Abstract
Background
Regadenoson is now widely used in single-photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI). However, the prognostic value of abnormal stress perfusion findings with regadenoson vs adenosine are unclear. The aim of this study was to evaluate the prognostic value of regadenoson SPECT and to compare it to that of adenosine SPECT.
Methods and Results
3698 consecutive patients undergoing either adenosine or regadenoson SPECT were assessed at 1 year for the endpoints of cardiovascular death and a composite endpoint of cardiovascular death or MI. Weighted Cox proportional hazards regression modeling with the inverse probability weighted (IPW) estimators method adjusting to propensity for agent was used to account for differences in baseline characteristics. Patients undergoing adenosine SPECT MPI had a significantly higher prevalence of smoking history, diabetes, hypertension, and prior myocardial infarction (P < .05, all). At 1 year of follow-up, there were 154 cardiovascular deaths and 204 with the composite endpoint of cardiovascular death or MI. Using IPW adjustment to propensity for agent in a model with stress agent, summed stress score (SSS) remained a significant predictor of the composite endpoint of cardiovascular death or MI (HR 1.36 CI 1.28-1.46; P < .0001) as well as cardiovascular death (HR 1.38 CI 1.28-1.49; P < .0001). The interaction of SSS with agent was not significant. Similar findings were seen with summed difference score (SDS).
Conclusions
SSS derived from either adenosine or regadenoson SPECT MPI is a significant predictor of events and provides incremental prognostic information beyond basic clinical variables. We have shown for the first time that use of regadenoson vs adenosine as stress agent does not modify the prognostic significance of SSS. Similar findings were seen with SDS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Single-photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) is widely used for risk stratification of patients with known or suspected coronary artery disease.1-4 In the United States, the majority of these procedures are performed with vasodilator stress. Traditionally, this was with the non-selective vasodilator agents - adenosine and dipyridamole, which have a significant body of published prognostic data.5-7 Regadenoson is a selective adenosine A2A receptor agonist and is now the stress agent most widely used in the United States.8,9 Unlike adenosine, regadenoson is given as a bolus rather than as an infusion, simplifying the testing protocol and is better-tolerated.9 Although randomized phase 3 multicenter trials have demonstrated that regadenoson is noninferior to adenosine for the detection of reversible perfusion abnormalities, there are limited data on risk prediction.10-12 Recently, Iqbal and colleagues demonstrated a similarly low rate of major cardiac events following a normal regadenoson or adenosine stress.8 However, the relative prognostic value of abnormal stress perfusion findings with regadenoson vs adenosine is unclear. In clinical practice, abnormal regadenoson MPI results are presumed to provide similar prognostic information as those performed with adenosine despite different mechanisms of action, pharmacodynamics, and pharmacokinetics. Therefore, given the widespread use of regadenoson it is critical to assess its prognostic performance against adenosine.
Methods
Study Participants
In this study, 3698 consecutive patients undergoing either adenosine (n = 1737) or regadenoson (n = 1961) SPECT MPI between 2005 and 2011 at Duke University hospital were identified from the Duke Nuclear Cardiology Databank. Adenosine was the agent used initially; but after approval of regadenoson at Duke University hospital, all studies were switched to regadenoson. The study protocol was reviewed and approved by the local Institutional Review Board.
Clinical Variables
Demographic and clinical characteristics were recorded prospectively at the time of MPI. This included: age, sex, race, hypertension, diabetes, smoking history, hyperlipidemia, cardiac medications, and prior myocardial infarction.
Pharmacological Stress Test and Imaging
MPI was performed according to previously described Duke University nuclear laboratory protocols.13,14 In brief, SPECT images were obtained with multi-head detectors with 30 s/projection at rest and 20 s/projection during stress. Whenever possible, β-blockers and calcium channel antagonists were terminated 48 hours before testing and nitrates at least 6 hours before testing. No caffeine intake was permitted <12 hours before the stress test. Heart rate, blood pressure, and electrocardiogram were monitored throughout the procedure. Adenosine (Adenoscan; Fujisawa Healthcare, Deerfield, IL) was administered as an infusion (140 mcg/kg/min for 6 minutes). The radionuclide perfusion agent was injected 3 minutes into the infusion. Regadenoson (Lexiscan; Astellas Pharma, Northbrook, IL) was administered as a single peripheral intravenous bolus of 0.4 mg, followed by a saline flush. The radionuclide perfusion agent was injected 30 seconds after the saline flush.
Image Analysis
The MPS studies were evaluated semi-quantitatively for severity and extent of abnormalities with relative perfusion recorded in each myocardial segment (0 = no defect, 1 = mild defect, 2 = moderate defect, and 3 = severe defect) at rest and during stress. The summed stress score (SSS) and summed difference score (SDS) were determined for each patient. The Duke Nuclear Cardiology Databank has used a 4-point severity scale since its inception and was initiated prior to the current American Society of Nuclear Cardiology recommended 5-point scale. We have kept the same system of scoring in order to maintain consistency throughout our database over time. At the time these data were collected, we used a 12-segment model. We used a previously reported algorithm for conversion of 12-segment perfusion scores to 17-segment scores, which is highly correlated with expert reading of the same studies by the 17-segment model.15 Thus, we have a robust method for converting 12- into 17-segment data.
Follow-Up
Patients were followed for 12 months to assess for the primary endpoints of cardiovascular death and a composite endpoint of cardiovascular death or MI. Patients were not censored for revascularization. Outcomes were obtained from the Duke Databank for Cardiovascular Disease, the social security death index, death certificates, hospital records, patient interviews, and mailed questionnaires. Cardiovascular death included death resulting from an acute myocardial infarction, sudden cardiac death, death due to heart failure, and death due to stroke. Two independent blinded data abstractors adjudicated deaths and their causes. When death certificates were not available, cause of death was adjudicated using data from telephone interviews with family members, and hospital discharge summaries. Occurrence of myocardial infarction was systematically determined using telephone and mailed questionnaires as well as review of hospital records by blinded adjudicators. Diagnosis of myocardial infarction was based on the presence of two of the following three features: symptoms of myocardial ischemia, elevation of cardiac enzymes, and typical ECG changes.
Statistical Analysis
Differences in baseline characteristics were compared between the regadenoson and adenosine groups. The t test or Wilcoxon rank test was used to compare continuous data and the χ 2 statistic to compare discrete data. Outcomes of the regadenoson group were compared with those of the adenosine group. To determine the relationship, if any between SSS and outcomes, several Cox regression analyses were conducted. First, univariable cox regression was used to look at the unadjusted relationship of SSS with outcomes. Then, a multivariable cox regression analysis was used to look at the relationship between SSS and outcomes, adjusting for a list of pre-specified clinical variables (age, sex, race, diabetes, hypertension, hyperlipidemia, smoking, and history of MI). In both models, stress agent was ignored and Inverse Probability Weighting (IPW) methods were not applied. Stabilized IPW was subsequently used to account for non-randomization to stress agent in this observational study.16,17 A logistic regression analysis was applied to estimate the propensity of regadenoson use, conditioned on a pre-specified list of clinical covariates (same variables as in the multivariable cox regression model above). The inverses of these propensities were used as weights in a Cox regression analysis looking at the relationship of SSS with outcomes while adjusting for stress agent. Thus, IPW was only used in the stress agent adjusted model. Similar analyses were performed for SDS. All statistical test were 2-tailed and P < .05 was considered statistically significant. SAS version 9.2 (SAS Institute Inc) was used to perform the statistical analyses.
Results
Baseline Characteristics
The total cohort in this analysis included 3698 patients; 1737 underwent stress imaging with adenosine, whereas 1961 underwent the study with regadenoson. As shown in Table 1, the patients were mostly Caucasian (60%), and a significant percentage had risk factors for coronary artery disease, including hypertension (85%), smoking (47%), hyperlipidemia (70%), and diabetes (45%). Overall, 16% of patients had a history of MI, 18% had prior PCI, and 16% had prior CABG. The patients undergoing SPECT MPI with adenosine were more likely to be male, and had a significantly higher prevalence of smoking history, diabetes, hypertension, and prior myocardial infarction (P < .05, all). These patients were also significantly more likely to be on ACE-inhibitors, β-blockers, and nitrates. The mean SSS was significantly higher in studies where adenosine was used compared with regadenoson (14.4 vs 8.9, P < .001). However, there was no significant difference in baseline clinical variables (age, sex, race, diabetes, hypertension, hyperlipidemia, smoking, and history of MI) between the adenosine and regadenoson groups after IPW adjustment (Supplementary Appendix—Table 4).
Primary Outcomes
At 12 months of follow-up, the composite endpoint of cardiovascular death or MI occurred in 96 patients in the regadenoson group and 108 patients in the adenosine group. The endpoint of cardiovascular death occurred in 73 patients in the regadenoson group and 81 patients in the adenosine group.
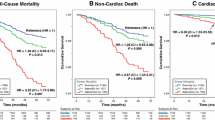
Comparative Outcomes of IPW Adjusted Adenosine and Regadenoson Groups
Outcomes of the regadenoson group were compared with those of the adenosine group. Figure 1 shows Kaplan-Meier curves (IPW adjusted to clinical variables of age, sex, race, diabetes, hypertension, hyperlipidemia, smoking, and history of MI) for each group for the composite endpoint of cardiovascular death or MI. Figure 2 shows Kaplan-Meier curves (IPW adjusted to clinical variables) for each group for the outcome of cardiovascular death. Similarly, Kaplan-Meier curves, (IPW adjusted to clinical variables) and stratified by SSS (SSS ≤ 3 vs >3) showed no significant difference between agents for the composite endpoint of cardiovascular death or MI in patients with SSS ≤ 3 (P = .24) or SSS > 3 (P = .60). Interaction of SSS with agent was not significant (P = .35) (Supplementary Appendix—Figures 3). Likewise, Kaplan-Meier curves, (IPW adjusted to clinical variables) and stratified by SSS (SSS ≤ 3 vs >3) showed no significant difference between agents for the endpoint of cardiovascular death with SSS ≤ 3 (P = .54) or SSS > 3 (P = .86). Interaction of SSS with agent was not significant (P = .63) (Supplementary Appendix—Figures 4).
Multivariable Analyses
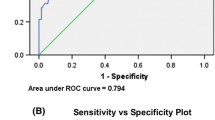
Cardiovascular death or myocardial infarction
SSS (HR per 5% 1.36 CI 1.27-1.45; P < .0001) was a significant predictor of the composite endpoint of cardiovascular death or MI in unadjusted analyses. SSS remained a significant predictor after adjustment to pre-specified clinical variables (age, sex, race, diabetes, hypertension, hyperlipidemia, smoking, and history of MI) in a multivariable Cox regression analysis—(HR per 5% 1.30 CI 1.20-1.40; P < .0001). Using IPW adjustment to propensity for agent in a Cox regression model with stress agent, SSS (HR 1.36 CI 1.28-1.46; P < .0001) remained a significant predictor of the composite endpoint of cardiovascular death or MI (Table 2). The interaction of SSS with agent was not significant (P = .35) in this setting.
Similarly, SDS was a significant predictor of the composite endpoint of cardiovascular death or MI in unadjusted analyses as well as when adjusted to pre-specified clinical variables in a multivariable Cox regression analysis. Likewise, after IPW adjustment to propensity for agent in a Cox regression model with stress agent, SDS (HR 1.61 CI 1.38-1.88; P < .0001) remained a significant predictor of the composite endpoint of cardiovascular death or MI (Table 2).
Cardiovascular death
SSS (HR per 5% 1.38 CI 1.28-1.48; P < .0001) was a significant predictor of cardiovascular death in unadjusted analyses. SSS remained a significant predictor after adjustment to pre-specified clinical variables (age, sex, race, diabetes, hypertension, hyperlipidemia, smoking, and history of MI) in a multivariable Cox regression analysis—(HR per 5% 1.33 CI 1.23-1.45; P < .0001). Using IPW adjustment to propensity for agent in a Cox regression model with stress agent, SSS (HR 1.38 CI 1.28-1.49; P < .0001) remained a significant predictor of cardiovascular death (Table 3). The interaction of SSS with agent was not significant (P = .63) in this setting.
Similarly, SDS was a significant predictor of cardiovascular death in unadjusted analyses as well as when adjusted to pre-specified clinical variables in a multivariable Cox regression analysis. Likewise, after IPW adjustment to propensity for agent in a Cox with stress agent, SDS (HR 1.46, CI 1.22-1.75; P < .0001) remained a significant predictor of cardiovascular death (Table 3).
Discussion
In this cohort of patients undergoing regadenoson or adenosine SPECT, SSS is an independent predictor of the primary endpoints of cardiovascular death and a composite endpoint of cardiovascular death or MI, independent of the type of vasodilator agent used. Moreover, there was no significant interaction in the adjusted multivariable models between stress agent and SSS for either endpoint. These findings suggest that use of regadenoson or adenosine as vasodilator agent does not modify the prognostic significance of SSS. Similar findings were seen with SDS. To the best of our knowledge, this is the first study to assess the prognostic value of abnormal regadenoson SPECT MPI.
The adenosine group had a significantly higher risk factor profile at baseline. The reasons for this are unclear but maybe related to temporal trends in SPECT MPI referrals, since our regadenoson studies were performed more recently. Rozanski and colleagues showed a marked progressive decline in abnormal SPECT MPI between 1991 and 2009 in 39,515 consecutive patients from Cedars-Sinai Medical Center.18 The declining frequency of abnormal SPECT MPI was accompanied by a progressive decline in several baseline risk factors. Iqbal et al also noted a similar trend with a higher risk profile in patients undergoing SPECT MPI with adenosine compared to regadenoson.8 One can speculate that changes in many other factors within our hospital may have contributed to this e.g., hiring of new faculty, addition of an extra outpatient nuclear camera, or increased use of stress testing by primary care physicians. In addition, changes in practice patterns and greater availability of other modalities likely impacted the referral population e.g., greater use of stress magnetic resonance imaging and fractional flow reserve.19-22 However, there were no changes in data documentation, electronic medical record system, or methods of documenting clinical history. Moreover, the patients were all derived from a single academic medical center.
In this study, we used Inverse probability weighted (IPW) estimators to correct for baseline differences between the two groups. IPW estimators are a type of propensity adjusted method that is becoming increasingly popular for use in observational studies—particularly those with a survival endpoint.16,17 This method is considered advantageous to simple baseline covariate adjustment with Cox regression, as it tries to mimic a randomized controlled trial environment. Specifically, it has the ability to balance the distribution of two non-randomized treatment groups, conditional on a set of covariates. While propensity score matching can be used in a similar fashion, the IPW method has the advantage of being more flexible and can be easily used to create adjusted Kaplan-Meier survival curves by treatment group.
Both adenosine and regadenoson induce coronary arteriolar vasodilation through activation of the A2A adenosine receptor—a powerful physiological regulator of coronary blood flow.9 Regadenoson is a selective adenosine A2A receptor agonist that has significantly lower affinity for non-A2A adenosine receptor subtypes, which are believed to be responsible for adverse effects.9 This is in contrast to adenosine which is a non-selective agonist and activates all four adenosine receptors. Regadenoson is given as a bolus of 0.4 mg with no weight adjustment, simplifying administration, and reducing errors in dose calculations which may occur with adenosine. Regadenoson induces peak coronary hyperemia starting within 30 seconds of injection and lasting 2-3 minutes.9,23
In the United States, regadenoson has become the most commonly used vasodilator stress agent for SPECT MPI. As of 2011, regadenoson was used in 68%, adenosine in 15%, and Dipyridamole in 13% of vasodilator SPECT MPI studies.8 The initial US approval of regadenoson was based on results of the ADVANCE MPI (adenosine versus regadenoson Comparative Evaluation for Myocardial Perfusion Imaging) trials, which showed similar sized perfusion defects with use of either adenosine and regadenoson in a wide spectrum of patients.10-12,24 However, these trials did not provide prognostic data for regadenoson MPI.
Given the widespread use of regadenoson, it is critical that it should not just provide similar diagnostic accuracy but also confer at least similar prognostic information. More recently, Iqbal and colleagues demonstrated a similarly low rate of major cardiac events following a normal regadenoson or adenosine SPECT MPI study.8 Moreover, Hage and colleagues have shown progressively increasing event rates with larger quantitative perfusion defect size using regadenoson SPECT MPI.25,26 Our results add to this body of knowledge by showing that SSS derived from either agent is significant in predicting events and provides incremental prognostic information above and beyond basic clinical variables. Furthermore, we have demonstrated no difference in SSS predicted probabilities for occurrence of events between the two stress agents. Thus, we have shown for the first time that there is no indication that the use of regadenoson or adenosine as the vasodilator agent modifies the prognostic significance of SSS. Similar findings were seen with SDS.
Limitations
This was a retrospective study with significant baseline differences between the regadenoson and adenosine groups. While we used IPW adjustment to account for these baseline differences, it is possible that we were not able to fully account for this. Despite the large sample size in this study, our results should be considered exploratory in nature. A direct comparison of the 2 agents would require a blinded randomized trial. However, given the current widespread use of regadenoson such a trial will be challenging to recruit for and fund. All patients in this study were recruited from a single academic institution and may not be representative of the wider population. However, this may have the advantage of providing uniform scanning, interpretation, and follow-up protocols. Despite our best efforts, it is possible that myocardial infarction events occurring at other institutions could have been missed. Clinical image interpretation was used in this study. Thus, knowledge of the clinical history may have introduced some bias into the interpretations. However, it can be argued that our results represent a “real world” scenario where interpreting physicians are usually aware of the patients clinical history and presentation. Background medical therapy is lower than that seen in some randomized clinical trial. However, these are “real world” figures and likely more akin to those seen in daily clinical practice.
New Knowledge Gained
This study suggests that SSS derived from either adenosine or regadenoson SPECT MPI is a significant predictor of events and provides incremental prognostic information beyond basic clinical variables. We found no difference in SSS predicted probabilities for occurrence of events between the two stress agents. Thus, we have shown for the first time that use of regadenoson vs adenosine as stress agent does not modify the prognostic significance of SSS. Similar findings were seen with SDS.
Abbreviations
- CABG:
-
Coronary Artery Bypass Grafting
- IPW:
-
Inverse Probability Weighted
- MPI:
-
Myocardial Perfusion Imaging
- MI:
-
Myocardial Infarction
- PCI:
-
Percutaneous Coronary Intervention
- SDS:
-
Summed Difference Score
- SPECT:
-
Single-photon emission computed tomography
- SRS:
-
Summed Rest Score
- SSS:
-
Summed Stress Score
References
Henzlova MJ, Cerqueira MD, Mahmarian JJ, Yao SS. Quality Assurance Committee of the American Society of Nuclear C. Stress protocols and tracers. J Nucl Cardiol 2006;13:e80-90.
Ladenheim ML, Pollock BH, Rozanski A, Berman DS, Staniloff HM, Forrester JS, et al. Extent and severity of myocardial hypoperfusion as predictors of prognosis in patients with suspected coronary artery disease. J Am Coll Cardiol 1986;7:464-71.
Hachamovitch R, Berman DS, Kiat H, Cohen I, Cabico JA, Friedman J, et al. Exercise myocardial perfusion SPECT in patients without known coronary artery disease: Incremental prognostic value and use in risk stratification. Circulation 1996;93:905-14.
Farzaneh-Far A, Borges-Neto S. Ischemic burden, treatment allocation, and outcomes in stable coronary artery disease. Circ Cardiovasc Imaging 2011;4(6):746-53.
Berman DS, Kang X, Hayes SW, Friedman JD, Cohen I, Abidov A, et al. Adenosine myocardial perfusion single-photon emission computed tomography in women compared with men. Impact of diabetes mellitus on incremental prognostic value and effect on patient management. J Am Coll Cardiol 2003;41:1125-33.
Amanullah AM, Berman DS, Erel J, Kiat H, Cohen I, Germano G, et al. Incremental prognostic value of adenosine myocardial perfusion single-photon emission computed tomography in women with suspected coronary artery disease. Am J Cardiol 1998;82:725-30.
Hachamovitch R, Berman DS, Shaw LJ, Kiat H, Cohen I, Cabico JA, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: Differential stratification for risk of cardiac death and myocardial infarction. Circulation 1998;97:535-43.
Iqbal FM, Hage FG, Ahmed A, Dean PJ, Raslan S, Heo J, et al. Comparison of the prognostic value of normal regadenoson with normal adenosine myocardial perfusion imaging with propensity score matching. JACC Cardiovasc Imaging 2012;5:1014-21.
Al Jaroudi W, Iskandrian AE. Regadenoson: A new myocardial stress agent. J Am Coll Cardiol 2009;54:1123-30.
Iskandrian AE, Bateman TM, Belardinelli L, Blackburn B, Cerqueira MD, Hendel RC, et al. Adenosine versus regadenoson comparative evaluation in myocardial perfusion imaging: Results of the ADVANCE phase 3 multicenter international trial. J Nucl Cardiol 2007;14:645-58.
Mahmarian JJ, Cerqueira MD, Iskandrian AE, Bateman TM, Thomas GS, Hendel RC, et al. Regadenoson induces comparable left ventricular perfusion defects as adenosine: A quantitative analysis from the ADVANCE MPI 2 trial. JACC Cardiovasc Imaging 2009;2:959-68.
Mahmarian JJ, Peterson LE, Xu J, Cerqueira MD, Iskandrian AE, Bateman TM, et al. Regadenoson provides perfusion results comparable to adenosine in heterogeneous patient populations: A quantitative analysis from the ADVANCE MPI trials. J Nucl Cardiol 2015;22:248-61.
Borges-Neto S, Shaw LK, Tuttle RH, Alexander JH, Smith WTt, Chambless M, et al. Incremental prognostic power of single-photon emission computed tomographic myocardial perfusion imaging in patients with known or suspected coronary artery disease. Am J Cardiol 2005;95:182-8.
Borges-Neto S, Tuttle RH, Shaw LK, Smith WTt, Jain D, Coleman RE, et al. Outcome prediction in patients at high risk for coronary artery disease: Comparison between 99mTc tetrofosmin and 99mTc sestamibi. Radiology 2004;232:58-65.
Salerno M, Elliot L, Shaw LK, Piccini JP, Pagnanelli R, Borges-Neto S. Prognostic validation of an algorithm to convert myocardial perfusion SPECT imaging data from a 12-segment model to a 17-segment model. J Nucl Cardiol 2009;16:605-13.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res 2011;46:399-424.
Cole SR, Hernan MA. Adjusted survival curves with inverse probability weights. Comput Methods Programs Biomed 2004;75:45-9.
Rozanski A, Gransar H, Hayes SW, Min J, Friedman JD, Thomson LE, et al. Temporal trends in the frequency of inducible myocardial ischemia during cardiac stress testing: 1991 to 2009. J Am Coll Cardiol 2013;61:1054-65.
Pijls NH, Fearon WF, Tonino PA, Siebert U, Ikeno F, Bornschein B, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the FAME (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) study. J Am Coll Cardiol 2010;56:177-84.
Dandekar VK, Bauml MA, Ertel AW, Dickens C, Gonzalez RC, Farzaneh-Far A. Assessment of global myocardial perfusion reserve using cardiovascular magnetic resonance of coronary sinus flow at 3 Tesla. J Cardiovasc Magn Reson 2014;16:24.
Greenwood JP, Maredia N, Younger JF, Brown JM, Nixon J, Everett CC, et al. Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease (CE-MARC): A prospective trial. Lancet 2012;379:453-60.
Abbasi SA, Ertel A, Shah RV, Dandekar V, Chung J, Bhat G, et al. Impact of cardiovascular magnetic resonance on management and clinical decision-making in heart failure patients. J Cardiovasc Magn Reson 2013;15:89.
Lieu HD, Shryock JC, von Mering GO, Gordi T, Blackburn B, Olmsted AW, et al. Regadenoson, a selective A2A adenosine receptor agonist, causes dose-dependent increases in coronary blood flow velocity in humans. J Nucl Cardiol 2007;14:514-20.
Cerqueira MD, Nguyen P, Staehr P, Underwood SR, Iskandrian AE. Investigators A-MT. Effects of age, gender, obesity, and diabetes on the efficacy and safety of the selective A2A agonist regadenoson versus adenosine in myocardial perfusion imaging integrated ADVANCE-MPI trial results. JACC Cardiovasc Imaging 2008;1(3):307-16.
Hage FG, Ghimire G, Lester D, McKay J, Bleich S, El-Hajj S, et al. The prognostic value of regadenoson myocardial perfusion imaging. J Nucl Cardiol 2015.
Acampa W, Salvatore M, Cuocolo A. Prognostication in the era of a new stressor for myocardial perfusion imaging. J Nucl Cardiol 2015.
Disclosures
This was an investigator-initiated study partly funded by Astellas Pharma. The company was not involved in study design, scan interpretation, data acquisition, endpoint adjudication, statistical analysis, or manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Additional information
See related editorials, doi:10.1007/s12350-015-0179-3 and doi:10.1007/s12350-015-0157-9.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Farzaneh-Far, A., Shaw, L.K., Dunning, A. et al. Comparison of the prognostic value of regadenoson and adenosine myocardial perfusion imaging. J. Nucl. Cardiol. 22, 600–607 (2015). https://doi.org/10.1007/s12350-015-0155-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-015-0155-y