miR-145 are distinct. In chondrosarcoma cells, low miR-145 expression is associated with decreased SOX9 transcription, the major transcription factor associated with chondrogenic differentiation [45]. In OS cells, miR-145 expression was found to inversely regulate the gene ROCK1, an important activator of tumor cell motility [46–48]. This difference in regulation demonstrates that individual miRNA has multiple targets and how the impact of miRNA dysregulation may be tissue or tumor type specific [49]. Expression of miR-221 is another example of differences between OS and chondrosarcoma miRNA expression. miR-221 is a negative regulator of PTEN and the PI3K/AKT cell survival pathway and has been shown to be upregulated in OS [50] as well as carcinomas [51, 52], but downregulated in chondrosarcoma [38]. The significance of this difference in miR-221 expression profiles is not fully understood. However, it is important to note that both OS and chondrosarcoma exist as a spectrum from low-grade to high-grade sarcomas and have a large range of histologic appearances. Unfortunately in the available current studies, most sample sizes are too small to realistically take into account this diversity in tumor grade and subtype. Further research is needed to expand upon and verify these initial observations.
MiRNA as diagnostic and prognostic tool for osteosarcoma
As mentioned, miRNAs are relatively stable and may be analyzed in tissue, fluid or even paraffin-embedded samples [53, 54]. Thus, they represent attractive targets for diagnostic and prognostic assays. Differential expression of related miRNAs has been proposed as helpful in the diagnosis of certain malignancies, such as carcinoma versus lymphoma [22]. While miRNA detection may be of future utility in the diagnosis of skeletal sarcomas, this has not yet been born out in the scientific literature. In terms of prognostication of OS, various miRNA expressions have been found to regulate resistance to chemotherapeutic agents [18, 20, 21, 35, 50]. For example, overexpression of miR-140 in OS xenografts led to resistance to antifolates and fluoropyrimidine-based compounds [55]. MiR-140-induced chemoresistance was found to be caused by the regulation of HDAC4, which is involved in cell proliferation through decreased S phase and increased cell cycle arrest [55]. Additionally, overexpression of miR-503 and underexpression of miR-451 and miR-195 correlate with a poor response to chemotherapy and unfavorable prognosis in OS patients [56–58]. These initial associations between miRNA dysregulation and chemoresistance may be the introduction into more customized chemotherapeutic protocols for OS patients.
Future directions in the study of miRNA and skeletal sarcomas
MiRNA shows widespread dysregulation in skeletal sarcomas, including OS and chondrosarcoma. While not discussed here, Ewing’s sarcoma also demonstrates a unique miRNA profile [59, 60]. Although still in its relative early stages, miRNA profiling may be of utility in the diagnosis of skeletal sarcomas versus competing diagnoses, as well as to identify individuals at risk for resistance to traditional chemotherapeutic agents. While detecting and targeting miRNAs is still limited to early scientific investigations, it may well find its way into the future clinical management of skeletal sarcomas.
References
Lovat F, Valeri N, Croce CM. MicroRNAs in the pathogenesis of cancer. Semin Oncol. 2011;38(6):724–33.
Yates LA, Norbury CJ, Gilbert RJ. The long and short of microRNA. Cell. 2013;153(3):516–9.
Sassen S, Miska EA, Caldas C. MicroRNA: implications for cancer. Virchows Arch. 2008;452(1):1–10.
Mishra PJ, Merlino G. MicroRNA reexpression as differentiation therapy in cancer. J Clin Invest. 2009;119(8):2119–23.
Mishra PJ. The miRNA-drug resistance connection: a new era of personalized medicine using noncoding RNA begins. Pharmacogenomics. 2012;13(12):1321–4.
Ottaviani G, Jaffe N. The epidemiology of osteosarcoma. Cancer Treat Res. 2009;152:3–13.
Rytting M, et al. Osteosarcoma in preadolescent patients. Clin Orthop Relat Res. 2000;373:39–50.
Ferguson WS, Goorin AM. Current treatment of osteosarcoma. Cancer Invest. 2001;19(3):292–315.
Levine AJ, Hu W, Feng Z. The P53 pathway: what questions remain to be explored? Cell Death Differ. 2006;13(6):1027–36.
Lau CC, et al. Frequent amplification and rearrangement of chromosomal bands 6p12-p21 and 17p11.2 in osteosarcoma. Genes Chromosomes Cancer. 2004;39(1):11–21.
Ognjanovic S, et al. Sarcomas in TP53 germline mutation carriers: a review of the IARC TP53 database. Cancer. 2012;118(5):1387–96.
Tsuchiya T, et al. Analysis of the p16INK4, p14ARF, p15, TP53, and MDM2 genes and their prognostic implications in osteosarcoma and Ewing sarcoma. Cancer Genet Cytogenet. 2000;120(2):91–8.
Jacks T, et al. Tumor spectrum analysis in p53-mutant mice. Curr Biol. 1994;4(1):1–7.
He L, et al. A microRNA component of the p53 tumour suppressor network. Nature. 2007;447(7148):1130–4.
Hermeking H. The miR-34 family in cancer and apoptosis. Cell Death Differ. 2010;17(2):193–9.
Chen F, Hu SJ. Effect of microRNA-34a in cell cycle, differentiation, and apoptosis: a review. J Biochem Mol Toxicol. 2012;26(2):79–86.
He C, et al. Functional elucidation of MiR-34 in osteosarcoma cells and primary tumor samples. Biochem Biophys Res Commun. 2009;388(1):35–40.
Zhou Y, et al. miR-33a is up-regulated in chemoresistant osteosarcoma and promotes osteosarcoma cell resistance to cisplatin by down-regulating TWIST. J Exp Clin Cancer Res. 2014;33:12.
Lee KW, et al. Twist1 is essential in maintaining mesenchymal state and tumor-initiating properties in synovial sarcoma. Cancer Lett. 2014;343(1):62–73.
Wu J, et al. TWIST interacts with β-catenin signaling on osteosarcoma cell survival against cisplatin. Mol Carcinog. 2014;53(6):440–6.
Zhou Y, et al. TWIST interacts with endothelin-1/endothelin A receptor signaling in osteosarcoma cell survival against cisplatin. Oncol Lett. 2013;5(3):857–61.
Maire G, et al. Analysis of miRNA-gene expression-genomic profiles reveals complex mechanisms of microRNA deregulation in osteosarcoma. Cancer Genet. 2011;204(3):138–46.
Wang S, et al. The endothelial-specific microRNA miR-126 governs vascular integrity and angiogenesis. Dev Cell. 2008;15(2):261–71.
Zhang K, et al. A key role of microRNA-29b in suppression of osteosarcoma cell proliferation and migration via modulation of VEGF. Int J Clin Exp Pathol. 2014;7(9):5701–8.
Zhao D, et al. VEGF-mediated suppression of cell proliferation and invasion by miR-410 in osteosarcoma. Mol Cell Biochem. 2015;400(1–2):87–95.
Kwiecinski M, et al. Expression of platelet-derived growth factor-C and insulin-like growth factor I in hepatic stellate cells is inhibited by miR-29. Lab Invest. 2012;92(7):978–87.
Czabotar PE, et al. Control of apoptosis by the BCL-2 protein family: implications for physiology and therapy. Nat Rev Mol Cell Biol. 2014;15(1):49–63.
Trieb K, Sulzbacher I, Kubista B. Bcl-2 correlates with localization but not outcome in human osteosarcoma. Oncol Lett. 2013;6(2):559–61.
Nedelcu T, et al. Livin and Bcl-2 expression in high-grade osteosarcoma. J Cancer Res Clin Oncol. 2008;134(2):237–44.
Aqeilan RI, Calin GA, Croce CM. miR-15a and miR-16-1 in cancer: discovery, function and future perspectives. Cell Death Differ. 2010;17(2):215–20.
Xia L, et al. miR-15b and miR-16 modulate multidrug resistance by targeting BCL2 in human gastric cancer cells. Int J Cancer. 2008;123(2):372–9.
Zhang H, et al. microRNA-143, down-regulated in osteosarcoma, promotes apoptosis and suppresses tumorigenicity by targeting Bcl-2. Oncol Rep. 2010;24(5):1363–9.
Fletcher C, Unni KK, Mertens F. World Health Organization classification of tumors. Lyon: IARC Press; 2002.
Rozeman LB, Cleton-Jansen AM, Hogendoorn PC. Pathology of primary malignant bone and cartilage tumours. Int Orthop. 2006;30(6):437–44.
Zhu Z, et al. MicroRNA-100 resensitizes resistant chondrosarcoma cells to cisplatin through direct targeting of mTOR. Asian Pac J Cancer Prev. 2014;15(2):917–23.
Huang J, et al. MicroRNA-100 inhibits osteosarcoma cell proliferation by targeting Cyr61. Tumour Biol. 2014;35(2):1095–100.
Lauvrak SU, et al. Functional characterisation of osteosarcoma cell lines and identification of mRNAs and miRNAs associated with aggressive cancer phenotypes. Br J Cancer. 2013;109(8):2228–36.
Yoshitaka T, et al. Analysis of microRNAs expressions in chondrosarcoma. J Orthop Res. 2013;31(12):1992–8.
Petrelli A, et al. By promoting cell differentiation, miR-100 sensitizes basal-like breast cancer stem cells to hormonal therapy. Oncotarget. 2015;6(4):2315–30.
Li Z, et al. MicroRNA-100 regulates pancreatic cancer cells growth and sensitivity to chemotherapy through targeting FGFR3. Tumour Biol. 2014;35(12):11751–9.
Zhou S, et al. Prognostic value of microRNA-100 in esophageal squamous cell carcinoma. J Surg Res. 2014;192(2):515–20.
Sarver AL, et al. MicroRNAs at the human 14q32 locus have prognostic significance in osteosarcoma. Orphanet J Rare Dis. 2013;8:7.
Wang L, et al. microRNA-377 suppresses the proliferation of human osteosarcoma MG-63 cells by targeting CDK6. Tumour Biol. 2015. doi:10.1007/s13277-014-3034-2.
Namløs HM, et al. Modulation of the osteosarcoma expression phenotype by microRNAs. PLoS ONE. 2012;7(10):e48086.
Mak IW, et al. The epigenetic regulation of SOX9 by miR-145 in human chondrosarcoma. J Cell Biochem. 2015;116(1):37–44.
Lei P, et al. microRNA-145 inhibits osteosarcoma cell proliferation and invasion by targeting ROCK1. Mol Med Rep. 2014;10(1):155–60.
Li E, et al. MiR-145 inhibits osteosarcoma cells proliferation and invasion by targeting ROCK1. Tumour Biol. 2014;35(8):7645–50.
Lochhead PA, et al. Activating ROCK1 somatic mutations in human cancer. Oncogene. 2010;29(17):2591–8.
Selbach M, et al. Widespread changes in protein synthesis induced by microRNAs. Nature. 2008;455(7209):58–63.
Zhao G, et al. MicroRNA-221 induces cell survival and cisplatin resistance through PI3K/Akt pathway in human osteosarcoma. PLoS ONE. 2013;8(1):e53906.
Chun-Zhi Z, et al. MicroRNA-221 and microRNA-222 regulate gastric carcinoma cell proliferation and radioresistance by targeting PTEN. BMC Cancer. 2010;10:367.
Galardi S, et al. miR-221 and miR-222 expression affects the proliferation potential of human prostate carcinoma cell lines by targeting p27Kip1. J Biol Chem. 2007;282(32):23716–24.
Lim LP, et al. Microarray analysis shows that some microRNAs downregulate large numbers of target mRNAs. Nature. 2005;433(7027):769–73.
Tang F, et al. MicroRNA expression profiling of single whole embryonic stem cells. Nucleic Acids Res. 2006;34(2):e9.
Song B, et al. Mechanism of chemoresistance mediated by miR-140 in human osteosarcoma and colon cancer cells. Oncogene. 2009;28(46):4065–74.
Yuan J, et al. The expression and function of miRNA-451 in osteosarcoma. Med Oncol. 2015;32(1):324.
Chong Y, et al. MicroRNA-503 acts as a tumor suppressor in osteosarcoma by targeting L1CAM. PLoS ONE. 2014;9(12):e114585.
Cai H, et al. Serum miR-195 is a diagnostic and prognostic marker for osteosarcoma. J Surg Res. 2014;194(2):505–10.
Dylla L, Moore C, Jedlicka P. MicroRNAs in Ewing sarcoma. Front Oncol. 2013;3:65.
Karnuth B, et al. Differentially expressed miRNAs in Ewing sarcoma compared to mesenchymal stem cells: low miR-31 expression with effects on proliferation and invasion. PLoS ONE. 2014;9(3):e93067.
Hu H, et al. Changes in microRNA expression in the MG-63 osteosarcoma cell line compared with osteoblasts. Oncol Lett. 2012;4(5):1037–42.
Gao Y, et al. miR-17 inhibitor suppressed osteosarcoma tumor growth and metastasis via increasing PTEN expression. Biochem Biophys Res Commun. 2014;444(2):230–4.
Li X, et al. MicroRNA-19b targets Mfn1 to inhibit Mfn1-induced apoptosis in osteosarcoma cells. Neoplasma. 2014;61(3):265–73.
Wang XH, et al. microRNA-25 promotes osteosarcoma cell proliferation by targeting the cell-cycle inhibitor p27. Mol Med Rep. 2014;10(2):855–9.
Montanini L, et al. MicroRNA cloning and sequencing in osteosarcoma cell lines: differential role of miR-93. Cell Oncol (Dordr). 2012;35(1):29–41.
Pei H, et al. MiR-135b promotes proliferation and invasion of osteosarcoma cells via targeting FOXO1. Mol Cell Biochem. 2015;400(1–2):245–52.
Lulla RR, et al. Identification of differentially expressed MicroRNAs in osteosarcoma. Sarcoma. 2011;2011:732690.
Won KY, et al. MicroRNA-199b-5p is involved in the Notch signaling pathway in osteosarcoma. Hum Pathol. 2013;44(8):1648–55.
Cai H, et al. Prognostic evaluation of microRNA-210 expression in pediatric osteosarcoma. Med Oncol. 2013;30(2):499.
Wang X, et al. MicroRNA-214 regulates osteosarcoma survival and growth by directly targeting phosphatase and tensin homolog. Mol Med Rep. 2014;10(6):3073–9.
Xu Z, Wang T. miR-214 promotes the proliferation and invasion of osteosarcoma cells through direct suppression of LZTS1. Biochem Biophys Res Commun. 2014;449(2):190–5.
Li H, et al. miR-542-3p overexpression is associated with enhanced osteosarcoma cell proliferation and migration ability by targeting Van Gogh-like 2. Mol Med Rep. 2015;11(2):851–6.
Guo S, et al. miR-22 inhibits osteosarcoma cell proliferation and migration by targeting HMGB1 and inhibiting HMGB1-mediated autophagy. Tumour Biol. 2014;35(7):7025–34.
Wang G, et al. miR-23a suppresses proliferation of osteosarcoma cells by targeting SATB1. Tumour Biol. 2015. doi:10.1007/s13277-015-3120-0.
Zhang W, et al. The microRNA-29 plays a central role in osteosarcoma pathogenesis and progression. Mol Biol (Mosk). 2012;46(4):622–7.
Di Fiore R, et al. MicroRNA-29b-1 impairs in vitro cell proliferation, self-renewal and chemoresistance of human osteosarcoma 3AB-OS cancer stem cells. Int J Oncol. 2014;45(5):2013–23.
Xu JQ, et al. MicroRNA-32 inhibits osteosarcoma cell proliferation and invasion by targeting Sox9. Tumour Biol. 2014;35(10):9847–53.
Xu N, et al. MicroRNA-33b suppresses migration and invasion by targeting c-Myc in osteosarcoma cells. PLoS ONE. 2014;9(12):e115300.
Lv H, et al. A polymorphism site in the pre-miR-34a coding region reduces miR-34a expression and promotes osteosarcoma cell proliferation and migration. Mol Med Rep. 2014;10(6):2912–6.
Tian Y, Zhang YZ, Chen W. MicroRNA-199a-3p and microRNA-34a regulate apoptosis in human osteosarcoma cells. Biosci Rep. 2014;34(4):479.
Liu Z, et al. The tumor-suppressive microRNA-135b targets c-myc in osteosarcoma. PLoS ONE. 2014;9(7):e102621.
Osaki M, et al. MicroRNA-143 regulates human osteosarcoma metastasis by regulating matrix metalloprotease-13 expression. Mol Ther. 2011;19(6):1123–30.
Zhao M, et al. The downregulation of miR-144 is associated with the growth and invasion of osteosarcoma cells through the regulation of TAGLN expression. Int J Mol Med. 2014;34(6):1565–72.
Duan Z, et al. MicroRNA-199a-3p is downregulated in human osteosarcoma and regulates cell proliferation and migration. Mol Cancer Ther. 2011;10(8):1337–45.
Sun Z, et al. miR-202 suppresses proliferation and induces apoptosis of osteosarcoma cells by downregulating Gli2. Mol Cell Biochem. 2014;397(1–2):277–83.
Luo XJ, et al. MicroRNA-212 inhibits osteosarcoma cells proliferation and invasion by down-regulation of Sox4. Cell Physiol Biochem. 2014;34(6):2180–8.
Shen L, et al. MicroRNA-217 regulates WASF3 expression and suppresses tumor growth and metastasis in osteosarcoma. PLoS ONE. 2014;9(10):e109138.
Zhang H, et al. Prognostic value of microRNA-223/epithelial cell transforming sequence 2 signaling in patients with osteosarcoma. Hum Pathol. 2014;45(7):1430–6.
Xu M, et al. miR-382 inhibits tumor growth and enhance chemosensitivity in osteosarcoma. Oncotarget. 2014;5(19):9472–83.
Sun XH, et al. miRNA-646 suppresses osteosarcoma cell metastasis by downregulating fibroblast growth factor 2 (FGF2). Tumour Biol. 2014;36(3):2127–34.
Xu H, Liu X, Zhao J. Down-regulation of miR-3928 promoted osteosarcoma growth. Cell Physiol Biochem. 2014;33(5):1547–56.
Poos K, et al. How microRNA and transcription factor co-regulatory networks affect osteosarcoma cell proliferation. PLoS Comput Biol. 2013;9(8):e1003210.
Wang Y, Zhao W, Fu Q. miR-335 suppresses migration and invasion by targeting ROCK1 in osteosarcoma cells. Mol Cell Biochem. 2013;384(1–2):105–11.
Acknowledgments
The present work was supported by the UCLA Department of Pathology and Laboratory Medicine, the Translational Research Fund and the UCLA Daljit S. and Elaine Sarkaria Fellowship award. The authors thank the staff of UCLA Translational Pathology Core Laboratory and A.S. James for their excellent technical assistance.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chang, L., Shrestha, S., LaChaud, G. et al. Review of microRNA in osteosarcoma and chondrosarcoma. Med Oncol 32, 172 (2015). https://doi.org/10.1007/s12032-015-0613-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-015-0613-z