Abstract
Background
Laparoscopic sleeve gastrectomy (SG) is a relatively new procedure that is gaining wide acceptance and represents an innovative new approach to the surgical management of morbid obesity. Our purpose is to evaluate the SG as a surgical bariatric procedure.
Methods
We conducted a literature review on “PubMed” based on all publications related to SG since 2000 to July 30, 2014.
Results
The complication rate after SG varies in the literature, ranging from 0 to 29 %. The most feared complication after SG is leakage on the staple line, occurring in 0–7 % of cases. The mortality rate reported varies between 0 and 3.3 %. No consensus has developed on the types of stapling used or the methods of strengthening the staple line. SG may aggravate and be responsible for gastroesophageal reflux disease (GERD). SG improves comorbidities in more than 50 % after 5 years.
Conclusions
SG can be proposed as a surgical technique at first intension in patients not having GERD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity now represents a public global health problem. The World Health Organization estimates the number of obese people in the world (body mass index (BMI) over 30 kg/m2) to be over 500 million people [1]. For 20 years, various surgical techniques have been proposed to lose excess weight and reduce the impact of comorbidities associated with obesity. Recently, a new procedure has become popular—the longitudinal gastrectomy, also known as “sleeve” gastrectomy (SG). This attractive and promising technique has continued to develop for 10 years, but is still subject to several controversies. We propose to make an update and review of the literature concerning the results of the SG and locate its place in the surgical treatment of morbid obesity.
History of sleeve gastrectomy
It was initially described by Hess and Marceau et al. [2, 3] in 1988 as the first restrictive part of a surgical malabsorptive procedure called “duodenal switch.” The isolated form of the SG was described for the first time in 1993 by Johnson et al. [4].
The first indications concerned “super” obese patients (BMI > 60 kg/m2) and those with a high anesthetic risk related to several comorbidities. At the time, bariatric surgery was performed in two separate operating times. The purpose of this first surgical step (SG) was to reach a consistent initial weight loss which is able to reduce the technical difficulties, and thus the perioperative morbidity [5, 6]. The second step (malabsorptive step) was performed within 6 months. Because of the encouraging initial results, the SG, considered technically easier and relatively faster than other malabsorptive bariatric procedures, was then used as an independent technique, showing a low rate of complications, a comparable excess weight loss, and a significant decrease of comorbidities [6, 7].
Methods
An online search in PubMed was performed by two authors independently to identify all relevant clinical literature on SG using keywords “laparoscopic sleeve gastrectomy,” “single port sleeve gastrectomy,” “complications,” “leak,” “weight loss,” “fistula,” “gastroesophageal reflux disease” in various combinations. The articles were also obtained from the references of these articles. The last search was carried out on July 30, 2014. These articles were chosen as they either described significant experience with this procedure or otherwise made a useful contribution to the debate on this procedure. Inclusion criteria for searches were: randomized controlled trials (RCTs), non-randomized clinical trials, retrospective and prospective cohort studies. We excluded a series of patients aged over 60 and under 20, case reports, conference abstracts, and those concerning revisional procedures.
Results
We selected 48 studies for review with a total number of 6699 SG, including 16 RCTs (SG, n = 856), 4 prospective non-randomized comparative studies (SG, n = 186), 2 retrospective non-randomized comparative studies (SG = 414), 15 prospective studies (n = 1059), and 11 retrospective studies (SG = 4203). Otherwise, we retained eight systematic reviews and one meta-analysis. There are a number of controversial aspects with the SG. We discuss below each of these aspects against available published scientific literature.
Discussion
Principles
The SG involves removing a large part of the stomach to form a tube and reduce the reservoir function of the stomach. Compared with other bariatric surgical techniques, the SG appears to be an attractive technique as it theoretically offers several benefits: it is easy to perform, it preserves the pylorus, entails no anastomoses, does not imply adding any foreign body, shows no risk of internal hernia, and does not prevent the exploration of the digestive tract.
Gastric tubulization is made under calibration probes, along the lesser curvature of the stomach. A small calibrator (32–42 Fr) is generally preferred instead of 60 Fr probes [8–10]. The stapling-section of the stomach is often started 5–6 cm proximal to the pylorus; the section line is then parallel to the lesser curvature (Figs. 1 and 2), ending 1 cm on the left of the esophagus.
Procedures to enhance the seal of the staple line have not yet been unanimously approved [11, 12]. Similarly, there is no consensus on the type of staples applied at tubulization stage. In a small experimental series, Fournier et al. [13] showed that the height of the staples used is a key factor in the development of a fistula on an SG. Indeed, staples low rise are more resistant. Strengthening the line of stapling Biosyn (transparent film, thin, and resorbable) further increases the resistance. Removing a portion of the stomach under 500 mL seems to be a failure and weight regain [14] factor.
What about single port?
Single-incision SG (SISG) is recently emerging in the field of bariatric surgery. Achieving superior cosmetic results is the most obvious benefit of this procedure. Saber et al. [15] published the first report of a SISG reporting seven obese patients with a BMI = 50 kg/m2. Various devices like the SILS™, R port™, Tri Port™, Gel port… have been developed for gaining intra-abdominal access. However, the size, shape, and location of the incision should not compromise safety and cosmetic outcomes.
SISG must be performed by experienced surgeons. Technically, enlarged livers pose the biggest difficulty during single-incision surgery, and liver retraction remains to be a challenge. Gentileschi et al. [16] proposed the use of a laparoscope for liver retraction, while Lakdawala et al. [17] retracted the liver using monofilament sutures on straight needles with a pledget to retract the liver to the anterior abdominal wall. However, Huang et al. [18] performed liver retraction using a silicone Penrose drain. Another difficulty described was distance between the xiphisternum and umbilicus encountered in taller patients. Fernández et al. [19] paid great attention to the xiphoideal–umbilicus distance, which should not exceed 22–25 cm.
With regards to operative outcomes, some authors reported longer operative times in SILS SG when compared with those in four or five-port SG [20, 21]. On the contrary, other authors [17, 22, 23] reported similar operating times in both procedures. Lakdawala et al. [17] believe that as the experience with SILS SG increases, the operative time proportionally decreases. Most authors report similar estimated blood loss and hospital stay in conventional SG and SILS cases [17, 22–25]. Similarly, in two randomized prospective studies, the authors demonstrated the benefits of SILS SG with reduction of postoperative pain [17, 22]. Most series reported that overall 90-day perioperative complication rate and short-term weight loss were comparable after SILS SG to those observed after conventional SG. All these results seem very promising but need high-power randomized clinical trials that use larger sample sizes to determine exactly the benefits and limitations of SILS in SG.
“Sleeve” and weight loss
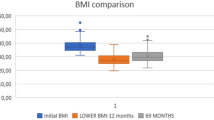
Weight loss after SG is partly based on a gastric restrictive mechanism tubulization which reduces the size of the new stomach. The SG has also a hormonal effect. By removing the gastric fundus, the secretion of ghrelin, a hormone that stimulates appetite secreted by fundic parietal cells, is almost stopped, causing loss of appetite. Similarly, some studies have shown the existence of high levels of the peptide hormone—YY (hormone that decreases appetite) and glucagon-like peptide-1 (pancreatic hormone that increases insulin secretion) after “sleeve,” leading to prolonged satiety, a decrease in gluconeogenesis, and an increase in insulin secretion [26, 27]. A recent large series of about 1000 SG reported an excess weight loss (EWL) of 86.6 % at 1 year, 84.2 % at 2 years, and 84.5 % at 3 years from the intervention [8]. In a systematic review, Brethauer et al. [28] showed an EWL of 55.4 % (1662 cases) and a mean BMI decrease from 51.2 to 37.1 kg/m2 after SG (n = 1940), with a maximum decrease at 5 years (3–60 months). The most recent studies show a drop in EWL at rates of 50–59 % after 5 years postoperatively [9, 29–33]. Based on 15 RCTs, comprising a total of 1191 patients, out of which 795 had undergone laparoscopic sleeve gastrectomy (LSG), Trastulli et al. [34] reported that the EWL ranged from 49 to 81 % in the SG group, from 62.1 to 94.4 % in the laparoscopic gastric bypass (LGB) group, and from 28.7 to 48 % in the laparoscopic adjustable gastric banding (LAGB) group with a follow-up ranging from 6 months to 3 years. However, reviewing the main studies comparing the SG with the LGB, we found almost similar results for EWL (Table 1).
“Sleeve” and comorbidities
One of the major challenges of bariatric surgery is the control of diabetes. It is now well established that the SG has a remission rate greater than the non-surgical treatment [42, 43]. The disappearance of type II diabetes occurs in 60–96 % of patients operated by SG [44]. In a systematic review, Gill et al. [45] showed a complete remission of diabetes in 66.2 % of cases, improvements in 29.9 % of cases, and stabilization in 13.1 % of cases within average 13.1 months. These results are similar to those obtained by the LGB at short term in comparative studies [35, 36, 46, 47], but seem to be inferior after 5 years in non-comparative studies [48, 49].
Other comorbidities, such as hypertension, dyslipidemia, arthritis, and sleep apnea, are clearly improved after SG, which gives satisfactory results (Table 2). It was also demonstrated that the SG significantly reduced the risk of developing coronary heart disease from the first 6 months postoperatively, and allows a significant risk reduction by up to 80 % within 12 months after intervention [53]. Pimenta et al. [54] concluded that quality of life has improved in 92.5 % of patients after an average of 19.1 months.
After a 1-year follow-up, Zhang et al. [55] found similar comorbidity remission rates between SG and LGB for sleep apnea (91.2 vs. 82.8 %; P = 0.338), hyperlipidemia (63 vs. 55.8 %; P = 0.633), hypertension (38.8 vs. 52.9 %; P = 0.062), diabetes (58.6 vs. 65.5 %; P = 0.638), and musculoskeletal disease (66.7 vs. 79.4 %; P = 0.472).
Complications of “sleeve”
The mortality rate reported in the literature varies between 0 and 3.3 % with a majority of publications reporting a rate close to 0 % [29, 56, 57].
The complication rate after SG varies in the literature, ranging from 0 to 29 % [29]. Most of these are minor complications, such as wound infections or non-major bleeding. Major complications were significantly less for sleeve gastrectomy patients (4.6 %) compared with patients who had laparoscopic gastric bypass (10.6 %) or duodenal switch (39.3 %) by the same surgeons [10]. The overall morbidity seems to be comparable to the bypass, ranging between 4.6 and 20.5 % in the literature [29, 58, 59]. Two RCTs [10, 35] reported a significantly higher incidence of complications in the LGB group than in the LSG group, but there was no major difference in reoperation between the two groups.
The most feared complication after SG is leakage on the staple line, occurring in 0–7 % of cases (Table 3). It is a serious complication requiring complex and non-consensual management. The International Sleeve Gastrectomy Expert Panel Consensus Statement in 2011 reported a gastric leakage rate of 1.06 % based on the study of 12,799 cases [60]. In a systematic review, the rate of leaks found was 2.4 % (115 out of 4888 SG). The leakage location is usually proximal to the esogastric junction (89 % of cases). Half of them are diagnosed after the 10th postoperative day [71]. The causes of these fistulas are not yet elucidated. Several theories have been advanced, including one that impugned increased intragastric pressure following pyloric dysfunction or loss of gastric compliance [57, 72]. According to Baker [73], the cause of the fistula can either be mechanical with fistulas declared on the 2nd or 3rd postoperative day or ischemic responsible in fistula on 5th or 6th postoperative day.
How to avoid fistula?
The surgical technique used is of vital importance to reduce the risk of postoperative complications, among which are leaks. Using a larger bougie size may give greater clearance at the dreaded esophagogastric junction thereby reducing the risk of leak. According Aurora et al. [71], the risk of these fistulas is increased in patients with a BMI > 50kg/m2 when using probe calibration < 40 Fr. Surgeons who used a bougie size of 40 Fr or greater had a 0.6 % leak rate (5/897 cases), however, the leak rate was 2.8 % (110/3991) in groups who used a bougie size < 40 Fr (P < 0.05). This difference was statistically significant, thus favoring the use of a bougie of 40 Fr to avoid leak, but it was independent of BMI.
Does staple line re-enforcement prevent fistula?
Baltasar et al. [57] protect the staple line with a continuous sero-serous suture (from the angle of Hiss to the half-way point and a second continuous suture from this point to the end) that inverts the staples, controls bleeding, and reduces the number of leaks, without increasing the cost of the procedure. No evidence-based results are confirming this technique. Aurora et al. [71] reported that 675 SG performed using staple line re-enforcement had a leak rate of 3 %. On the contrary, surgeons who did not re-enforce the staple line by any means had 16 leaks out of 688 patients (or 2.3 %).
Recently, fibrin glue was used to cover the staple line to prevent fistula and hemorrhage. Bellanger et al. [69] published their study of 529 cases using fibrin glue without a leak. Other studies have reported that these materials reduce the number of leaks [74, 75], but the evidence for the use of fibrin glue is currently limited and will require larger controlled studies.
Other authors used to begin tissue compression carefully, when using endostaples, and sustain this position for enough time to allow the tissue fluids to exit, as well as to carefully place the staples [73]. Some authors advise waiting for around 10 s before beginning stapling [68].
Some other principles are reiterated throughout much of the literature to prevent fistulas after SG, such as: avoid creating a stricture by not stapling too close to the incisura, avoid stapling too close to the gastro-esophageal junction [69], optimal use of endostaplers, prevention of distal stenosis, and good hemostasis without damaging tissues [65].
How to manage the fistula?
The treatment of fistulas that appear after SG is very problematic and controversial. What remains difficult is to stop the leak. Management mainly depends on the state of the patient.
Patients presenting hemodynamic instability, complicated fistulas, or signs of sepsis require surgical reintervention [76]. In case of early fistula (< 3 days after surgery), some authors support primary repair, when possible, despite a high percentage of recurrences [65]. If it is not technically possible or in the case of late fistulas, washing out the cavity and placing a drain seems to be the best option. Some authors have used endoscopically placed fibrin glue with variable success [64].
On the other hand, stable patients without a sepsis, or those who develop fistulas after a long postoperative period, should be managed conservatively by placing a drain under radiologic or endoscopic control, parenteral or better an early enteral nutrition [61, 64], high-dose proton pump inhibitors, and the use of broad spectrum antibiotics.
When the fistula persists for more than 4 weeks or the size of the collection does not clearly decrease, most authors have supported the use of gastric flexible coated stents as a second step [61, 64, 77–80] placed under endoscopy or fluoroscopic guidance which combined with percutaneous drainage and a short duration of parenteral nutrition usually provides a good result. A period of 6–8 weeks is recommended as the optimal time to withdraw the stent [77]. Patients who do not respond to any of these procedures and those with persistent fistula are candidates for three types of reintervention: conversion to gastric bypass, Roux en-Y, or total gastrectomy [81, 82].
The second most frequently reported complication of the SG is gastroesophageal reflux disease (GERD). This is a complication that can occur in 12.1 % of cases (± 8.9 %) [70]. However, the rates reported in literature are highly variable and sometimes contradictory. Carter et al. [83] in a retrospective study, found an increase in GERD during the first postoperative month of 12.6 % and a late increase by 14 % with a mean follow-up of 32 weeks. Prospective multicenter study done by Nocca et al. [84] on 163 patients showed an increased incidence of GERD by 5.7 %. Tai [85] in his prospective study conducted by a single-surgeon operator showed an increase by 34.9 %, the highest rate reported in the literature. More recently, DuPree et al. [86], performed a retrospective national review and compared 4832 patients undergoing SG with a concurrent cohort undergoing 33,867 LGB. Pre-existing GERD was present in 44.5 % of the SG cohort and 50.4 % of the LGB cohort. Most SG patients (84.1 %) continued to have GERD symptoms postoperatively, with only 15.9 % demonstrating GERD resolution. Of SG patients who did not demonstrate preoperative GERD, 8.6 % developed symptoms postoperatively. In comparison, LGB resolved GERD in most patients (62.8 %) within 6 months postoperatively (P < 0.001). Among the SG cohort, the presence of preoperative GERD was associated with increased postoperative complications (15.1 vs. 10.6 %), gastrointestinal adverse events (6.9 vs. 3.6 %), and increased need for revisional surgery (0.6 vs. 0.3 %) (all P < 0.05). The presence of GERD had no effect on weight loss for the LGB cohort but was associated with decreased weight loss in the SG group [86]. Several theories have been advanced to explain the role of the SG in the genesis and exacerbation of GERD, but proved unfounded. The only evidence is the existence of a hypotonic lower esophageal sphincter after an SG (possibly from division of ligaments and blunting of the angle of His) [87] and the existence of hypotonia of the digestive tract after a fall in ghrelin rate in animals [88]. It was also discussed that the remnant gastric pouch, being much more restrictive, may increase gastric pressure by reducing gastric compliance and emptying, and decreasing volume and dispensability [89]. It thus seems logical to avoid SG in patients with GERD because of the risk of worsening postoperatively [90]. Most experts recommend making a 24 h pH monitoring test for screening of GERD before making a SG. Omentopexy did not significantly decrease postoperative GERD symptoms in morbidly obese patients undergoing SG. If there is a hiatal hernia, it is recommended to repair it by closing the diaphragm pillars intra-operatively before performing SG [70, 91, 92]. Patients with persistent GERD after SG can be treated by a conversion to Roux-en-Y gastric bypass [93].
In contrast, other studies report that SG can improve symptoms and reduce the rate of GERD by up to 20 % [14, 94, 95]. Factors that may contribute to this effect include accelerated gastric emptying and increased weight loss, which decrease abdominal pressure. It was also suggested that long-term resolution of GERD could be explained by increase in compliance and restoration at the angle of His, which occurs about 3 years postoperatively [89]. However, it should be noted that all results reported in the literature on GERD after SG lack uniformity and accuracy as the criteria for the definition and diagnosis of GERD.
Conclusion
The sleeve gastrectomy is a new, simple bariatric procedure which entails no anastomoses. It has many technical variations and it is subject to much controversy. It seems preferable to use calibration probes around 40 Fr. No consensus has developed on the types of stapling used or the methods of strengthening the staple line. SISG seems to be feasible in carefully selected bariatric patients and results in short-term outcomes comparable to those observed after conventional SG. Improved pain and cosmesis are potential benefits of SILS. The main complication of SG is severe gastric fistula. No study has succeeded in demonstrating risk factors of this complication. Fistula management is difficult and should combine different procedures. SG may aggravate and be responsible for GERD, so it seems reasonable to avoid SG in patients with GERD. The results of the SG in terms of weight loss and control of comorbidities are encouraging at medium term but seem to fade over time, however, without dropping any lower after 5–6 years. Comparing with gastric bypass, SG can be proposed as a surgical technique at first intension in patients not having GERD.
References
World Health Organisation. Overweight and Obesity. http://www.who.int/mediacentre/factsheets/fs311/en. Fact sheet N°311. Updated August 2014.
Hess DS, Hess DW. Biliopancreatic diversion with duodenal switch. Obes Surg. 1988;8:267–82.
Marceau P, Hould FS, Simard S, et al. Biliopancreatic diversion with duodenal switch. World J Surg. 1998;22:947–54.
Johnson D, Dachtler J, Sue-Ling HM, King RF, Martin G. The magenstrasse and Mill operation for morbid obesity. Obes Surg. 2003;13:10–6.
Cottam D, Qureshi FG, Mattar SG, et al. Laparoscopic sleeve gastrectomy as an initial weight-loss procedure for high-risk patients with morbid obesity. Surg Endosc. 2006;20(6):859–63.
Tucker ON, Szomstein S, Rosenthal RJ. Indications for sleeve gastrectomy as a primary procedure for weight loss in themorbidly obese. J Gastrointest Surg. 2008;12:662–7.
Hamoui N, Anthone GJ, Kaufman HS, Crookes PF. Sleeve gastrectomy in the high-risk patient. Obes Surg. 2006;16:1445–9.
Boza C, Salinas J, Salgado N, et al. Laparoscopic sleeve gastrectomy as a stand-alone procedure for morbid obesity: report of 1,000 Cases and 3-year follow-up. Obes Surg. 2012;22:866–7.
Deitel M, Gagner M, Erickson AL, Crosby RD. Third International Summit: current status of sleeve gastrectomy. Surg Obes Relat Dis. 2011;6:7749–59.
Helmiö M, Victorzon M, Ovaska J, Leivonen M, Juuti A, Jaser N, Peromaa P, Tolonen P, Hurme S, Salminen P. Sleevepass: a randomized prospective multicenter study comparing laparoscopic sleeve gastrectomy and gastric bypass in the treatment of morbid obesity: preliminary results. Surg Endosc. 2012;26(9):2521–6.
Basso N, Casella G, Rizzello M, Abbatini F, Soricelli E, Alessandri G, Maglio C, Fantini A. Laparoscopic sleeve gastrectomy as first stage or definitive intent in 300 consecutive cases. Surg Endosc. 2011;25(2):444–9.
Gentileschi P, Camperchioli I, D’Ugo S, Benavoli D, Gaspari AL. Staple-line reinforcement during laparoscopic sleeve gastrectomy using three different techniques: a randomized trial. Surg Endosc. 2012;26(9):2623–9.
Fournier P, De Courville G, Upex P, Marmuse JP. Les fistules après Sleeve gastrectomie: étude expérimentale de la théorie mécanique portant sur la résistance de l’agrafage linéaire gastrique. Journal de Chirurgie Viscérale. 2013;150:9.
Weiner RA, Weiner S, Pomhoff I, Jacobi C, Makarewicz W, Weigand G. Laparoscopic sleeve gastrectomy—influence of sleeve size and resected gastric volume. Obes Surg. 2007;17:1297–305.
Saber AA, Elgamal MH, Itawi EA, Rao AJ. Single-incision laparoscopic sleeve gastrectomy (SILS): a novel technique. Obes Surg. 2008;18:1338–42.
Gentileschi P, Camperchioli I, Benavoli D, et al. Laparoscopic single-port sleeve gastrectomy for morbid obesity: preliminary series. Surg Obes Relat Dis. 2010;6:65–9.
Lakdawala MA, Muda NH, Goel S, Bhasker A. Single-incision sleeve gastrectomy versus conventional laparoscopic sleeve gastrectomy—a randomised pilot study. Obes Surg. 2011;11:1664–70.
Huang CK, Tsai JC, Lo CH, et al. Preliminary surgical results of ingle-incision transumbilical laparoscopic bariatric surgery. Obes Surg. 2011;21(3):391–6.
Fernández JI, Ovalle C, Farias C, et al. Transumbilical laparoscopic Roux-en-Ygastric bypass with hand-sewn gastrojejunal anastomosis. Obes Surg. 2013;23(1):140–4.
Nguyen NT, Smith BR, Reavis KM, et al. Strategic laparoscopic surgery for improved cosmesis in general and bariatric surgery: analysis of initial 127 cases. J Laparoendosc Adv Surg Tech A. 2012;22(4):355–61.
Delgado S, Ibarzabal A, Adelsdorfer C, Adelsdorfer W, Corcelles R, Momblán D, Lacy AM. Transumbilical single-port sleeve gastrectomy: initial experience and comparative study. Surg Endosc. 2012;26(5):1247–53.
Rogula T, Daigle C, Dua M, Shimizu H, Davis J, Lavryk O, Aminian A, Schauer P. Laparoscopic bariatric surgery can be performed through a single incision: a comparative study. Obes Surg. 2014;24(7):1102–8.
Park K, Afthinos JN, Lee D, Koshy N, McGinty JJ, Teixeira JA. Single port sleeve gastrectomy: strategic use of technology to re-establish fundamental tenets of multiport laparoscopy. Surg Obes Relat Dis. 2012;8(4):450–7.
Alevizos L, Lirici MM. Laparo-endoscopic single-site sleeve gastrectomy: results from a preliminary series of selected patients. Minim Invasive Ther Allied Technol. 2012;21(1):40–5.
Mittermair R, Pratschke J, Sucher R. Single-incision laparoscopic sleeve gastrectomy. Am Surg. 2013;79(4):393–7.
Ikramuddin S, Buchwald H. How bariatric and metabolic operations control metabolic syndrome. Br J Surg. 2007;98:1339–41.
Karamanakos N, Vagenas K, Kalfarentzos F, Alexandrides TK. Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide-YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy: a prospective, double blind study. Ann Surg. 2008;247:401–7.
Brethauer SA, Hammel JP, Schauer PR. Systematic review of sleeve gastrectomy as staging and primary bariatric procedure. Surg Obes Relat Dis. 2009;5:469–75.
Shi X, Karmali S, Sharma AM, Birch DW. A review of Laparoscopic sleeve gastrectomy for morbid obesity. Obes Surg. 2010;20:1171–7.
Catheline JM, Fysekidis M, Bachner I, Bihan H, Kassem A, Dbouk R, Bdeoui N, Boschetto A, Cohen R. Five-year results of sleeve gastrectomy. J Visc Surg. 2013;150(5):307–12.
Bohdjalian A, Langer FB, Shakeri-Leidenmühler S, Gfrerer L, Ludvik B, Zacherl J, Prager G. Sleeve gastrectomy as sole and definitive bariatric procedure: 5-year results for weight loss and ghrelin. Obes Surg. 2010;20(5):535–40.
Diamantis T, Apostolou KG, Alexandrou A, Griniatsos J, Felekouras E, Tsigris C. Review of long-term weight loss results after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2014;10(1):177–83.
Himpens J, Dobbeleir J, Peeters G. Long-term results of laparoscopic sleeve gastrectomy for obesity. Ann Surg. 2010;252(2):319–24.
Trastulli S, Desiderio J, Guarino S, Cirocchi R, Scalercio V, Noya G, Parisi A. Laparoscopic sleeve gastrectomy compared with other bariatric surgical procedures: a systematic review of randomized trials. Surg Obes Relat Dis. 2013;9(5):816–29.
Kehagias I, Karamanakos SN, Argentou M, Kalfarentzos F. Randomized clinical trial of laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy for the management of patients with BMI < 50 kg/m2. Obes Surg. 2011;21(11):1650–6.
Leyba JL, Aulestia SN, Llopis SN. Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy for the treatment of morbid obesity. A prospective study of 117 patients. Obes Surg. 2011;21(2):212–6.
Woelnerhanssen B, Peterli R, Steinert RE, Peters T, Borbély Y, Beglinger C. Effects of postbariatric surgery weight loss on adipokines and metabolic parameters: comparison of laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy–a prospective randomized trial. Surg Obes Relat Dis. 2011;7(5):561–8.
Lee WJ, Chong K, Ser KH, Lee YC, Chen SC, Chen JC, Tsai MH, Chuang LM. Gastric bypass vs sleeve gastrectomy for type 2 diabetes mellitus: a randomized controlled trial. Arch Surg. 2011;146(2):143–8.
Boza C, Gamboa C, Salinas J, Achurra P, Vega A, Perez G. Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy: a case-control study and 3 years of follow-up. Surg Obes Relat Dis. 2012;8:243–9.
Vidal P, Ramón JM, Goday A, Benaiges D, Trillo L, Parri A, González S, Pera M, Grande L. Laparoscopic gastric bypass versus laparoscopic sleeve gastrectomy as a definitive surgical procedure for morbid obesity. Mid-term results. Obes Surg. 2013;23(3):292–9.
Albeladi B, Bourbao-Tournois C, Huten N. Short- and midterm results between laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy for the treatment of morbid obesity. J Obes. 2013;2013:934653.
Leonetti F, Capoccia D, Coccia F, Casella G, Baglio G, Paradiso F, Abbatini F, Iossa A, Soricelli E, Basso N. Obesity, type 2 diabetes mellitus, and other comorbidities: a prospective cohort study of laparoscopic sleeve gastrectomy vs medical treatment. Arch Surg. 2012;147(8):694–700.
Schauer PR, Kashyap SR, Wolski K, Brethauer SA, Kirwan JP, Pothier CE, Thomas S, Abood B, Nissen SE, Bhatt DL. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366:1567–76.
Van Rutte PW, Luyer MD, de Hingh IH, Nienhuijs SW. To Sleeve or not to Sleeve in Bariatric Surgery? ISRN Surg. 2012;2012:674042. doi:10.5402/2012/674042.
Gill RS, Birch DW, Shi X, Sharma AM, Karmali S. Sleeve gastrectomy and type 2 diabetes mellitus: a systematic review. Surg Obes Relat Dis. 2010;6(6):707–13.
Chouillard EK, Karaa A, Elkhoury M. Greco VJ; Intercontinental Society of Natural Orifice, Endoscopic, and Laparoscopic Surgery (i-NOELS). Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy for morbid obesity: case-control study. Surg Obes Relat Dis. 2011;7(4):500–5.
Benaiges D, Flores Le-Roux JA, Pedro-Botet J, Chillarón JJ, Renard M, Parri A, Ramón JM, Pera M, Goday A. Sleeve gastrectomy and Roux-en-Y gastric bypass are equally effective in correcting insulin resistance. Int J Surg. 2013;11(4):309–13.
Li JF, Lai DD, Ni B, Sun KX. Comparison of laparoscopic Roux-en-Y gastric bypass with laparoscopic sleeve gastrectomy for morbid obesity or type 2 diabetes mellitus: a meta-analysis of randomized controlled trials. Can J Surg. 2013;56(6):158–64.
Arterburn DE, Bogart A, Sherwood NE, Sidney S, Coleman KJ, Haneuse S, O’Connor PJ, Theis MK, Campos GM, McCulloch D, Selby J. A multisite study of long-term remission and relapse of type 2 diabetes mellitus following gastric bypass. Obes Surg. 2013;23(1):93–102.
Moon Han S, Kim WW, Oh JH. Results of laparoscopic sleeve gastrectomy (LSG) at 1 year in morbidly obese Korean patients. Obes Surg. 2005;15(10):1469–75.
Silecchia G, Boru C, Pecchia A, et al. Effectiveness of laparoscopic sleeve gastrectomy (first stage of biliopancreatic diversion with duodenal switch) on co-morbidities in super-obese high-risk patients. Obes Surg. 2006;16(9):1138–44.
Zachariah SK, Chang PC, Ooi AS, Hsin MC, Kin Wat JY, Huang CK. Laparoscopic sleeve gastrectomy for morbid obesity: 5 years experience from an Asian center of excellence. Obes Surg. 2013;23(7):939–46.
Iancu M, Copăescu C, Şerban M, Ginghină C. Laparoscopic sleeve gastrectomy reduces the predicted coronary heart disease risk and the vascular age in obese subjects. Chirurgia (Bucur). 2013;108(5):659–65.
Pimenta GP, Moura DD, Adorno Filho ET, Jaudy TR, Jaudy TR, Aguilar-Nascimento JE. Long-term quality of life after vertical sleeve gastroplasty. Rev Col Bras Cir. 2013;40(6):453–7.
Zhang N, Maffei A, Cerabona T, Pahuja A, Omana J, Kaul A. Reduction in obesity-related comorbidities: is gastric bypass better than sleeve gastrectomy? Surg Endosc. 2013;27(4):1273–80.
Chazelet C, Verhaeghe P, Perterli R, Fennich S, Houdart R, Topart R, et al. Longitudinal sleeve gastrectomy as a stand-alone bariatric procedure: results of a multicenter retrospective study. J Chir. 2009;146(4):368–72.
Baltasar A, Serra C, Perez N. Laparoscopic sleeve gastrectomy: a multi-purpose bariatric operation. Obes Surg. 2005;15(8):1124–8.
Bennett JMH, Mehta S, Rhodes M. Surgery for morbid obesity. Postgrad Med J. 2007;83:8–15.
Frezza EE. Reddy S, Gee LL, Wachtel MS. Complications after sleeve gastrectomy for morbid obesity. Obes Surg. 2009;19:684–7.
Moy J, Pomp A, Dakin G, et al. Laparoscopic sleeve gastrectomy for morbid obesity. Am J Surg. 2008;196:56–9.
Serra C, Baltasar A, Andreo L, et al. Treatment of gastric leaks with coated self-expanding stents after sleeve gastrectomy. Obes Surg. 2007;17:866–72.
Lalor PF, Tucker ON, Szomstein S, et al. Complications after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2008;1:33–8.
Felberbauer FX, Langer F, Shakeri-Manesch S, Schmaldienst E, Kees M, Kriwanek S, Prager M, Prager G. Laparoscopic sleeve gastrectomy as an isolated bariatric procedure: intermediate-term results from a large series in three Austrian centers. Obes Surg. 2008;18(7):814–8.
Casella G, Soricelli E, Rizello M, et al. Nonsurgical treatment of staple line leaks after laparoscopic sleeve gastrectomy. Obes Surg. 2009;19:821–6.
Burgos AM, Braghetto I, Csendes A, et al. Gastric leak after laparoscopic-sleeve gastrectomy for obesity. Obes Surg. 2009;19:1672–7.
Stroh C, Birk D, Flade-Kuthe R, et al. Results of sleeve gastrectomy—data from a nationwide survey on bariatric surgery in Germany. Obes Surg. 2009;19(5):632–40.
Ser KH, Lee WJ, Lee YC, Chen JC, Su YH, Chen SC. Experience in laparoscopic sleeve gastrectomy for morbidly obese Taiwanese: staple-line reinforcement is important for preventing leakage. Surg Endosc. 2010;24(9):2253–9.
Armstrong J, O’Malley S. Outcomes of sleeve gastrectomy for morbid obesity: a safe and effective procedure? Int J Surg. 2010;8:69–71.
Bellanger DE, Greenway FL. Laparoscopic sleeve gastrectomy, 529 cases without a leak: short-term results and technical considerations. Obes Surg. 2011;21:146–50.
Rosenthal RJ, et al. International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of > 12,000 cases. Surg Obes Relat Dis. 2012;8(1):8–19.
Aurora AR, Khaitan L, Saber AA. Sleeve gastrectomy and the risk of leak: a systematic analysis of 4,888 patients. Surg Endosc. 2012;26:1509–15.
Yehoshua RT, Eidelman LA, Stein M, et al. Laparoscopic sleeve gastrectomy—volume and pressure assessment. Obes Surg. 2008;18(9):1083–8.
Baker RS, Foote J, Kemmeter P, et al. The science of stapling and leaks. Obes Surg. 2004;14(10):1290–8.
Sapala JA, Wood MH, Schuhknecht MP. Anastomotic leak prophylaxis using a vapor-heated fibrin sealant: report on 738 gastric bypass patients. Obes Surg. 2004;14(1):35–42.
Liu CD, Glantz GJ, Livingston EH. Fibrin glue as a sealant for high-risk anastomosis in surgery for morbid obesity. Obes Surg. 2003;13(1):45–8.
Gonzalez R, Nelson L, Gallagher S, et al. Anastomotic leaks after laparoscopic gastric bypass. Obes Surg. 2004;14:1299–307.
Fukumoto R, Orlina J, McGinty J, et al. Use of polyflex stents in treatment of acute esophageal and gastric leaks after bariatric surgery. Surg Obes Relat Dis. 2006;2:570–2.
Eubanks S, Edwards CA, Fearing NM, et al. Use of endoscopic stents to treat anastomotic complications after bariatric surgery. J Am Coll Surg. 2008;206(5):935–8.
Salinas A, Baptista A, Santiago E, et al. Self-expandable metal stents to treat gastric leaks. Surg Obes Relat Dis. 2006;2(5):570–2.
Blackmon SH, Santora R, Schwarz P, et al. Utility of removable esophageal covered self-expanding metal stents for leak and fistula management. Ann Thorac Surg. 2010;89(3):931–7.
Deitel M, Crosby RD, Gagner M. The first International Consensus Summit for Sleeve Gastrectomy (SG), New York City, 2007. Obes Surg. 2008;18:487–96.
Baltasar A, Serra C, Bengochea M, et al. Use of Roux limb as remedial surgery for sleeve gastrectomy fistulas. Surg Obes Relat Dis. 2008;4(6):759–63.
Carter PR, Leblanc KA, Hausmann MG, Kleinpeter KP, Debarros SN, Jones SM. Association between gastroesophageal reflux disease and laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2011;7:569–72.
Nocca D, Krawczykowsky D, Bomans B, et al. A prospective multicenter study of 163 sleeve gastrectomies: results at 1 and 2 years. Obes Surg. 2008;18:560–5.
Tai CM, Huang CK, Lee YC, Chang CY, Lee Ct, Lin JT. Increase in gastroesophageal reflux disease symptoms and erosive esophagitis 1 year after laparoscopic sleeve gastrectomy among obese adults. Surg Endosc. 2013;27:1260–6.
DuPree CE, Blair K, Steele SR, Martin MJ. Laparoscopic sleeve gastrectomy in patients with preexisting gastroesophageal reflux disease: a national analysis. JAMA Surg. 2014;149(4):328–34.
Braghetto I, Lanzarini e, Korn O, Valladares H, Molina JC, Henriquez A. Manometric changes of the lower esophageal sphincter after sleeve gastrectomy in obese patients. Obes Surg. 2010;20:357–62.
Nahata M, Muto S, Oridate N, et al. Impaired ghrelin signaling is associated with gastrointestinal dysmotility in rats with gastroesophageal reflux disease. Am J Physiol-Gastrointest Liver Physiol. 2012;303:42–53.
El-Hadi M, Birch DW, Gill RS, Karmali S. The effect of bariatric surgery on gastroesophageal reflux disease. Can J Surg. 2014;57(2):139–44.
Chiu S, Birch DW, Shi X, Sharma AM, Karmali S. Effect of sleeve gastrectomy on gastroesophageal reflux disease: a systematic review. Surg Obes Relat Dis. 2011;7:510–15.
Daes J, Jimenez ME, Said N, Daza JC, Dennis R. Laparoscopic sleeve gastrectomy: symptoms of gastroesophageal reflux can be reduced by changes in surgical technique. Obes Surg. 2012;22:1874–9.
Soricelli E, Iossa A, Casella G, Abbatini F, Cali B, N. Basso. Sleeve gastrectomy and crural repair in obese patients with gastroesophageal reflux disease and/or Hiatal Hernia. Surg Obes Relat Dis. 2013;9:356–61.
Langer FB, Bohdjalian A, Shakeri-Leidenmuhler S, Schoppmann SF, Zacherl J, Prager G. Conversion from sleeve gastrectomy to roux-en-y gastric bypass-indications and outcome. Obes Surg. 2010;20:835–40.
Chopra A, Chao E, Etkin Y, Merklinger L, Lieb J, Delany H. Laparoscopic sleeve gastrectomy for obesity: can it be considered a definitive procedure? Surg Endosc Other Intervent Tech. 2012;26:831–7.
Rawlins L, Rawlins MP, Brown CC, Schumacher DL. Sleeve gastrectomy: 5 year outcomes of a single institution. Surg Obes Relat Dis. 2013;9:21–5.
Conflict of interest
No conflicts of interest; no financial relationship.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guirat, A., Guenzi, M., Pereira, P. et al. What is the role of the sleeve gastrectomy in the surgical treatment of morbid obesity?. Eur Surg 46, 181–188 (2014). https://doi.org/10.1007/s10353-014-0285-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-014-0285-5