Abstract
Background
Laparoscopic sleeve gastrectomy (LSG) is gaining acceptance among bariatric surgeons as a viable option for treating morbidly obese patients. We describe results of a single surgeon’s experience with LSG in a community practice revealing a low complication rate and describing the surgical technique.
Methods
LSG was performed in 529 consecutive patients from December 2006 to March 2010. A technique is described where all operations were performed with attention to avoiding strictures at the incisura angularis and stapling close to the esophagus at the angle of His. No operations performed used buttressing material or over-sewing of the staple line. A retrospective chart review and e-mail survey was conducted to determine the occurrence of complications and weight loss.
Results
Follow-up data was collected on 490 of the 529 (92.6%) patients at 6 weeks. A total complication rate of 3.2% and a 1.7% 30-day readmission rate were observed. No leaks occurred in any of the 529 patients, and one death (0.19%) was observed. The most common complications were nausea and vomiting with dehydration and venous thrombosis. The percentages of excess weight loss were 42.36, 65.92, 66.11, and 64.42 with a follow-up of 71%, 68%, 63%, and 49% at 6 months, 1 year, 2, and 3 years, respectively.
Conclusion
The LSG can be performed in a community practice with a low complication rate. Surgeons performing LSG should strive to minimize the risk of creating strictures at the incisura angularis and stapling near the esophagus at the angle of His.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Morbid obesity has become a major health problem in the United States [1]. Laparoscopic sleeve gastrectomy (LSG) has shown promise as an operation that can be done with a reduced rate of complications [2]. LSG was first performed as a stage procedure for high-risk individuals undergoing staged bypass procedures [3], and recently, LSG is showing more promise as a primary procedure to treat morbid obesity [4, 5]; however, for any bariatric procedure to be widely adopted, the procedure must be performed with minimal complications [6].
This paper will attempt to illustrate a single surgeon’s experience in 529 consecutive laparoscopic sleeve gastrectomy operations in a community practice, performing the procedures in a 90-bed suburban hospital. Technical considerations that we feel can decrease the risk of staple line leak will be discussed. Additionally, the paper will examine the incidence of complications of this emerging procedure.
Methods
All patients entering our practice requesting bariatric surgery were offered three procedure options: laparoscopic gastric bypass, adjustable gastric banding, and LSG. After a one-on-one consultation with the surgeon, the patients made an informed decision to have LSG and informed consent was obtained. All patients were required to have psychological screening, routine labs, electrocardiogram, upper gastrointestinal X-rays, pulmonary function studies, and a medical evaluation. All patients were scheduled for LSG as a primary definitive procedure.
All patients received intravenous antibiotics, subcutaneous unfractionated heparin and sequential compression devices preoperatively.
Surgical Technique
The abdomen is entered under direct vision with an OptiView (Ethicon Endo-Surgery, Cincinnati, OH) trocar. Three 5-mm, one 12-mm, and one 15-mm ports are placed as pictured (Fig. 1). A liver retractor is used to support the liver. The pylorus is identified, and an area approximately 3 to 4 cm from the pylorus is chosen to begin ligating and transecting the greater curvature vessels with a Harmonic Scalpel (Ethicon Endo-Surgery, Cincinnati, OH). The greater curvature of the stomach is mobilized to the angle of His, with particular attention paid to mobilizing the entire fundus to the mid-portion of the left crura of the diaphragm. A 34-French bougie is passed by anesthesia and positioned in the distal antrum. Resectioning of the antrum is started tangentially from the right lateral port using a green load (4.1 mm), positioning the tip of the stapler to give a distance of one and a half times the width of a bougie at the area of the incisura angularis (Fig. 2). All stapling is performed using the Echelon 60 Endopath (Ethicon Endo-Surgery, Cincinnati, OH) stapler, holding initial compression for a minimum of 15 and 5 s of compression between strokes of the device. Resectioning of the body and fundus of the stomach is achieved using blue loads (3.5 mm) via the 15-mm left mid-clavicular port site to the angle of His. We intentionally do not mobilize the periesophageal fat pad in order to visually position the stapler to leave approximately 1 cm of gastric tissue lateral to the angle of His (Fig. 3). It is our practice not to use buttress material or over-sew the staple line, but our routine practice is to wait and allow adequate compression with the stapling device. Fibrin glue is applied to the staple line and the 15-mm port site is closed with absorbable suture.
Patients are monitored postoperatively on the surgical ward and receive heparin as prophylaxis for deep vein thrombosis and are ambulated the night of the surgery. Patients are given water and ice the day of the surgery and a clear liquid diet on postoperative day number one. Patients are discharged postoperative day number one as tolerated and are routinely placed on a daily proton pump inhibitor for 1 month.
Results
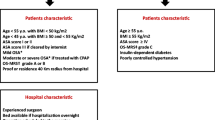
The charts of 529 consecutive patients beginning December 2006 through March 2010 who had undergone LSG in our practice were evaluated retrospectively. The patient’s weight, body mass index (BMI), age, and gender are summarized (Table 1). Sixty-three of the 529 patients (12%) were categorized as super obese (BMI ≥ 55).
Follow-up data was obtained on 490 of 529 (92.6%) patients at 6 weeks. The total complication rate was 3.2% with 1.7% readmission within 30 days of surgery. Mortality was 0.19% out of the 529 patients. That one patient died from a suspected pulmonary embolus at home, 9 days after the operation. There were no leaks in 529 consecutive sleeve gastrectomy patients. The most common complications were vomiting with dehydration and venous thrombosis (five each) with other complications being less common (Table 2). Weight loss data was collected by a combination of office measurement and self-reported weight via e-mail and telephony. Data was collected on 81 of 166 (49%) at 3 years, on 206 of 328 (63%) at 2 years, on 294 of 434 (68%) at 1 year, and on 377 of 529 (71%) patients at 6 months. Percent excess weight loss was chosen to track successful weight loss for the procedure. Patients lost 64.42%, 66.11%, 65.92%, and 42.36% excess weight at 3 years, 2 years, 1 year, and 6 months, respectively (Fig. 4).
Discussion
LSG originally proved to be a beneficial procedure for interval weight loss as the first stage of a two-staged bypass procedure [3]. More recently, LSG is showing promise as a primary bariatric procedure for appropriate candidates [4–6]. Currently, LSG comprises only 2% of all bariatric operations in the United States [5].
As a two-stage procedure, the initial reports of LSG were performed with a 60-French bougie and were reported to have a 33% excess weight loss (percent EWL) at 11 months [3]. From there, surgeons began using LSG as a primary bariatric procedure using smaller-sized bougies with reported greater percent excess weight loss (62% EWL) [7]. In a systematic review by Brethauer et al. [8], weight loss ranged from 33% to 85% of excess weight in patients having LSG. Wiener et al. [9] have demonstrated the durability of LSG at 5 years. Some reports have shown that decreasing the size of the bougie can lead to a greater percent excess weight loss [9], although some have disputed a cause and effect relationship between weight loss and bougie size in the short-term [10]. In addition, there is continued disagreement as to whether LSG represents a strictly restrictive procedure versus a combination restrictive/hormonal procedure [11]. Studies have shown the effects of LSG on ghrelin levels and hunger [12], as well as additional metabolic hormones [13].
As LSG becomes adopted by more bariatric surgeons, there becomes a need for the procedure to become standardized to achieve similar results across different practices and must be considered safe by the public [9]. Additionally, Wiener et al. noted that LSG is not a simple procedure, and owing to the fact that the procedure is irreversible, surgeons should strive to avoid complications [9]. In Louisiana, very few insurance plans have coverage for any form of bariatric surgery; therefore many patients must finance their own procedures. The current system in Louisiana also allows the patient to directly choose the procedure that they feel will balance their concern for surgical side effects with their personal desires and expectations for a weight loss operation. Minimizing the chance of complications is a major consideration, and we feel our technique has achieved this for our patients.
Technically, when performing LSG we use the harmonic scalpel to ligate and transect the greater curvature vasculature and short gastric vessels. We avoid thermal injury to any tissue that will be subsequently involved in the staple line by placing the active blade anterior and angling the blade away from gastric tissue. Devices using bipolar electrocautery can also be used safely when dissecting the great curvature of the stomach, and when used properly, either device should not increase the incidence of staple line dehiscence.
We advocate the use of a 34-French bougie without the use of buttressing material or over-sewing of the staple line. Our philosophy is to begin 3 to 4 cm from the pylorus thereby decreasing the antral volume while preserving its function. We feel we are able to minimize the chance of stricture formation and proximal staple line failure by allowing an effective 50-French diameter at the incisura angularis and concentrating on a 34-French diameter proximal to this area. Esophagogastroscopy and saline submersion was employed as a leak test for the first 350 patients, and no leaks were detected. No intraoperative leak test is currently employed; however, all staple lines are carefully inspected at the time of the operation. We do not, as a routine, leave a drain; however, we may leave a drain for complex cases or procedures with greater than the average blood loss.
The incidence of staple line dehiscence after LSG ranges from 0% to 5.5% [2, 14–17] and with overall complication rates ranging from 0% to 24% [8]. Lalor et al. [15] have advocated over-sewing the staple line to minimize staple line dehiscence while others routinely use only buttress material [10] or both [9]. Additionally, some technique studies have advocated avoiding the incorporation of the area of the gastroesophageal junction into the staple line [14, 15]. Our results of 0% leak rate in the 529 cases compares favorably with the literature while simplifying the procedure by avoiding the use of staple line protective maneuvers. We firmly believe there are two main tenets to adopt in order to minimize leaks. First, and of utmost importance, is to avoid creating a physiologic stricture at the incisura angularis and second, avoid stapling too close to the esophagus in the area of the cardia. We also advocate time for compression of the gastric tissue with the stapling device, thus promoting proper staple formation and reducing both serosal trauma and bleeding.
Leaks after LSG can result in significant morbidity [18]. There is also a tendency for leaks after LSG to occur in a latent fashion and appears to be associated with an increase pressure in the sleeved stomach and/or improper staple formation [18]. Regarding pressure, Gagner et al. have noted an inverse relationship between bougie size and leak rate and advocates a bougie size between 50 and 60 French to minimize this complication [18]. Mery et al. describe the relationship between staple height and the pressure required to produce staple line failure in a bench study using porcine small bowel [19]. Using this model, staple line failure was experienced at 50.4 mmHg for white loads (2.5 mm), 59.8 mmHg for blue loads (3.5 mm), and 18.7 mmHg for green loads (4.1 mm) when the staplers were used without buttress material [19]. The obvious limits of this study as it applies to LSG is the use of an animal model and much thinner small bowel, although one may be able to argue that the white and blue staple loads would perform similar to the blue and green loads in gastric tissue. Yehoshua et al. have described what is probably the most ideal technique to determine sleeve volume and pressure relationship to date and determined the basal sleeve pressure to be 19 mmHg and the filled pressure to be 43 mmHg [20]. Therefore, using all the information previously presented, a properly performed LSG should avoid creating a high-pressure situation within the sleeve lumen (<55 mmHg) and should be executed with appropriately sized staples for the tissue being coapted.
We have not performed pressure–volume measurements on our patients after LSG; however, we feel that our technique minimizes pressure in the sleeve as advocated by Gagner (50 French at the incisura angularis) while providing for complete resection of the fundus (34 French for body and fundus). Likewise, staple cartridge selection for our technique (green for antrum, blue for body and fundus) has resulted in a clinically low incidence of staple line failure. Which of these two factors, if any, is most important, would be of interest for further study.
Conclusion
Laparoscopic sleeve gastrectomy has shown promise as a primary bariatric procedure and as a staged procedure for high-risk patients. Our data reveal that the procedure can be performed in a community practice with a low complication rate and adequate medium-term weight loss. Additionally, surgeons performing LSG should strive to minimize the risk of creating strictures at the incisura angularis and stapling near the esophagus at the angle of His. We concede that the major weaknesses of our study include the marginal follow-up rates, the self-reported weight data, and the lack of primary pressure–volume measurements.
References
Buchwald H, Avidor Y, Braunnwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;14:1724–37.
Lee CM, Cirangle PT, Jossart GH. Vertical gastrectomy for morbid obesity in 216 patients: report of two-year results. Surg Endosc. 2007;21:1810–6.
Regan JP, Inabet WB, Gagner M, et al. Early experience with two-staged laparoscopic Roux-en-Y gastric bypass as an alternative in the super-super obese. Obes Surg. 2003;13:861–4.
Frezza EE. Laparoscopic vertical sleeve gastrectomy for morbid obesity. The procedure of choice? Surg Today. 2007;37:275–81.
Dietel M, Crosby RD, Gagner M. The First International Consensus Summit for Sleeve Gastrectomy (SG), New York City, October 25–27, 2007. Obes Surg. 2008;18:487–96.
Tucker ON, Szomstein S, Rosenthal RJ. Indications for sleeve gastrectomy as a primary procedure for weight loss in the morbidly obese. J Gastrointest Surg. 2008;12:662–7.
Baltasar A, Serra C, Perez N, et al. Laparoscopic sleeve gastrectomy: a multi-purpose bariatric operation. Obes Surg. 2005;15:1124–8.
Brethauer SA, Hammel JP, Schauer PR. Systematic review of sleeve gastrectomy as staging and primary bariatric procedure. Surg Obes Relat Dis. 2009;5:469–75.
Weiner RA, Weiner S, Pomhoff I, et al. Laparoscopic sleeve gastrectomy-influence of sleeve size and resected gastric volume. Obes Surg. 2007;17:1297–305.
Parikh M, Gagner M, Heacock L, et al. Laparoscopic sleeve gastrectomy: does bougie size affect mean %EWL? Short-term outcomes. Surg Obes Relat Dis. 2008;4:528–33.
Gagner M, Deitel M, Kalberer TL, et al. The Second International Consensus Summit for Sleeve Gastrectomy, March 19–21, 2009. Surg Obes Relat Dis. 2009;5:476–85.
Langer FB, Bohdjalian A, Shakeri-Manesch S, et al. Eating behavior in laparoscopic sleeve gastrectomy: correlation between plasma ghrelin levels and hunger. Eur Surg. 2008;3:120–4.
Karamanakos SN, Vegenas K, Kalfarentzos F, et al. Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide-YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy; a prospective, double blind study. Ann Surg. 2008;247:401–7.
Nocca D, Krawczykowsky D, Bomans B, et al. A prospective multicenter study of 163 sleeve gastrectomies: results at 1 and 2 years. Obes Surg. 2008;18:560–5.
Lalor PF, Tucker ON, Szomstein S, et al. Complications after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2008;4:33–8.
Aggarwal S, Kini SU, Herron DM. Laparoscopic sleeve gastrectomy for morbid obesity: a review. Surg Obes Relat Dis. 2007;3:189–94.
Fuks D, Verhaeghe P, Brehaut O, et al. Results of laparoscopic sleeve gastrectomy: a prospective study in 135 patients with morbid obesity. Surgery. 2009;145:106–13.
Gagner M. Leaks after sleeve gastrectomy are associated with smaller bougies: prevention and treatment strategies. Surg Laparosc Endosc Percutan Tech. 2010;20:166–9.
Mery CM, Shafi BM, Binyamin G, et al. Profiling surgical staplers: effect of staple height, buttress, and overlap on staple line failure. Surg Obes Relat Dis. 2008;4:416–22.
Yehoshua RT, Eidelman LA, Stein M, et al. Laparoscopic sleve gastrectomy-volume and pressure assessment. Obes Surg. 2008;18:1083–8.
Conflict of Interest Disclosure
Dr. Bellanger receives teaching honoraria from Ethicon Endo-Surgery. Dr. Greenway is a consultant or board member for Basic Research, Dow Chemical, General Nutrition Corporation, GlaxoSmithKline, Jenny Craig, Leptos Biomedical, Lithera Inc., NuMe Health LLC, Obecure Ltd., Oncometa Pharmaceutical, Orexigen Therapeutics, Third Rock Ventures, and Schering-Plough. Dr. Greenway also receives honoraria from Carolinas Medical Center and has stock/stock options in Lithera, Oncometa Pharmaceuticals and PlenSat Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bellanger, D.E., Greenway, F.L. Laparoscopic Sleeve Gastrectomy, 529 Cases Without a Leak: Short-Term Results and Technical Considerations. OBES SURG 21, 146–150 (2011). https://doi.org/10.1007/s11695-010-0320-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-010-0320-y