Abstract
Background
In patients undergoing regadenoson SPECT myocardial perfusion imaging (MPI), the prognostic value of ischemic ST-segment depression (ST↓) and the optimal ST↓ threshold have not been studied.
Methods
A retrospective cohort study of consecutive patients referred for regadenoson stress MPI was conducted. Patients with uninterpretable ECG were excluded. Two diagnostic thresholds of horizontal or downsloping ST↓ were studied, ≥ 0.5 mm and ≥ 1.0 mm. The primary endpoint was the composite major adverse cardiac events (MACE) of cardiac death, myocardial infarction, or coronary revascularization.
Results
Among 8615 subjects (mean age 62 ± 13 years; 55% women), 89 (1.0%) had ST↓ ≥ 1.0 mm and 133 (1.5%) had ST↓ ≥ 0.5 mm. Regadenoson-induced ST↓ was more common in women (P < .001). Mean follow-up was 2.5 ± 2.2 years. After multivariate adjustment, ST↓ ≥ 1.0 mm was associated with a non-significant increase in MACE risk (P = .069), irrespective to whether MPI was abnormal (P = .162) or normal (P = .214). Ischemic ST↓ ≥ 0.5 mm was independently associated with MACE in the entire cohort (HR 2.14; CI 1.38-3.32; P = .001), whether MPI is normal (HR 2.07; CI 1.07-4.04; P = .032) or abnormal (HR 2.24; CI 1.23-4.00; P = .007), after adjusting for clinical and imaging covariates. An ST↓ threshold of ≥ 0.5 mm provided greater incremental prognostic value beyond clinical and imaging parameters (Δχ2 = 12.78; P < .001) than ≥ 1.0 mm threshold (Δχ2 = 3.72; P = .093).
Conclusion
Regadenoson-induced ischemic ST↓ is more common in women and it provides a modest independent prognostic value beyond MPI and clinical parameters. ST↓ ≥ 0.5 mm is a better threshold than ≥ 1.0 mm to define ECG evidence for regadenoson-induced myocardial ischemia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Myocardial perfusion imaging (MPI) with single-photon emission computed tomography (SPECT) is a valuable diagnostic and prognostic tool in the evaluation of patients with known or suspected coronary artery disease (CAD).1,2 Currently, vasodilator stress is used in the majority of MPI studies performed in the U.S.3 Although scintigraphic images are the source of most information derived from MPI, electrocardiographic (ECG) response to vasodilator stress occasionally provides incremental diagnostic or prognostic utility.4,5,6,–7 Nonetheless, previous studies evaluating the prognostic value of adenosine-induced ST↓ have yielded conflicting results.8,9,10,11,–12 In these studies, ST↓ ≥ 1.0 mm has been used to define an ischemic ECG response to vasodilator stress, a threshold that is conventionally applied to exercise stress. However, ST↓ ≥ 1.0 mm is infrequently observed with vasodilator stress (< 5%), limiting the clinical utility of ST-segment analysis.5,6,12,13,14,–15 A lower ST↓ threshold of 0.5 mm was investigated a few decades ago with exercise stress16, but it was ultimately abandoned due to inferior specificity, favoring the 1.0 mm cutoff which was subsequently adopted for pharmacologic stress.16,17 However, vasodilator stress is not confounded by many of the problems that plague the ECG specificity with exercise testing, such as motion, hyperventilation, and tachycardia. Therefore, 0.5 mm has been suggested as a viable ST↓ threshold for vasodilator stress, as it may provide enhanced sensitivity with fewer specificity challenges.18,19
In recent years, regadenoson, a selective A2A receptor agonist, has become the preferred vasodilator stress agent in the U.S., owing to its ease of use and favorable side-effect profile.13,14,–15,20,21,–22 Data regarding the value of regadenoson-induced ST↓ are lagging.18,23,24,25,26,–27 In a recent study of patients selected to undergo coronary angiography following regadenoson stress MPI, our group demonstrated that regadenoson-induced ST↓ ≥ 0.5 mm was associated with a higher rate of severe CAD and major adverse cardiac events (MACE), even among those with normal MPI.19 The study also found that ST↓ threshold ≥ 0.5 mm had a better discriminatory capacity in the diagnosis of severe CAD and the prediction of MACE when compared to the conventional 1.0 mm threshold.19 However, the prognostic data derived from the aforementioned study is limited by the fact that the patient population was restricted to patients selected to undergo coronary angiography.
In this investigation, we sought to evaluate the prognostic value of ST↓ in unselected patient population undergoing regadenoson stress MPI and to determine whether a pre-specified diagnostic ST↓ threshold of ≥ 0.5 mm provides better prognostic value than the conventional ≥ 1.0 mm threshold.
Methods
Design and Patient Population
A retrospective cohort study design was implemented. We queried the cardiology information system at Rush University Medical Center for all patients who underwent a clinically indicated regadenoson stress SPECT-MPI in the period from July 1, 2009 through September 11, 2015. In patients who underwent multiple regadenoson stress MPI during the study period, only the first regadenoson stress MPI was analyzed. The exclusion criteria were (1) patients who received a regadenoson injection after failing to achieve ≥ 85% of maximal predicted heart rate or adequate level of exercise; (2) missing clinical, ECG, or MPI data; (3) uninterpretable ECG, defined as left bundle branch block, ventricular paced rhythm, Wolff-Parkinson-White pattern, left ventricular hypertrophy with secondary ST↓ ≥ 0.5 mm, and resting ST↓ ≥ 0.5 mm due to digoxin effect or other nonspecific ST↓ ≥ 0.5 mm. Cardiovascular history and CAD risk factors (hypertension, diabetes mellitus, dyslipidemia, tobacco use, and family history) were collected prior to testing. CAD was defined as history of prior myocardial infarction (MI) or coronary revascularization.
Regadenoson Stress SPECT-MPI
Standard 1-day, rest/regadenoson stress 99mTc-tetrofosmin (~ 10 mCi rest; ~ 30 mCi stress) protocol was implemented in nearly all patients, except for occasional use of dual-isotope protocol (~ 3.5 mCi 201Tl rest; ~ 30 mCi 99mTc stress) during periods of 99mTc shortage and 2-day, rest/stress 99mTc-tetrofosmin (~ 30 mCi rest and stress) protocol in morbidly obese individuals.28 All patients underwent standard regadenoson stress protocol, without low-level exercise.20 Subsequent to each radioisotope injection, patients underwent SPECT-MPI acquisition using a dual-head, Siemens Ecam® camera (Siemens—Hoffman Estates, IL), without attenuation correction. The details of MPI acquisition and processing protocol are outlined elsewhere.29,30
MPI Analysis
Using 4DM-SPECT software package (INVIA—Ann Arbor, MI), MPI scans were quantitatively analyzed by operators (RK, CA, IF) blinded to clinical, ECG, angiography, and outcome data.31,32 On a 17-segment model, the segmental radiotracer activity in the rest and stress scans was quantitatively scored according to the standard 5-point scale (0: normal; 1: mild; 2: moderate; 3: severe; 4: absent activity) and summed to generate summed rest score and summed stress score (SSS).33 The summed difference score (SDS) was calculated from the sum of segmental difference scores between the stress and rest scans. Normal MPI was defined as SSS ≤ 3. The quantitative rest and post-stress left ventricular ejection fraction (LVEF) values were tabulated and the post-stress change in LVEF (stress LVEF minus rest LVEF) was calculated.34 Transient ischemic dilation (TID) ratios from the ungated SPECT-MPI were recorded and a TID > 1.31 was considered abnormal.35
ECG Analysis
Baseline and stress ECG data were determined using the formal structured clinical reports of regadenoson stress test. The generation of these structured reports prompts the description (upsloping, horizontal, or downsloping) and quantification of ST depression within specific ranges (no change, < 0.5 mm, 0.5-1.0 mm, 1.0-1.5 mm, 1.5-2.0 mm, > 2.0 mm), based on the manual analysis of the interpreting cardiologist at the time of the stress test. At our laboratory, the magnitude of ST↓ is conventionally measured at 80 ms from the J point.
In the present study, the morphology and magnitude of ST-segment deviation at rest, infusion, and recovery were tabulated. ST-segment depression was categorized into 3 ranges: 0-0.5 mm, 0.5-1.0 mm, and ≥ 1.0 mm. When present, ST↓ morphology was described as upsloping, horizontal, or downsloping. Only horizontal or downsloping ST↓ was considered to represent ischemic response. Upsloping ST depression was considered non-diagnostic. In patients with right bundle branch block, ST↓ in leads V1-V3 was not considered to represent an ischemic response. Based on existing literature, two distinct ST↓ thresholds, ≥ 0.5 mm and ≥ 1.0 mm, were selected a priori to investigate.16,19 Patients were grouped based on these ST↓ thresholds: < 1.0 vs ≥ 1.0 mm and < 0.5 vs ≥ 0.5 mm.
Outcomes
Subjects were followed for events of all-cause death, cardiac death (CD), nonfatal MI, and percutaneous or surgical coronary revascularization (CR) at any time following MPI. The outcome assessors (AA, SK, FI, MI, and MS) were blinded to ECG and MPI findings. Outcome status, date of event, and date of last encounter were determined by conducting a comprehensive chart review and a Social Security Death Index search. Death certificates and hospitalization records were reviewed to determine the cause of death. Late CRs was defined as revascularization occurring > 90 days post-MPI, signifying revascularization events not directly triggered by stress ECG or MPI findings. The primary outcome was defined as a composite MACE of CD, MI, or any CR (CD/MI/CR). The secondary outcomes were the composite of CD or MI and all-cause death.
Statistical Analyses
We powered the study to establish the prognostic utility of ST↓ ≥ 1.0 mm in patients with normal MPI. Assuming 5% incidence of ST↓ ≥ 1.0 mm, 2% annual MACE (CD/MI/CR) rate among patients without ST↓, and mean follow-up of 2 years,36 we determined that 5040 subjects with normal MPI would be needed to demonstrate a twofold increase in MACE rate in patients with ST↓ ≥ 1.0 mm compared to those with ST↓ < 1.0 mm using the unadjusted Chi-square test (α = 0.05, power = 0.80). Assuming 60% MPI normalcy rate, we calculated that a total of 8400 subjects of all comers (normal or abnormal MPI) are needed to demonstrate a statistically significant difference in the primary endpoint among subjects with normal MPI.
The Chi-square test was used to compare categorical variables, which were expressed as frequencies (percentages). The two-tailed, independent-samples Student’s t test was used to compare normally distributed continuous variables, which were expressed as means ± standard deviations. The Mann–Whitney test was used to compare skewed or non-parametric data.
Kaplan–Meier survival plots and the log-rank test were used to compare event-free survival. Multivariate Cox proportional hazard models were used to compare event-free survival, adjusting for clinical and imaging covariates. These covariates were age, gender, CAD status, CAD risk factors (diabetes mellitus, hypertension, tobacco use, dyslipidemia, and family history of CAD), SSS, and LVEF. Risk of outcome events was expressed as hazard ratio (HR) with 95% confidence intervals (CI). Moreover, multivariate Cox proportional hazard models were used to test for interactions between ST↓ and select clinical variables impacting the primary outcome. In these models, ST↓ status, a clinical variable, and an interaction term (ST↓*clinical variable) were entered as independent variables, while MACE was the dependent variable. The interaction P value was used to determine the significance of the interaction term.
Stepwise multivariate Cox regression models were used to determine the incremental prognostic value of ST-segment depression. The global Chi-square statistic and the corresponding P value (likelihood ratio test) were used as measures of significance of the incremental prognostic value.
In all statistical analyses, two-tailed P values < .05 were considered statistically significant. All analyses were conducted using SPSS-23 software package (IBM, Inc.—Armonk, NY). The study was approved by the institutional review board of Rush University Medical Center (Chicago, IL).
Results
A regadenoson stress database query yielded 10,564 patients who were referred for a regadenoson SPECT-MPI. A total of 1949 had 1 or more exclusion criteria; 330 had missing ECG or MPI data and 1619 had uninterpretable ECG (Supplemental Figure 1). Among the remaining 8615 analyzed subjects, a total of 870 (10%) patients were lost to clinical follow-up. The mean age was 62 ± 13 years and 55% were women. There was a small but statistically significant difference in the mean age between men and women (61 ± 13 vs 63 ± 13 years, respectively; P < .001). Notably, 89 (1.0%) subjects had ST↓ ≥ 1.0 mm and 133 (1.5%) had ST↓ ≥ 0.5 mm. There were no cases of regadenoson-induced ST elevation. The baseline characteristics of patients with and without ST↓ are summarized in Table 1. Notably, patients with ST↓ were more likely to be women regardless of the threshold used. Table 2 summarizes MPI findings. Of note, patients with ST↓ had a greater prevalence of TID and a mean decline in left ventricular ejection fraction following stress.
Primary Outcome: MACE (CD/MI/CR)
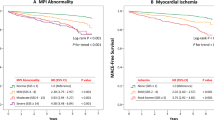
During a mean follow-up of 2.5 ± 2.2 years, there were 707 (8.2%) deaths, 105 (1.2%) CD, 203 (2.4%) MI, and 495 (5.7%) CR. Among 707 death events, 164 (23.2%) deaths were adjudicated using death certificates. There were a total of 669 (7.8%) composite MACE events of CD/MI/CR. In the entire cohort, ST↓ of any degree (0.5-1.0 mm and ≥ 1.0 mm) was associated with an increase in MACE risk (Figure 1).
Impact of various degrees of ST-segment depression on event-free survival. ST↓, regadenoson-induced ST-segment depression; HR, hazard ratio; CI, 95% confidence interval; MACE, major adverse cardiac events, defined as cardiac death, myocardial infarction, or coronary revascularization. *There was no significant difference in MACE-free survival between subjects in these groups (log-rank P = .266)
When ST↓ threshold was defined at 1.0 mm, ischemic ≥ 1.0 mm ST↓ was associated with a non-significant increase in the risk of CD/MI/CR and a significant increase in risk among those with abnormal MPI. Among patients with normal MPI, ST↓ ≥ 1.0 mm was not associated with increased risk of CD/MI/CR. After adjusting for clinical and imaging covariates, ST↓ ≥ 1.0 mm was not associated with increased risk of CD/MI/CR in the entire cohort or among those with normal or abnormal MPI (Figure 2).
Impact of ST↓ ≥ 1.0 mm on the composite of cardiac death, MI, or coronary revascularization. ST↓, regadenoson-induced ST-segment depression; MI, myocardial infarction; MPI, myocardial perfusion imaging; SSS, summed stress score; HR, hazard ratio; Adj HR, adjusted hazard ratio; CI, 95% confidence interval. *Adjusted for age, sex, hypertension, diabetes, dyslipidemia, smoking, family history of CAD, known CAD, SSS, and LVEF. †Adjusted for age, sex, hypertension, diabetes, dyslipidemia, smoking, family history of CAD, known CAD, and LVEF
When ST↓ threshold was defined at 0.5 mm, ischemic ST↓ was associated with increase in the risk of CD/MI/CR in the entire cohort and among patients with normal and abnormal MPI after adjusting for clinical and imaging covariates (Figure 3, Table 3, and Supplemental Table 1). In separate interaction analyses, we found no significant interactions impacting the primary outcome between ST↓ ≥ 0.5 mm and each of gender (P = .442), age (P = .394), diabetes mellitus (P = .932), and CAD status (P = .116). These negative interaction tests indicate that there are no differential prognostic implications of ST↓ ≥ 0.5 mm on the basis of gender, age, diabetic status, or CAD status.
Impact of ST↓ ≥ 0.5 mm on the composite of cardiac death, MI, or coronary revascularization. ST↓, regadenoson-induced ST-segment depression; MI, myocardial infarction; MPI, myocardial perfusion imaging; SSS, summed stress score; HR, hazard ratio; Adj HR, adjusted hazard ratio; CI, 95% confidence interval. *Adjusted for age, sex, hypertension, diabetes, dyslipidemia, smoking, family history of CAD, known CAD, SSS, and LVEF, †Adjusted for age, sex, hypertension, diabetes, dyslipidemia, smoking, family history of CAD, known CAD, and LVEF
We further analyzed CR events since they constituted the majority of the primary outcome events. As summarized in Table 3, when ST↓ threshold was defined as 0.5 mm, ST↓ was associated with a significant increase in the risk of CR and Late CR in the entire cohort and in patients with normal MPI after adjusting for clinical and imaging covariates. In order to exclude CR triggered by ECG and MPI findings, we analyzed Late CR (> 90 days post-MPI) separately and in a composite endpoint of CD/MI/Late CR. Ischemic ST↓ ≥ 0.5 mm was associated with a trend towards increased risk of the composite of CD/MI/Late CR in the entire cohort and a significant increase in this risk in patients with normal MPI, after adjusting for clinical and imaging covariates (Table 3). When ST↓ threshold was defined at 1.0 mm, ST↓ was associated with a statistically insignificant difference in the risk of the composite outcome of CD/MI/Late CR (Table 3).
Finally, given the inaccuracy of cause of death determination on the basis of death certificates, we performed sensitivity analyses using all-cause death, rather than cardiac death, in a composite endpoint of Death/MI/CR. Similar to the primary outcome analysis, when ≥ 0.5 mm threshold was used, ST↓ was associated with an increased risk of Death/MI/CR (P = 0.045); this was not the case when ≥ 1.0 mm threshold was used (P = .125).
Secondary Outcome: CD/MI
During follow-up, 286 (3.3%) composite CD/MI events were observed. In the entire cohort, using ≥ 1.0 mm threshold, ST↓ was not associated with a significant increase in the risk of CD/MI; this was also the case whether MPI is normal or abnormal. These insignificant differences persisted after adjusting for clinical and imaging covariates (Supplemental Figure 2). When ST↓ was defined as ≥ 0.5 mm, ST↓ was associated with insignificant increase in the risk of CD/MI in the entire cohort and among those with abnormal MPI. However, ST↓ ≥ 0.5 mm was associated with a trend towards increased risk of CD/MI among patients with normal MPI. After adjusting for clinical and imaging covariates, ST↓ ≥ 0.5 mm was associated with a significant increase in the risk of CD/MI among patients with normal MPI (Supplemental Figure 3).
Secondary Outcome: All-Cause Death
There were 707 (8.2%) deaths of any cause. In the entire cohort, patients with abnormal MPI and those with normal MPI, ischemic ST↓ was not associated with increased risk of all-cause death, irrespective of whether ST↓ threshold was defined as ≥ 1.0 mm or ≥ 0.5 mm. The lack of association between ST↓ (of any degree) and all-cause death persisted after adjusting for clinical and imaging covariates (Supplemental Figures 4 and 5).
Incremental Prognostic Value
As shown in Figure 4, while using ST↓ threshold of ≥ 1.0 mm did not provide significant incremental prognostic value to clinical and imaging covariates, ST↓ at a threshold of ≥ 0.5 mm provided significant incremental prognostic value in predicting CD/MI/CR. Moreover, a model that contains clinical and imaging covariates and ST↓ status, using 0.5 mm threshold, was more predictive of CD/MI/CR than a model that contains clinical and imaging covariates and ST↓ status, using 1.0 mm threshold. These analyses indicate that an ST↓ threshold of ≥ 0.5 mm is superior to ≥ 1.0 mm in predicting CD/MI/CR (Figure 4). On the other hand, ST↓, of any degree, did not provide significant incremental prognostic value for CD/MI (Figure 4) or all-cause death.
Incremental prognostic value of ST-segment depression. SSS, summed stress score; EF, left ventricular ejection fraction; ST↓, regadenoson-induced ST-segment depression; CD, cardiac death; MI, myocardial infarction; CR, coronary revascularization. Clinical covariates: age, sex, hypertension, diabetes mellitus, dyslipidemia, smoking, family history of CAD, known CAD
Discussion
This study is not only the first to investigate the prognostic value of regadenoson-induced ST↓, but also is the first to optimize the diagnostic threshold of ST↓ in order to maximize the prognostic utility of ECG analysis in patients undergoing vasodilator stress SPECT-MPI. The study demonstrated that regadenoson-induced ST↓ is uncommon but more frequently encountered in women in 3:1 ratio, which is consistent with previous publications.5,6,8 An ST↓ threshold of ≥ 0.5 mm provided a modest but significant incremental prognostic value for the composite of CD, MI, or CR, above and beyond clinical and perfusion imaging. ST↓ ≥ 0.5 mm was predictive of MACE among patients with normal and abnormal MPI. The prognostic utility of ST↓ ≥ 0.5 mm was consistent irrespective of gender, age, diabetic status, or CAD status. Moreover, an ST↓ diagnostic threshold of ≥ 0.5 mm provided greater incremental prognostic value than the traditional threshold of ≥ 1.0 mm which did not demonstrate a significant prognostic utility. The study findings support our previous work demonstrating a greater diagnostic utility of ST↓ threshold ≥ 0.5 mm in identifying patients with severe and extensive CAD.19 The present study, along with our previous work, proposes ≥ 0.5 mm as a preferred ST↓ threshold for diagnosis of myocardial ischemia in patients undergoing vasodilator regadenoson stress MPI.
Vasodilator stress produces heterogeneity of blood flow to regions supplied by normal vs diseased coronary arteries, without inducing true myocardial ischemia. This heterogeneity in blood flow manifests as perfusion defects. Occasionally, vasodilation of collateral coronary circulation may cause coronary “steal” from regions supplied by severely stenotic or totally occluded coronary arteries into a coronary bed with less abnormal coronary flow. Coronary steal may cause true myocardial ischemia which may manifest as ST-segment deviation on ECG.9,37,38 Thus, ischemic ECG changes with vasodilator stress have been speculated to represent a surrogate for severe CAD burden and worse prognosis. Our previous work in patients selected to undergo coronary angiography supports this hypothesis, demonstrating that regadenoson-induced ST↓ is associated with severe and extensive coronary artery disease.19 In addition, coronary microvascular dysfunction has been suggested as a potential cause of worse outcomes in some patients, particularly women.7 The microvascular dysfunction hypothesis may explain the observed increased incidence of ischemic events associated with vasodilator-induced ST-segment depression in women, despite the lower burden of obstructive CAD.39,40
The diagnostic significance of ST↓ during vasodilator stress has been evaluated in multiple studies, yielding conflicting results. Iskandrian et al demonstrated that ST↓ ≥ 1.0 mm during adenosine stress was independently predictive of left main or three-vessel CAD, and the same was demonstrated by Laarman with dipyridamole stress.4,41 On the other hand, Yap and colleagues established a correlation between adenosine-induced ST↓ and reversible perfusion abnormalities.42 Recently, Azemi and colleagues concluded that ST↓ ≥ 1.0 mm after adenosine or dipyridamole stress had some diagnostic value in patients with abnormal MPI but not in those with normal perfusion.12 On the other hand, Zahid et al found poor correlation between regadenoson-induced ST↓ and perfusion abnormalities by SPECT; however, their study lacked coronary angiography reference or clinical outcomes.18 More recently, in a cohort of patients selected to undergo coronary angiography following regadenoson stress MPI, our group demonstrated that regadenoson-induced ST↓ ≥ 0.5 mm was associated with higher rates of severe CAD and MACE, even among those with normal MPI.19
Prognostic studies of vasodilator-induced ST↓ have also been discordant in their findings. Abbott et al and Klodas et al identified ischemic ECG changes with adenosine or dipyridamole stress to be a marker of adverse cardiac events in patients with normal MPI.5,6 More recently, Hage et al found no demonstrable increase in adverse cardiac outcomes in patients with adenosine-induced ischemic ECG changes and normal MPI.9 Similarly, in a cohort of 3566 patients, Azemi et al concluded that ST↓ ≥ 1.0 mm during vasodilator SPECT-MPI provides no additional risk stratification beyond perfusion imaging.12 In the era of regadenoson stress, Uthamalingam et al reported that subjects with ST↓ ≥ 1.0 mm and normal MPI had higher than expected annual rates of cardiac death and coronary revascularization (1.9% and 9.9%, respectively).43,44,–45 However, the study lacked a control group.23. Our study affirms the prognostic utility of ST↓ analysis with vasodilator stress, even among patients with normal MPI. However, the study proposes ≥ 0.5 mm as an optimal ST↓ threshold, rather than the conventional 1.0 mm threshold, as patients with 0.5-1.0 mm ST↓ had increased MACE risk.
Lack of consistent diagnostic and prognostic utility of ST↓ ≥ 1.0 mm in our study and some reports in the literature can be explained, in part, by the low incidence of vasodilator-induced ST↓ ≥ 1.0 mm, which limits the statistical power of ST-segment analysis. More importantly, we demonstrated that there are significant diagnostic and prognostic implications for ST↓ in the range of 0.5-1.0 mm (Figure 1).19 Thus, when 1.0 mm threshold is used, classifying ST↓ in the range of 0.5-1.0 mm as “non-significant” would increase event rate in the control group (< 1.0 mm) and bias the ST-segment analysis to the null. It should be made clear that ST↓ ≥ 1.0 mm has diagnostic and prognostic significance (as it is ≥ 0.5 mm). However, using 1.0 mm as a cutoff to diagnose ischemia with vasodilator stress is suboptimal because patients with 0.5-1.0 mm are still at increased risk. We propose ≥ 0.5 mm as an alternative threshold for ST-segment analysis with vasodilator stress.
In the present cohort of all comers, the incidence of regadenoson-induced ST↓ ≥ 1.0 mm and ≥ 0.5 mm was 1% and 1.5%, respectively. This low rate is similar to the incidence of ST↓ ≥ 1.0 mm reported in the ASSUAGE and ASSUAGE-CKD trials (2% and 1%, respectively),13,21 but significantly lower than our previous study in patients selected for coronary angiography (19% and 5% for ST↓ ≥ 0.5 mm and ≥ 1.0 mm, respectively).19 The high rates of ST↓ in the latter study is likely due to higher CAD prevalence in patients selected to undergo coronary angiography.19 On the other hand, low rates of ST↓ ≥ 0.5 mm in the present study may be due to under-reporting of ST↓ in the range of 0.5-1.0 mm due to perceived lack of clinical significance. Additionally, declining burden of ischemia in patients tested in modern era may account for the relatively low incidence of ST↓.46
Notably, only 15% of deaths were due to a cardiac cause. This is may be due to the inaccuracy of death certificates, and assuming non-cardiac death in patients with unknown cause of death. To account for this limitation, we performed sensitivity analysis using an alternative composite endpoint Death/MI/CR, which yielded similar results. It is also notable that the association between ST↓ ≥ 0.5 mm and events in the normal MPI group appears stronger when early CR are excluded, which seems counter-intuitive. We speculate that ST↓ in the range of 0.5-1.0 mm in patients with normal MPI were disregarded as “insignificant,” and therefore, an early CR was not pursued. However, ensuing clinical course may have mandated a Late CR.
Based on our results, regadenoson-induced ST-segment depression, as little as ≥ 0.5 mm, should be routinely reported. Clearly, patients with ST↓ ≥ 0.5 mm and abnormal MPI should be considered for coronary angiography and revascularization. In patients with ST↓ ≥ 0.5 mm and normal MPI, decision-making should be guided by Bayesian principles. In patients with low likelihood of CAD, ST↓ ≥ 0.5 mm is less likely to represent “true” myocardial ischemia and may be candidates for careful observation or coronary calcium scoring. On the other hand, in patients with a higher likelihood of CAD, additional testing with coronary CT angiography, or even invasive coronary angiography, could be considered. In the near future, machine learning algorithms can incorporate ST-segment response along with numerous clinical and imaging variables to produce more accurate diagnostic and prognostic predictions.47,48
Limitations
The retrospective, single-center study design is an obvious limitation. Additionally, ST↓ was determined from clinical reports, rather than blinded rigorous measurements. The loss to follow-up in 10% of subjects is another limitation. Finally, the cause of death in some patients was determined using death certificates which can be inaccurate.
New Knowledge Gained
In the first study to evaluate the prognostic value of regadenoson-induced ST↓ in an unselected population, we demonstrated that ST↓ ≥ 0.5 mm was predictive of MACE, mostly driven by increased rate of coronary revascularization. Among patients with normal MPI, ST↓ ≥ 0.5 mm is associated with an independent and incremental increase in prognostic value beyond clinical and perfusion imaging. ST↓ threshold of 1.0 mm did not demonstrate significant discriminative prognostic utility. Our study proposes 0.5 mm as a preferred threshold for defining ischemic ST↓ in patients undergoing regadenoson stress SPECT-MPI.
Conclusion
Regadenoson-induced ischemic ST↓ is uncommon, but more frequently encountered in women. This ECG finding provides modest independent prognostic value beyond clinical and MPI data. ST↓ ≥ 0.5 mm is a preferred threshold to define ischemic ECG response to regadenoson stress. ST↓ should be considered in decision-making in patients with normal MPI.
Abbreviations
- AUC:
-
Area under the curve
- CABG:
-
Coronary artery bypass graft
- CAD:
-
Coronary artery disease
- ECG:
-
Electrocardiogram
- LVEF:
-
Left ventricular ejection fraction
- MACE:
-
Major adverse cardiac events
- MI:
-
Myocardial infarction
- MPI:
-
Myocardial perfusion imaging
- PCI:
-
Percutaneous coronary intervention
- ST↓:
-
ST-segment depression
- TID:
-
Transient ischemic dilation
References
Shaw LJ, Iskandrian AE. Prognostic value of gated myocardial perfusion SPECT. J Nucl Cardiol 2004;11:171-85.
Hachamovitch R, Berman DS, Shaw LJ, Kiat H, Cohen I, Cabico JA, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: Differential stratification for risk of cardiac death and myocardial infarction. Circulation 1998;97:535-43.
Zoghbi GJ, Iskandrian AE. Selective adenosine agonists and myocardial perfusion imaging. J Nucl Cardiol 2012;19:126-41.
Iskandrian AS, Heo J, Lemlek J, Ogilby JD, Untereker WJ, Iskandrian B, et al. Identification of high-risk patients with left main and three-vessel coronary artery disease by adenosine-single photon emission computed tomographic thallium imaging. Am Heart J 1993;125:1130-5.
Abbott BG, Afshar M, Berger AK, Wackers FJ. Prognostic significance of ischemic electrocardiographic changes during adenosine infusion in patients with normal myocardial perfusion imaging. J Nucl Cardiol 2003;10:9-16.
Klodas E, Miller TD, Christian TF, Hodge DO, Gibbons RJ. Prognostic significance of ischemic electrocardiographic changes during vasodilator stress testing in patients with normal SPECT images. J Nucl Cardiol 2003;10:4-8.
Bajaj NS, Singh S, Farag A, El-Hajj S, Heo J, Iskandrian AE, et al. The prognostic value of non-perfusion variables obtained during vasodilator stress myocardial perfusion imaging. J Nucl Cardiol 2016;23:390-413.
Abbott BG. The vasodilator stress ECG: Should depression cause anxiety? J Nucl Cardiol 2012;19:13-5.
Hage FG, Heo J, Iskandrian AE. Adenosine-induced ST segment depression with normal perfusion. Cardiol J 2009;16:121-6.
Hage FG, Dubovsky EV, Heo J, Iskandrian AE. Outcome of patients with adenosine-induced ST-segment depression but with normal perfusion on tomographic imaging. Am J Cardiol 2006;98:1009-11.
Sharma J, Roncari C, Giedd KN, Fox JT, Kanei Y. Patients with adenosine-induced ST-segment depressions and normal myocardial perfusion imaging: Cardiac outcomes at 24 months. J Nucl Cardiol 2010;17:874-80.
Azemi T, Rai M, Parwani P, Baghdasarian S, Kazi F, Ahlberg AW, et al. Electrocardiographic changes during vasodilator SPECT myocardial perfusion imaging: Does it affect diagnosis or prognosis? J Nucl Cardiol 2012;19:84-91.
Doukky R, Demori RM, Jain S, Kiriakos R, Mwansa V, Calvin JE. Attenuation of the side effect profile of regadenoson: A randomized double-blinded placebo-controlled study with aminophylline in patients undergoing myocardial perfusion imaging. “The ASSUAGE trial”. J Nucl Cardiol 2012;19:448-57.
Doukky R, Rangel MO, Dick R, Wassouf M, Alqaid A, Margeta B. Attenuation of the side effect profile of regadenoson: A randomized double-blind placebo-controlled study with aminophylline in patients undergoing myocardial perfusion imaging and have severe chronic kidney disease-the ASSUAGE-CKD trial. Int J Cardiovasc Imaging 2013;29:1029-37.
Doukky R, Rangel MO, Wassouf M, Dick R, Alqaid A, Demori RM. The safety and tolerability of regadenoson in patients with end-stage renal disease: The first prospective evaluation. J Nucl Cardiol 2013;20:205-13.
Gibbons RJ, Balady GJ, Bricker JT, Chaitman BR, Fletcher GF, Froelicher VF, et al. ACC/AHA 2002 guideline update for exercise testing: summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). J Am Coll Cardiol 2002;40:1531-40.
Redwood DR, Epstein SE. Uses and limitations of stress testing in the evaluation of ischemic heart disease. Circulation 1972;46:1115-31.
Zahid M, Kapila A, Eagan CE, Yusko DA, Miller ED, Missenda CD. Prevalence and significance of electrocardiographic changes and side effect profile of regadenoson compared with adenosine during myocardial perfusion imaging. J Cardiovasc Dis Res 2013;4:7-10.
Doukky R, Olusanya A, Vashistha R, Saini A, Fughhi I, Mansour K, et al. Diagnostic and prognostic significance of ischemic electrocardiographic changes with regadenoson-stress myocardial perfusion imaging. J Nucl Cardiol 2015;22:700-13.
Iskandrian AE, Bateman TM, Belardinelli L, Blackburn B, Cerqueira MD, Hendel RC, et al. Adenosine versus regadenoson comparative evaluation in myocardial perfusion imaging: Results of the ADVANCE phase 3 multicenter international trial. J Nucl Cardiol 2007;14:645-58.
Rangel MO, Demori RM, Doukky R. Age and gender as predictors of benefit from aminophylline administration in patients undergoing regadenoson stress myocardial perfusion imaging: A substudy of the ASSUAGE trial. Am J Ther 2013;20:622-9.
Astellas Pharma US. Lexiscan; 2014.
Uthamalingam S, Gurm GS, Ahmado I, Sidhu MS, Flynn J. Outcome of patients with regadenoson-induced ST-segment depression but normal perfusion on single-photon emission computed tomography. Angiology 2013;64:46-8.
Doukky R, Golzar Y. Safety of stress testing in patients with elevated cardiac biomarkers: Are all modalities created equal? J Nucl Cardiol 2017;24:735-73.
Golzar Y, Doukky R. Regadenoson use in patients with chronic obstructive pulmonary disease: The state of current knowledge. Int J Chron Obstruct Pulmon Dis 2014;9:129-37.
Vij A, Golzar Y, Doukky R. Regadenoson use in chronic kidney disease and end-stage renal disease: A focused review. J Nucl Cardiol 2017. https://doi.org/10.1007/s12350-017-0960-6.
Rai M, Ahlberg AW, Marwell J, Chaudhary W, Savino JA III, Alter EL, et al. Safety of vasodilator stress myocardial perfusion imaging in patients with elevated cardiac biomarkers. J Nucl Cardiol 2017;24:724-34.
Henzlova M, Cerqueira M, Mahmarian J, Yao S-S. Stress protocols and tracers. J Nucl Cardiol 2006;13:e80-90.
Chawla D, Rahaby M, Amin AP, Vashistha R, Alyousef T, Martinez HX, et al. Soft tissue attenuation patterns in stress myocardial perfusion SPECT images: A comparison between supine and upright acquisition systems. J Nucl Cardiol 2011;18:281-90.
Ballany W, Mansour K, Demori RM, Al-Amoodi M, Doukky R. The impact of regimented aminophylline use on extracardiac radioisotope activity in patients undergoing regadenoson stress SPECT myocardial perfusion imaging: A substudy of the ASSUAGE trial. J Nucl Cardiol 2014;21:496-502.
Johansson L, Lomsky M, Marving J, Ohlsson M, Svensson SE, Edenbrandt L. Diagnostic evaluation of three cardiac software packages using a consecutive group of patients. EJNMMI Res 2011;1:1-22.
Guner LA, Karabacak NI, Cakir T, Akdemir OU, Kocaman SA, Cengel A, et al. Comparison of diagnostic performances of three different software packages in detecting coronary artery disease. Eur J Nucl Med Mol Imaging 2010;37:2070-8.
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 2002;105:539-42.
Gomez J, Golzar Y, Fughhi I, Olusanya A, Doukky R. The significance of post-stress decrease in left ventricular ejection fraction in patients undergoing regadenoson stress gated SPECT myocardial perfusion imaging. J Nucl Cardiol 2017. https://doi.org/10.1007/s12350-017-0802-6.
Golzar Y, Olusanya A, Pe N, Dua SG, Golzar J, Gidea C, et al. The significance of automatically measured transient ischemic dilation in identifying severe and extensive coronary artery disease in regadenoson, single-isotope technetium-99 m myocardial perfusion SPECT. J Nucl Cardiol 2015;22:526-34.
Hachamovitch R, Hayes S, Friedman JD, Cohen I, Shaw LJ, Germano G, et al. Determinants of risk and its temporal variation in patients with normal stress myocardial perfusion scans: What is the warranty period of a normal scan? J Am Coll Cardiol 2003;41:1329-40.
Chow BJ, Wong JW, Yoshinaga K, Ruddy TD, Williams K, deKemp RA, et al. Prognostic significance of dipyridamole-induced ST depression in patients with normal 82Rb PET myocardial perfusion imaging. J Nucl Med 2005;46:1095-101.
Bajaj NS, Singh S, Farag A, El-Hajj S, Heo J, Iskandrian AE, et al. The prognostic value of non-perfusion variables obtained during vasodilator stress myocardial perfusion imaging. J Nucl Cardiol 2016;23:390-413.
Taqueti VR, Dorbala S, Wolinsky D, Abbott B, Heller GV, Bateman TM, et al. Myocardial perfusion imaging in women for the evaluation of stable ischemic heart disease-state-of-the-evidence and clinical recommendations. J Nucl Cardiol 2017;24:1402-26.
Pepine CJ, Anderson RD, Sharaf BL, Reis SE, Smith KM, Handberg EM, et al. Coronary microvascular reactivity to adenosine predicts adverse outcome in women evaluated for suspected ischemia results from the National Heart, Lung and Blood Institute WISE (Women’s Ischemia Syndrome Evaluation) study. J Am Coll Cardiol 2010;55:2825-32.
Laarman GJ, Verzijlbergen JF, Ascoop CA. Ischemic ST-segment changes after dipyridamole infusion. Int J Cardiol 1987;14:384-6.
Yap LB, Arshad W, Jain A, Kurbaan AS, Garvie NW. Significance of ST depression during exercise treadmill stress and adenosine infusion myocardial perfusion imaging. Int J Cardiovasc Imaging 2005;21:253-8.
Doukky R, Hayes K, Frogge N, Balakrishnan G, Dontaraju VS, Rangel MO, et al. Impact of appropriate use on the prognostic value of single-photon emission computed tomography myocardial perfusion imaging. Circulation 2013;128:1634-43.
Doukky R, Frogge N, Balakrishnan G, Hayes K, Collado FM, Rangel MO, et al. The prognostic value of cardiac SPECT performed at the primary care physician’s office. J Nucl Cardiol 2013;20:519-28.
Doukky R, Frogge N, Bayissa YA, Balakrishnan G, Skelton JM, Confer K, et al. The prognostic value of transient ischemic dilatation with otherwise normal SPECT myocardial perfusion imaging: A cautionary note in patients with diabetes and coronary artery disease. J Nucl Cardiol 2013;20:774-84.
Duvall WL, Rai M, Ahlberg AW, O’Sullivan DM, Henzlova MJ. A multi-center assessment of the temporal trends in myocardial perfusion imaging. J Nucl Cardiol 2015;22:539-51.
Sanghani RM, Doukky R. Fully automated analysis of perfusion data: The rise of the machines. J Nucl Cardiol 2017. https://doi.org/10.1007/s12350-017-0884-1.
Betancur J, Otaki Y, Motwani M, Fish MB, Lemley M, Dey D, et al. Prognostic value of combined clinical and myocardial perfusion imaging data using machine learning. JACC Cardiovasc Imaging 2018;11:1000-9.
Disclosures
Rami Doukky receives research funding from Astellas Pharma Global Development (Northbrook, IL). The other authors have no conflicts to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarizes the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Funding
The study was funded by a research grant from Astellas Pharma Global Development (Northbrook, IL).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Doukky, R., Nigatu, A., Khan, R. et al. Prognostic significance of ischemic electrocardiographic changes with regadenoson stress myocardial perfusion imaging. J. Nucl. Cardiol. 27, 1521–1532 (2020). https://doi.org/10.1007/s12350-018-1415-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-018-1415-4