Abstract
Recent data strongly suggest the important role of miRNAs in various cancer-related processes. Osteosarcoma (OS) is the most common primary cancer of the bone and usually leads to deaths due to its rapid proliferation and metastasis. Here, we demonstrated that compared with noncancerous bone tissues, miR-135b expression is frequently upregulated in OS specimens, inversely correlated with potential target-FOXO1 expression pattern. Bioinformatics analysis combined with experimental confirmation revealed FOXO1 is a direct target of miR-135b in OS. Functionally, miR-135b inhibitor significantly inhibited OS cells proliferation and invasion. Forced expression of FOXO1 showed the opposite effect, and FOXO1 knockdown abolished the effect of miR-135b inhibitor. Taken together, our data provide compelling evidence that miR-135b functions as an onco-miRNA in OS to promote OS cells proliferation and invasion, and its oncogenic effects are mediated chiefly through targeting FOXO1.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteosarcoma (OS) is the most common malignant primary bone tumor in children and adolescents with about 75 % patients between 15 and 25 years old, and it has a predilection for the metaphyseal portions of the long bone, with the distal femur and proximal tibia accounting for 50 % of all cases [1]. OS is locally destructive and has a high metastatic potential, primarily to the lung. Despite the rapid development of treatment strategies, curing OS patients is still difficult [2]. Due to the combined use of anti-OS drugs, the 5-year survival rate in patients with localized OS reached about 70 %. However, patients with metastatic or recurrent OS have a <20 % chance of long-term survival despite aggressive therapies. These situations have changed little in the past 30 years [3]. Therefore, it is necessary to investigate the fundamental molecular mechanisms that underlie the histological heterogeneity, drug resistance, and metastasis to identify novel markers for the diagnosis, prognosis, and treatment of patients with OS.
miRNAs (microRNA) are a family of small, single strand, non-coding, endogenous RNA molecules that post-transcriptionally regulate target gene expression by binding to the 3′-untranslated region (3′UTR) of target messenger RNA (mRNA), mainly leading to translational repression or target mRNA degradation [4]. Growing evidence has suggested that miRNAs play important roles in many physiology and pathophysiology processes, including development, proliferation, differentiation, apoptosis, migration, and invasion, especially in carcinogenesis. MiRNAs can function as both tumor suppressors and tumor promoters because of the diversity of miRNAs themselves [5]. The aberrant expression of specific miRNAs has been found to be associated with the development and clinical outcomes of various cancers, but deregulated miRNAs and their roles in tumorigenesis are still largely unknown [6]. In regard to OS, although, there are also several reports suggested the involvement of miRNAs in OS, such as miR-34a [7], miR-183 [8], and miR-132 [9], the roles of miRNAs in OS are far from full understanding. In the present study, we found miR-135b was upregulated in primary tumor samples. Inhibition of miR-135b expression significantly inhibited proliferation and invasion of OS cells, and this effect is mainly mediated via directly targeting FOXO1 expression.
Materials and methods
Clinical specimens and cell culture
Seven OS tissues and adjacent morphologically normal bone tissues (located >3 cm away from the OS) were collected from OS patients at Renmin Hospital of Wuhan University (Hubei, China). Tissue samples were cut into two parts and immediately snap-frozen in liquid nitrogen. One section was used for mRNA and miRNA extraction, and the other section was used for protein extraction. The study was approved by each of the patients and by the ethics committee of Renmin Hospital of Wuhan University. Human OS cell lines, Saos-2, and U2OS were cultured in RPMI 1640 (Life Technologies) supplemented with 10 % fetal bovine serum (Life Technologies) in a humidified cell incubator with an atmosphere of 5 % CO2 at 37 °C.
Real-time PCR for mature miRNAs and mRNA
MiRNAs from cultured cells and tissues were isolated and purified with miRNA isolation system (OMEGA Bio-Tek). cDNA was generated with the miScript II RT Kit (QIAGEN), and the quantitative real-time PCR (qRT-PCR) was done using the miScript SYBR Green PCR Kit (QIAGEN) following the manufacturer’s instructions. The miRNA sequence-specific qRT-PCR primers for miR-135b and endogenous control RNU6 were purchased from QIAGEN, and the qRT-PCR analysis was carried out using 7500 Real-Time PCR System (Applied Biosystems). The gene expression threshold cycle (CT) values of miRNAs were calculated by normalizing with internal control RNU6, and relative quantization values were calculated. Total RNA was extracted with a Trizol protocol, and cDNAs from the mRNAs were synthesized with the Super-Script first-strand synthesis system (Fermentas Life Science). Real-time PCR was carried out according to the standard protocol on ABI 7500 with SYBR Green detection (Applied Biosystems). GAPDH was used as an internal control, and the qRT-PCR was repeated three times. The primers for GAPDH were forward primer 5′-ATTCCATGGCACCGTCAAGGCTGA-3′, reverse primer 5′-TTCTCCATGGTGGTGAAGACGCCA-3′; for FOXO1 were forward primer 5′-GAGGAGCCTCGATGTGGATG-3′, reverse primer 5′-CCGAGATTTGGGGGAACGAA-3′.
Western blot
Total proteins were extracted from corresponding cells using the RIPA buffer (Pierce) in the presence of Protease Inhibitor Cocktail (Pierce). The protein concentration of the lysates was measured using a BCA Protein Assay Kit (Pierce). Equivalent amounts of protein were resolved and mixed with 5× Lane Marker Reducing Sample Buffer (Pierce), electrophoresed in a 10 % SDS–acrylamide gel and transferred onto Immobilon-P Transfer Membrane (Millipore). The membranes were blocked with 5 % non-fat milk in Tris-buffered saline and then incubated with primary antibodies followed by secondary antibody. The signal was detected using an ECL detection system (Millipore). The FOXO1 antibody and β-Actin antibody were from Cell Signaling Technology. HRP-conjugated secondary antibody was from Thermo.
Luciferase reporter assay
Two single strands of the wild-type 3′UTR with miR-135b binding site and two single strands of the mutant type with eight bases deleted in the miR-135b binding site (as mutant control) of FOXO1 were synthesized with restriction sites for SpeI and HindIII located at both ends of the oligonucleotides for further cloning. The single strands DNA sequences were following: the wild-type 3′UTR of FOXO1 (sense: 5′-CTAGT ACAATCTTTGCTATAATTGTATAAAGCCATAAATGTACATAAATTATGTTTAA-3′; antisense: 5′-AGCTT TAAACATAATTTATGTACATTTATGGCTTTATACAATTATAGCAAAGATTGTA-3′) and the mutated type 3′UTR of FOXO1 (sense: 5′-CTAGT ACAATCTTTGCTATAATTGTATA--------AATGTACATAAATTATGTTTAA-3′; antisense: 5′-AGCTTTAAACATAATTTATGTACATT--------TATACAATTATAGCAAAGATTGTA-3′). The corresponding sense and antisense strands were annealed and subsequently cloned into pMir-Report plasmid downstream of firefly luciferase reporter gene. Cells were seeded in 96-well plates and co-transfected with pMir-Report luciferase vector, pRL-TK Renilla luciferase vector, and miR-135b inhibitor or control. Forty-eight hours later, the luciferase activities were determined using a Dual-Luciferase Reporter Assay System (Promega) where the Renilla luciferase activity was used as an internal control and the firefly luciferase activity was calculated as the mean ± SD after being normalized by Renilla luciferase activity.
Cells transfection
MiR-135b inhibitor and relative control were purchased from Ambion. Cells were trypsinized, counted, and seeded onto 6-well plates the day before transfection to ensure 70 % cell confluence on the day of transfection. The transfection of inhibitor, pLEX-FOXO1 vector, and related controls was carried out using Lipofectamine 2000 (Invitrogen) in accordance with the manufacturer’s procedure. The inhibitor and controls were used at a final concentration of 100 nM. At 36 h post-transfection, follow-up experiments were performed.
Cell proliferation assay
Cell proliferation was monitored by the MTS assay using the CellTiter96®AQueous One Solution Cell Proliferation Assaykit (Promega) according to the manufacturer’s instructions. Related treated cells were seeded into 96-well plates at 2,000 cells/well (0.20 ml/well). The cell proliferation assay was performed on days 0, 1, 2, 3, 4, and 5 by incubation with MTS (0.02 ml/well). After 2 h further incubation, the absorbance at 490 nm of each well was recorded on the BiotexELX800 and the absorbance represented the cell number.
Cell invasion assay
Invasion of OS cells was assessed using the Cell Invasion Assay Kit (BD Biosciences) according to the manufacturer’s instructions. Briefly, at 36 h post-transfection, 3 × 104 cells in 300 μl serum-free medium were added to the upper chamber precoated with ECMatrix™ gel. Then, 0.5 ml of 10 % FBS-containing medium was added to the lower chamber as a chemoattractant. Cells were incubated for 24 h at 37 °C, and then non-invading cells were removed with cotton swabs. Cells that migrated to the bottom of the membrane were fixed with pre-cold methanol and stained with 2 % Giemsa solution. Stained cells were visualized under a microscope. To minimize the bias, at least three randomly selected fields with 100× magnification were counted, and the average number was taken.
Statistical analysis
All data are expressed as mean ± SD from three independent experiments. Statistical analyses were performed using SPSS16.0 software (SPSS, Chicago, IL). The differences between groups were analyzed using Student’s t test with only two groups or one-way analysis of variance (ANOVA) when more than two groups were compared. P values less than 0.05 were considered statistically significant.
Results
MiR-135b is upregulated and inversely correlates with FOXO1 expression in human OS
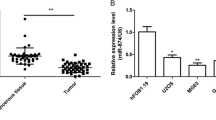
To explore the potential role of miR-135b in OS, its expression pattern was detected in seven pairs of human OS and adjacent non-neoplastic bone tissues. As shown in Fig. 1a, miR-135b expression was significantly higher in OS tissues than adjacent non-neoplastic bone tissues. Potential targets of miR-135b were predicted using public database-TargetScan (http://www.targetscan.org), and FOXO1 with critically conserved binding site was selected for further expression and function confirmation (Fig. 1b). Then, the examination of FOXO1 expression pattern in above tissues showed FOXO1 mRNA and protein expression in OS tissues were much lower than in paired adjacent non-neoplastic bone (Fig. 1c). Moreover, miR-135b levels were inversely correlated with those of FOXO1 mRNA and protein (Fig. 1d). In view of these findings, we propose that FOXO1 is a direct target of miR-135b.
The expression patterns of miR-135b and FOXO1 in OS tissues. a Relative miR-135b expression was determined in seven human OS and adjacent normal bone tissues using qRT-PCR. b Schematic of the putative binding sites of miR-135b in 3′-UTR of FOXO1 is presented, which is broadly conserved among vertebrates. c FOXO1 mRNA and protein levels in OS and adjacent normal bone tissues were detected using qRT-PCR and Western blot, respectively. d Pearson’s correlation analyses between relative miR-135b expression and FOXO1 mRNA level in seven human OS tissues. *P < 0.01
MiR-135b directly targets FOXO1
To determine whether FOXO1 is directly regulated by miR-135b in OS cells, we transfected the OS cell lines Saos-2 and U2OS with miR-135b inhibitor, and relative miR-135b expression was verified (Fig. 2a). As shown, miR-135b inhibitor significantly increased FOXO1 mRNA and protein levels in Saos-2 and U2OS cell lines (Fig. 2b). To assess whether FOXO1 is a direct target of miR-135b, the luciferase reporter vectors with the putative FOXO1 3′-UTR target site for miR-135b downstream of the luciferase gene (pMir-FOXO1-Wt, set as wild-type) and mutant version with a deletion of 8 bp in the seed region (pMir-FOXO1-Mut) were constructed. As shown in Fig. 2c, miR-135b inhibitor in both Saos-2 and U2OS cell lines significantly enhanced luciferase activity of the vector with the wild-type FOXO1 3′-UTR, but the mutant version abrogated the suppressive ability of miR-135b. These results strongly suggest miR-135b negatively regulates FOXO1 expression via direct binding to putative binding site in the FOXO1 3′-UTR region.
MiR-135b targets FOXO1 in OS cells. a The relative miR-135b expression level in Saos-2 and U2OS cell lines using qRT-PCR after transfection with miR-135b inhibitor or control. b FOXO1 mRNA and protein levels were determined with qRT-PCR and Western blot, respectively. c Luciferase reporter assay in Saos-2 and U2OS cells co-transfected with miR-135b inhibitor, a luciferase reporter containing wild-type FOXO1 3′-UTR or a mutant version, and a renilla luciferase reporter for normalization. The mean of the results from cells transfected with pMir-FOXO1-Wt and inhibitor-control was set as 1. *P < 0.01
MiR-135b promotes OS cells proliferation and invasion
As shown above, miR-135b was upregulated in OS tissues. To explore the role of miR-135b in OS cells, we determined the effect of miR-135b inhibition on proliferation and invasion using MTS and Transwell assays. We found miR-135b inhibition significantly inhibited the proliferation potential of Saos-2 and U2OS cells, compared to control-transfected cells (Fig. 3a). Similarly, transwell assay showed miR-135b inhibition markedly reduced the invasion of Saos-2 and U2OS cells (Fig. 3b). These data indicate upregulated miR-135b expression may be involved in OS cells proliferation and invasion.
MiR-135b promotes OS cell proliferation and invasion. a The proliferation patterns of Saos-2 and U2OS cells transfected with miR-135b inhibitor or the corresponding control using MTS assays. b Transwell invasion assays of Saos-2 and U2OS cells transfected with miR-135b inhibitor or the corresponding control. *P < 0.01
FOXO1 knockdown reverses miR-135b inhibitor-induced proliferation and invasion inhibition in OS cells
FOXO1 down-regulated in OS tissues is a direct target of miR-135b, to determine whether tumor promotive role of miR-135b is mediated by FOXO1, we firstly investigated the role of FOXO1 in OS. FOXO1 was overexpressed with pLEX-FOXO1 vector without FOXO1-3′-UTR that significantly increased FOXO1 protein level in Saos-2 and U2OS cell lines, compared to control (Fig. 4a). Moreover, we found FOXO1 overexpression also inhibited the proliferation (Fig. 4b) and invasion of Saos-2 and U2OS cell lines (Fig. 4c). To investigate miR-135b exerts its role via FOXO1, here OS cells were cotransfected with miR-135b inhibitor and siRNA specifically targeting FOXO1 and we found si-1# significantly attenuated the upregulation of FOXO1 induced by miR-135b inhibitor which will be used in the followed experiments (Fig. 4d). Importantly, we found FOXO1 knockdown significantly abolished miR-135b inhibitor-induced proliferation inhibition (Fig. 4e) and invasion inhibition in Saos-2 and U2OS cells (Fig. 4f). These results demonstrate that miR-135b promotes the proliferation and invasion of OS cells via suppression of FOXO1 expression.
MiR-135b regulates OS cells proliferation and invasion via modulating FOXO1 expression. a Western blot analysis of FOXO1 expression in Saos-2 and U2OS cells transfected with FOXO1 expression vector pLEX-FOXO1. b Overexpression of FOXO1 inhibited OS cells proliferation. c Overexpressed FOXO1 inhibited OS cells invasion. d Selection of effective siRNAs targeting FOXO1 upon miR-135b transfection in OS cells. e Knockdown of FOXO1 reserved the proliferation mediated by miR-135b inhibitor in OS cells. f Knockdown of FOXO1 reserved the invasion mediated by miR-135b inhibitor in OS cells. *P < 0.01
Discussion
Proliferation and metastasis play a critical role in cancer progression, and most cancer deaths are caused by complications arising from metastasis, so the targeting of metastasis-based strategy is pivotal in anti-cancer treatment. Dysregulation of miRNAs has been well documented in nearly all types of human malignancies, and numerous miRNAs are involved in tumor formation and progression by regulating the expression and action of many oncogenes and tumor suppressor genes. Recent studies have revealed a critical role of miRNAs in tumor invasion and metastasis through the regulation of a variety of genes that are necessary for invasion or metastasis [10]. In this study, we initially examined miR-135b expression in normal as well as tumor tissues from OS patients and found miR-135b was dramatically upregulated in OS. In addition, we found miR-135b promoted OS cells proliferation and invasion, suggesting its involvement in OS carcinogenesis and progression.
Emerging data have shown that miR-135b is upregulated and functions as a potential tumor promoter in several human cancer types, such as in colon, breast and lung cancers. Wu et al. found miR-135b was upregulated in colorectal cancer tissues associated with lymph node and distant metastasis, and miR-135b inhibition reduced cell migration and invasion [11]. Study from Arigoni et al. showed miR-135b was upregulated in ErbB2-driven mammary carcinoma, and it correlated with patient survival and early metastasis [12]. Lin et al. observed miR-135b was upregulated in highly invasive non-small-cell lung cancer cells, promoting cancer cell invasion and metastasis in vitro and in vivo [13]. Moreover, the tumor promoter role of miR-135b also has been found in head and neck squamous cell carcinoma [14], in pancreatic ductal adenocarcinoma [15], and in lymphoma [16]. Recently, reports also showed miR-135b was activated during neuroectoderm development, and ectopic miR-135b expression in hESC promoted differentiation toward neuroectoderm via inhibiting TGF-β and BMP signaling pathways [17], and miR-135b was involved in the impaired osteogenic differentiation and negatively regulated osteogenesis from human mesenchymal stem cells [18], suggesting the important role of miR-135b in physiology and pathophysiology processes.
FOXO1 was subsequently identified as a direct target of miR-135b in OS cells using bioinformatics analysis and experimental confirmation. Forkhead box protein O1 (FOXO1), a member of the FOXO family of transcription factors, was characterized by a conserved forkhead domain containing a DNA binding domain [19]. Numbers of studies have shown FOXO1 plays critical roles in a variety of biological processes, including cell proliferation, apoptosis, differentiation, DNA damage repair, and stress responses. Such as, FOXO1 can lead to cell cycle arrest through upregulation of the cyclin-dependent kinase inhibitors, p27 and p21, and downregulation of the cell cycle regulator cyclin D1 [20, 21]. Growing evidence suggested the involvement of FOXO1 in many types of cancer. FOXO1 targeted by miR-107 negatively correlated with proliferation in human gastric cancer cells [22]. Both nuclear FOXO1 and transcript levels have been shown to be often decreased in prostate cancers [23], and overexpression of FOXO1 induced a strong apoptotic phenotype [24]. In lung cancer, FOXO1 negatively regulated activated EGFR signaling in both cell culture and in vivo models [25] and induction of FOXO1 by curcumin inhibited lung cancer progression and metastasis [26]. Moreover, in OS cells, FOXO1 expression status was negatively associated with proliferation [27]. Given the tumor suppressor role of FOXO1, in the present study, we found FOXO1 showed a converse expression pattern of miR-135b, and overexpression of FOXO1 significantly inhibited OS cells proliferation and invasion. Furthermore, our results demonstrated miR-135b exerted its role via suppressing FOXO1 expression in OS cells.
In conclusion, we demonstrated for the first time that upregulation of miR-135b accompanied with FOXO1 downregulation is a common event in OS. Furthermore, miR-135b functions as an oncogene by directly targeting FOXO1 in OS. These findings collectively implicate miR-135b-FOXO1 axis as a promising prognostic and therapeutic target for future OS therapy.
References
He H, Ni J, Huang J (2014) Molecular mechanisms of chemoresistance in osteosarcoma. Oncol Lett 7:1352–1362
Yang J, Zhang W (2013) New molecular insights into osteosarcoma targeted therapy. Curr Opin Oncol 25:398–406
Sakamoto A, Iwamoto Y (2008) Current status and perspectives regarding the treatment of osteo-sarcoma: chemotherapy. Rev Recent Clin Trials 3:228–231
Croce CM, Calin GA (2005) miRNAs, cancer and stem cell division. Cell 122:6–7
Croce CM (2009) Causes and consequences of microRNA dysregulation in cancer. Nat Rev Genet 10:704–714
Di Leva G, Garofalo M, Croce CM (2014) MicroRNAs in cancer. Annu Rev Pathol 9:287–314
Wu X, Zhong D, Gao Q, Zhai W, Ding Z, Wu J (2013) MicroRNA-34a inhibits human osteosarcoma proliferation by downregulating ether a go-go 1 expression. Int J Med Sci 10:676–682
Zhao H, Guo M, Zhao G, Ma Q, Ma B, Qiu X, Fan Q (2012) miR-183 inhibits the metastasis of osteosarcoma via downregulation of the expression of Ezrin in F5M2 cells. Int J Mol Med 30:1013–1020
Yang J, Gao T, Tang J, Cai H, Lin L, Fu S (2013) Loss of microRNA-132 predicts poor prognosis in patients with primary osteosarcoma. Mol Cell Biochem 381:9–15
Xu Y, Zhao F, Wang Z, Song Y, Luo Y, Zhang X, Jiang L, Sun Z, Miao Z, Xu H (2012) MicroRNA-335 acts as a metastasis suppressor in gastric cancer by targeting Bcl-w and specificity protein 1. Oncogene 31:1398–1407
Wu W, Wang Z, Yang P, Yang J, Liang J, Chen Y, Wang H, Wei G, Ye S, Zhou Y (2014) MicroRNA-135b regulates metastasis suppressor 1 expression and promotes migration and invasion in colorectal cancer. Mol Cell Biochem 388:249–259
Arigoni M, Barutello G, Riccardo F, Ercole E, Cantarella D, Orso F, Conti L, Lanzardo S, Taverna D, Merighi I, Calogero RA, Cavallo F, Quaglino E (2013) miR-135b coordinates progression of ErbB2-driven mammary carcinomas through suppression of MID1 and MTCH2. Am J Pathol 182:2058–2070
Lin CW, Chang YL, Chang YC, Lin JC, Chen CC, Pan SH, Wu CT, Chen HY, Yang SC, Hong TM, Yang PC (2013) MicroRNA-135b promotes lung cancer metastasis by regulating multiple targets in the Hippo pathway and LZTS1. Nat Commun 4:1877
Zhang L, Sun ZJ, Bian Y, Kulkarni AB (2013) MicroRNA-135b acts as a tumor promoter by targeting the hypoxia-inducible factor pathway in genetically defined mouse model of head and neck squamous cell carcinoma. Cancer Lett 331:230–238
Munding JB, Adai AT, Maghnouj A, Urbanik A, Zöllner H, Liffers ST, Chromik AM, Uhl W, Szafranska-Schwarzbach AE, Tannapfel A, Hahn SA (2012) Global microRNA expression profiling of microdissected tissues identifies miR-135b as a novel biomarker for pancreatic ductal adenocarcinoma. Int J Cancer 131:E86–E95
Matsuyama H, Suzuki HI, Nishimori H, Noguchi M, Yao T, Komatsu N, Mano H, Sugimoto K, Miyazono K (2011) miR-135b mediates NPM-ALK-driven oncogenicity and renders IL-17-producing immunophenotype to anaplastic large cell lymphoma. Blood 118:6881–6892
Bhinge A, Poschmann J, Namboori SC, Tian X, Jia Hui Loh S, Traczyk A, Prabhakar S, Stanton LW (2014) MiR-135b is a direct PAX6 target and specifies human neuroectoderm by inhibiting TGF-β/BMP signaling. EMBO J 33:1271–1283
Xu S, Cecilia Santini G, De Veirman K, Vande Broek I, Leleu X, De Becker A, Van Camp B, Vanderkerken K, Van Riet I (2013) Upregulation of miR-135b is involved in the impaired osteogenic differentiation of mesenchymal stem cells derived from multiple myeloma patients. PLoS One 8:e79752
Huang H, Tindall DJ (2007) Dynamic FoxO transcription factors. J Cell Sci 120:2479–2487
Huang H, Regan KM, Lou Z, Chen J, Tindall DJ (2006) CDK2-dependent phosphorylation of FOXO1 as an apoptotic response to DNA damage. Science 314:294–297
Greer EL, Brunet A (2005) FOXO transcription factors at the interface between longevity and tumor suppression. Oncogene 24:7410–7425
Li F, Liu B, Gao Y, Liu Y, Xu Y, Tong W, Zhang A (2014) Upregulation of microRNA-107 induces proliferation in human gastric cancer cells by targeting the transcription factor FOXO1. FEBS Lett 588:538–544
Dong XY, Chen C, Sun X, Guo P, Vessella RL, Wang RX, Chung LW, Zhou W, Dong JT (2006) FOXO1A is a candidate for the 13q14 tumor suppressor gene inhibiting androgen receptor signaling in prostate cancer. Cancer Res 66:6998–7006
Fendler A, Jung M, Stephan C, Erbersdobler A, Jung K, Yousef GM (2013) The antiapoptotic function of miR-96 in prostate cancer by inhibition of FOXO1. PLoS One 8:e80807
Sangodkar J, Dhawan NS, Melville H, Singh VJ, Yuan E, Rana H, Izadmehr S, Farrington C, Mazhar S, Katz S, Albano T, Arnovitz P, Okrent R, Ohlmeyer M, Galsky M, Burstein D, Zhang D, Politi K, Difeo A, Narla G (2012) Targeting the FOXO1/KLF6 axis regulates EGFR signaling and treatment response. J Clin Invest 122:2637–2651
Li ZC, Zhang LM, Wang HB, Ma JX, Sun JZ (2014) Curcumin inhibits lung cancer progression and metastasis through induction of FOXO1. Tumour Biol 35:111–116
Chang YW, Zhao YF, Cao YL, Gu XF, Li ZQ, Wang SQ, Miao JH, Zhan HS (2013) Liver X receptor α inhibits osteosarcoma cell proliferation through up-regulation of FoxO1. Cell Physiol Biochem 32:180–186
Author information
Authors and Affiliations
Corresponding author
Additional information
Hong Pei and Zhiliang Jin have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Pei, H., Jin, Z., Chen, S. et al. MiR-135b promotes proliferation and invasion of osteosarcoma cells via targeting FOXO1. Mol Cell Biochem 400, 245–252 (2015). https://doi.org/10.1007/s11010-014-2281-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-014-2281-2