Abstract
Laparoscopic Roux-en-Y gastric bypass (LRYGB) is one of the most widely used bariatric procedures today, and laparoscopic sleeve gastrectomy (LSG) as a single-stage procedure for the treatment of morbid obesity is becoming increasingly popular. In this study, we prospectively compared both techniques in order to establish whether there is any superiority of one over the other based on morbidity and effectiveness. From January 2008 to December 2008, 117 obese patients with indication for bariatric surgery were assigned by patient choice after informed consent to either a LRYGB procedure (n = 75) or a LSG procedure (n = 42). We determined operative time, length of stay, morbidity, co-morbidity outcomes, and excess weight loss at 1 year postoperative. Both groups were comparable in age, sex, body mass index, and co-morbidities. Mean operative time of LSG was 82 min while LRYGB was 98 min (p < 0.05). Differences in length of stay, major complications, improvement in co-morbidities, and excess weight loss were not significant (p > 0.05). One year after surgery, average excess weight loss was 86% in LRYGB and 78.8% in LSG (p > 0.05). In the short term, both techniques are comparable regarding safety and effectiveness, so not one procedure is clearly superior to the other.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Changes that have occurred in recent decades in the pattern of human behavior, specifically regarding diet and physical activity, have led to significant alterations in the health of the world’s population, characterized among other things, by a larger increase in the prevalence and incidence of obesity [1].
Scientific efforts to control severe or morbid obesity with surgery, the most effective long-term treatment option for sustained weight loss at present time, have been gradually transforming conventional bariatric surgical techniques into routine minimally invasive surgeries, which have led to a growing acceptance and demand among the obese patients around the world.
Currently, the laparoscopic approach in some bariatric procedures has irrefutably proved their superiority over the traditional approach via laparotomy [2–4]. Among these, the laparoscopic Roux-en-Y gastric bypass (LRYGB) is one of the most used techniques worldwide because it has proven to be safe and effective in the long term [5, 6]. However, this is a technically demanding procedure, with a long learning curve, and with significant morbidity and mortality rates, especially in super-super obese patients (body mass index (BMI) ≥60 kg/m2) [7, 8].
Among the bariatric options, the laparoscopic sleeve gastrectomy (LSG), initially used in patients with high surgical risk as the first stage of a more complex procedure (duodenal switch or gastric bypass), has gained popularity in recent years due to reported good short-term results and its relative lower technical complexity [9–24]. However, the long-term efficacy is under investigation and there are very few studies that compare it with other bariatric techniques, including LRYGB.
In this study, we prospectively compared the results of both techniques (LRYGB and LSG) in a similar universe of patients in order to obtain evidence on the advantages and disadvantages of each technique so we could establish which is closest to the ideal procedure.
Methods
This study was performed prospectively at Hospital Universitario de Caracas and Clinica Santa Sofia. From January 2008 to December 2008, obese patients with BMI of 35 to 49.9 kg/m2, were assigned to a LRYGB or LSG according to their personal expectations after being thoroughly explained all potential advantages and disadvantages of each procedure.
We excluded patients with previous bariatric surgery, super obesity (BMI ≥50 kg/m2), alcohol or drug abuse, and/or major psychiatric disorders.
The study was approved by the local ethics committee and written informed consent was obtained from all patients.
Surgical Technique
The LRYGB was performed with a 30-ml gastric pouch, 150-cm antecolic gastric limb, and latero-lateral jejunojejunostomy with a 45-mm linear stapler (blue load, 3.5 mm staples). The end-side gastrojejunostomy was constructed using a 45-mm linear stapler (blue load) inserted only 15 mm into the gastric and jejuna lumina, and closing the common enterotomy with two layers of 2–0 polyester running sutures. The resulting mesenteric defects were not closed at the time of surgery.
In LSG, the vascular supply of the greater curvature of the stomach was divided inside the arcade, starting at 5 cm proximal to the pylorus until the His angle exposing the left crus of the diaphragm. The gastric tube was calibrated with a 46 Fr bougie (introduced perorally by the anesthetist) to perform the gastric section with a 60-mm linear stapler, starting at 5 cm from the pylorus with two golden loads (3.8 mm staples), and continuing towards the angle of His with blue loads. The golden load staple line was overlapped with a polyester 2–0 running suture. The specimen was removed through the port of the left upper quadrant.
Oral fluids were started on the second postoperative day, and patients were discharged when tolerance was good. Patients were followed up at 1 week postoperative, at 1 month, and then every 3 months up to 1 year postoperative.
Operative time, length of stay, morbidity, excess weight loss, and improvement of co-morbidities were prospective collected.
Wilcoxon and Fisher exact tests were used for statistical analysis considering p < 0.05 as significant.
Results
Of 202 patients operated for morbid obesity between January and December 2008, 117 patients were included in the study, 75 of which underwent LRYGB and 42 LSG. Both groups were comparable in age, sex, and BMI (Table 1).
There were 17 (22.6%) co-morbidities in the LRYGB group versus five (11.9%) in the LSG group, p > 0.05 (Table 2).
Mean operative time for LSG was 82 min (45–120 min) while for LRYGB it was 98 min (60–180 min), p < 0.05.
Length of stay was 2.4 days (2–7 days) for the LSG patients and 2.1 days (2–5 days) for LRYGB patients, p > 0.05.
There were four minor complications, all in the LSG group corresponding to early episodes of persistent nausea and sialorrhea (>48 h), which solved spontaneously without consequences. This represented a significant difference compared to LRYGB, p < 0.02.
There were four (5.3%) early major complications in patients who underwent LRYGB, three were upper gastrointestinal bleeding manifested as hematemesis and/or melena with a drop in hemoglobin levels, and one was the torsion of the blind limb; while in the LSG there was one (2.3%) major complication which was an early intra-abdominal bleeding with hypotension, but this did not represent a significant difference, p > 0.05 (Table 3). Patients with gastrointestinal bleeding (LRYGB) were successfully treated with upper endoscopy and blood transfusions, and the patient with torsion of the blind limb (LRYGB) required a relaparoscopy to correct the position of the limb through its fixation with sutures to the gastric remnant. The patient with intra-abdominal bleeding (LSG) was reoperated on via laparotomy and recovered without further complications.
There were three (4%) late complications (>1 month after operation) in the LRYGB group, two of which were gastrojejunostomy stenosis, successfully treated by endoscopic dilation, and a Petersen hernia treated by laparoscopy, and there was one (2.3%) in the LSG group which was an episode of hemorrhagic gastritis diagnosed by upper gastrointestinal endoscopy and treated with oral antisecretory drugs on an outpatient basis. This represented no statistical difference, p > 0.05.
If we add the total of major complications (early and late), we have seven (9.3%) for the LYRGB procedure and two (4.7%) for the LSG procedure, p > 0.05.
There were no fistulas or leaks in any patients and there was no mortality in the series.
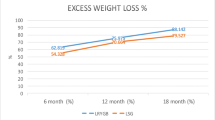
Ninety-nine patients (84.6%) were available to assess the excess weight loss at 1 year postoperative, 60 (80%) of the LRYGB group, and 39 (92.8%) of the LSG group, p > 0.05. The percentage of excess weight loss at 1 year after surgery was 86% for LRYGB and 78.8% for LSG, p > 0.05.
The co-morbidity improvement after 12 months of follow-up is shown in Table 4. Most of the medical diseases associated with obesity improved with both procedures, p > 0.05.
Discussion
The results of this series show that although the LSG is technically less complex than the LYRGB, which is reflected by a lower operative time (p < 0.05), this does not necessarily translate into higher morbidity for LRYGB. Minor complications were significantly more common in the LSG procedure (p < 0.02), while major complications in both groups showed no statistically significant difference (p > 0.05).
It is notable that fistulas and leaks, which are the most feared and devastating complications of bariatric surgery, did not happen in any patient.
We still have to evaluate the occurrence of late complications, such as gastrogastric fistula and internal hernias in LRYGB, and gastroesophageal reflux or gastric tube dilation in LSG.
The few studies comparing LRYGB and LSG that have been published show similar results to those obtained by us on the morbidity of these procedures. Karamanakos et al. [25], in a prospective series of 32 patients had no complications, while Lakdawala et al. [26], recently published a retrospective study without evidence of significant differences in perioperative morbidity but with an increase in gastroesophageal reflux in LSG.
The results of our work also show that the excess weight loss at 1 year follow-up was satisfactory with both techniques (LRYGB = 86% vs. LSG = 78.8%), with no significant difference. In the study of Karamanakos [25], also with 1 year follow up, there was a lower excess weight loss compared to what our patients showed, 69.7% in LSG and 60.5% in LRYGB, with a weight loss of 40 ± 8.3 kg in LRYGB and 43.6 ± 11.7 kg in LSG (p = 0.32). Likewise, in the study of Lakdawala, no significant difference was evident between the two techniques in terms of excess weight loss at 1 year postoperative [26].
Our results in co-morbidity outcomes with both procedures was towards improvement in all cases, with resolution in a significant percentage of patients and no significant differences, such as reported in the works of Karamanakos and Lakdawala [25, 26].
Another comparative study available is the one published by Peterli et al. [27], where they prospectively evaluated changes in insulin levels, glucose, and GLP-1 after a LSG and LRYGB in a total of 27 obese patients without diabetes. The results show improved glucose homeostasis after both techniques without significant differences.
Although it was not an objective in our study, micronutrient deficiency is an aspect to evaluate after bariatric surgery, which is common in those techniques that involve some degree of malabsorption. Gehrer et al. [28], prospectively studied 136 patients (86 with LRYGB and 50 with LSG) with a mean follow up of 24 months and showed that in both cases there are deficits of certain micronutrients, significantly higher in LRYGB only for vitamin B12 and calciferol.
Although our study was done prospectively, we must acknowledge some weak points that should be taken into account when making conclusions as well as when planning new research.
The study is still short-term, so a second assessment is needed. We have planned it in 5 years, which will allow us to establish the final behavior of weight loss and morbidity. Groups were unequal in size (the bias was created by the method in which the patients chose their own procedures), and super-obese patients (BMI >50 kg/m2) were excluded from the study, who are known to represent a distinct category in terms of morbidity, technical complexity, and performance.
We could not achieve 100% follow-up to assess the excess weight loss at 1 year postoperative. Some patients were pregnant (although we recommended not to do so until 18 months after surgery), and other patients came from distant locations and came to control after 14 to 16 months. While these patients did not have any new complications related to the procedure, it is likely that they continued losing weight in those two to four additional months, so we decided to asses this point only with the patients who were available a year postoperative, since from that period on, control is performed every 6 months. In the LRYGB group, 15 patients were not available at 1 year postoperative but only two of them had any comorbidity (hypertension), which was in remission at 6 months postoperative, and this was also confirmed at 16 months in both patients. In the LSG group, three patients that were not available at 1 year postoperatively were pregnant at that time and none suffered any comorbidities associated. This means that comorbidities follow-up could be completed in all patients.
Finally, we may conclude that both the LSG as well as the LRYGB are safe and effective bariatric techniques in the short term with no significant differences in terms of morbidity, excess weight loss, and improvement of co-morbidities during the first postoperative year.
Therefore, for the group of patients with BMI between 35 and 50 kg/m2, we believe that, at least in the short term, no technique was superior to the other, so the choice of which surgery to perform should be individualized according to the patient.
It is necessary to evaluate this group of patients in the long term to make definitive conclusions.
References
Satia-Abouta J. Dietary acculturation: definition, process, assessment, and implications. IJHE. 2003;4:71–86.
Lacy A, Delgado S. Controversias en Cirugía Laparoscópica de la obesidad. Contraindicaciones y límites de la cirugía laparoscópica. Cir Esp. 2004;75:287–9.
Samuel I, Mason E, Renquist K, et al. Bariatric surgery trends: an 18-year report from the International Bariatric Surgery Registry. Am J Surg. 2006;192:657–62.
Nguyen NT, Goldman C, Rosenquist J, et al. Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and cost. Ann Surg. 2001;234:279–91.
Buchwald H, Williams SE. Bariatric surgery worldwide 2003. Obes Surg. 2004;14:1157–64.
Picot J, Jones J, Colquitt JL, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for morbid obesity: a systematic review and economic evaluation. Health Technol Assess. 2009;13:41.
Søvik TT, Aasheim ET, Kristinsson J, et al. Establishing laparoscopic Roux-en-Y gastric bypass: perioperative outcome and characteristics of the learning curve. Obes Surg. 2009;19:158–65.
Stephens DJ, Saunders JK, Belsley S, et al. Short-term outcomes for super-super obese (BMI > or =60 kg/m2) patients undergoing weight loss surgery at a high-volume bariatric surgery center: laparoscopic adjustable gastric banding, laparoscopic gastric bypass, and open tubular gastric bypass. Surg Obes Relat Dis. 2008;4:408–15.
Aggarwal S, Kini SU, Herron D. Laparoscopic sleeve gastrectomy for morbid obesity: a review. Surg Obes Relat Dis. 2007;3:189–94.
Baltazar A, Serra C, Perez N, et al. Laparoscopic sleeve gastrectomy: a multi-purpose bariatric operation. Obes Surg. 2005;15:1124–8.
Moon Han S, Kim WW, Oh JH. Results of laparoscopic sleeve gastrectomy (LSG) at 1 year in morbidly obese Korean patients. Obes Surg. 2005;15:1469–75.
Gumbs AA, Gagner M, Dakin G, et al. Sleeve gastrectomy for morbid obesity. Obes Surg. 2007;17:962–9.
Weiner RA, Weiner S, Pomhoff I, et al. Laparoscopic sleeve gastrectomy—influence of sleeve size and resected gastric volume. Obes Surg. 2007;17:1297–305.
Braghetto I, Korn O, Valladares H, et al. Laparoscopic sleeve gastrectomy: surgical technique, indications and clinical results. Obes Surg. 2007;17:1442–50.
Iannelli A, Dainese R, Piche T, et al. Laparoscopic sleeve gastrectomy for morbid obesity. World J Gastroenterol. 2008;14:821–7.
Nocca D, Krawczykowsky D, Bomans B, et al. A prospective multicenter study of 163 sleeve gastrectomies: results at 1 and 2 years. Obes Surg. 2008;18:560–5.
Kasalicky M, Michalsky D, Housova J, et al. Laparoscopic sleeve gastrectomy without an over-sewing of the staple line. Obes Surg. 2008;18:1257–62.
Frezza EE, Reddy S, Gee LL, et al. Complications after sleeve gastrectomy for morbid obesity. Obes Surg. 2009;19:684–7.
Fuks D, Verhaeghe P, Brehant O, et al. Results of laparoscopic sleeve gastrectomy: a prospective study in 135 patients with morbid obesity. Surgery. 2009;145:106–13.
Brethauer SA, Hammel JP, Schauer PR. Systematic review of sleeve gastrectomy as staging and primary bariatric procedure. Surg Obes Relat Dis. 2009;5:469–75.
Rubin M, Yehoshua RT, Stein M, et al. Laparoscopic sleeve gastrectomy with minimal morbidity. Early results in 120 morbidly obese patients. Obes Surg. 2008;18:1567–70.
Tucker ON, Szomstein S, Rosenthal RJ. Indications for sleeve gastrectomy as a primary procedure for weight loss in the morbidly obese. J Gastrointest Surg. 2008;12:662–7.
Ross MD, Gagner M. The first International Consensus Summit for sleeve gastrectomy (SG), New York City, October 25–27, 2007. Obes Surg. 2008;18:487–96.
Felberbauer FX, Langer F, Shakeri-Manesch S, et al. Laparoscopic sleeve gastrectomy as an isolated bariatric procedure: intermediate-term results from a large series in three Austrian centers. Obes Surg. 2008;18:814–8.
Karamanakos SN, Vagenas K, Kalfarentzos F, et al. Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and paptide-YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy. A prospective, double blind study. Ann Surg. 2008;247:401–7.
Lakdawala MA, Bhasker A, Mulchandani D, et al. Comparison between the results of laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass in the indian population: a retrospective 1 year study. Obes Surg. 2010;20:1–6.
Peterli R, Wölnerhanssen B, Peters T, et al. Improvement in glucose metabolism after bariatric surgery: comparison of laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy: a prospective randomized trial. Ann Surg. 2009;250:234–41.
Gehrer S, Kern B, Peters T, et al. Fewer nutrient deficiencies after laparoscopic sleeve gastrectomy (LSG) than after laparoscopic Roux-Y-gastric bypass (LRYGB)-a prospective study. Obes Surg. 2010;20:447–53.
Conflict of Interest Disclosure
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leyba, J.L., Aulestia, S.N. & Llopis, S.N. Laparoscopic Roux-en-Y Gastric Bypass Versus Laparoscopic Sleeve Gastrectomy for the Treatment of Morbid Obesity. A Prospective Study of 117 Patients. OBES SURG 21, 212–216 (2011). https://doi.org/10.1007/s11695-010-0279-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-010-0279-8