Abstract
Background
Transient ischemic dilation (TID) of the left ventricle (LV) has not been validated as a marker of extensive coronary artery disease (CAD) for studies using a cadmium-zinc-telluride (CZT) camera with upright imaging.
Methods
TID ratios were obtained from upright stress and rest images on a CZT camera. Separate cut-off values were determined for exercise and for regadenoson stress. The cutoffs were then applied to 28 patients with extensive CAD and 101 patients without extensive CAD.
Results
With treadmill exercise, an upright TID ratio ≥1.16 provided a positive predictive value of 50% and a negative predictive value of 85.4% for the identification of extensive CAD. In the regadenoson group, an upright TID ratio of 1.29 provided a positive predictive value of 20% and a negative predictive value of 75.9%. Although not an independent predictor of extensive CAD in all subjects, in subjects with a normal upright LVEF, it provided a predictive value by receiver operating characteristics comparable to the SSS.
Conclusions
Increased upright TID measurements on a CZT camera are associated with extensive CAD. The upright TID measurements can serve in an adjunctive role to SSS, and may be most effective in patients with a normal upright exercise LVEF.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Transient ischemic dilation (TID) of the left ventricle (LV) during stress and rest myocardial perfusion imaging (MPI) refers to an imaging pattern in which the LV cavity appears larger on the stress images compared to those at rest without a significant difference in epicardial ventricular size.1 Hypothetical mechanisms to explain the presence of TID include: diffuse subendocardial hypoperfusion, post-stress “myocardial stunning,” and decreased LV function with resultant elevated end-systolic volume.2–5 TID has proven to be a useful diagnostic and prognostic marker of severe and extensive CAD in a variety of patient populations and testing modalities.2,6–11 TID is associated with a poor prognosis even in the presence of normal MPI in patients with diabetes and LV hypertrophy.12–14 Despite its widespread acceptance and use, a recent study has questioned the utility of TID when used with regadenoson SPECT MPI.15
The cut-off value for a “significant” TID ratio varies depending on the stress modality, imaging protocol, and radioisotope used. To date, the authors are aware of no published study identifying a significant cut-off value for TID for upright imaging using the recently introduced dedicated cardiac cameras with solid-state CZT (cadmium-zinc-telluride) detectors. Various studies have validated CZT SPECT MPI in comparison with conventional SPECT, and with coronary angiography.16–18 In this study, we investigated a threshold value for the TID ratio using upright imaging on a CZT SPECT camera and the capability of the upright TID ratio to differentiate extensive CAD from non-extensive CAD.
Method
Study Population
The medical records of 740 patients who underwent either exercise or pharmacologic (regadenoson) SPECT MPI for clinical indications from November 2013 to June 2014 were reviewed. From this cohort, 140 subjects underwent coronary angiography within three months of the stress MPI and were included in the present study, regardless of any past history of coronary revascularization by PCI or CABG. A control group of “exercise normals” consisted of 48 subjects with <5% pretest probability of CAD19 and a normal SPECT MPI study. This was a different group of normal subjects, distinct from the group whose studies had been used to create the locally derived normal MPI SPECT database. A separate set of 14 “pharmacologic normals” was identified by the combination of (1) no history of CAD or documented non-ischemic cardiomyopathy, (2) no angiographic coronary artery stenosis >30% luminal diameter stenosis, (3) a summed stress score (SSS) of 0, and (4) an end-systolic volume ≥20 mL2. This study was approved by the Institutional Review Board of the University of Cincinnati as a retrospective data review and was exempt from informed consent.
Myocardial Perfusion SPECT Imaging
Patients were instructed not to use caffeinated beverages for 12 hours prior to testing. Beta-blockers were withheld for 24 to 48 hours prior to testing if approval to do so was granted by the referring physician. Stress imaging was performed on a treadmill according to the Bruce protocol and/or using pharmacologic stress with regadenoson 0.4 mg.
Stress and rest imaging were performed in the upright position with additional stress images acquired in the supine position. Images were acquired on a D-SPECT CZT dedicated cardiac camera (Spectrum Dynamics Inc., Palo Alto, CA). Upright imaging was performed with the imaging chair at a 65°-70° angle. Breast and/or abdominal binders were used as appropriate to improve image quality. Stress images were acquired for at least 3 minutes at 30-45 minutes following injection of 30-40 mCi of technetium-99 m tetrofosmin. Rest images were acquired for 3-11 minutes based on body weight at 60 minutes following injection of 10-13 mCi of technetium-99 m tetrofosmin.
SPECT images were processed with iterative reconstruction (ordered subset expectation maximization) on a Spectrum Dynamics Cedars View processing station. Physician review and interpretation of the images were accomplished with the Corridor4DM SPECT software (Invia Medical Imaging Solutions, Ann Arbor, Michigan) in blinded fashion without the knowledge of test indication or patients’ clinical data, except gender, height, and weight. Close attention was provided by the nuclear medicine technologist in positioning the base and apex limits to assure the congruence of stress and rest limits. A single additional adjustment was made by the interpreting physician if needed. SSS was recorded from upright and supine positions, summed rest score upright only, upright summed difference score, and average SSS from the average of the upright and supine stress images. TID ratio from the ungated images, rest, and exercise LVEF were automatically calculated by the 4DM SPECT software.
Coronary Angiography
Patients underwent coronary angiography as part of the evaluation for CAD. All the angiography films were blinded for patient’s age, gender, past medical history, presenting symptoms, and stress MPI results. Extensive CAD was defined as an angiographic lesion either ≥50% in the left main, ≥70% in the proximal left anterior descending (LAD) or ≥70% in any two or three epicardial coronary arteries2,10,11.
Statistical Analysis
Continuous variables were described using mean and standard deviation (SD) while categorical data were described using frequency and proportion. Student’s t test was used to determine significant difference between samples for quantitative variables while Fisher’s exact test was used for categorical variables. The unadjusted logistic regression analysis was carried out to determine factors associated with extensive CAD. The multivariable logistic regression analysis was carried out to determine predictors for extensive CAD. The diagnostic performance of the TID ratio in relation to extensive CAD was summarized by receiver operating characteristics (ROC) using the area under the curve (AUC) with 95% confidence intervals (CI). A TID ratio 2SD above the mean for each normal group was used to define separately a cutoff for the prediction of extensive CAD in the exercise and pharmacologic stress study groups. Stepwise multivariable logistic regression was performed for determining adjusted associations. The results of regression analysis were summarized using odds ratio (OR) along with 95% CI and P values. P values <5% were considered significant. The best predictive model was selected based on the highest AUC for the model. ROC curves were constructed for considered tests. All analyses were performed using STATA 12.1.
Results
Characteristics of the 48 exercise normals and the 14 pharmacologic normals are shown in Table 1. Hypertension, beta-blocker use, family history of CAD, and larger TID ratio were more frequent in the pharmacologic controls.
Twenty-eight patients (14.7%) were documented to have extensive CAD and 101 study patients did not. By the univariate analysis, patients with extensive CAD (Table 2) were significantly more likely to be using a beta-blocker, to be dyslipidemic, to have a known history of CAD and/or coronary revascularization, to have undergone pharmacologic stress, and to have a lower stress and rest LVEF. Each of the summed stress scores, summed rest score, summed difference score, and averaged SSS was significantly associated with extensive CAD.
The TID mean ± SD was 0.92 ± 0.12 for exercise controls, 1.03 ± 0.13 for pharmacologic controls, 1.02 ± 0.15 for patients without extensive CAD, and 1.06 ± 0.12 for patients with extensive CAD. The cutoff for an abnormal exercise TID threshold was determined to be ≥1.16, using the mean + 2SD from the exercise controls. An exercise TID cut off of ≥1.16 separated patients with extensive CAD from patients without extensive CAD with a sensitivity of 25%, specificity 94.6%, positive predictive value 50%, and negative predictive value 85.4%. The cutoff for an abnormal pharmacologic TID threshold was determined to be ≥1.29, using the mean + 2SD from the pharmacologic normal subjects. A pharmacologic TID cut off of ≥1.29 separated patients with extensive CAD from patients without extensive CAD with a sensitivity of 5%, specificity 93.8%, positive predictive value 20%, and negative predictive value 75.9%.
The multivariable logistic regression analysis (Table 3) showed hypertension, known history of CAD, history of CABG, resting LVEF, and exercise LVEF to be associated with extensive CAD. After excluding the history of CAD and coronary revascularization, hyperlipidemia (OR: 4.2, 95% CI 1.4-12.9, P = 0.012) and upright exercise LVEF (OR 0.95, 95% CI 0.91-0.98, P = 0.003) remained significantly associated with extensive CAD. The average SSS was the most predictive of the 5 summed scores analyzed (AUC 0.0.69, 95% CI 0.58-0.80). Average SSS was independently predictive of extensive CAD only after subjects with a resting upright LVEF <50% were excluded. For the full study population, TID was not an independent predictor of extensive CAD.
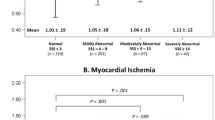
Individual and combined model performance of TID, average SSS, and upright stress LVEF are shown in Table 4 and Figure 1. The combined model of average SSS and upright stress LVEF provided best predictive ability for extensive CAD (AUC = 0.732) followed by a model with TID and upright stress LVEF (AUC = 0.706). The given equations in Table 4 can be used for predicting likelihood of extensive CAD compared with no extensive CAD. When patients with a normal exercise LVEF were considered, average SSS and TID provided comparable prediction of extensive CAD.
(A) Receiver operating characteristics (ROC) curves for prediction of extensive coronary artery disease for TID, average SSS, and upright exercise left ventricular ejection fraction. (B) Receiver operating characteristics (ROC) curves for the prediction of extensive coronary artery disease for the combinations of TID and exercise left ventricular ejection fraction
An infrequent but clinically very important issue is the identification of patients who may have extensive CAD with no regional perfusion abnormality (i.e., “balanced ischemia”). In the present population, no patient with extensive CAD and a normal (<4) summed stress score had a TID ratio ≥1.16.
Discussion
TID has long been used to identify patients with multi-vessel or extensive CAD, who are at increased risk of adverse cardiovascular events. Abnormal TID ratios have been published previously using specific camera and testing protocols8. However, to date, no validated TID ratio cutoff has been published for upright imaging on a CZT camera. As in previous studies, the present study defined an abnormal treadmill exercise only TID cutoff based on a value that is 2SD above the mean TID of a population of subjects with a very low pretest likelihood that coronary disease is present7,10,11,14,15. The resultant TID ratio cutoff in the present study was 1.16, which provided a positive predictive value of 50% and a negative predictive value of 85.4% in differentiating patients with extensive CAD from those without. As noted previously15, very few subjects who are referred for pharmacologic stress MPI have a pretest likelihood of CAD <5%. Consistent with a previous report15, pharmacologic stress control subjects were identified for the present study based on a low likelihood of CAD from historical and clinical variables. Thus, the pharmacologic normal group for the present study was identified by a SSS of 0, no known coronary disease or history of revascularization, no documented lesion >30% by subsequent coronary angiography, no documented non-ischemic cardiomyopathy, and no end-systolic volume less than 20 mL. A TID cut-off value of 1.29 for subjects who underwent pharmacologic stress was based on a value 2SD above the mean of the 14 pharmacologic controls. A cutoff of 1.29 yielded a positive predictive value of 20% and a negative predictive value of 75.9% for the identification of extensive CAD.
The SSS is an index that reflects both extent and severity of CAD. In the present study the optimal SSS for identifying extensive CAD was the average of the upright and supine SSS; however, the upright SSS alone was also predictive. The SSS has served as a marker for extensive angiographic CAD and for high risk for cardiac death or myocardial infarction in previously published studies20,21. On the multivariable analysis, the average SSS was an independent predictor of extensive CAD, but only after the clinical variables, known CAD, PCI, and CABG, and an exercise LVEF <50% were removed. By the multivariable analysis, the TID ratio was not an independent predictor of extensive CAD.
The TID ratio is automatically computed by most MPI analysis programs and serves in an adjunctive role for the identification of extensive CAD. This adjunctive role reflects limited sensitivity of the TID ratio for the identification of extensive CAD, varying from 15% to 28% in published series when severe coronary artery stenosis is defined as a ≥70% luminal narrowing9,11. When a more conservative 90% stenosis is required to define a significant stenosis to extensive or multi-vessel CAD, higher sensitivity of the TID ratio has been described7. In the present study a significant stenosis was defined as 70% and the prospectively defined TID ratio of 1.16 also provided the optimal combination of sensitivity and specificity (i.e., diagnostic accuracy) by the ROC analysis (data not shown). Attempts to use a lower TID cutoff to improve sensitivity are limited by a resultant decline in specificity, as increasing TID has been shown in response to hypertension13,22, diabetes13,14, gender23, small left ventricular volumes2, change in heart rate from rest to post-stress image acquisition24, and patient motion25.
Compared to the mean TID ratio with exercise stress testing, the mean TID ratio with pharmacologic stress testing was higher for both patients with and without extensive CAD, which is in agreement with previously published findings8. Overall exercise TID was found to be superior to pharmacologic TID for the separation of patients with vs without extensive CAD.
Although an upright TID ratio was automatically provided by the commercial software used in the present study, little attention in the literature has been addressed to the role of an upright TID ratio in identifying extensive CAD. Past studies with first pass angiocardiography documented that left ventricular volumes in the upright position differ in the response to exercise between subjects with CAD and normal subjects26. In the present study, an upright TID ratio cutoff was identified that separated patients with extensive CAD from normal subjects and patients with less extensive disease; however, much of the information from the TID ratio for the identification of patients with extensive CAD was also available from historical and clinical variables and from the SSS.
Golzar and associates15 recently described limited utility of the TID ratio for separating patients with extensive vs non-extensive CAD using regadenoson coronary vasodilation, a conventional SPECT camera system, and supine imaging. They questioned the utility of the TID ratio for the assessment of CAD severity and extent in an era of decreasing prevalence of extensive CAD. Findings of the present study are in agreement with that report.
Findings from the present study are limited to patients from a single center, the upright position, and using a CZT camera with analysis on a single software system. The TID ratio cutoff in the present study is not intended to apply to images acquired on a CZT camera using the supine position. In addition, as is common practice to reduce interference with myocardial images from adjacent activity in digestive organs27, adjunctive exercise was added to pharmacologic stress in patients who were able to perform low-level treadmill exercise.
New Knowledge Gained
The present study provides validation for exercise and pharmacologic stress cutoff TID ratios for the identification of patients with vs without extensive CAD as determined by upright imaging on a CZT cardiac camera.
Conclusion
Increased upright TID measurements on a CZT camera are associated with extensive CAD. The upright TID measurements can serve in an adjunctive role to SSS, and may be most effective in patients with a normal upright exercise LVEF.
Abbreviations
- AUC:
-
Area under the curve
- CABG:
-
Coronary artery bypass surgery
- CAD:
-
Coronary artery disease
- CZT:
-
Cadmium-zinc-telluride
- LV:
-
Left ventricle
- LVEF:
-
Left ventricular ejection fraction
- MPI:
-
Myocardial perfusion imaging
- PCI:
-
Percutaneous coronary intervention
- SPECT:
-
Single-photon emission computerized tomography
- SSS:
-
Summed stress score
- TID:
-
Transient ischemic dilation
References
McLaughlin MG, Danias PG. Transient ischemic dilation: A powerful diagnostic and prognostic finding of stress myocardial perfusion imaging. J Nucl Cardiol 2002;9:663–7.
Mazzanti M, Germano G, Kiat H, Kavanagh PB, Alexanderson E, Friedman JD, et al. Identification of severe and extensive coronary artery disease by automatic measurement of transient ischemic dilation of the left ventricle in dual-isotope myocardial perfusion SPECT. J Am Coll Cardiol 1996;27:1612–20.
Johnson LL, Verdesca SA, Aude WY, Xavier RC, Nott LT, Campanella MW, et al. Postischemic stunning can affect left ventricular ejection fraction and regional wall motion on post-stress gated sestamibi tomograms. J Am Coll Cardiol 1997;30:1641–8.
Emmett L, Ng A, Ha L, Russo R, Mansberg R, Zhao W, et al. Comparative assessment of rest and post-stress left ventricular volumes and left ventricular ejection fraction on gated myocardial perfusion imaging (MPI) and echocardiography in patients with transient ischaemic dilation on adenosine MPI: Myocardial stun. J Nucl Cardiol 2012;19:735–42.
Van Tosh A, Hecht S, Berger M, Roberti R, Luna E, Horowitz SF. Exercise echocardiographic correlates of transient dilatation of the left ventricular cavity on exercise thallium-201 SPECT imaging. Chest 1994;106:1725–9.
Iskandrian AS, Heo J, Nguyen T, Lyons E, Paugh E. Left ventricular dilatation and pulmonary thallium uptake after single-photon emission computer tomography using thallium-201 during adenosine-induced coronary hyperemia. Am J Cardiol 1990;66:807–11.
Abidov A, Bax JJ, Hayes SW, Cohen I, Nishina H, Yoda S, et al. Integration of automatically measured transient ischemic dilation ratio into interpretation of adenosine stress myocardial perfusion SPECT for detection of severe and extensive CAD. J Nucl Med 2004;45:1999–2007.
Abidov A, Germano G, Berman DS. Transient ischemic dilation ratio: A universal high-risk diagnostic marker in myocardial perfusion imaging. J Nucl Cardiol 2007;14:497–500.
Katz JS, Ruisi M, Giedd KN, Rachko M. Assessment of transient ischemic dilation (TID) ratio in gated SPECT myocardial perfusion imaging (MPI) using regadenoson, a new agent for pharmacologic stress testing. J Nucl Cardiol 2012;19:727–34.
Xu Y, Arsanjani R, Clond M, Hyun M, Lemley M Jr, Fish M, et al. Transient ischemic dilation for coronary artery disease in quantitative analysis of same-day sestamibi myocardial perfusion SPECT. J Nucl Cardiol 2012;19:465–73.
Petretta M, Acampa W, Daniele S, Petretta MP, Nappi C, Assante R, et al. Transient ischemic dilation in SPECT myocardial perfusion imaging for prediction of severe coronary artery disease in diabetic patients. J Nucl Cardiol 2013;20:45–52.
Emmett L, Magee M, Freedman SB, Van der Wall H, Bush V, Trieu J, et al. The role of left ventricular hypertrophy and diabetes in the presence of transient ischemic dilation of the left ventricle on myocardial perfusion SPECT images. J Nucl Med 2005;46:1596–601.
Emmett L, Van Gaal WJ, Magee M, Bass S, Ali O, Freedman SB, et al. Prospective evaluation of the impact of diabetes and left ventricular hypertrophy on the relationship between ischemia and transient ischemic dilation of the left ventricle on single-day adenosine Tc-99 m myocardial perfusion imaging. J Nucl Cardiol 2008;15:638–43.
Doukky R, Frogge N, Bayissa YA, Balakrishnan G, Skelton JM, Confer K, et al. The prognostic value of transient ischemic dilatation with otherwise normal SPECT myocardial perfusion imaging: A cautionary note in patients with diabetes and coronary artery disease. J Nucl Cardiol 2013;20:774–84.
Golzar Y, Olusanya A, Pe N, Dua SG, Golzar J, Gidea C, et al. The significance of automatically measured transient ischemic dilation in identifying severe and extensive coronary artery disease in regadenoson, single-isotope technetium-99 m myocardial perfusion SPECT. J Nucl Cardiol 2015;22:526–34.
Gambhir SS, Berman DS, Ziffer J, Nagler M, Sandler M, Patton J, et al. A novel high-sensitivity rapid-acquisition single-photon cardiac imaging camera. J Nucl Med 2009;50:635–43.
Sharir T, Ben-Haim S, Merzon K, Prochorov V, Dickman D, Ben-Haim S, et al. High-speed myocardial perfusion imaging. Initial clinical comparison with conventional dual detector anger camera imaging. JACC Cardiovasc Imaging 2008;1:156–63.
Duvall WL, Sweeny JM, Croft LB, Barghash MH, Kulkarni NK, Guma KA, et al. Comparison of high efficiency CZT SPECT MPI to coronary angiography. J Nucl Cardiol 2011;18:595–604.
Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med 1979;300:1350–8.
Hachamovitch R, Berman DS, Shaw LJ, Kiat H, Cohen I, Cabico JA, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: Differential stratification for risk of cardiac death and myocardial infarction. Circulation 1998;97:535–43.
Amanullah AM, Berman DS, Hachamovitch R, Kiat H, Kang X, Friedman JD. Identification of severe or extensive coronary artery disease in women by adenosine technetium-99 m sestamibi SPECT. Am J Cardiol 1997;80:132–7.
Smelley MP, Virnich DE, Williams KA, Ward RP. A hypertensive response to exercise is associated with transient ischemic dilation on myocardial perfusion SPECT imaging. J Nucl Cardiol 2007;14:537–43.
Rivero A, Santana C, Folks RD, Esteves F, Verdes L, Esiashvili S, et al. Attenuation correction reveals gender-related differences in the normal values of transient ischemic dilation index in rest-exercise stress sestamibi myocardial perfusion imaging. J Nucl Cardiol 2006;13:338–44.
van der Veen BJ, Kuperij N, Stokkel MPM. Transient ischemic dilation ratio derived from myocardial perfusion scintigraphy: What are we looking at? J Nucl Cardiol 2010;17:207–15.
Fitzgerald J, Danias PG. Effect of motion on cardiac SPECT imaging: Recognition and motion correction. J Nucl Cardiol 2001;8:701–6.
Rerych SK, Scholz PM, Newman GE, Sabiston DC Jr, Jones RH. Cardiac function at rest and during exercise in normals and in patients with coronary heart disease. Evaluation by radionuclide angiocardiography. Ann Surg 1978;187:449–63.
Thomas GS, Thompson RC, Miyamoto MI, Ip TK, Rice DL, Milikien D, et al. The RegEx trial: A randomized, double-blind, placebo- and active-controlled pilot study combining regadenoson, a selective A2A adenosine agonist, with low-level exercise, in patients undergoing myocardial perfusion imaging. J Nucl Cardiol 2009;16:63–72.
Disclosure
This work was funded by the John R. Strauss Fund for Research and Education in Cardiac Imaging, Cincinnati, Ohio.
Author information
Authors and Affiliations
Corresponding author
Additional information
See related editorial, doi:10.1007/s12350-016-0582-4.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jameria, Z.A., Abdallah, M., Dwivedi, A. et al. Computer derived transient ischemic dilation ratio for identifying extensive coronary artery disease using a CZT camera and imaging in the upright position. J. Nucl. Cardiol. 24, 1702–1708 (2017). https://doi.org/10.1007/s12350-016-0515-2
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-016-0515-2