Abstract
Background
An absent left ventricular ejection fraction (LVEF) reserve with vasodilator stress with PET cardiac imaging has been shown to provide significant independent and incremental value to the perfusion images for prediction of future cardiovascular adverse events. However, the prognostic value of LVEF reserve has not been well characterized with SPECT myocardial perfusion imaging (MPI).
Methods
We studied 858 consecutive patients with normal and abnormal perfusion pattern with regadenoson SPECT MPI. Change in LVEF was calculated as post-stress LVEF—rest LVEF. Absent LVEF reserve was defined as a drop in LVEF by 5% or more on the post-stress images. The primary outcome was a composite of cardiac death, non-fatal myocardial infarction and late coronary revascularization.
Results
An absent LVEF reserve was more common in patients with abnormal vs normal MPI (31% vs 19%, P = .001). During a median follow-up of 32 months, the primary outcome was experienced by 31% of the study population. An absent LVEF reserve was not associated with an increased risk of the primary outcome in patients with normal (hazard ratio 1.1, 95% CI .4-2.7, P = .8) or abnormal (.75, .56-1.00, P = .05) MPI. There was no significant correlation between extent of ischemia and post-stress change in LVEF (Pearson r = − .072, P = .07).
Conclusions
In patients undergoing regadenoson SPECT MPI, absent LVEF reserve is not associated with worse cardiac outcomes. Thus, routine reporting of both post-stress and rest LVEF measurements in this setting may not be necessary.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
More than 50% of the 8 million single-photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) studies performed in the USA annually use vasodilator stress agents, most commonly regadenoson, a selective adenosine A2A receptor agonist.1,2 The perfusion pattern and perfusion defect size obtained with regadenoson MPI have been shown to provide powerful diagnostic and prognostic information that can inform patient management.3,4,5,6,7,8,9 In addition to myocardial perfusion, numerous non-perfusion variables have been identified as providing incremental prognostic information.10,11,12
The left ventricular ejection fraction (LVEF) derived from gated regadenoson SPECT MPI is a strong predictor of cardiac death incremental to that of perfusion defect extent and severity.3 Further, severe and extensive myocardial ischemia has been shown to be associated with transient ischemic dilatation (TID), myocardial stunning, and a drop or a lack of augmentation of LVEF post-stress.10,13,14 Absent LVEF reserve (most commonly defined as a drop in LVEF by 5% or more on stress compared to rest imaging) with vasodilator stress using positron emission tomography (PET) has been shown to associate with high-risk coronary artery disease, and it provides significant independent and incremental value to the perfusion images for prediction of future cardiovascular adverse events.15 However, with conventional SPECT MPI, the value of LVEF reserve has not been well characterized. A recent study of patients who underwent regadenoson SPECT MPI and invasive coronary angiography failed to demonstrate an association between absent LVEF reserve and severe/extensive angiographic coronary artery disease (CAD).16 The aim of the current study is to examine the prevalence of an absent LVEF reserve with regadenoson SPECT MPI in patients undergoing clinically indicated studies with normal and abnormal myocardial perfusion, and the association of absent LVEF reserve with cardiovascular risk.
Methods
Study Cohort
A retrospective cohort study design was implemented. The study population consisted of patients who underwent regadenoson MPI at the University of Alabama at Birmingham Nuclear Cardiology Laboratory from July 2008 to January 2010. This cohort has been described in details previously.3,17 Briefly, the cohort consisted of consecutive patients with normal and abnormal myocardial perfusion who underwent regadenoson-rest SPECT MPI. Of the 921 patients, 63 (7%) patients had missing gated data or their images could not be properly gated and therefore were excluded, leaving 858 patients in the analysis. Patient demographics (age, gender, race) and comorbidities (diabetes, hypertension, hyperlipidemia, end-stage renal disease, and coronary revascularization) were obtained via medical record queries. MPI images were retrieved and processed for automated evaluation of parameters of interest: perfusion defect size (PDS), %LV ischemia, TID, post-stress and rest LVEF, post-stress and rest end-diastolic and end-systolic volumes (EDV and ESV, respectively). The clinical reports at our institution routinely report a single assessment of LVEF unless when there is clinical suspicion for myocardial stunning. The study was approved by the institutional board for human research at the University of Alabama at Birmingham.
Myocardial Perfusion Imaging
Regadenoson MPI was performed using standard protocols approved by the American Society of Nuclear Cardiology.18 Details related to stress testing, imaging, and interpretation of images in this study population have been previously described.3,17 All patients underwent both stress and rest imaging, and the vast majority were performed on the same day with stress-first imaging. All stress tests occurred in the absence of exercise. Regadenoson was administered as a 400 µg fixed intravenous bolus followed by 5 mL saline flush. Technetium-99m sestamibi was injected 10-20 seconds later. In general, the stress dose in non-obese patients was 8-12 mCi, and the rest dose 24-36 mCi. SPECT gated images were acquired using a dual-head detector with an elliptical 180° acquisition (45° RAO to 45° LAO) and 8-16 frames per R-R cycle. Stress image acquisition started 30-60 minutes following injection of regadenoson and tracer. Rest imaging was performed if the stress images were abnormal or if there was uncertainty in the interpretation of the stress images. Image analysis was performed using automated software with visual supervision by readers who were blinded to subsequent events as previously described3,17 to characterize PDS, extent, severity, and reversibility at rest. Both sets of gated images were analyzed for LV volumes at end-diastole and end-systole to allow for calculation of LVEF.19 The reader was not blinded to whether the image dataset was from the stress or rest study. TID ratio was calculated as the ratio of LV volume on the summed post-stress images to that on the summed rest images. TID was deemed present when this ratio was ≥ 1.33.17 ΔLVEF was calculated as LVEF on the post-stress images—LVEF on the rest images. Absent LVEF reserve with regadenoson was defined as a drop in LVEF by 5% or more on the post-stress images, i.e., negative ΔLVEF ≥ 5%.
Outcomes
The primary outcome was a composite of cardiac death, myocardial infarction, and late coronary revascularization (CR). Coronary revascularization included both coronary artery bypass grafting and percutaneous coronary intervention. Late coronary revascularization was defined as occurring > 90 days from index MPI. Outcomes were obtained by review of electronic medical records and adjudicated by a blinded reviewer. For those patients whose medical records follow-up was less than two years, scripted telephone interviews were used. Death was verified against the Social Security Death Index database. In cases where the cause of death was unknown, the death was categorized as cardiac.
Statistical Analysis
Statistical analysis was performed using SPSS version 25 for Windows (SPSS Inc., Chicago, Illinois). Continuous variables were presented as mean ± SD or median and interquartile ranges (Q1 to Q3) and compared between the groups using the unpaired t test or Mann-Whitney U test, as appropriate. Discrete variables were presented as frequencies and percentages and compared between the groups using the χ2 test. Survival curves were constructed for patients with and without LVEF reserve using the Kaplan-Meier method, and differences between survival curves were estimated by the log rank test. Survival analysis treated the time of MPI as “time 0.” Estimated risks were reported as hazard ratios and the corresponding 95% confidence interval. All tests were 2-tailed, and a P value of < .05 was considered statistically significant.
Results
Our study cohort consisted of 858 patients with a mean age of 62 years, of which 66% were men, 66% Caucasian, 48% had diabetes, 29% end-stage renal disease, and 46% history of prior coronary revascularization. The cohort included 210 patients with normal perfusion and 648 patients with abnormal perfusion. The characteristics of the cohort according to their perfusion status and presence or absence of LVEF reserve are listed in Table 1.
LVEF Reserve
The median post-stress LVEF was 53% (interquartile range 41% to 63%) and the rest LVEF was 55% (43% to 63%). Median ΔLVEF was − 1% (− 5% to 3%). An absent LVEF reserve post-stress was present in 237 (28%) patients. Any drop in LVEF post stress (i.e., ΔLVEF < 0%) was present in 462 (54%) patients. The characteristics of MPI findings according to patients’ perfusion status and ΔLVEF are shown in Table 2. Absent LVEF reserve was present in 19% of the normal perfusion cohort and 31% of the abnormal perfusion cohort (P = .001). There were no significant differences in the baseline characteristics between those with and without LVEF reserve in both cohorts (Table 1). In the cohort with normal perfusion, patients without LVEF reserve had lower post-stress LVEF and higher rest LVEF compared to those with LVEF reserve. In the cohort with abnormal perfusion pattern, patients without LVEF reserve had higher rest LVEF but similar post-stress LVEF compared to those with LVEF reserve. These patients were more likely to have TID on their perfusion scan (15% vs 5%, P < .001).
Outcomes
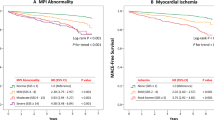
During a median follow-up of 32 months (12 to 45 months), 263 (31%) patients experienced the primary outcome of cardiac death, MI, or late CR. There were 278 (32%) all-cause deaths including 183 (21%) cardiac deaths. 47 (6%) patients experienced MI, and 71 (8%) underwent late CR. In patients with normal perfusion, there was no significant difference in rate of primary outcome between patients with and without LVEF reserve. The hazard ratio for those without LVEF reserve was 1.1 (95% CI .4-2.7), P = .8 (Figure 1A). In patients with abnormal perfusion pattern, there was a non-statistically significant trend towards a lower risk of the primary outcome in patients without LVEF reserve; hazard ratio .75 (.56-1.00), P = .05 (Figure 1B).
Kaplan-Meier survival curves for the composite outcome of cardiac death, MI, and late CR according to LVEF reserve status in patients with normal (A) and abnormal (B) regadenoson SPECT MPI. The association was not statistically significant as indicated by the log rank p value shown on the graph. Absent LVEF reserve with regadenoson was defined as a drop in LVEF by 5% or more on the post-stress images compared to rest images
Myocardial Ischemia and LVEF Reserve
There was no significant correlation between extent of ischemia (%LV) and post-stress ΔLVEF (%), (Pearson r = − .072, P = .07). Within the 648 patients with abnormal perfusion, 370 (57%) patients had large areas of ischemia (defined as ≥ 10% of the LV involved). In this subset, there was no significant difference in rate of primary outcome between the patients with and without LVEF reserve (Figure 2A).
Kaplan-Meier survival curves for the composite outcome of cardiac death, MI, and late CR according to LVEF reserve status in patients with large areas of myocardial ischemia (≥ 10% of the LV) (A) and in those with abnormal regadenoson SPECT MPI in the presence of transient ischemic dilation (TID) (B). The association was not statistically significant as indicated by the log rank P value shown on the graph. Absent LVEF reserve with regadenoson was defined as a drop in LVEF by 5% or more on the post-stress images compared to rest images
Abnormal Rest LVEF and LVEF Reserve
Since the intrinsic variability of repeated measures of LVEF in the abnormal range is narrower than in the normal range,27 we assessed the significance of absent LVEF reserve in patients with abnormal rest LVEF. In our abnormal myocardial perfusion cohort, 298 (46%) patients had a rest LVEF < 50%. In these patients, an absent LVEF reserve was not associated with increased risk of the primary outcome (HR .92, 95%CI .61-1.39, P = .7).
TID and LVEF Reserve
In patients with normal perfusion, there was no significant difference in ΔLVEF between those with TID (1%, interquartile range − 4% to 6%) vs without TID (2%, − 3% to 6%), P = .6. A similar proportion of patients had absent LVEF reserve irrespective of whether they had TID (14% vs 19%, P > .9). In patients with abnormal perfusion, those with TID had a more robust drop in LVEF post-stress (− 6%, − 12 to − 1%), than those without TID (− 2%, − 5% to 2%, P < .001). Significantly more patients with TID had no LVEF reserve than those without TID (54% vs 29%, P < .001). However, even in patients with abnormal perfusion and TID, an absent LVEF reserve was not associated with the primary outcome (Figure 2B).
Discussion
The main aim of this study was to evaluate the association of an absent LVEF reserve with regadenoson technetium-99m sestamibi MPI and future adverse cardiovascular outcomes. An absent LVEF reserve with regadenoson, defined here as a decrease in LVEF by 5% or more on the post-stress images, was present in 28% of our cohort. An absent LVEF reserve was not associated with future cardiac death, MI, or late CR on long-term follow-up. The lack of prognostic value of an absent LVEF reserve was evident in patients with normal myocardial perfusion pattern on imaging, in patients with abnormal myocardial perfusion, in patients with large area of myocardial ischemia, and in patients with abnormal myocardial perfusion and TID. The robustness of this data strengthens the validity of our findings. Further, the lack of association between absent LVEF reserve and adverse cardiac events in patients with normal myocardial perfusion suggests that no further evaluation for obstructive CAD is warranted in these patients. Furthermore, although patients with abnormal myocardial perfusion and TID were more likely to have absence of LVEF reserve, the extent of ischemia did not correlate with post-stress ΔLVEF. This is the first study in the literature examining the association of LVEF reserve with regadenoson (or other vasodilators) on SPECT MPI and outcomes in an unselected population undergoing stress testing for clinical indications.
An earlier study by Gomez et al.16 examined the association of post-stress ΔLVEF with regadenoson with coronary artery disease (CAD) on angiography. Unlike our study, the study by Gomez et al.16 pre-selected patients who underwent invasive coronary angiography within 6 months of MPI. They found that, irrespective of the perfusion pattern on imaging, post-stress decrease in LVEF by 5% (or 10%) was not predictive of severe or extensive CAD in patients who underwent gated SPECT MPI followed by coronary angiography within 6 months. Additionally, these patients were not at increased risk of the composite endpoint of cardiac death, MI or CR. In contrast to these findings, another study utilizing vasodilator (dipyridamole or adenosine) stress 82Rb positron emission tomography (PET) MPI found that an absent LVEF reserve was an independent predictor of left main or 3-vessel CAD.15 Notably, the presence of LVEF reserve with vasodilator PET MPI provides valuable information by excluding left main or 3-vessel CAD noninvasively.
The most likely reason for these conflicting findings is the timing of image acquisition with the different imaging modalities. In the 82Rb PET imaging study, the radionuclide was administered during adenosine infusion or within 3 minutes of dipyridamole administration and image acquisition was started within 90-120 seconds after tracer injection. This likely enabled measurement of LVEF during peak hyperemia. In another cross-sectional, multicenter, international study,20 post-exercise SPECT images were acquired at 15 ± 5 minutes after 99mTc-sestamibi injection; acquisition was repeated at 60 ± 15 minutes after injection. They found that early imaging was more likely to detect reduction in post-stress LVEF, especially in patients with high summed difference scores. The conclusion from these studies is that early post-stress imaging is more likely to detect differences in post-stress ΔLVEF.
Juxtaposed with the previously mentioned sequences, in our study using technetium-99m SPECT MPI, stress image acquisition started 30-60 minutes following injection of vasodilator and tracer. Similarly, images were acquired 45 minutes after stress in the study by Gomez et al..16 It is likely that by the time images in these studies were acquired, ischemia-induced LV dysfunction has largely resolved and thus LVEF has normalized. Evidence of this was noted in another study which evaluated post-stress ΔLVEF obtained using technetium-99m sestamibi high-efficiency SPECT.21 In that study, it was noted that in images obtained within five to nine minutes of regadenoson injection, there was a correlation between myocardial ischemia and reduction in post-stress ΔLVEF. This association became statistically non-significant when imaging was performed starting at 13 minutes and completely absent at 21 minutes. Thus, early imaging during or shortly after peak stress can detect presence or absence of LVEF reserve which provides important prognostic information. However, when imaging is delayed, as is routinely done with SPECT, this association is no longer detected.
Another imaging finding that has been associated with the presence of severe myocardial ischemia is TID.10 Recent studies have reported conflicting findings regarding the prognostic value of TID in the current era.17,22,23,24,25,26 We have previously reported that TID on regadenoson MPI provides incremental prognostic information to myocardial perfusion and LVEF only in patients with abnormal myocardial perfusion pattern on imaging.17 Further, this association was largely driven by late CR with no difference in hard outcomes (cardiac death or non-fatal MI) between patients with or without TID. In this manuscript, we found that TID is associated with a more profound reduction in post-stress ΔLVEF only in patients with abnormal myocardial perfusion on imaging. There was no significant relationship between TID and post-stress ΔLVEF in normal perfusion patients. However, even in patients with abnormal perfusion images and TID, an absent LVEF reserve with regadenoson did not provide prognostic information.
Our findings are subject to all the limitations inherent to single-center retrospective study design. Further, since low-risk patients with stress-only MPIs were systematically excluded from our study, our findings should not be extrapolated to that patient population although changes in LVEF, at least theoretically, should be less profound in lower-risk patients with normal perfusion. Indeed, in our study an absent LVEF reserve was more common in the abnormal myocardial perfusion cohort vs the normal perfusion cohort. All of our patients underwent stress-rest imaging and therefore these findings do not apply to rest-stress imaging, but we have no reason to believe that the sequence of imaging will alter our findings. Our studies were performed using traditional Anger cameras and therefore may not apply to the newer generation cameras that use Cadmium Zinc Telluride (CZT) crystals that provide improved count statistics and special resolution allowing for more accurate LVEF assessment.28 Although image interpretation was done while blinded to subsequent events, bias may have been introduced due to the absence of blinding to patient identification or whether a given study was rest or stress. In addition, our inability to detect an association does not prove the absence of such an association. In this regard, the trend towards decreased cardiovascular risk in patients with an absent LVEF reserve with regadenoson amongst those with an abnormal myocardial perfusion pattern (Figure 1B, P = .05) is paradoxical to our hypothesis, did not meet statistical significance, and is likely due to chance. We are cognizant of the limitation of categorizing a continuous variable such as ΔLVEF into artificial groups (i.e., presence or absence of LVEF reserve). This is particularly important since patients who experience a significant increase in LVEF post-stress may have different outcomes than those without any LVEF change. We therefore reanalyzed our data using patients who experienced an increase in LVEF by 5% or more post-stress as a reference group. In the normal perfusion cohort, the hazard ratio for those without a significant change in LVEF (ΔLVEF between − 4% and 4%) was 1.1 (95%CI .5-2.5, P = .8) and for those with a drop in LVEF by 5% or more post-stress was 1.2 (.4-3.3, P = .8) (Figure 3A). The corresponding hazard ratios for the abnormal perfusion cohort were .9 (.6-1.3, P = .7) and .7 (.5-1.1, P = .1) (Figure 3B), respectively. Finally, when ΔLVEF was analyzed as a continuous variable, there was no significant association with outcomes (hazard ratio 1.0, 95%CI .99-1.0, P = .5).
Kaplan-Meier survival curves for the composite outcome of cardiac death, MI, and late CR in patients with normal (A) and abnormal (B) regadenoson SPECT MPI comparing patients with LVEF reserve (an increase in LVEF by 5% or more post-stress) to those with no change in LVEF post-stress (ΔLVEF between − 4% and 4%) and those with absent LVEF reserve (a drop in LVEF by 5% or more post-stress). The association was not statistically significant as indicated by the log rank p value shown on the graph
It is important to point out that our findings do not negate the real possibility of myocardial stunning with regadenoson that can be detected on routine SPECT MPI (see Bajaj et al.10 for examples from our laboratory), and when this occurs it is usually an indicator of severe ischemia that has persisted for 30-60 minutes and therefore associated with severe and extensive CAD and poor outcomes. Similarly, we cannot completely rule out the possibility of post-stress regional myocardial wall stunning with a compensatory increase in normal segmental wall contraction yielding no net change in global LVEF, nor can we make any determinations on the prognostic significance these changes may portend.
New Knowledge Gained
In patients undergoing regadenoson technetium-99m sestamibi SPECT MPI, an absent LVEF reserve does not portend a worse prognosis. Specifically, it is not associated with future cardiac death, MI, or late CR. This is most likely because the delayed timing of image acquisition in standard gated SPECT MPI protocols allows time for ischemia-induced LV dysfunction to resolve. Thus, routine reporting of both post-stress and rest LVEF measurements in this setting may not be necessary.
Abbreviations
- CAD:
-
Coronary artery disease
- CR:
-
Coronary revascularization
- EDV:
-
End-diastolic volume
- ESV:
-
End-systolic volume
- LVEF:
-
Left ventricular ejection fraction
- MPI:
-
Myocardial perfusion imaging
- PDS:
-
Perfusion defect size
- PET:
-
Positron emission tomography
- SPECT:
-
Single-photon emission computed tomography
- TID:
-
Transient ischemic dilatation
References
2013 Nuclear Cardiology Trend Survey. J Nucl Cardiol 2014;21:S5-88.
Hage FG. Regadenoson for myocardial perfusion imaging: Is it safe? J Nucl Cardiol 2014;21:871-6.
Hage FG, Ghimire G, Lester D, McKay J, Bleich S, El-Hajj S, et al. The prognostic value of regadenoson myocardial perfusion imaging. J Nucl Cardiol 2015;22:1214-21.
Iqbal FM, Hage FG, Ahmed A, Dean PJ, Raslan S, Heo J, et al. Comparison of the prognostic value of normal regadenoson with normal adenosine myocardial perfusion imaging with propensity score matching. JACC Cardiovasc Imaging 2012;5:1014-21.
Shaw LJ, Hage FG, Berman DS, Hachamovitch R, Iskandrian A. Prognosis in the era of comparative effectiveness research: Where is nuclear cardiology now and where should it be? J Nucl Cardiol 2012;19:1026-43.
Iskandrian AE, Bateman TM, Belardinelli L, Blackburn B, Cerqueira MD, Hendel RC, et al. Adenosine versus regadenoson comparative evaluation in myocardial perfusion imaging: Results of the ADVANCE phase 3 multicenter international trial. J Nucl Cardiol 2007;14:645-58.
Cerqueira MD, Nguyen P, Staehr P, Underwood SR, Iskandrian AE, Investigators A-MT. Effects of age, gender, obesity, and diabetes on the efficacy and safety of the selective A2A agonist regadenoson versus adenosine in myocardial perfusion imaging integrated ADVANCE-MPI trial results. JACC Cardiovasc Imaging 2008;1:307-16.
Farzaneh-Far A, Shaw LK, Dunning A, Oldan JD, O’Connor CM, Borges-Neto S. Comparison of the prognostic value of regadenoson and adenosine myocardial perfusion imaging. J Nucl Cardiol 2015;22:600-7.
Ghimire G, Hage FG, Heo J, Iskandrian AE. Regadenoson: A focused update. J Nucl Cardiol 2013;20:284-8.
Bajaj NS, Singh S, Farag A, El-Hajj S, Heo J, Iskandrian AE, et al. The prognostic value of non-perfusion variables obtained during vasodilator stress myocardial perfusion imaging. J Nucl Cardiol 2016;23:390-413.
Hage FG, Dean P, Iqbal F, Heo J, Iskandrian AE. A blunted heart rate response to regadenoson is an independent prognostic indicator in patients undergoing myocardial perfusion imaging. J Nucl Cardiol 2011;18:1086-94.
Andrikopoulou E, Hage FG. Heart rate response to regadenoson: Making the case for its value in clinical practice. J Nucl Cardiol 2016;23:575-80.
Bestetti A, Cuko B, Decarli A, Galli A, Lombardi F. Additional value of systolic wall thickening in myocardial stunning evaluated by stress-rest gated perfusion SPECT. J Nucl Cardiol 2019;26:833-40.
AlJaroudi WA, Hage FG. Myocardial stunning by gated SPECT: An old tool reinvented in a stunning turn. J Nucl Cardiol 2019;26:841-4.
Dorbala S, Vangala D, Sampson U, Limaye A, Kwong R, Di Carli MF. Value of vasodilator left ventricular ejection fraction reserve in evaluating the magnitude of myocardium at risk and the extent of angiographic coronary artery disease: A 82Rb PET/CT study. J Nucl Med 2007;48:349-58.
Gomez J, Golzar Y, Fughhi I, Olusanya A, Doukky R. The significance of post-stress decrease in left ventricular ejection fraction in patients undergoing regadenoson stress gated SPECT myocardial perfusion imaging. J Nucl Cardiol 2018;25:1313-23.
Lester D, El-Hajj S, Farag AA, Bhambhvani P, Tauxe L, Heo J, et al. Prognostic value of transient ischemic dilation with regadenoson myocardial perfusion imaging. J Nucl Cardiol 2016;23:1147-55.
Henzlova MJ, Duvall WL, Einstein AJ, Travin MI, Verberne HJ. ASNC imaging guidelines for SPECT nuclear cardiology procedures: Stress, protocols, and tracers. J Nucl Cardiol 2016;23:606-39.
Germano G, Kiat H, Kavanagh PB, Moriel M, Mazzanti M, Su HT, et al. Automatic quantification of ejection fraction from gated myocardial perfusion SPECT. J Nucl Med 1995;36:2138-47.
Mut F, Giubbini R, Vitola J, Lusa L, Sobic-Saranovic D, Peix A, et al. Detection of post-exercise stunning by early gated SPECT myocardial perfusion imaging: Results from the IAEA multi-center study. J Nucl Cardiol 2014;21:1168-76.
Brodov Y, Fish M, Rubeaux M, Otaki Y, Gransar H, Lemley M, et al. Quantitation of left ventricular ejection fraction reserve from early gated regadenoson stress Tc-99 m high-efficiency SPECT. J Nucl Cardiol 2016;23:1251-61.
Golzar Y, Olusanya A, Pe N, Dua SG, Golzar J, Gidea C, et al. The significance of automatically measured transient ischemic dilation in identifying severe and extensive coronary artery disease in regadenoson, single-isotope technetium-99m myocardial perfusion SPECT. J Nucl Cardiol 2015;22:526-34.
Doukky R, Frogge N, Bayissa YA, Balakrishnan G, Skelton JM, Confer K, et al. The prognostic value of transient ischemic dilatation with otherwise normal SPECT myocardial perfusion imaging: A cautionary note in patients with diabetes and coronary artery disease. J Nucl Cardiol 2013;20:774-84.
Alama M, Labos C, Emery H, Iwanochko RM, Freeman M, Husain M, et al. Diagnostic and prognostic significance of transient ischemic dilation (TID) in myocardial perfusion imaging: A systematic review and meta-analysis. J Nucl Cardiol 2018;25:724-37.
Petretta M, Acampa W, Daniele S, Petretta MP, Nappi C, Assante R, et al. Transient ischemic dilation in SPECT myocardial perfusion imaging for prediction of severe coronary artery disease in diabetic patients. J Nucl Cardiol 2013;20:45-52.
Jameria ZA, Abdallah M, Dwivedi A, Washburn E, Khan N, Khaleghi M, et al. Computer derived transient ischemic dilation ratio for identifying extensive coronary artery disease using a CZT camera and imaging in the upright position. J Nucl Cardiol 2017;24:1702-8.
Wackers FJ, Berger HJ, Johnstone DE, Goldman L, Reduto LA, Langou RA, et al. Multiple gated cardiac blood pool imaging for left ventricular ejection fraction: Validation of the technique and assessment of variability. Am J Cardiol 1979;43:1159-66.
Bailliez A, Blaire T, Mouquet F, Legghe R, Etienne B, Legallois D, et al. Segmental and global left ventricular function assessment using gated SPECT with a semiconductor Cadmium Zinc Telluride (CZT) camera: Phantom study and clinical validation vs cardiac magnetic resonance. J Nucl Cardiol 2014;21:712-22.
Disclosure
Dr. Hage reports research grant support from Astellas Pharma and GE Healthcare. The other authors report no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
All editorial decisions for this article, including selection of reviewers and the final decision, were made by guest editor Saurabh Malhotra, MD, MPH.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Smith, P., Farag, A., Bhambhvani, P. et al. Prognostic value of absent left ventricular ejection fraction reserve with regadenoson SPECT MPI. J. Nucl. Cardiol. 29, 978–986 (2022). https://doi.org/10.1007/s12350-020-02390-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-020-02390-z