Abstract
Background
Epithelial-to-mesenchymal transition (EMT) is involved in tumor progression, invasion, migration and metastasis. EMT is a process by which polarized epithelial cells acquire motile mesothelial phenotypic features. This process is initiated by disassembly of cell-cell contacts through the loss of epithelial markers and replacement of these markers by mesenchymal markers. Reconstruction of the cytoskeleton and degradation of the tumor basement membrane ensures the spread of invasive malignant tumor cells to distant locations. Accumulating evidence indicates that curcumin, as a well-known phytochemical, can inhibit EMT/metastasis through various mechanisms and pathways in human tumors.
Conclusions
In this review, we summarize the mechanisms by which curcumin may affect EMT in cells under pathological conditions to understand its potential as a novel anti-tumor agent. Curcumin can exert chemo-preventive effects by inhibition and reversal of the EMT process through both TGF-β-dependent (e.g. in hepatoma and retinal pigment epithelial cancer) and -independent (e.g. in oral cancer, colorectal cancer, pancreatic cancer, hepatocellular carcinoma, breast cancer, melanoma, prostate cancer, bladder cancer, thyroid cancer and lung cancer) pathways. Curcumin can also mitigate chemoresistance through EMT suppression and promotion of the antiproliferative effects of conventional chemotherapeutics. Therefore, curcumin has the potential to be used as a novel adjunctive agent to prevent tumor metastasis, which may at least partly be attributed to its hampering of the EMT process.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Over the last decade, substantial efforts have been devoted to determine the genes and pathways that are involved in tumor invasion and metastasis [1]. It has been suggested that increases in cell movement, scattering and epithelial-to-mesenchymal transition (EMT) are among the main properties of advanced tumors [2]. EMT is a reversible, multistep and highly regulated trans-differentiation process, whereby cells shed their epithelial properties and adopt a more mesenchymal and invasive phenotype [3]. This process occurs at both morphological and molecular levels [4]. EMT is not only related to tumor cell growth and invasion, but also to chemotherapy resistance and apoptosis. It is considered to be the first step in the complex process of metastasis [5, 6] occurring in several types of cancer such as those of breast, colon, lung and pancreas [7,8,9,10]. Curcumin can inhibit EMT/metastasis via different mechanisms and pathways in human tumors (Table 1). In this review, we summarize the mechanisms by which curcumin affects EMT, as well as experimental and (pre)clinical data supporting its potential application as therapeutic agent.
1.1 The EMT process
EMT is a complex and highly conserved process by which, during normal embryogenesis, epithelial cells lose their junctions and polarity, thereby producing migratory mesenchymal cell types such as mesoderm and neural crest cells [38, 39]. In the adult, EMT has been implicated in wound healing, tissue fibrosis and cancer metastasis [40]. In females, EMT also occurs during placenta formation and post-delivery with the formation of fibroblasts consistent with inflammation and tissue repair [38, 39]. In the developing embryo and adults also the reverse process, mesenchymal-to-epithelial transition (MET), may occur whereby mesenchymal cells after migration to a particular location dedifferentiate to epithelial cells [41].
Through EMT, epithelial cells with a "cobblestone” shape acquire motile mesothelial features with an elongated fibroblast-like shape after which they detach from the epithelial basement in human cancers (Fig. 1a) [42]. The typical interdependent cascade of EMT events consists of invasion, propagation, intravasation into the bloodstream, extravasation from blood vessels, followed by colonization to surrounding tissues and distant locations (Fig. 1b) [43,44,45]. This process is characterized by disassembly of cell-cell contacts through the loss of epithelial markers including E-cadherin (E-cad) in adherent junctions, zonula occludens-1 (ZO-1) in tight junctions and desmoplakin in desmosomes [46]. These epithelial markers are replaced by mesenchymal markers, which leads to reconstruction of the cytoskeleton, degradation of the tumor basement membrane, destruction of the extracellular matrix (ECM) and upregulation of mesenchymal proteins such as vimentin (VIM), α-smooth muscle actin (α-SMA), fibronectin (FN), and N-cadherin (N-cad) [47]. This process allows phenotypic mesenchymal cells to exhibit lower polarity and reduced cell adhesion properties, which underlie invasion, migration and metastasis to distant organs [48,49,50,51]. E-cadherin (E-cad) as a transmembrane glycoprotein plays a critical role in cell-cell contacts and the process of EMT [52].
Epithelial-to-mesenchymal transition (EMT) process and inhibitory role of curcumin. (A) Curcumin suppresses EMT by which epithelial cells with a "cobblestone” morphology acquire motile mesothelial features and an elongated fibroblast-like morphology. This process is initiated via various processes (i.e., EMT inducer signaling pathways , growth factors, EMT transcription factors and dysregulation of microRNAs) and is characterized by disassembly of cell-cell contacts through the loss of epithelial marker proteins including E-cadherin in adherent junctions, zonula occludens-1 (ZO-1) in tight junctions and desmoplakin in desmosomes, reconstruction of the cytoskeleton, destruction of the ECM and upregulation of mesenchymal marker proteins including vimentin, α-smooth muscle actin (α-SMA), fibronectin and N-cadherin. Curcumin may also induce a reversal of the EMT process, mesenchymal-to-epithelial transition (MET). (B) Typical interdependent EMT cascades induced by inflammation, mechanical stress and hypoxia in tumors including invasion, propagation, intravasation into the bloodstream, extravasation from the bloodstream, MET and colonization in surrounding tissues and at distant locations
Several specific EMT-inducing transcription factors, including zinc-finger E-box binding homeobox 1 (ZEB1), Smad interacting protein 1 (SIp1; also known as ZEB2), Snail1 (also known as Snail), Snail2 (also known as Slug), Twist1 (also known as Twist), and E47 (also known as T cell factor, TCF3), have been reported to exhibit important regulatory effects on the EMT process in tumor cells [53, 54]. The signaling pathways participating in the advancement of EMT have also been shown to play a role in the self-renewal and maintenance of cancer stem cells (CSCs) [3, 55]. CSCs are characterized by their unique ability to initiate and extend tumor growth, as well as their selective ability for self-renewal and differentiation into tumorigenic cells [53]. CSCs have also been found to be enriched within circulating tumor cell populations in patients with a variety of cancers [56, 57]. EMT is thought to generate CSCs and to contribute to chemoresistance [58]. Based on this notion, a causal association between CSCs and EMT has been proposed and it has been suggested that CSCs may effect both local and distant propagation by acquiring mesenchymal phenotypes that allow for systemic migration away from the primary tumor mass [59].
Transforming growth factor-beta (TGF-β) is a ubiquitous prototypic multifunctional cytokine involved in EMT development, mediating the regulation of EMT-causing transcription factors such as Snail, ZEB1, Slug, SOX2, SOX4, Twist and ID1 (inhibitor of differentiation/DNA binding-1) [60]. TGF-β can induce the EMT process via both Smad-dependent and Smad-independent pathways [61]. Smad2 and Smad3 proteins undergo phosphorylation and interact with Smad4, thereby translocating to the nucleus and regulating the expression of EMT target genes [62]. Several other signaling pathways have been also implicated in TGF-β1-induced EMT in tumor cells, such as the phosphatidylinositol-3-kinase (PI3K)/AKT, mitogen-activated protein kinase (MAPK), Wnt/β-catenin, and nuclear factor-kappa B (NF-κB) pathways [63]. Vimentin (VIM) is an intermediate filament protein and a key cytoskeletal element that is only expressed by mesenchymal cells. Epithelial cells express cytokeratin, which is replaced by VIM during EMT [64]. VIM expression is positively associated with tumor progression to metastasis [65]. ZEB1 regulates the expression of target genes such as E-cad, which leads to chromatin condensation and gene silencing [51, 66]. SIp1 (or ZEB2) is a member of the δEF-1 or ZEB protein family [67], which efficiently inactivates the E-cad gene by direct binding to its promoter. As such, it plays a critical role in tumor cell invasion and propagation [68, 69]. Twist promotes EMT and ECM destruction during tumor progression [70]. Slug belongs to the SNAI family of transcription suppressors and is involved in EMT during normal development [71].
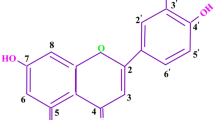
1.2 Curcumin: a bioactive compound
Curcumin (diferuloylmethane), the major component of the root of Curcuma longa Linn (turmeric; Zingiberaceae), a perennial plant, has been used for centuries by humans as a curry spice for cooking, as well as a conventional medicine in India and China [72]. In traditional Asian medicine, curcumin is employed for the treatment of multiple diseases such as rheumatism, liver disease, insect bites, cough, sinusitis, anorexia and biliary disorders [73]. It exerts diverse biological functions including anti-inflammatory [74,75,76], lipid-modifying [77,78,79], anti-thrombotic [80, 81], anti-diabetic [82], anti-oxidative [83, 84], analgesic [85], hepato-protective [86, 87] and anti-tumorigenic [88,89,90,91] functions, and it has been reported to elicit desirable medicinal effects [92,93,94]. One of the most interesting properties of curcumin is its ability to interfere with several signaling pathways and to target various bioactive molecules [93]. Curcumin maintains cellular homeostasis against oxidation by blocking endoplasmic reticulum stress [95]. Curcumin also suppresses fibrosis in organs such as the liver and kidney [96, 97], attenuates adipose dysfunction and decreases hyperglycemia via improvements in insulin sensitivity and glucose metabolism [98]. Accumulating evidence indicates that curcumin may also be effective in inhibiting various phases of tumor development, i.e., initiation, proliferation, angiogenesis, dissemination and apoptosis [99]. Several preclinical and clinical investigations have noted a therapeutic potency of curcumin against several malignancies, including brain, breast, skin and gastrointestinal cancers [100,101,102]. Curcumin has been found to interact with more than 30 proteins, including transcription factors, growth factors, proinflammatory cytokines, enzymes, as well as free radicals and protein targets that are involved in human cancer [103, 104].
Curcumin directly binds to cyclooxygenase-2 (COX-2), DNA polymerase, cytokines, and cellular signaling proteins such as NF-κB, signal transducer and activator of transcription (STAT) proteins, activator protein 1 (AP-1), early growth response protein 1 (Egr-1), Nrf-2 (also known NFE2L2), β-catenin and peroxisome proliferator-activated receptor γ (PPARγ), which are important for tumor development [105,106,107]. Curcumin blocks the induction of NF-κB, AP-1 and several regulatory genes involved in cell survival [Bcl- 2, Bcl-xL, inhibitor of apoptosis (IAP) and cellular FLICE-inhibitory protein (cFLIP)], proliferation [cyclin D1(CycD1) and c-Myc], invasion [matrix metalloproteinases (MMP-9) and urokinase-type plasminogen activator (uPA)] and angiogenesis [vascular epithelial growth factor (VEGF)] by interfering with Akt/protein kinase B (PKB) and IκBα (inhibitor of NF- kB) kinase (IKK) [108,109,110]. Curcumin likewise attenuates protein kinase C (PKC), MAPK, macrophage stimulating 1 (MST1), enhancer of zeste homolog 2 (EZH2), and STAT3 signaling cascades, which are all crucial for cancer development and progression [111,112,113]. Curcumin initiates apoptosis in cancerous cells through the activation of caspases and the release of mitochondrial cytochrome C [114]. Curcumin also may suppress both tumor formation and progression through overexpression of glutathione S-transferases (GSTs) [115], by repressing cytochrome P450 (CYP) enzymes [116, 117], or by abrogating oxidative stress [118] and inflammation [119]. The anti-inflammatory properties of curcumin relate to its ability to decrease the transcription of COX-2, xanthine oxidase, lipoxygenase, interleukin-1, -6 and -8, prostaglandins, and tumor necrosis factor-alpha (TNF-α) [120]. Curcumin plays an anti-oxidative role by scavenging superoxide anions, hydroxyl and peroxyl radicals, hydrogen peroxide (H2O2), nitric oxide (NO), and peroxynitrite [121, 122]. It can stimulate the regulation of superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase (GPx), heme oxygenase 1 (HO-1), GST, NAD(P)H quinone oxidoreductase 1 (NQO-1), and γ-glutamyl-cysteine ligase (GCL) [123]. Recent studies have indicated that curcumin can prevent EMT in different disorders through interference with different cellular signaling pathways (Fig. 2).
Mechanisms of action of curcumin (CUR) through interference with signaling pathways affecting EMT, migration, invasion, metastasis, chemoresistance and stemness. Chemokine(C-X-C motif) ligand 18 (CXCL18); curcumin (CUR); glycogen synthase kinase-3β (GSK-3β); extracellular signal regulated-protein kinase (ERK); Hedgehog (Hh); hypoxia-inducible factor-1α (HIF-1α); lipopolysaccharide (LPS); mitogen-activated protein kinase (MAPK); matrix metalloproteinase-9 (MMP-9); mammalian target of rapamycin (mTOR); nuclear factor kappa B (NF-κB); patched (PTCH); receptor tyrosine kinases (RTK); transforming growth factor-beta (TGF-β); zinc-finger E-box binding homeobox 1 (ZEB1)
2 Effect of curcumin on EMT in human cancers
2.1 Gastrointestinal cancers
2.1.1 Oral cancer
EMT and invasion contribute to the pathogenesis of oral tumorigenesis and its propagation [124]. Concordantly, low E-cad expression and high Twist expression have been associated with the prognosis and clinical outcome of patients with oral squamous cell carcinoma (OSCC) [125, 126]. Curcumin has the potential to prevent oral cancer progression and metastasis, not only by downregulating MMP-2 and -9, but also by reducing the expression of EMT markers such as Snail, Twist, and inducing the expression of E-cad and p53, which is crucial for EMT suppression [11]. As such, curcumin may serve as a promising compound to be used in adjuvant regimens directed against oral cancer progression and invasion.
2.1.2 Colorectal cancer
There is accumulating evidence supporting an inhibitory role of curcumin in EMT of colon cells. Recent findings indicate that curcumin may prevent EMT through suppression of the Wnt signaling pathway in colorectal cancer (CRC) [12]. Curcumin upregulates the expression of naked cuticle homolog 2 (NKD2), a secreted-type Wnt axis inhibitor. Curcumin can also downregulate the expression of chemokine receptor 4 (CXCR4), and decrease tumor invasion and motility, thus suggesting a mechanism for preventing the progression of CRC [12].
Curcumin has been found to suppress transcription factor Sp-1 and Sp-1 related genes, including ADAM10, calmodulin, EPHB2, histone deacetylase 4 (HDAC4), and selenoprotein P (SEPP1) in CRC cells [13]. Curcumin has also been found to block the phosphorylation of focal adhesion kinase (FAK) and to increase the regulation of ECM components that are involved in tumor invasion and propagation [13]. In addition, curcumin has been found to decrease CD24 expression and increase E-cad expression in vitro and in vivo [13]. These findings indicate that curcumin may effectively obstruct CRC metastasis through downregulation of Sp-1 and its downstream elements, and may abrogate CRC invasion via inhibition of cell adhesion molecules and cell surface proteins whilst promoting cell adhesion through increases in cell-cell tight junctions [13].
Resistance to cytotoxic chemotherapy is one of the main obstacles in the treatment of CRC patients [127]. Chemoresistance has been associated with EMT [128]. Although curcumin has been reported to increase tumor cell sensitivity to chemotherapeutic regimens, its underlying molecular mechanism is, as yet, not completely understood. Zhang and colleagues explored the sensitization mechanism of curcumin on resistance of colon cancer cells to irinotecan chemotherapy [129]. They found that administration of curcumin suppressed the proliferation of drug-resistant cells and enhanced their apoptosis. In addition, they found that treatment with a combination of curcumin and irinotecan led to upregulation of E-cad and downregulation of VIM and N-cad [129]. These observations indicate that EMT may play an important role in irinotecan resistance in colon cancer cells and that curcumin may reverse this resistance via reversal of the EMT process. Similarly, Toden et al. assessed the impact of curcumin and 5-fluorouracil (5-FU) alone, and in combination, in both parental and 5-FU resistant CRC cells [130]. They found that combination therapy with curcumin and 5-FU increased apoptosis and suppressed proliferation in both parental and resistant cells, while 5-FU alone was inefficient in resistant cells. In addition, they found that curcumin induced the expression of a cluster of EMT-suppressive miRNAs in resistant cells and inhibited EMT in these cells by downregulating the transcription of an oncogene (BMI1) and Polycomb group protein genes (SUZ12 and EZH2), major modulators of cancer stemness-associated polycomb group repressive complex subunits. Furthermore, they found that curcumin sensitized cells to 5-FU, thereby preventing tumor growth in both xenograft and theoretical models [130]. Targeting both cancer stemness and EMT has been suggested to serve as a promising approach to overcome chemoresistance, and underscores the potential use of curcumin as adjuvant to conventional chemotherapy regimens in CRC and other human tumors.
Interestingly, curcumin has also been reported to elicit anti-fibrotic effects [131]. Pretreatment with curcumin has been found to mitigate the TGF-β1-induced Smad/α-SMA pathway and to promote the transcription of PPAR-γ and E-cad in intestinal epithelial cells [35]. Using a rat model of intestinal fibrosis, the authors found that oral curcumin supplementation reduced intestinal fibrosis via increased expression of E-cad and PPARγ, as well reduced expression of α-SMA, FN, and connective-tissue growth factor (CTGF) in colon tissue. Taken together, these findings indicate that curcumin can inhibit EMT during intestinal fibrosis development through PPARγ-mediated suppression of the TGF-β1/Smad pathway [35].
2.1.3 Pancreatic, liver and hepatocellular carcinoma
Tumors have stroma that is required for nutritional support and the removal of waste products [132]. Reactive stroma consists of heterogeneous cell populations, including macrophages, cancer-associated fibroblasts (CAFs), and endothelial cells (ECs) [133,134,135,136]. CAFs are activated fibroblasts in the tumor microenvironment (TME) [137] that may affect tumor progression and metastasis and may mediate EMT in tumor cells, thereby promoting CSC traits [138]. It has been suggested that curcumin may regulate CAF-mediated invasion and metastasis in pancreatic cancer. In addition, it has been found that following curcumin treatment of pancreatic cancer the expression of mesenchymal markers in CAFs may recede and that EMT may be reversed [14]. The TME has been reported to be able to induce invasive features in cancer cells via over-expression of NF-kB and TGF-β, and via inducing a TME feedback loop [139]. In one study, curcumin has been proposed to act as a promising regulator of synergistic interactions between CSCs and CAFs in the TME through its anti-EMT activities [140].
Hypoxia, a common feature of the TME that results from unordered neovascularization of the tumor mass, is closely related to aggressive tumor behavior [141, 142]. Hypoxia-inducible factor-1α (HIF-1α) is a transcription factor that mediates cellular responses under hypoxic conditions and has been found to be aberrantly expressed in various human malignancies. Several studies have shown a potential inhibitory effect of curcumin on HIF-1α [15, 19, 143]. In particular, curcumin has been found to decrease HIF-1α levels in hepatoma cells and to decrease their proliferation and migration. Curcumin has also been found to abrogate EMT alterations related to HIF-1α accumulation resulting from a hypoxic TME [19]. In addition, it has been reported that a synthetic analogue of curcumin, CDF, can inhibit cell motility, invasion, and angiogenesis under hypoxic conditions [15]. Interestingly, CDF has been found to reduce HIF-1α expression in a mouse orthotopic model of human pancreatic cancer and to reduce the expression of mesenchymal markers such as VIM, ZEB1, and Twist in hypoxic tumor spheres [15].
In support of this, Coa and co-workers found that curcumin may attenuate EMT of pancreatic cancer cells via Hedgehog (Hh) signaling inhibition [143]. Previously, aberrant activation of the Hh pathway has been shown to be involved in tumor progression and metastasis [144]. The Hh signaling cascade represents a highly conserved cascade, consisting of the signal molecule Hh, the membrane receptors Ptch and Smo, and the downstream nuclear transcription factor Gli, which activates the expression of target genes that play a role in cell proliferation and death, invasion, angiogenesis and EMT [142]. Moreover, TGF-β1 has been found to activate EMT of hepatoma cells via induction of the Hh pathway [16]. TGF-β1 causes pancreatic cancer cells to express mesenchymal features and to develop a fibroblast-like phenotype, i.e., overexpression of VIM and FN and downregulation of E-cad, indicating that TGF-β1 can stimulate hepatoma cells to undergo EMT [16]. The authors found that curcumin significantly reversed the EMT of TGF-β1-induced pancreatic cancer cells by inhibiting Hh signaling and, thereby, inhibiting the proliferation, migration and metastasis of these cells [16]. These findings suggest that curcumin may serve as a promising drug for the treatment of pancreatic cancer through EMT inhibition via Hh signaling repression.
In line with these results, curcumin has been found to abrogate Smad2 phosphorylation and its translocation to the nucleus, thereby preventing its binding to the Snail gene promoter and, thus, Snail expression induction [17, 20, 21]. In hepatic CSC-like cells, curcumin has been found to effectively inhibit phthalate-induced migration and invasion, and to prevent EMT via the aryl hydrocarbon receptor (AhR)/extracellular signal regulated-protein kinase(ERK)/Sphingosine kinase 1(SK1)/sphingosine 1-phosphate receptor (S1PR3) pathways [21].
Additionally, curcumin has been found to reduce SOD-induced formation of ROS and H2O2 in pancreatic cancer cells (BxPC-3 and Panc-1) [17] and to reduce SOD-induced malignant growth and metastasis of these cells by reducing the expression of EMT-related factors through the PI3K/Akt/NF-κB signaling pathway. This pathway is frequently deregulated in different tumors [1, 145]. Thus, suppression of the H2O2/Akt/NF-κB signaling pathway by curcumin may be indicative for its potential in the treatment of pancreatic cancer [17].
Kong and co-workers developed a hypoxia-induced EMT model by treating human hepatocytes with non-toxic doses of cobalt chloride (CoCl2), and used this model to assess the effects of curcumin on hepatocyte EMT [18]. They found that treatment with CoCl2 induced mesenchymal cell features in hepatocytes and caused overexpression of several mesenchymal markers (α-SMA, VIM, N-cad, FN and Snail), whilst downregulating the epithelial marker E-cad. Subsequent curcumin treatment reversed the morphological alterations, blocked the expression of mesenchymal markers, and induced E-cad expression. They also found that curcumin perturbed the TGF-β pathway through abrogating the expression of TGF-β1 and preventing the phosphorylation of Smad molecules [18]. Using an experimental in vivo fibrotic liver model in rats, it was found that curcumin inhibited hepatic EMT induced by carbon tetrachloride (CCl4) through abrogation of the TGF-β/Smad cascade [18]. These in vitro and in vivo results offer a mode of action for curcumin as a therapeutic drug in the management of liver fibrosis through EMT inhibition.
Tobacco smoke is considered as a one of the main risk factor for hepatic cancer [146]. EMT elicited by tobacco smoke has been found to play an important role in the initiation and progression of this type of cancer [147]. MAPK signaling in tobacco smoke-related tumors affects EMT [28]. Liang et al. found that in tobacco smoke-exposed mice the ERK1/2, ERK5, and JNK-p38 cascades and the AP-1 protein were induced in liver tissue [148]. Tobacco exposure has also been found to decrease the expression of epithelial markers and increase the expression of mesenchymal markers at both the transcriptional and translational levels in BALB/c mice [148]. The authors also found that curcumin could significantly modulate tobacco smoke-induced activation of the ERK1/2 and JNK/MAPK signaling pathways, as well as AP-1 and EMT alterations, in mouse hepatic tissues. These findings suggest a possibility of chemoprevention of tobacco smoke-related pathological changes in hepatocytes, including EMT.
2.2 Non-gastrointestinal cancers
2.2.1 Breast cancer
Mukherjee et al. reported that curcumin may inhibit the nuclear translocation of β-catenin, thereby hampering activation of its EMT-promoting target genes, such as Slug [22]. They found that curcumin mediates E-cad upregulation and leads to an increase in E-cad/β-catenin complex formation which, in turn, inhibits the nuclear translocation of β-catenin through a negative feedback loop. Under normal conditions, E-cad in epithelial cells is associated with β-catenin in adherens junctions, thus preventing the translocation of β-catenin to the nucleus and impeding its role as a transcriptional activator [149]. Aberrant expression of β-catenin has been reported to induce malignant transformation-associated pathways in normal cells [150] and to play a role in maintaining CSCs, thus rendering it into a putative drug target. Concordantly, it has been reported that curcumin can effectively impede the aggressive migration properties of breast CSCs by preventing the initiation of EMT [22]. This finding may be relevant for its adjunct to current therapies, such as chemotherapy and radiotherapy, since these usually do not have the ability to eradicate CSCs. A combination approach may, thus, allow for a more effective treatment of highly invasive breast cancers [22].
PAC (4-hydroxy-3-methoxybenzylidene)-N-methyl-4-piperidone), a curcumin derivative, is more stable, has a better bioavailability profile and is more effective in inducing apoptosis in breast cancer cells than curcumin itself [151]. Moreover, it has been found that PAC-induced cytotoxicity is more efficient in ERα− cells than in ERα+ cells and that PAC suppresses pro-metastatic EMT in breast cancer cells, with superior potency in the triple-negative subtype [152].
Gallardo et al. reported that curcumin can reduce the expression of EMT-related genes in breast cancer cells, including E-cad, N-cad, SIP2, Twist, Slug, Axl, VIM, STAT-3, FN, p53 and Cav-1, as well as the pro-apoptotic genes caspase-3 and -8, and other cancer-related genes such as CycD1and NF-κB [23]. All these expression effects were found to result in reduced migration, invasion, apoptosis and metastatic capabilities of breast cancer cells [23].
More recently, the effect of curcumin on lipopolysaccharide (LPS)-induced EMT in breast cancer cells (MCF-7 and MDA-MB-231) was investigated [24]. It was found that curcumin significantly reduced the morphological changes related to LPS, reduced the expression of the LPS-induced EMT marker VIM, and increased the expression of E-cad [24]. This effect was mediated through suppression of the NF-κB-Snail signaling cascade. This observation indicates that curcumin has the ability to oppose LPS-stimulated EMT through inhibition of NF-κB-Snail activity in breast cancer cells, thereby hampering their dissemination and invasion [24]. In contrast, Paramita et al. reported that curcumin administration in selected doses was unable to modulate the expression of VIM, TGF-β1 and E-cad and, thereby, could not prevent EMT in cancer cells subjected to prolonged endoxifen treatment [153]. The discrepancy between these results may at least partly be attributed to differences in treatment duration.
Doxorubicin is commonly administered for the treatment of metastatic breast cancer [149]. Doxorubicin treatment may, however, elicit several undesirable effects such as drug resistance and the acquisition of invasive potential by tumor cells through EMT and attainment of a mesenchymal phenotype [154]. It has been shown that the TGF-β and PI3K/AKT signaling cascades underlie doxorubicin-induced EMT, and that curcumin can prevent doxorubicin-induced EMT, morphological changes, down-regulation of E-cad and/or over-expression of VIM through suppressing these cascades [155]. The authors also found that curcumin may increase the antiproliferative potency of doxorubicin and, thereby, decrease the clinical dosage of doxorubicin and inhibit its adverse effects [155].
2.2.2 Melanoma
Diphenyl difluoroketone (EF24) is another curcumin analog that exhibits a better bioavailability and tolerance than curcumin itself [156]. Low-dose EF24 has been reported to cause cell cycle arrest and cell death [25]. EF24 has also been found to abrogate metastatic behavior and EMT in melanoma cells (Lu1205 and A375) through expression induction of E-cad, dephosphorylation of STAT3 and downregulation of VIM and N-cad [25]. In addition, EF24 has been found to induce upregulation of miR-33b via direct targeting of the archetype transcription factor high mobility group AT-hook 2 (HMGA2) [25]. HMGA2 can alter chromatin structures and, by doing so, affect gene expression through specific DNA binding [157]. Previous studies have reported that HMGA2 may, next to its involvement in various biological processes such as embryonic development, cell growth, cell cycle regulation, migration and senescence, be overexpressed in epithelial and interstitial tumors [158]. Moreover, it has been found that EF24 can attenuate melanoma metastasis and EMT through miR-33b-dependent HMGA2 inhibition, thereby providing new leads to the treatment of metastatic melanoma [25].
Fibroblast activation protein α (FAPα) is a serine protease that plays a role in ECM remodeling which is augmented by CAFs, but is not found in normal human tissues [159]. Although FAPα is considered to be a target for cancer treatment, it has been found that inhibition of FAPα+ fibroblasts induces secretion of IFN-γ and TNF-α [160]. Both these cytokines are known to play a role in tumor progression and to prevent effective treatment, especially vaccine-based treatment. This is due to the fact that IFN-γ can induce the expression of indolamine-2,3-dioxygenase (IDO), thereby contributing to immunosuppression, while TNF-α can induce EMT. It has been found that curcumin can block the expression of IDO and TNF-α-activated EMT, thereby ameliorating the invasive and metastatic behavior of melanoma cells [160]. The authors also found that administration of FAPαc vaccine together with curcumin can modulate tumor tolerance and induce tumor-responsive T cells through IDO expression suppression, thereby stimulating FAPα antibody production and CD8+ T cell-mediated killing of FAPα-expressing stromal cells. This combination was found to prolong the survival of mice implanted with melanoma cells [160]. Collectively, these data indicate that administration of FAPαc vaccine together with curcumin may be a promising approach for the treatment of melanoma [160].
2.2.3 Urological cancers
Renal fibrosis is an indicator of end-stage renal disease (ESRD) and of chronic allograft nephropathy [161]. Since EMT is the major mechanism underlying renal fibrosis, its prevention may slow down the advancement of fibrosis [162]. Myofibroblasts are known to be the major effector cells involved in the initiation and progression of renal fibrosis in chronic kidney disease [163]. It has been estimated that nearly one third of myofibroblasts originate from the EMT process [161, 164]. TGF-β1 induces EMT, not only by activating the Smad-dependent pathway, but also by activating Smad-independent pathways such as the Akt/mTOR pathway, which is involved in renal fibrosis [165, 166]. Activation of Akt triggers EMT development in tubular epithelial cells through downregulation of epithelial cell markers (E-cad and β-catenin) and overexpression of mesenchymal markers (VIM) [167]. It has been found that curcumin can significantly enhance the proliferation and maintain the shape and morphology of renal tubular epithelial cells [36]. Interestingly, it has also been found that curcumin can inhibit TGF-β1-induced EMT by preventing Akt/mTOR pathway signaling, one of the mechanism by which curcumin exerts its anti-fibrotic effects [36]. Consistent with this observation, others found that curcumin can decrease TGF-β1 and TGF-β receptor type II levels, without affecting the phosphorylation of Smad2 and Smad3 in renal tubular epithelial cells [37]. Instead, curcumin was found to decrease the phosphorylation of ERK and PPARγ that are both induced by TGF-β1, and to increase the nuclear translocation of PPARγ in a Smad-independent way. Additionally, these authors found that use of an ERK inhibitor or a PPARγ inhibitor reversed the effects of curcumin on α-SMA, PAI-1, E-cad, and TGF-β receptors [37]. Inhibition of PPARγ signaling did not affect ERK phosphorylation, but blocking of the ERK pathway prevented PPARγ phosphorylation. Taken together, these data indicate that curcumin may interfere with TGF-β1-induced EMT via both ERK- and PPARγ-dependent pathways in renal tubular epithelial cells [37].
In vivo and in vitro studies have provided evidence supporting the beneficial effects of curcumin in reversing EMT in podocytes [168]. It was found that curcumin treatment significantly attenuated metabolic aberrations, kidney function, and morphological changes in streptozotocin (STZ)-induced diabetic rats and that curcumin inhibited EMT of podocytes in these rats by preventing Canine adenovirus 1 (cav-1) phosphorylation and effecting cav-1 and β-catenin stabilization [168]. Cav-1 retains β-catenin at the cell membrane and, thereby, prevents β-catenin nuclear translocation, binding to its specific transcription factor Lef-1 [169] and expression of its target genes [170]. Knockdown of cav-1 has been found to lead to a remarkable decrement in E-cad and β-catenin accumulation in inter-endothelial junctions [170].
Involvement of hepatocyte growth factor (HGF) and its receptor tyrosine kinase and the c-Met pathway in tumor growth, invasion and metastasis has been reported in various human tumors [171]. The downstream phosphorylation axis of HGF, specifically the MAPK and PI3K/AKT pathways, has been found to regulate the EMT process [26]. HGF can induce EMT in prostate cancer cells by increasing the expression of VIM, whereas curcumin can attenuate their cell migration and invasion [26]. Furthermore, curcumin was found to effectively reverse HGF-induced EMT in prostate cancer cells by downregulating the expression of phosphorylated c-Met, Snail and their associated signaling pathways [26].
CAFs can trigger EMT of prostate cancer cells via the monoamine oxidase A (MAOA)/mTOR/HIF-1α signaling pathway [27]. MAOA, a mitochondrial enzyme, has been associated with prostate tumorigenesis and invasion by activation of EMT, regulation of Twist1, and stabilization of the transcription factor HIF-1α, which mediates hypoxia through increases in reactive oxygen species (ROS) [172]. Two transcription factors, mTOR and HIF-1α, are known to play a major role in CAF-mediated EMT induction in prostate cancer cells [173]. mTOR regulates EMT through downregulation of the RhoA and Rac1 cascades [173]. Indeed, HIF-1α has been found to be associated with the EMT process via induction of both Twist and Snail-1, causing increased invasiveness [174, 175]. Curcumin has been found to inhibit CAF-induced EMT of prostate cancer cells via prevention of the MAOA/mTOR/HIF-1α signaling pathway [27].
In another study the role of the ERK5/AP-1 pathway in benzidine-induced EMT in human normal SV-40 immortalized human urothelial cells (SV-HUC-1) was evaluated, as well as the impact of curcumin on EMT induced by benzidine [176]. A specific ERK5 inhibitor, XMD8-92, was found to reverse the EMT process [177], whereas curcumin was found to decrease benzidine-elicited urocystic EMT by abrogating the ERK5/AP-1 pathway [176]. The inhibitory role of curcumin on benzidine-induced EMT via the ERK5/AP-1 pathway suggests a potential application for curcumin in the treatment of bladder cancer [176].
CSCs play a crucial role in the advancement of several cancers including tobacco smoke-associated cancers [178]. Exposure to tobacco smoke (TS) is a key independent risk factor for bladder cancer [179], although the exact mechanism of TS exposure-induced urocystic EMT and the development of CSC features is as yet unknown. It has been found that prolonged exposure to tobacco smoke may trigger EMT and elevated levels of stemness markers [147], whereas the Wnt/β-catenin pathway has been found to mediate tobacco smoke-induced EMT and stemness [180]. In addition, it has been found that curcumin administration may reverse TS-induced urocystic activation of Wnt/β-catenin, EMT and the accumulation of CSC traits [178]. Similarly, tobacco smoke exposure for 12 weeks has been found to cause upregulation of the ERK1/2, JNK-p38 and ERK5/MAPK pathways, as well as AP-1, in bladder cancer cells [28]. Smoke exposure also decreased the expression of E-cad and zona occludens-1 (ZO-1), but increased the expression of VIM and N-cad at both the mRNA and protein levels in bladder cancer cells. After curcumin administration, upregulation of the ERK1/2, JNK and p38 MAPK pathways, AP-1 and EMT changes induced by tobacco smoke were found to be significantly decreased in bladder tissues [28]. These results indicate a beneficial role of curcumin in tobacco smoke-elicited MAPK activation and EMT, thereby opening new avenues for chemoprevention of tobacco smoke-related bladder cancer [28].
2.2.4 Thyroid cancer
Curcumin induces significant morphological changes in thyroid cancer cells, changing them from a spindle fibroblast-like, mesenchymal phenotype to a more epithelial polarized phenotype [29, 30]. Curcumin has been found to increase the expression of E-cad and decrease the expression of VIM in papillary thyroid cancer cells and to impede TGF-β1-induced EMT through downregulation of the Smad2/3 signaling pathways and the MMP-2 and MMP-9 proteins [29]. These unique anti-metastatic and anti-EMT effects of curcumin may allow for the design of effective regimens for chemoprevention of relapse and metastasis in thyroid cancer.
2.2.5 Lung cancer
Tobacco smoke is known as a critical risk factor for the development of lung cancer, and determining the molecular mechanisms underlying tobacco smoke-induced cancer are therefore of paramount importance [181]. Both the mRNA and protein expression levels of the epithelial markers E-cad and ZO-1 were found to be decreased, while those of the mesenchymal markers VIM and N-cad were found to be increased, in response to tobacco smoke exposure. Also, increases in ERK1/2, JNK and p38 MAPK signaling, and the AP-1 protein, and a decrease in ERK5/MAPK signaling were observed in lung tissues of mice exposed to tobacco smoke [31]. The authors found that curcumin treatment ameliorated tobacco smoke-induced MAPK/AP-1 activation (ERK1/2, JNK and p38 MAPK pathways, and AP-1) and induced EMT in lung tissues [31].
It has also been found that curcumin may reverse HGF-induced motility and EMT-associated morphological alterations in lung cancer cells (A549 and PC-9) by targeting the c-Met/Akt/mTOR signaling cascades [32]. In human umbilical vein endothelial cells (HUVECs), curcumin has been found to reduce PI3K/Akt/mTOR signaling and to activate apoptosis, thereby decreasing the metastatic capacity of HGF-treated HUVECs. The authors also found that, in an experimental animal model, curcumin suppressed HGF-induced tumor growth and induced overexpression of E-cad and downregulation of VIM, CD34, and VEGF expression [32]. These findings emphasize the ability of curcumin to avert HGF-induced EMT and angiogenesis by interfering with the c-Met and PI3K/Akt/mTOR axes [32].
Bisdemethoxycurcumin (BDMC) is a putative analogue of curcumin with anti-cancer properties including suppression of EMT, invasion and dissemination [182]. BDMC has been found to repress TGF-β1-induced EMT in 95D non-small cell lung cancer (NSCLC) cells and to disrupt the Wnt/β-catenin pathway by elevating Wnt inhibitory factor-1 (WIF-1) protein expression [33]. WIF-1 is a key molecule regulating the response of BDMC to TGF-β1-induced EMT via the control of tumor progression and metastasis[33]. These data indicate that BDMC may affect EMT induced by TGF-β1 in NSCLC cells, which is regulated by WIF-1 [33].
2.2.6 Retinal pigment epithelial EMT
Proliferative vitreoretinopathy (PVR) is characterized by a series of steps initiating from the occurrence of a retinal tear, and terminating in detachment, apoptosis and constriction of membranes [183]. Aberrant deposition of collagen and matrix components followed by accumulation of excessive numbers of fibroblasts leads to tissue fibrosis [184]. A key element of PVR is an excessive inflammatory response to tears and detachment of the retina [185]. Release of retinal pigment epithelial (RPE) cells via retinal breaks causes migration through the retinal surface [186]. RPE cells undergo EMT to form fibroblast-like cells that are actively involved in scar formation through ECM genesis in the retina and, subsequently, PVR [187]. Adjuvant therapies to suppress the relapse of PVR post-surgery have been proven unsuccessful in clinical trials [188]. It has been found, however, that curcumin may reverse EMT by blocking Smad-3 phosphorylation elicited by TGF-β1 in adult human RPE cells, ARPE-19 [34]. In addition, it has been found that curcumin can effectively decrease the mRNA and protein levels of EMT markers induced by TGF-β1, including α-SMA, VIM, ZO-1 and MMP-2 in ARPE-19 cells. As such, curcumin can be proposed as option for pre-clinical assessment in PVR adjuvant therapy [34].
3 Conclusions and perspectives
Several studies have documented an important role of EMT in cancer progression [7,8,9]. The process of EMT involves a wide range of signaling pathways and crosstalk between different molecules. EMT contributes to the emergence of CSC traits and to recurrence and resistance to chemo- and immuno-therapy. Its reverse process, MET, is less well characterized. The exact determination of EMT in cell culture systems is limited due to its transient and reversible nature. TGF-β has emerged as an effective inducer of EMT through both SMAD-dependent and SMAD-independent pathways. Thus, therapies aimed at targeting these signaling pathways via TGF-β may serve as promising approaches to prevent invasive growth of cancer cells and to inhibit metastasis. In the past two decades, curcumin has attracted increasing attention as a plausible novel anti-tumor agent based on its potent anti-tumor effects in experimental models and its low toxicity in normal tissues (Fig. 3). Data from preclinical and clinical studies confirm that oral administration of curcumin is safe and well-tolerated, though low water-solubility and bioavailability may hamper its clinical application. Several studies have confirmed that curcumin may considerably inhibit tumor cell growth, proliferation, invasion, and angiogenesis. Curcumin may also modulate and potentially prevent EMT, thereby enhancing cell adhesion and the formation of cell-cell tight junctions (Fig. 3). Recent data indicate that curcumin can also exert chemo-preventive effects by inhibition and reversal of the EMT process through both TGF-β-dependent (e.g. hepatoma and retinal pigment epithelial cancer) and -independent (e.g. oral cancer, CRC, pancreatic cancer, hepatocellular carcinoma, breast cancer, melanoma, prostate cancer, bladder cancer, thyroid cancer and lung cancer) pathways. In addition, it has been found that curcumin can evade chemoresistance through EMT suppression and promote the antiproliferative effects of conventional chemotherapeutics. Therefore, curcumin has the potential to be used as a novel adjunctive agent to prevent tumor metastasis, which may at least partly be attributed to its potency to hamper the EMT process. Future knowledge gained from pre-clinical studies may allow a further elaboration of strategies to target EMT related to intestinal and renal fibrosis, as well as to tumor progression and metastasis.
Inhibitory actions of curcumin in cancer. Curcumin directly binds to cyclooxygenase-2 (COX-2), DNA polymerase, cytokines, transcription factors and cellular proteins such as NF-κB, signal transducer and activator of transcription (STAT) proteins, activator protein 1 (AP-1), early growth response protein 1 (Egr-1), Nrf-2 (also known NFE2L2), β-catenin, and peroxisome proliferator-activated receptor γ (PPARγ), that play important roles in tumor development. Curcumin blocks NF-κB, AP-1 and proteins that are involved in cell survival [Bcl- 2, Bcl-xL, inhibitor of apoptosis (IAP) and cellular FLICE-inhibitory protein (cFLIP)], proliferation [cyclin D1(CycD1) and c-Myc], dissemination [matrix metalloproteinases (MMP-9) and urokinase-type plasminogen activator (uPA)] and angiogenesis [vascular epithelial growth factor (VEGF)] by interfering with Akt/protein kinase B (PKB) and IκBα (inhibitor of NF-κB) kinase (IKK). Curcumin likewise attenuates protein kinase C (PKC), MAPK, macrophage stimulating 1 (MST1), enhancer of zeste homolog 2 (EZH2), and STAT3 signaling cascades, which are crucial for tumor initiation and progression and initiates apoptosis in tumor cells through activating caspases and the release of mitochondrial cytochrome C
References
A. Bahrami, A. Hesari, M. Khazaei, S.M. Hassanian, G.A. Ferns, A. Avan, The therapeutic potential of targeting the BRAF mutation in patients with colorectal cancer. J Cell Physiol. 233, 2162–2169 (2018)
F. Bocci, H. Levine, J.N. Onuchic and M.K. Jolly Deciphering the dynamics of epithelial-mesenchymal transition and cancer stem cells in tumor progression, arXiv preprint arXiv:1808.09113, (2018)
J.P. Thiery, H. Acloque, R.Y. Huang, M.A. Nieto, Epithelial-mesenchymal transitions in development and disease. Cell 139, 871–890 (2009)
M. Diepenbruck, G. Christofori, Epithelial–mesenchymal transition (EMT) and metastasis: yes, no, maybe? Curr Opin Cell Biol. 43, 7–13 (2016)
L. Ombrato, I. Malanchi, The EMT universe: space between cancer cell dissemination and metastasis initiation. Crit Rev Oncog. 19, 349–361 (2014)
H. Zheng, Y. Kang, Multilayer control of the EMT master regulators. Oncogene 33, 1755 (2014)
M. Guarino, Epithelial–mesenchymal transition and tumour invasion. Int J Biochem Cell Biol. 39, 2153–2160 (2007)
A. Natalwala, R. Spychal, C. Tselepis, Epithelial-mesenchymal transition mediated tumourigenesis in the gastrointestinal tract. World J Gastroenterol. 14, 3792 (2008)
Y. Wang, B.P. Zhou, Epithelial-mesenchymal transition—a hallmark of breast cancer metastasis. Cancer Hallm. 1, 38–49 (2013)
A. Fortunato, The role of hERG1 ion channels in epithelial-mesenchymal transition and the capacity of riluzole to reduce cisplatin resistance in colorectal cancer cells. Cell Oncol. 40, 367–378 (2017)
A.Y.-L. Lee, C.-C. Fan, Y.-A. Chen, C.-W. Cheng, Y.-J. Sung, C.-P. Hsu, T.-Y. Kao, Curcumin inhibits invasiveness and epithelial-mesenchymal transition in oral squamous cell carcinoma through reducing matrix metalloproteinase 2, 9 and modulating p53-E-cadherin pathway. Integr Cancer Ther. 14, 484–490 (2015)
Z. Zhang, H. Chen, C. Xu, L. Song, L. Huang, Y. Lai, Y. Wang, H. Chen, D. Gu, L. Ren, Curcumin inhibits tumor epithelial-mesenchymal transition by downregulating the Wnt signaling pathway and upregulating NKD2 expression in colon cancer cells. Oncol Rep. 35, 2615–2623 (2016)
C.-C. Chen, M. Sureshbabul, H.-W. Chen, Y.-S. Lin, J.-Y. Lee, Q.-S. Hong, Y.-C. Yang, S.-L. Yu, Curcumin suppresses metastasis via Sp-1, FAK inhibition, and E-cadherin upregulation in colorectal cancer. Evid Based Complement Alternat Med. 2013, 541695 (2013)
Q. Wang, C. Qu, F. Xie, L. Chen, L. Liu, X. Liang, X. Wu, P. Wang, Z. Meng, Curcumin suppresses epithelial-to-mesenchymal transition and metastasis of pancreatic cancer cells by inhibiting cancer-associated fibroblasts. Am J Cancer Res. 7, 125 (2017)
B. Bao, S. Ali, A. Ahmad, A.S. Azmi, Y. Li, S. Banerjee, D. Kong, S. Sethi, A. Aboukameel, S.B. Padhye, Hypoxia-induced aggressiveness of pancreatic cancer cells is due to increased expression of VEGF, IL-6 and miR-21, which can be attenuated by CDF treatment. PloS one 7, e50165 (2012)
X.-D. Sun, X.-E. Liu, D.-S. Huang, Curcumin reverses the epithelial-mesenchymal transition of pancreatic cancer cells by inhibiting the Hedgehog signaling pathway. Oncol Rep. 29, 2401–2407 (2013)
W. Li, Z. Jiang, X. Xiao, Z. Wang, Z. Wu, Q. Ma, L. Cao, Curcumin inhibits superoxide dismutase-induced epithelial-to-mesenchymal transition via the PI3K/Akt/NF-κB pathway in pancreatic cancer cells. Int J Oncol. 52, 1593–1602 (2018)
D. Kong, F. Zhang, J. Shao, L. Wu, X. Zhang, L. Chen, Y. Lu, S. Zheng, Curcumin inhibits cobalt chloride-induced epithelial-to-mesenchymal transition associated with interference with TGF-β/Smad signaling in hepatocytes. Lab Invest. 95, 1234 (2015)
W. Duan, Y. Chang, R. Li, Q. Xu, J. Lei, C. Yin, T. Li, Y. Wu, Q. Ma, X. Li, Curcumin inhibits hypoxia inducible factor-1α-induced epithelial-mesenchymal transition in HepG2 hepatocellular carcinoma cells. Mol Med Rep. 10, 2505–2510 (2014)
M.-T. Cao, H.-F. Liu, Z.-G. Liu, P. Xiao, J.-J. Chen, Y. Tan, X.-X. Jiang, Z.-C. Jiang, Y. Qiu, H.-J. Huang, Curcumin downregulates the expression of Snail via suppressing Smad2 pathway to inhibit TGF-β1-induced epithelial-mesenchymal transitions in hepatoma cells. Oncotarget 8, 108498 (2017)
C.-F. Tsai, T.-H. Hsieh, J.-N. Lee, C.-Y. Hsu, Y.-C. Wang, K.-K. Kuo, H.-L. Wu, C.-C. Chiu, E.-M. Tsai, P.-L. Kuo, Curcumin suppresses phthalate-induced metastasis and the proportion of cancer stem cell (CSC)-like cells via the inhibition of AhR/ERK/SK1 signaling in hepatocellular carcinoma. J Agric Food Chem. 63, 10388–10398 (2015)
S. Mukherjee, M. Mazumdar, S. Chakraborty, A. Manna, S. Saha, P. Khan, P. Bhattacharjee, D. Guha, A. Adhikary, S. Mukhjerjee, Curcumin inhibits breast cancer stem cell migration by amplifying the E-cadherin/β-catenin negative feedback loop. Stem Cell Res Ther. 5, 116 (2014)
M. Gallardo, G.M. Calaf, Curcumin and epithelial-mesenchymal transition in breast cancer cells transformed by low doses of radiation and estrogen. Int J Oncol. 48, 2534–2542 (2016)
T. Huang, Z. Chen, L. Fang, Curcumin inhibits LPS-induced EMT through downregulation of NF-κB-Snail signaling in breast cancer cells. Oncol Rep. 29, 117–124 (2013)
P. Zhang, H. Bai, G. Liu, H. Wang, F. Chen, B. Zhang, P. Zeng, C. Wu, C. Peng, C. Huang, MicroRNA-33b, upregulated by EF24, a curcumin analog, suppresses the epithelial-to-mesenchymal transition (EMT) and migratory potential of melanoma cells by targeting HMGA2. Toxicol Lett. 234, 151–161 (2015)
H.J. Hu, X.L. Lin, M.H. Liu, X.J. Fan, W.W. Zou, Curcumin mediates reversion of HGF-induced epithelial-mesenchymal transition via inhibition of c-Met expression in DU145 cells. Oncol Lett. 11, 1499–1505 (2016)
Y. Du, Q. Long, L. Zhang, Y. Shi, X. Liu, X. Li, B. Guan, Y. Tian, X. Wang, L. Li, Curcumin inhibits cancer-associated fibroblast-driven prostate cancer invasion through MAOA/mTOR/HIF-1α signaling. Int J Oncol. 47, 2064–2072 (2015)
Z. Liang, W. Xie, R. Wu, H. Geng, L. Zhao, C. Xie, X. Li, M. Zhu, W. Zhu, J. Zhu, Inhibition of tobacco smoke-induced bladder MAPK activation and epithelial-mesenchymal transition in mice by curcumin. Int J Clin Exp Pathol. 8, 4503 (2015)
L. Zhang, X. Cheng, Y. Gao, C. Zhang, J. Bao, H. Guan, H. Yu, R. Lu, Q. Xu, Y. Sun, Curcumin inhibits metastasis in human papillary thyroid carcinoma BCPAP cells via down-regulation of the TGF-β/Smad2/3 signaling pathway. Exp Cell Res. 341, 157–165 (2016)
C.-Y. Zhang, L. Zhang, H.-X. Yu, J.-D. Bao, R.-R. Lu, Curcumin inhibits the metastasis of K1 papillary thyroid cancer cells via modulating E-cadherin and matrix metalloproteinase-9 expression. Biotechnol Lett. 35, 995–1000 (2013)
Z. Liang, R. Wu, W. Xie, M. Zhu, C. Xie, X. Li, J. Zhu, W. Zhu, J. Wu, S. Geng, Curcumin reverses tobacco smoke-induced epithelial-mesenchymal transition by suppressing the MAPK pathway in the lungs of mice. Mol Med Rep. 17, 2019–2025 (2018)
D. Jiao, J. Wang, W. Lu, X. Tang, J. Chen, H. Mou, Q.-y. Chen, Curcumin inhibited HGF-induced EMT and angiogenesis through regulating c-Met dependent PI3K/Akt/mTOR signaling pathways in lung cancer. Mol Ther Oncolytics. 3 (2016)
J.-H. Xu, H.-P. Yang, X.-D. Zhou, H.-J. Wang, L. Gong, C.-L. Tang, Role of Wnt inhibitory factor-1 in inhibition of bisdemethoxycurcumin mediated epithelial-to-mesenchymal transition in highly metastatic lung cancer 95D cells. Chin Med J. 128, 1376 (2015)
S. Shanmuganathan, V.N. Sumantran, N. Angayarkanni, Epigallocatechin gallate & curcumin prevent transforming growth factor beta 1-induced epithelial to mesenchymal transition in ARPE-19 cells. Indian J Med Res. 146, S85 (2017)
S. Xu, B. Jiang, H. Wang, C. Shen, H. Chen, L. Zeng, Curcumin suppresses intestinal fibrosis by inhibition of PPARγ-mediated epithelial-mesenchymal transition. Evid Based Complement Alternat Med. 2017, 7876064 (2017)
F.-q. Zhu, M.-j. Chen, M. Zhu, R.-s. Zhao, W. Qiu, X. Xu, H. Liu, H.-w. Zhao, R.-j. Yu, X.-f. Wu, Curcumin suppresses epithelial–mesenchymal transition of renal tubular epithelial cells through the inhibition of Akt/mTOR Pathway. Biol Pharm Bull. 40, 17–24 (2017)
R. Li, Y. Wang, Y. Liu, Q. Chen, W. Fu, H. Wang, H. Cai, W. Peng, X. Zhang, Curcumin inhibits transforming growth factor-β1-induced EMT via PPARγ pathway, not Smad pathway in renal tubular epithelial cells. PloS one 8, e58848 (2013)
Z. Wang, Y. Li, A. Ahmad, A.S. Azmi, D. Kong, S. Banerjee, F.H. Sarkar, Targeting miRNAs involved in cancer stem cell and EMT regulation: An emerging concept in overcoming drug resistance. Drug Res Updates 13, 109–118 (2010)
Z. Wang, Y. Li, D. Kong, F.H. Sarkar, The role of Notch signaling pathway in epithelial-mesenchymal transition (EMT) during development and tumor aggressiveness. Current Drug Targets 11, 745–751 (2010)
R. Kalluri, R.A. Weinberg, The basics of epithelial-mesenchymal transition. J Clin Invest. 119, 1420–1428 (2009)
A. Singh, J. Settleman, EMT, cancer stem cells and drug resistance: an emerging axis of evil in the war on cancer. Oncogene 29, 4741 (2010)
Y. Liu, Z. Dong, H. Liu, J. Zhu, F. Liu, G. Chen, Transition of mesothelial cell to fibroblast in peritoneal dialysis: EMT, stem cell or bystander? Peritoneal Dialysis International 35, 14–25 (2015)
J.P. Thiery, Epithelial–mesenchymal transitions in tumour progression. Nature Rev Cancer 2, 442 (2002)
M. Yousefi, R. Nosrati, A. Salmaninejad, S. Dehghani, A. Shahryari, A. Saberi, Organ-specific metastasis of breast cancer: molecular and cellular mechanisms underlying lung metastasis. Cell Oncol. 41, 123–140 (2018)
M. Yousefi, T. Bahrami, A. Salmaninejad, R. Nosrati, P. Ghaffari, S.H. Ghaffari, Lung cancer-associated brain metastasis: Molecular mechanisms and therapeutic options. Cell Oncol. 40, 419–441 (2017)
J.P. Thiery, J.P. Sleeman, Complex networks orchestrate epithelial–mesenchymal transitions. Nat Rev Mol Cell Biol. 7, 131 (2006)
Y. Liu, Epithelial to mesenchymal transition in renal fibrogenesis: pathologic significance, molecular mechanism, and therapeutic intervention. J Am Soc Nephrol. 15, 1–12 (2004)
H. Hugo, M.L. Ackland, T. Blick, M.G. Lawrence, J.A. Clements, E.D. Williams, E.W. Thompson, Epithelial—mesenchymal and mesenchymal—epithelial transitions in carcinoma progression. J Cell Physiol. 213, 374–383 (2007)
V.H. Haase, Oxygen regulates epithelial-to-mesenchymal transition: insights into molecular mechanisms and relevance to disease. Kidney Int. 76, 492–499 (2009)
J.M. Lee, S. Dedhar, R. Kalluri, E.W. Thompson, The epithelial–mesenchymal transition: new insights in signaling, development, and disease. J Cell. Biol. 172, 973–981 (2006)
J. Jiang, Y.-l. Tang, X.-h. Liang, EMT: a new vision of hypoxia promoting cancer progression. Cancer Biol Ther. 11, 714–723 (2011)
T. Brabletz, A. Jung, S. Spaderna, F. Hlubek, T. Kirchner, Migrating cancer stem cells—an integrated concept of malignant tumour progression. Nat Rev Cancer 5, 744 (2005)
M. Al-Hajj, M.F. Clarke, Self-renewal and solid tumor stem cells. Oncogene 23, 7274 (2004)
T.R. Graham, H.E. Zhau, V.A. Odero-Marah, A.O. Osunkoya, K.S. Kimbro, M. Tighiouart, T. Liu, J.W. Simons, R.M. O'Regan, Insulin-like growth factor-I–dependent up-regulation of ZEB1 drives epithelial-to-mesenchymal transition in human prostate cancer cells. Cancer Res. 68, 2479–2488 (2008)
C. Scheel and R.A. Weinberg, in Seminars in cancer biology, (Elsevier, 2012), p. 396-403
A.J. Armstrong, M.S. Marengo, S. Oltean, G. Kemeny, R. Bitting, J. Turnbull, C.I. Herold, P.K. Marcom, D. George and M. Garcia-Blanco, Circulating tumor cells from patients with advanced prostate and breast cancer display both epithelial and mesenchymal markers. Mol Cancer Res. 9, 997–1007 (2011)
W. Wang, L. Wan, S. Wu, J. Yang, Y. Zhou, F. Liu, Z. Wu, Y. Cheng, Mesenchymal marker and LGR5 expression levels in circulating tumor cells correlate with colorectal cancer prognosis. Cell Oncol. 41, 495–504 (2018)
G. van der Horst, L. Bos, G. van der Pluijm, Epithelial plasticity, cancer stem cells and the tumor supportive stroma in bladder carcinoma. Mol Cancer Res. 10, 995–1009 (2012)
I. Malanchi, Tumour cells coerce host tissue to cancer spread. Bonekey Rep. 2, 371 (2013)
F. Amerizadeh, A. Bahrami, M. Khazaei, A. Hesari, M. Rezayi, S. Talebian, M. Maftouh, M. Moetamani-Ahmadi, S. Seifi, S. ShahidSales, M. Joudi-Mashhad, G.A. Ferns, F. Ghasemi, A. Avan, Current status and future prospects of transforming growth factor-β as a potential prognostic and therapeutictarget in the treatment of breast cancer. J Cell Biochem. (2019). https://doi.org/10.1002/jcb.27831
J. Zavadil, L. Cermak, N. Soto-Nieves, E.P. Böttinger, Integration of TGF-β/Smad and Jagged1/Notch signalling in epithelial-to-mesenchymal transition. EMBO J. 23, 1155–1165 (2004)
H. Ikushima, K. Miyazono, TGFβ signalling: a complex web in cancer progression. Nature Rev Cancer 10, 415 (2010)
M.A. Huber, N. Kraut, H. Beug, Molecular requirements for epithelial–mesenchymal transition during tumor progression. Curr Opin Cell Biol. 17, 548–558 (2005)
S.A. Mani, W. Guo, M.-J. Liao, E.N. Eaton, A. Ayyanan, A.Y. Zhou, M. Brooks, F. Reinhard, C.C. Zhang, M. Shipitsin, The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell 133, 704–715 (2008)
M.E. Kidd, D.K. Shumaker, K.M. Ridge, The role of vimentin intermediate filaments in the progression of lung cancer. Am J Respir Cell Mol Biol. 50, 1–6 (2014)
J.J. Christiansen, A.K. Rajasekaran, Reassessing epithelial to mesenchymal transition as a prerequisite for carcinoma invasion and metastasis. Cancer Res. 66, 8319–8326 (2006)
K. Verschueren, J.E. Remacle, C. Collart, H. Kraft, B.S. Baker, P. Tylzanowski, L. Nelles, G. Wuytens, M.-T. Su, R. Bodmer, SIP1, a novel zinc finger/homeodomain repressor, interacts with Smad proteins and binds to 5′-CACCT sequences in candidate target genes. J Biol Chem. 274, 20489–20498 (1999)
E.-H. Nam, Y. Lee, Y.-K. Park, J.W. Lee, S. Kim, ZEB2 upregulates integrin α5 expression through cooperation with Sp1 to induce invasion during epithelial–mesenchymal transition of human cancer cells. Carcinogenesis 33, 563–571 (2012)
M.A. Eckert, T.M. Lwin, A.T. Chang, J. Kim, E. Danis, L. Ohno-Machado, J. Yang, Twist1-induced invadopodia formation promotes tumor metastasis. Cancer Cell 19, 372–386 (2011)
E. Casas, J. Kim, A. Bendesky, L. Ohno-Machado, C.J. Wolfe, J. Yang, Snail2 is an essential mediator of Twist1-induced epithelial mesenchymal transition and metastasis. Cancer Res. 71, 245–254 (2011)
A. Barrallo-Gimeno, M.A. Nieto, The Snail genes as inducers of cell movement and survival: implications in development and cancer. Development 132, 3151–3161 (2005)
M. Mohajeri, B. Behnam, A.F. Cicero, A. Sahebkar, Protective effects of curcumin against aflatoxicosis: A comprehensive review. J Cell Physiol. 233, 3552–3577 (2018)
A.B. Kunnumakkara, C. Koca, S. Dey, P. Gehlot, S. Yodkeeree, D. Danda, B. Sung, B.B. Aggarwal, Molecular targets and therapeutic uses of spices: modern uses for ancient medicine. World Scientific 57, 1510–1528 (2009)
A. Sahebkar, A.F.G. Cicero, L.E. Simental-Mendía, B.B. Aggarwal, S.C. Gupta, Curcumin downregulates human tumor necrosis factor-α levels: A systematic review and meta-analysis ofrandomized controlled trials. Pharmacol Res. 107, 234–242 (2016)
Y. Panahi, M.S. Hosseini, N. Khalili, E. Naimi, M. Majeed, A. Sahebkar, Antioxidant and anti-inflammatory effects of curcuminoid-piperine combination in subjects with metabolic syndrome: A randomized controlled trial and an updated meta-analysis. Clin Nutr. 34, 1101–1108 (2015)
E. Abdollahi, A.A. Momtazi, T.P. Johnston, A. Sahebkar, Therapeutic effects of curcumin in inflammatory and immune-mediated diseases: A nature-made jack-of-all-trades? J Cell Physiol. 233, 830–848 (2018)
A.F.G. Cicero, A. Colletti, G. Bajraktari, O. Descamps, D.M. Djuric, M. Ezhov, Z. Fras, N. Katsiki, M. Langlois, G. Latkovskis, D.B. Panagiotakos, G. Paragh, D.P. Mikhailidis, O. Mitchenko, B. Paulweber, D. Pella, C. Pitsavos, Ž. Reiner, K.K. Ray, M. Rizzo, A. Sahebkar, M.C. Serban, L.S. Sperling, P.P. Toth, D. Vinereanu, M. Vrablík, N.D. Wong, M. Banach, Lipid lowering nutraceuticals in clinical practice: Position paper from an International Lipid Expert Panel. Arch Med Sci. 13, 965–1005 (2017)
Y. Panahi, M.S. Hosseini, N. Khalili, E. Naimi, S.S. Soflaei, M. Majeed, A. Sahebkar, Effects of supplementation with curcumin on serum adipokine concentrations: A randomized controlled trial. Nutrition 32, 1116–1122 (2016)
S. Ganjali, C.N. Blesso, M. Banach, M. Pirro, M. Majeed, A. Sahebkar, Effects of curcumin on HDL functionality. Pharmacol Res. 119, 208–218 (2017)
F. Keihanian, A. Saeidinia, R.K. Bagheri, T.P. Johnston, A. Sahebkar, Curcumin, hemostasis, thrombosis, and coagulation. J Cell Physiol. 233, 4497–4511 (2018)
J. Tabeshpour, M. Hashemzaei, A. Sahebkar, The regulatory role of curcumin on platelet functions. J Cell Biochem. 119, 8713–8722 (2018)
Y. Panahi, N. Khalili, E. Sahebi, S. Namazi, L.E. Simental-Mendía, M. Majeed, A. Sahebkar, Effects of curcuminoids plus piperine on glycemic, hepatic and inflammatory biomarkers in patients with Type 2 diabetes mellitus: A randomized double-blind placebo-controlled trial. Drug Res. 68, 403–409 (2018)
A. Sahebkar, M.C. Serban, S. Ursoniu, M. Banach, Effect of curcuminoids on oxidative stress: A systematic review and meta-analysis of randomized controlled trials. J Funct Foods 18, 898–909 (2015)
Y. Panahi, N. Khalili, E. Sahebi, S. Namazi, M.S. Karimian, M. Majeed, A. Sahebkar, Antioxidant effects of curcuminoids in patients with type 2 diabetes mellitus: a randomized controlled trial. Inflammopharmacology 25, 25–31 (2017)
A. Sahebkar, Y. Henrotin, Analgesic efficacy and safety of curcuminoids in clinical practice: A systematic review and meta-analysis of randomized controlled trials. Pain Med. (United States) 17, 1192–1202 (2016)
N.A. Zabihi, M. Pirro, T.P. Johnston, A. Sahebkar, Is there a role for curcumin supplementation in the treatment of non-alcoholic fatty liver disease? The data suggest yes. Curr Pharm Des. 23, 969–982 (2017)
Y. Panahi, P. Kianpour, R. Mohtashami, R. Jafari, L.E. Simental-Mendía, A. Sahebkar, Efficacy and Safety of Phytosomal Curcumin in Non-Alcoholic Fatty Liver Disease: A Randomized Controlled Trial. Drug Res. 67, 244–251 (2017)
H. Mirzaei, G. Naseri, R. Rezaee, M. Mohammadi, Z. Banikazemi, H.R. Mirzaei, H. Salehi, M. Peyvandi, J.M. Pawelek, A. Sahebkar, Curcumin: A new candidate for melanoma therapy? Int J Cancer. 139, 1683–1695 (2016)
A.A. Momtazi, F. Shahabipour, S. Khatibi, T.P. Johnston, M. Pirro and A. Sahebkar. Curcumin as a MicroRNA regulator in cancer: A review. Rev Physiol Biochem Pharmacol. 171, 1–38 (2016)
M. Iranshahi, A. Sahebkar, M. Takasaki, T. Konoshima, H. Tokuda, Cancer chemopreventive activity of the prenylated coumarin, umbelliprenin, in vivo. Eur J Cancer Prev. 18, 412–415 (2009)
A.A. Momtazi, A. Sahebkar, Difluorinated curcumin: A promising curcumin analogue with improved anti-tumor activity and pharmacokinetic profile. Curr Pharm Des. 22, 4386–4397 (2016)
A. Soltani, A. Salmaninejad, M. Jalili-Nik, A. Soleimani, H. Javid, S.I. Hashemy, A. Sahebkar, 5′-Adenosine monophosphate-activated protein kinase: A potential target for disease prevention by curcumin. J Cell Physiol. 234, 2241–2251 (2019)
R.M. Marjaneh, F. Rahmani, S.M. Hassanian, N. Rezaei, M. Hashemzehi, A. Bahrami, F. Ariakia, H. Fiuji, A. Sahebkar, A. Avan, Phytosomal curcumin inhibits tumor growth in colitis-associated colorectal cancer. J Cell Physiol. 233, 6785–6798 (2018)
D. Lelli, A. Sahebkar, T.P. Johnston, C. Pedone, Curcumin use in pulmonary diseases: State of the art and future perspectives. Pharmacol Res. 115, 133–148 (2017). https://doi.org/10.1016/j.phrs.2016.11.017
L. Wang, B. Zhang, F. Huang, B. Liu, Y. Xie, Curcumin inhibits lipolysis via suppression of endoplasmic reticulum stress in adipose tissue and prevents hepatic insulin resistance. J Lipid Res. 57, 1243–1255 (2016)
N. Parsamanesh, M. Moossavi, A. Bahrami, A.E. Butler, A. Sahebkar, Therapeutic potential of curcumin in diabetic complications. Pharmacol Res. 136, 181–193 (2018)
X. Zhou, J. Zhang, C. Xu, W. Wang, Curcumin ameliorates renal fibrosis by inhibiting local fibroblast proliferation and extracellular matrix deposition. J Pharmacol Sci. 126, 344–350 (2014)
L. Ding, J. Li, B. Song, X. Xiao, B. Zhang, M. Qi, W. Huang, L. Yang, Z. Wang, Curcumin rescues high fat diet-induced obesity and insulin sensitivity in mice through regulating SREBP pathway. Toxicol Appl Pharmacol. 304, 99–109 (2016)
N. Barati, A.A. Momtazi-Borojeni, M. Majeed, A. Sahebkar, Potential therapeutic effects of curcumin in gastric cancer. J Cell Physiol. 234, 2317–2328 (2019)
A. Shakeri, N. Ward, Y. Panahi, A. Sahebkar, Anti-angiogenic activity of curcumin in cancer therapy: a narrative review. Curr Vasc Pharmacol. 17, 262–269 (2019)
M. Hashemzehi, R. Behnam-Rassouli, S.M. Hassanian, M. Moradi-Binabaj, R. Moradi-Marjaneh, F. Rahmani, H. Fiuji, M. Jamili, M. Mirahmadi, N. Boromand, Phytosomal-curcumin antagonizes cell growth and migration, induced by thrombin through AMP-Kinase in breast cancer. J Cell Biochem. 119, 5996–6007 (2018)
L. Hamzehzadeh, S.L. Atkin, M. Majeed, A.E. Butler, A. Sahebkar, The versatile role of curcumin in cancer prevention and treatment: A focus on PI3K/AKT pathway. J Cell Physiol. 233, 6530–6537 (2018)
M. Shanmugam, G. Rane, M. Kanchi, F. Arfuso, A. Chinnathambi, M. Zayed, S. Alharbi, B. Tan, A. Kumar, G. Sethi, The multifaceted role of curcumin in cancer prevention and treatment. Molecules 20, 2728–2769 (2015)
J.G. Devassy, I.D. Nwachukwu, P.J. Jones, Curcumin and cancer: barriers to obtaining a health claim. Nutr Rev. 73, 155–165 (2015)
A. Shehzad, F. Wahid, Y.S. Lee, Curcumin in cancer chemoprevention: molecular targets, pharmacokinetics, bioavailability, and clinical trials. Archiv der Pharmazie 343, 489–499 (2010)
A. Jacob, R. Wu, M. Zhou, P. Wang, Mechanism of the anti-inflammatory effect of curcumin: PPAR-γ activation. PPAR Res. 2007, 89369 (2007)
B.H. Choi, C.G. Kim, Y.-S. Bae, Y. Lim, Y.H. Lee, S.Y. Shin, p21Waf1/Cip1 expression by curcumin in U-87MG human glioma cells: role of early growth response-1 expression. Cancer Res. 68, 1369–1377 (2008)
S.-S. Han, Y.-S. Keum, H.-J. Seo, Y.-J. Surh, Curcumin suppresses activation of NF-κB and AP-1 induced by phorbol ester in cultured human promyelocytic leukemia cells. BMB Rep. 35, 337–342 (2002)
R.L. Thangapazham, A. Sharma, R.K. Maheshwari, Multiple molecular targets in cancer chemoprevention by curcumin. AAPS J. 8, E443 (2006)
S.S. Bhandarkar and J.L. Arbiser, in The molecular targets and therapeutic uses of curcumin in health and disease. (Springer, 2007), p. 185-195
M.S. Squires, E.A. Hudson, L. Howells, S. Sale, C.E. Houghton, J.L. Jones, L.H. Fox, M. Dickens, S.A. Prigent, M.M. Manson, Relevance of mitogen activated protein kinase (MAPK) and phosphotidylinositol-3-kinase/protein kinase B (PI3K/PKB) pathways to induction of apoptosis by curcumin in breast cells. Biochem Pharmacol. 65, 361–376 (2003)
J.H. Seo, K.J. Jeong, W.J. Oh, H.J. Sul, J.S. Sohn, Y.K. Kim, J.K. Kang, C.G. Park, H.Y. Lee, Lysophosphatidic acid induces STAT3 phosphorylation and ovarian cancer cell motility: their inhibition by curcumin. Cancer Lett. 288, 50–56 (2010)
J. Yu, Y. Peng, L.-C. Wu, Z. Xie, Y. Deng, T. Hughes, S. He, X. Mo, M. Chiu, Q.-E. Wang, Curcumin down-regulates DNA methyltransferase 1 and plays an anti-leukemic role in acute myeloid leukemia. PloS one 8, e55934 (2013)
R.J. Anto, A. Mukhopadhyay, K. Denning, B.B. Aggarwal, Curcumin (diferuloylmethane) induces apoptosis through activation of caspase-8, BID cleavage and cytochrome c release: its suppression by ectopic expression of Bcl-2 and Bcl-xl. Carcinogenesis 23, 143–150 (2002)
R. Hayeshi, I. Mutingwende, W. Mavengere, V. Masiyanise, S. Mukanganyama, The inhibition of human glutathione S-transferases activity by plant polyphenolic compounds ellagic acid and curcumin. Food Chem Toxicol. 45, 286–295 (2007)
S. Oetari, M. Sudibyo, J.N. Commandeur, R. Samhoedi, N.P. Vermeulen, Effects of curcumin on cytochrome P450 and glutathione S-transferase activities in rat liver. Biochem Pharmacol. 51, 39–45 (1996)
R. Thapliyal, G. Maru, Inhibition of cytochrome P450 isozymes by curcumins in vitro and in vivo. Food Chem Toxicol. 39, 541–547 (2001)
A.J. Ruby, G. Kuttan, K.D. Babu, K. Rajasekharan, R. Kuttan, Anti-tumour and antioxidant activity of natural curcuminoids. Cancer Lett. 94, 79–83 (1995)
S.M. Plummer, K.A. Holloway, M.M. Manson, R.J. Munks, A. Kaptein, S. Farrow, L. Howells, Inhibition of cyclo-oxygenase 2 expression in colon cells by the chemopreventive agent curcumin involves inhibition of NF-κB activation via the NIK/IKK signalling complex. Oncogene 18, 6013 (1999)
R. Motterlini, R. Foresti, R. Bassi, C.J. Green, Curcumin, an antioxidant and anti-inflammatory agent, induces heme oxygenase-1 and protects endothelial cells against oxidative stress. Free Radic Biol Med. 28, 1303–1312 (2000)
T. Ak, İ. Gülçin, Antioxidant and radical scavenging properties of curcumin. Chem Biol Interact. 174, 27–37 (2008)
K.C. Das, C.K. Das, Curcumin (diferuloylmethane), a singlet oxygen (1O2) quencher. Biochem Biophys Res Commun. 295, 62–66 (2002)
A. Barzegar, A.A. Moosavi-Movahedi, Intracellular ROS protection efficiency and free radical-scavenging activity of curcumin. PLoS One 6, e26012 (2011)
T. Onoue, D. Uchida, N.M. Begum, Y. Tomizuka, H. Yoshida, M. Sato, Epithelial-mesenchymal transition induced by the stromal cell-derived factor-1/CXCR4 system in oral squamous cell carcinoma cells. Int J Oncol. 29, 1133–1138 (2006)
S.W. Pyo, M. Hashimoto, Y.S. Kim, C.H. Kim, S.H. Lee, K.R. Johnson, M.J. Wheelock, J.U. Park, Expression of E-cadherin, P-cadherin and N-cadherin in oral squamous cell carcinoma: correlation with the clinicopathologic features and patient outcome. J Craniomaxillofac Surg. 35, 1–9 (2007)
C.-C. Fan, T.-Y. Wang, Y.-A. Cheng, S.S. Jiang, C.-W. Cheng, A.Y.-L. Lee, T.-Y. Kao, Expression of E-cadherin, Twist, and p53 and their prognostic value in patients with oral squamous cell carcinoma. J Cancer Res Clin Oncol. 139, 1735–1744 (2013)
N.A. Dallas, L. Xia, F. Fan, M.J. Gray, P. Gaur, G. Van Buren, S. Samuel, M.P. Kim, S.J. Lim, L.M. Ellis, Chemoresistant colorectal cancer cells, the cancer stem cell phenotype, and increased sensitivity to insulin-like growth factor-I receptor inhibition. Cancer Res. 69, 1951–1957 (2009)
K.R. Fischer, A. Durrans, S. Lee, J. Sheng, F. Li, S.T. Wong, H. Choi, T. El Rayes, S. Ryu, J. Troeger, Epithelial-to-mesenchymal transition is not required for lung metastasis but contributes to chemoresistance. Nature 527, 472 (2015)
C. Zhang, Y. Xu, H. Wang, G. Li, H. Yan, Z. Fei, Y. Xu, W. Li, Curcumin reverses irinotecan resistance in colon cancer cell by regulation of epithelial–mesenchymal transition. Anticancer Drugs 29, 334–340 (2018)
S. Toden, Y. Okugawa, T. Jascur, D. Wodarz, N.L. Komarova, C. Buhrmann, M. Shakibaei, C.R. Boland, A. Goel, Curcumin mediates chemosensitization to 5-fluorouracil through miRNA-induced suppression of epithelial-to-mesenchymal transition in chemoresistant colorectal cancer. Carcinogenesis 36, 355–367 (2015)
D. Zhang, C. Huang, C. Yang, R.J. Liu, J. Wang, J. Niu, D. Brömme, Antifibrotic effects of curcumin are associated with overexpression of cathepsins K and L in bleomycin treated mice and human fibroblasts. Respir Res. 12, 154 (2011)
A. Bahrami, M. Khazaei, S.M. Hassanian, S. ShahidSales, M. Joudi-Mashhad, M. Maftouh, M.H. Jazayeri, M.R. Parizade, G.A. Ferns, A. Avan, Targeting the tumor microenvironment as a potential therapeutic approach in colorectal cancer: Rational and progress. J Cell Physiol. 233, 2928–2936 (2018)
A. Bahrami, M. Khazaei, F. Bagherieh, M. Ghayour-Mobarhan, M. Maftouh, S.M. Hassanian, A. Avan, Targeting stroma in pancreatic cancer: Promises and failures of targeted therapies. J Cell Physiol. 232, 2931–2937 (2017)
P. Nilendu, S.C. Sarode, D. Jahagirdar, I. Tandon, S. Patil, G.S. Sarode, J.K. Pal, N.K. Sharma, Mutual concessions and compromises between stromal cells and cancer cells: driving tumor development and drug resistance. Cell Oncol. 41, 353–367 (2018)
N. Eiro, L. Gonzalez, A. Martinez-Ordonez, B. Fernandez-Garcia, L.O. Gonzalez, S. Cid, F. Dominguez, R. Perez-Fernandez, F.J. Vizoso, Cancer-associated fibroblasts affect breast cancer cell gene expression, invasion and angiogenesis. Cell Oncol. 41, 369–378 (2018)
M.M. Koczorowska, C. Friedemann, K. Geiger, M. Follo, M.L. Biniossek, O. Schilling, Differential effect of TGFbeta on the proteome of cancer associated fibroblasts and cancer epithelial cells in a co-culture approach - a short report. Cell Oncol. 40, 639–650 (2017)
A. Bahrami, S.M. Hassanian, M. Khazaei, M. Hasanzadeh, S. Shahidsales, M. Maftouh, G.A. Ferns, A. Avan, The therapeutic potential of targeting tumor microenvironment in breast cancer: Rational strategies and recent progress. J Cell Biochem. 119, 111–122 (2018)
M. Vered, D. Dayan, R. Yahalom, A. Dobriyan, I. Barshack, I.O. Bello, S. Kantola, T. Salo, Cancer-associated fibroblasts and epithelial-mesenchymal transition in metastatic oral tongue squamous cell carcinoma. Int J Cancer 127, 1356–1362 (2010)
Y. Jing, Z. Han, S. Zhang, Y. Liu, L. Wei, Epithelial-Mesenchymal Transition in tumor microenvironment. Cell & Bioscience 1, 29 (2011)
C. Buhrmann, P. Kraehe, C. Lueders, P. Shayan, A. Goel, M. Shakibaei, Curcumin suppresses crosstalk between colon cancer stem cells and stromal fibroblasts in the tumor microenvironment: potential role of EMT. PLoS One 9, e107514 (2014)
F.C. Kelleher, Hedgehog signaling and therapeutics in pancreatic cancer. Carcinogenesis 32, 445–451 (2010)
Y. Katoh, M. Katoh, Hedgehog target genes: mechanisms of carcinogenesis induced by aberrant hedgehog signaling activation. Curr Mol Med. 9, 873–886 (2009)
L. Cao, X. Xiao, J. Lei, W. Duan, Q. Ma, W. Li, Curcumin inhibits hypoxia-induced epithelial-mesenchymal transition in pancreatic cancer cells via suppression of the hedgehog signaling pathway. Oncol Rep. 35, 3728–3734 (2016)
J. Dai, K. Ai, Y. Du, G. Chen, Sonic hedgehog expression correlates with distant metastasis in pancreatic adenocarcinoma. Pancreas 40, 233–236 (2011)
A. Bahrami, S.L. Atkin, M. Majeed, A. Sahebkar, Effects of curcumin on hypoxia-inducible factor as a new therapeutic target. Pharmacol Res. 137, 159–169 (2018)
A. Sasco, M. Secretan, K. Straif, Tobacco smoking and cancer: a brief review of recent epidemiological evidence. Lung Cancer 45, S3–S9 (2004)
T. Vu, L. Jin, P. Datta, Effect of cigarette smoking on epithelial to mesenchymal transition (EMT) in lung cancer. J Clin Med. 5, 44 (2016)
Z. Liang, R. Wu, W. Xie, C. Xie, J. Wu, S. Geng, X. Li, M. Zhu, W. Zhu, J. Zhu, Effects of Curcumin on Tobacco Smoke-induced Hepatic MAPK Pathway Activation and Epithelial–Mesenchymal Transition In Vivo. Phytother Res. 31, 1230–1239 (2017)
A.H. Huber, W.I. Weis, The structure of the β-catenin/E-cadherin complex and the molecular basis of diverse ligand recognition by β-catenin. Cell 105, 391–402 (2001)
R. Thakur, D.P. Mishra, Pharmacological modulation of beta-catenin and its applications in cancer therapy. J Cell Mol Med. 17, 449–456 (2013)
E.M. Al-Hujaily, A.G. Mohamed, I. Al-Sharif, K.M. Youssef, P.S. Manogaran, B. Al-Otaibi, A. Al-Haza’a, I. Al-Jammaz, K. Al-Hussein, A. Aboussekhra, PAC, a novel curcumin analogue, has anti-breast cancer properties with higher efficiency on ER-negative cells. Breast Cancer Res Treat. 128, 97–107 (2011)
H.A. Al-Howail, H.A. Hakami, B. Al-Otaibi, A. Al-Mazrou, M.H. Daghestani, I. Al-Jammaz, H.H. Al-Khalaf, A. Aboussekhra, PAC down-regulates estrogen receptor alpha and suppresses epithelial-to-mesenchymal transition in breast cancer cells. BMC Cancer 16, 540 (2016)
P. Paramita, B.W. Wardhani, S.I. Wanandi, M. Louisa, Curcumin for the Prevention of Epithelial-Mesenchymal Transition in Endoxifen-Treated MCF-7 Breast Cancer Cells. Asian Pac J Cancer Prev. 19, 1243 (2018)
J. Xu, D. Liu, H. Niu, G. Zhu, Y. Xu, D. Ye, J. Li, Q. Zhang, Resveratrol reverses Doxorubicin resistance by inhibiting epithelial-mesenchymal transition (EMT) through modulating PTEN/Akt signaling pathway in gastric cancer. Clin Cancer Res. 36, 19 (2017)
W.-C. Chen, Y.-A. Lai, Y.-C. Lin, J.-W. Ma, L.-F. Huang, N.-S. Yang, C.-T. Ho, S.-C. Kuo, T.-D. Way, Curcumin suppresses doxorubicin-induced epithelial–mesenchymal transition via the inhibition of TGF-β and PI3K/AKT signaling pathways in triple-negative breast cancer cells. J Agric Food Chem. 61, 11817–11824 (2013)
R. Bakalova, Z. Zhelev, S. Shibata, B. Nikolova, I. Aoki, T. Higashi, Impressive Suppression of Colon Cancer Growth by Triple Combination SN38/EF24/Melatonin:“Oncogenic” Versus “Onco-Suppressive” Reactive Oxygen Species. Anticancer Res. 37, 5449–5458 (2017)
W. Ren, L. Gao, F. Li, C. Qiang, S. Li, J. Zheng, X. Kong, J. Deng, G. Cai, H. Zhang, Circulating high mobility group AT-hook 2 and pleomorphic adenoma gene 1 in blood of patients with oral squamous cell carcinoma. J Oral Pathol Med. 46, 998–1003 (2017)
Q. Zou, L. Xiong, Z. Yang, F. Lv, L. Yang, X. Miao, Expression levels of HMGA2 and CD9 and its clinicopathological significances in the benign and malignant lesions of the gallbladder. World J Surg Oncol. 10, 92 (2012)
M.J. Scanlan, B. Raj, B. Calvo, P. Garin-Chesa, M.P. Sanz-Moncasi, J.H. Healey, L.J. Old, W.J. Rettig, Molecular cloning of fibroblast activation protein alpha, a member of the serine protease family selectively expressed in stromal fibroblasts of epithelial cancers. Proc Natl Acad Sci USA 91, 5657–5661 (1994)
G.-M. Jiang, W.-Y. Xie, H.-S. Wang, J. Du, B.-P. Wu, W. Xu, H.-F. Liu, P. Xiao, Z.-G. Liu, H.-Y. Li, Curcumin combined with FAPαc vaccine elicits effective antitumor response by targeting indolamine-2, 3-dioxygenase and inhibiting EMT induced by TNF-α in melanoma. Oncotarget 6, 25932 (2015)
M. Iwano, D. Plieth, T.M. Danoff, C. Xue, H. Okada, E.G. Neilson, Evidence that fibroblasts derive from epithelium during tissue fibrosis. J Clin Invest. 110, 341–350 (2002)
R. Kalluri, E.G. Neilson, Epithelial-mesenchymal transition and its implications for fibrosis. J Clin Invest. 112, 1776–1784 (2003)
S. Meran, R. Steadman, Fibroblasts and myofibroblasts in renal fibrosis. Int J Exp Pathol. 92, 158–167 (2011)
M. Zeisberg, J.S. Duffield, Resolved: EMT produces fibroblasts in the kidney. J Am Soc Nephrol. 21, 1247–1253 (2010)
I. Loeffler, G. Wolf, Transforming growth factor-β and the progression of renal disease. Dial Transplant. 29, i37–i45 (2013)
M.R. Farahpour, A. Dilmaghanian, M. Faridy, E. Karashi, Topical Moltkia coerulea hydroethanolic extract accelerates the repair of excision wound in a rat model. Chin J Traumatol. 19, 97–103 (2016)
S.J. Grille, A. Bellacosa, J. Upson, A.J. Klein-Szanto, F. Van Roy, W. Lee-Kwon, M. Donowitz, P.N. Tsichlis, L. Larue, The protein kinase Akt induces epithelial mesenchymal transition and promotes enhanced motility and invasiveness of squamous cell carcinoma lines. Cancer Res. 63, 2172–2178 (2003)
L.-n. Sun, Z.-x. Chen, X.-c. Liu, H.-y. Liu, G.-j. Guan, G. Liu, Curcumin ameliorates epithelial-to-mesenchymal transition of podocytes in vivo and in vitro via regulating caveolin-1. Biomed Pharmacother. 68, 1079–1088 (2014)
F. Galbiati, A.M. Brown, D.E. Weinstein, A. Ben-Ze'ev, R.G. Pestell, M.P. Lisanti, Caveolin-1 expression inhibits Wnt/β-catenin/Lef-1 signaling by recruiting β-catenin to caveolae membrane domains. J Biol Chem. 275, 23368–23377 (2000)
R. Kronstein, J. Seebach, S. Großklaus, C. Minten, B. Engelhardt, M. Drab, S. Liebner, Y. Arsenijevic, A.A. Taha, T. Afanasieva, Caveolin-1 opens endothelial cell junctions by targeting catenins. Cardiovasc Res. 93, 130–140 (2011)
A. Bahrami, S. Shahidsales, M. Khazaei, M. Ghayour-Mobarhan, M. Maftouh, S.M. Hassanian, A. Avan, C-Met as a potential target for the treatment of gastrointestinal cancer: Current status and future perspectives. J Cell Physiol. 232, 2657–2673 (2017)
J.B. Wu, C. Shao, X. Li, Q. Li, P. Hu, C. Shi, Y. Li, Y.-T. Chen, F. Yin, C.-P. Liao, Monoamine oxidase A mediates prostate tumorigenesis and cancer metastasis. J Clin Invest. 124, 2891–2908 (2014)
X. Chen, H. Cheng, T. Pan, Y. Liu, Y. Su, C. Ren, D. Huang, X. Zha, C. Liang, mTOR regulate EMT through RhoA and Rac1 pathway in prostate cancer. Mol Carcinog. 54, 1086–1095 (2015)
S. Cannito, E. Novo, A. Compagnone, L. Valfrè di Bonzo, C. Busletta, E. Zamara, C. Paternostro, D. Povero, A. Bandino, F. Bozzo, Redox mechanisms switch on hypoxia-dependent epithelial–mesenchymal transition in cancer cells. Carcinogenesis 29, 2267–2278 (2008)
M.-H. Yang, K.-J. Wu, TWIST activation by hypoxia inducible factor-1 (HIF-1): implications in metastasis and development. Cell Cycle 7, 2090–2096 (2008)
Z. Liu, J. Liu, L. Zhao, H. Geng, J. Ma, Z. Zhang, D. Yu, C. Zhong, Curcumin reverses benzidine-induced epithelial-mesenchymal transition via suppression of ERK5/AP-1 in SV-40 immortalized human urothelial cells. Int J Oncol. 50, 1321–1329 (2017)
S.M. Sureban, R. May, N. Weygant, D. Qu, P. Chandrakesan, E. Bannerman-Menson, N. Ali, P. Pantazis, C.B. Westphalen, T.C. Wang, XMD8-92 inhibits pancreatic tumor xenograft growth via a DCLK1-dependent mechanism. Cancer Lett. 351, 151–161 (2014)
Z. Liang, L. Lu, J. Mao, X. Li, H. Qian, W. Xu, Curcumin reversed chronic tobacco smoke exposure induced urocystic EMT and acquisition of cancer stem cells properties via Wnt/β-catenin. Cell Death Dis. 8, e3066 (2017)
C. Samanic, M. Kogevinas, M. Dosemeci, N. Malats, F.X. Real, M. Garcia-Closas, C. Serra, A. Carrato, R. García-Closas, M. Sala, Smoking and bladder cancer in Spain: effects of tobacco type, timing, environmental tobacco smoke, and gender. Cancer Epidemiol Biomarkers Prev. 15, 1348–1354 (2006)
W. Zou, Y. Zou, Z. Zhao, B. Li, P. Ran, Nicotine Induced Epithelial-Mesenchymal Transition via Wnt/β-catenin Signaling in Human Airway Epithelial Cells. Am J Physiol Heart Circ Physiol. 304, 199–209 (2012)
S.S. Hecht, Tobacco smoke carcinogens and lung cancer. J Natl Cancer Inst. 91, 1194–1210 (1999)
C.-C. Yu, M.-D. Yang, H.-Y. Lin, A.-C. Huang, J.-P. Lin, C.-L. Kuo, K.-C. Liu, H.-C. Liu, S.-T. Yang, J.-G. Chung, Bisdemethoxycurcumin (BDMC) alters gene expression-associated cell cycle, cell migration and invasion and tumor progression in human lung cancer NCI-H460 cells. In Vivo 29, 711–728 (2015)
G. Hilton, R. Machemer, R. Michels, E. Okun, C. Schepens, A. Schwartz, The classification of retinal detachment with proliferative vitreoretinopathy. Ophthalmology 90, 121–125 (1983)
R.M. Feist, J.L. King, R. Morris, C.D. Witherspoon, C. Guidry, Myofibroblast and extracellular matrix origins in proliferative vitreoretinopathy. Graefes Arch Clin Exp Ophthalmol. 252, 347–357 (2014)
J.G. Garweg, C. Tappeiner, M. Halberstadt, Pathophysiology of proliferative vitreoretinopathy in retinal detachment. Surv Ophthalmol. 58, 321–329 (2013)
P.A. Campochiaro, J.A. Jerdan, B.M. Glaser, A. Cardin, R.G. Michels, Vitreous aspirates from patients with proliferative vitreoretinopathy stimulate retinal pigment epithelial cell migration. Arch Ophthalmol. 103, 1403–1405 (1985)
R. Chaudhary, J. Dretzke, R. Scott, A. Logan, R. Blanch, Clinical and surgical risk factors in the development of proliferative vitreoretinopathy following retinal detachment surgery: a systematic review protocol. Syst Rev. 5, 107 (2016)
S. Ganekal, S. Dorairaj, Effect of intraoperative 5-fluorouracil and low molecular weight heparin on the outcome of high-risk proliferative vitreoretinopathy. Saudi J Ophthalmol. 28, 257–261 (2014)
Funding
This project has been supported by a grant from the Cancer Research Center of the Cancer Institute of Iran (Shams cancer charity, Grant No: 37312-202-01-97). This project was also financially supported by grant No. 960206 of the Biotechnology Development Council of the Islamic Republic of Iran.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
Muhammed Majeed is the founder of Sabinsa Corporation and Sami Labs Ltd. Other authors have no direct competing interests to declare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bahrami, A., Majeed, M. & Sahebkar, A. Curcumin: a potent agent to reverse epithelial-to-mesenchymal transition. Cell Oncol. 42, 405–421 (2019). https://doi.org/10.1007/s13402-019-00442-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13402-019-00442-2