Abstract
Background
Bariatric surgery is currently the most effective treatment for morbid obesity. It provides not only substantial weight loss, but also resolution of obesity-related comorbidities. Laparoscopic sleeve gastrectomy (LSG) has rapidly been gaining in popularity. However, there are limited data on the reduction of obesity-related comorbidities for LSG compared to laparoscopic Roux-en-Y gastric bypass (LRYGB). The aim of this study was to assess the effectiveness of laparoscopic LSG versus LRYGB for the treatment of obesity-related comorbidities.
Methods
A total of 558 patients who underwent either LSG or LRYGB for morbid obesity at the Westchester Medical Center between April 2008 and September 2010 were included. Data were collected prospectively into a computerized database and reviewed for this study. Fisher’s exact test analyses compared 30-day, 6-month, and 1-year outcomes of obesity-related comorbidities.
Results
A total of 558 patients were included in the analysis of obesity-related comorbidity resolution; 200 underwent LSG and 358 underwent LRYGB. After 1 year, 86.2 % of the LSG patients had one or more comorbidities in remission compared to 83.1 % LRYGB patients (P = 0.688). With the exception of GERD (−0.09 vs. 50 %; P < 0.001), similar comorbidity remission rates were observed between LSG and LRYGB for sleep apnea (91.2 vs. 82.8 %; P = 0.338), hyperlipidemia (63 vs. 55.8 %; P = 0.633), hypertension (38.8 vs. 52.9 %; P = 0.062), diabetes (58.6 vs. 65.5 %; P = 0.638), and musculoskeletal disease (66.7 vs. 79.4 %; P = 0.472).
Conclusions
Laparoscopic sleeve gastrectomy markedly improves most obesity-related comorbidities. Compared to LRYGB, LSG may have equal in reducing sleep apnea, hyperlipidemia, hypertension, diabetes, and musculoskeletal disease. LRYGB appears to be more effective at GERD resolution than LSG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Obesity is a worldwide epidemic disease. Morbidly obese patients have a high prevalence of obesity-related comorbidities [1]. Bariatric surgery is the most reliable method for obtaining significant and sustained weight loss, which in turn results in improved comorbidities and survival [2]. Laparoscopic sleeve gastrectomy (LSG) is a newer procedure that is being performed with increasing frequency for the treatment of obesity and obesity-related diseases. It was initially performed as part of a biliopancreatic diversion with duodenal switch and subsequently was promoted as the initial part of a staged procedure for the super obese [3–5].
Sleeve gastrectomy is commonly used as a stand-alone operation and is performed laparoscopically [6]. It has been shown to have multiple advantages when compared with other bariatric surgery procedures. Sleeve gastrectomy is becoming increasingly popular because when compared to Roux-en-Y gastric bypass (RYGB), it is relatively easier to perform, preserves the pylorus and antrum, avoids complications with the gastrojejunostomy or jejuno-jejunostomy, has no risk of internal hernia, and results in less dumping syndrome [7].
LRYGB is currently the most commonly performed bariatric surgery worldwide because of its effective long-term weight loss as well as amelioration of comorbidities [2, 8]. Recent studies have shown that LSG can achieve a satisfactory weight loss and resolution of comorbidities at 3–5 years of follow-up [9]. Kehagias et al. [10] compared LSG to LRYGB in a randomized trial and demonstrated that LSG and LRYGB are equally safe and effective in the amelioration of comorbidities. However, results did not attain statistical significance due to the small sample size.
The purpose of this study was to analyze a prospectively maintained database at a tertiary-care teaching hospital between April 2008 and September 2010 and assess the effectiveness of LSG compared to LRYGB with respect to reduction of obesity-related comorbidities. The comorbidities analyzed include hypertension (HTN), type 2 diabetes mellitus (T2DM), obstructive sleep apnea (OSA), hyperlipidemia (LPD), gastroesophageal reflux disease (GERD), and musculoskeletal disease.
Patients and methods
This is a prospective, single-institution, observational study that analyzed 1 year of follow-up outcomes from our American College of Surgeons Bariatric Surgery Center Network (ACS-BSCN)-accredited program. A total of 558 patients underwent either LSG or LRYGB as treatment for morbid obesity between April 2008 and September 2010 at the Westchester Medical Center. Inclusion criteria for bariatric surgery followed 1991 NIH guidelines with a BMI ≥ 40 kg/m2 or a BMI > 35 kg/m2 with associated comorbidities; All the operations were performed by the same surgical team that included three primary surgeons and minimally invasive surgery (MIS) fellows. All patients were evaluated preoperatively by a multidisciplinary team. Patients were followed longitudinally postoperatively in the office setting on a regular basis. The patients were required to complete a questionnaire that included a list of their current medications and symptoms related to their comorbidities. Data included baseline variables as well as outcomes at 30 days, 6 months, 12 months, and yearly thereafter.
Surgical technique
All cases were performed by the same surgical team. In LSG, a 38–40-Fr bougie was used to size the sleeve and the distance for first firing at the antrum for the sleeve was 4–5 cm from the pylorus. The staple line was oversewn with a running 2–0 Vicryl suture. The LRYGB technique included the formation of a small gastric pouch (15–20 ml), 50-cm biliopancreatic limb, a 120–150-cm Roux limb, hand-sewn small gastrojejunostomy(1 cm), and retrocolic–retrogastric Roux-en-Y reconstruction.
Postoperative care
Patients were kept on clear liquids for 3 days, then advanced to pureed food for the next 2 weeks, and then to soft food. Patients were encouraged to take high-protein food. Pepcid and Actigall were prescribed to all patients for 6 months after surgery. All patients received daily multivitamin and mineral supplementation. A complete laboratory workup was performed at 3 months, 6 months, 1 year, and yearly thereafter to evaluate CBC, fasting glucose, HbA1C, lipid profile, and potential mineral or vitamin deficiencies.
Data collection
Data were collected prospectively during the preoperative visit and postoperative visits at 30 days, 6 months, and 1 year. A form was completed during each visit to assess the evolution of obesity-related comorbidities, including sleep apnea, GERD, hyperlipidemia, hypertension, diabetes, and musculoskeletal disease. This evaluation was based on the individual patient’s interview and the lab results. Weight loss was assessed using the evolution of the excess BMI loss (%EBL). Follow-up rate after LSG was 80 % at 30 days, 67 % at 6 months, and 46 % at 1 year. The follow-up rate after LRYGB was 80.7 % at 30 days, 67.8 % at 6 months, and 54.2 % at 1 year.
Definition of comorbidities
The five comorbidities followed in this study were defined as follows:
Sleep apnea is repeated episodes of upper-airway occlusion during sleep with or without sleepiness and a high apnea–hypopnea index and the need for nasal continuous positive airway pressure during sleep.
GERD is when the patient needs proton pump inhibitor (PPI) agents and/or has esophagitis revealed on endoscopy.
Hyperlipidemia is a fasting lipid profile of HDL < 40 mg/dl for men and <50 mg/dl for women, and/or TG > 150, and/or LDL > 100 mg/dl, or use of lipid-lowering agents.
Hypertension is defined as SBP ≥ 140 and/or DBP ≥ 90 mmHg or the use of antihypertensive drug therapy.
Diabetes is a fasting plasma glucose of ≥126 mg/dl or a 2-h plasma glucose ≥200 mg/dl during OGTT or the use of antidiabetic drug ± insulin therapy.
Musculoskeletal disease is shown with clinical and radiological documentation.
Statistical analysis
Continuous data analyses were performed using Student’s t test. Fisher’s exact test was used to compare 30-day, 6-month, and 1-year outcomes of obesity-related comorbidities. A P value of <0.05 was considered statistically significant.
Results
The study included 558 morbidly obese patients. Of the 558 patients, 200 underwent LSG and 358 had LRYGB. The demographics of LSG versus LRYGB patients were as follows: age = 44.2 ± 11.8 versus 47.5 ± 18.5 years, BMI = 47.9 ± 10.2 versus 46.1 ± 7.1 kg/m2, female 71 versus 79.1 %. The most common obesity-related comorbidity was hypertension (HTN), which occurred in 52 % in both groups. Compared to LRYGB patients, the LSG group has a higher percentage of sleep apnea present at baseline, but there was no statistical difference between the two groups with respect to GERD, hyperlipidemia, HTN, type 2 diabetes mellitus (T2DM), and musculoskeletal disease at baseline (Table 1).
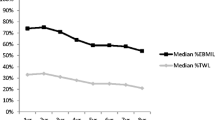
The %EBL is the best way to report weight loss and the improvement in metabolic syndrome in morbidly obese patients [11]. The %EBL after LSG versus LRYGB was 10.2 versus 9.3 % at 30 days, 23 versus 24.5 % at 6 months, and 30.7 versus 33.4 % at 1 year. There was no significant statistical difference between the two groups (Fig. 1).
The six obesity-related comorbidities were tracked over time for evaluating the clinical effectiveness of LSG and LRYGB. The reduction in each comorbidity over time was shown individually.
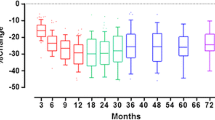
The percentage of patients with sleep apnea in the LSG group was 34, 24, 14.9, and 3.26 % at baseline, 30 days, 6 months, and 1 year compared to 25.1, 6.2, 3.1, and 4.15 % for the LRYGB group. The sleep apnea in both groups had a significant improvement in 1 year (P < 0.001 in both groups) (Fig. 2). Table 2 shows that the LRYGB group had statistically earlier resolution of sleep apnea than the LSG group at 30 days and 6 months. However, there was no statistical significant difference in the improvement of sleep apnea between two groups at 1 year.
The prevalence of GERD in the LSG group was 13 % at baseline, 12.8 % at 30 days, 11.4 % at 6 months, and 13.2 % at 1 year compared to 13.7, 10, 9.5, and 7.3 %, respectively, in the LRYGB group. Figure 3 shows that GERD in the LSG group did not improve at 1 year (P = 0.885); however, GERD significantly improved after LRYGB at 1 year (P = 0.037). Table 3 indicates that one patient without GERD at baseline suffered from GERD at 1 year following LSG, which suggests that LSG may increase the risk of GERD after surgery.
The prevalence of hyperlipidemia in the LSG group was 25.5 % at baseline, 19 % at 30 days, 12.9 % at 6 months, and 11.1 % at 1 year compared to 27.1, 21.9, 17.4, and 12 % in the LRYGB group. Figure 4 shows that the significant improvement of hyperlipidemia at 1 year in both groups (P = 0.0049 for the LSG group and P < 0.001 for the LRYGB group). The statistical difference in the resolution of hyperlipidemia for LSG versus LRYGB was insignificant (Table 4).
The resolution of hypertension in both groups is shown in Fig. 5. The percentage of patients with hypertension in the LSG group was 52 % at baseline, 41.4 % at 30 days, 34.4 % at 6 months, and 37.8 % at 1 year. The LRYGB group had 52.5, 39.4, 32.1, and 25.8 % at baseline, 30 days, 6 months, and 1 year, respectively. Both groups demonstrated significant resolution of hypertension (P = 0.034 in the LSG group and P < 0.001 in the LRYGB group). Analysis of the reduction of hypertension showed that there was no significant difference between the two groups (Table 5).
Figure 6 indicates that the prevalence of diabetes in the LSG group was 28 % at baseline, 14.6 % at 30 days, 9.9 % at 6 months, and 13.5 % at 1 year. The corresponding diabetes rates in the LRYGB group were 31.8, 13.5, 10.3, and 10.4 %, respectively. The improvement of diabetes at 1 year was significant in both groups (P = 0.011 in the LSG group and P < 0.001 in the LRYGB group). There was no significant difference in the resolution of diabetes between the two groups (Table 6).
The percentage of patients with musculoskeletal disease in the LSG group was 20 % at baseline, 6.25 % at 30 days, 3.73 % at 6 months, and 5.62 % at 1 year compared to 18.7, 3.1, 2.5, and 3.7 % in the LRYGB group. Figure 7 shows the improvement of musculoskeletal disease after LSG and LRYGB (P = 0.003 in the LSG group and P < 0.001 in the LRYGB group). There was no significant difference in the resolution of musculoskeletal disease between the two groups (Table 7).
Discussion
This study was a single-institution, prospective, longitudinal data collection and analysis study. Both procedures were performed and patients were followed up by the same surgical team. Patients in both groups had similar demographics. To the best of our knowledge, this study is the largest single-center comparative study on resolution of comorbidities between LSG and LRYGB.
Currently, LRYGB is considered the gold standard procedure for morbid obesity, and it leads to excellent long-term sustained weight loss and remarkable resolution of comorbidities [12]. However, LRYGB is a technically difficult operation and patients who undergo LRYGB have a higher risk of vitamin deficiency afterward. LSG is a restrictive procedure that is becoming more popular as it is easier to perform and is associated with less malabsorption compared to LRYGB [13]. Studies have shown that LSG provides satisfactory weight loss and comorbidity resolution [14–17]. Hutter et al. [18] analyzed the data of 28,616 patients from July 2007 to September 2010 from the ACS-BSCN. They concluded that the morbidity and effectiveness of LSG is somewhere between that of laparoscopic adjustable gastric banding (LAGB) and LRYGB/ORYGB (open Roux-en-Y gastric bypass). However, that was a multicenter study and had limitations as to how procedures were performed and how data were collected.
Our data suggest that both LSG and LRYGB provide significant weight loss and we found no statistical difference between LSG and LRYGB in weight loss at the 1-year follow-up. Weight loss after LSG as reported in the literature is variable. It may depend on multiple factors, including the size of the sleeve created, the size of antrum retained, and the amount of fundus resected.
A consensus report on the best practice guidelines for the performance of LSG, with recommendations for the standardization of techniques and adoption of working recommendations formulated according to expert experience with over 12,000 cases, was published recently [19].
The goal of bariatric surgery is not only satisfactory weight loss, but also improvement in obesity-related comorbidities, including sleep apnea, hyperlipidemia, hypertension, diabetes, and musculoskeletal disease.
Obesity is a well-known risk factor for OSA [20, 21]. The prevalence of OSA in our data was 28.3 %. Schafer et al. [22] reported that OSA severity is significantly correlated with fat accumulation in the intra-abdominal region. The most important therapy for OSA in obese patients is weight loss. Weight loss changes pharyngeal anatomy and decreases airway collapsibility by increasing the pharyngeal closing pressure [23]. Bariatric surgery is the most effective way to lose weight. Our study shows a dramatic reduction of OSA after LSG and LRYGB. The resolution rate at 1 year is 91.2 % in the LSG group and 82.8 % in the LRYGB group. Interestingly, our study shows that the resolution of OSA in the LRYGB group is faster than in the LSG group, 76.3 versus 36.1 % at 30 days and 87.7 versus 66.7 % at 6 months. Since the rate of weight loss in both groups is similar, some other factors after surgery may play a role. There is growing evidence that hormonal changes underlie the association between OSA and obesity. The most well-studied adipocyte-derived factor affecting respiratory control is leptin [24], which was initially determined to have a primary role of binding to receptors in the hypothalamus to reduce satiety and increase metabolism. Although the level of leptin after LSG and LRYGB was decreased, gastric bypass may promote a greater degree of leptin change than LSG in the early postoperative period [25]. This phenomenon could perhaps explain the rapid amelioration of OSA in LRYGB. Nevertheless, in our series the resolution rate of OSA at 1 year is comparable in both groups.
GERD is the only comorbidity for which there was a significant difference between LSG and LRYGB in our study. There was a significant improvement of GERD in the LRYGB group and a reduction rate of 50 % at 1 year. However the incidence of GERD symptoms after LSG is an issue of concern. In the LSG group, 13 % of the patients were suffering from GERD before surgery. The number of patients who complained of GERD at the end of 1 year slightly increased to 13.2 % in the LSG group. This finding is consistent with most studies that have reported an increase in GERD during the first year following LSG [14, 26]. Some surgical techniques may increase the risk of GERD after LSG including narrowing incisura angularis which may lead to dilatation of fundus, and persistence of hiatal hernia with a wild cardia. In our study, we routinely corrected hiatal hernia, avoided strictures at the incisura angularis and stapled close to the esophagus at the angle of His. We have observed GERD worsen in some patients, but we have also seen it improved in many patients. The exact mechanism of the development of GERD after LSG is still under investigation. It has been shown that intragastric pressure after saline infusion increases after sleeve gastrectomy [27]. Lack of gastric compliance, severely restricted gastric capacity with an intact pylorus, division of sling fibers, and impaired gastric emptying have also been suggested as factors leading to increased reflux after LSG [28]. During the LSG procedure, the angle of His is resected thus affecting the lower esophageal sphincter (LES) and the resting pressure is reduced [29]. The hypotensive LES, either preexisting or as a result of LSG, could have led to the onset of new GERD symptoms [30]. With respect to GERD, we have to stress the advantage of the gastric bypass compared to gastric sleeve. The minimal acid production of the gastric pouch in LRYGB results in no acid-reflux esophagitis and the Roux loop of 120–150 cm inhibits biliary reflux. However, some publications on the effect of LSG on reflux symptoms are controversial. Himpens et al. [31] reported that the appearance of GERD in 21.8 % of patients after 1 year, but 3 years later only 3.1 % of patients had GERD. The explanation for this improvement is believed to be related to accelerated gastric emptying observed in patients with LSG and a decrease of intra-abdominal pressure when a reduction in body weight is obtained. Therefore, further analysis reflecting the long-term effects of LSG on GERD is necessary in order to draw more definitive conclusions.
In general, LRYGB is considered to result in the better remission of diabetes compared to LSG. In our series, the remission of diabetes after LSG versus LRYGB was 48.9 versus 56.2 % at 30 days, 69 versus 66.7 % at 6 months, and 58.6 versus 65.5 % at 1 year. Statistically, LRYGB is not more effective than LSG in the remission of diabetes. Bariatric surgery was called “diabetes surgery” during the first Diabetes Surgery Summit in 2008 because it has been recognized that bariatric surgery is a valuable tool to treat obesity and T2DM. A report by Hutter et al. [18] in 2011 showed that 55 % of patients who were diabetic at baseline had resolution or improvement of their diabetes 1 year after LSG compared to 44 % after LAGB and 83 % after LRYGB. Nevertheless, the high rate of resolution of diabetes after LSG has also been reported by many researchers [9, 14, 17]. The mechanisms of T2DM resolution after surgery are not completely understood. Certainly, surgery-induced weight loss and subsequent decrease in adiposity and lipotoxicity are responsible for the long-term benefits in metabolic function. Current data suggest that hormonal mechanisms other than weight loss alone account for the beneficial effect of bariatric surgery on T2DM [32]. The importance of gut hormones in mediating weight loss and resolution of T2DM after LRYGB is clear. The immediate weight loss independent of T2DM resolution after LRYGB suggests that surgery modifies the enteroinsular axis. Changes in gut hormones such as ghrelin, peptide YY (PYY), and glucagon-like peptide-1 (GLP-1) after LRYGB are well documented. The increasing level of GLP-1 appears to be critical for improving the response to insulin. The primary function of GLP-1 includes the potentiation of glucose-stimulated insulin secretion, enhancement of β-cell growth and survival, inhibition of glucagon release, and control of food intake. LRYGB reduces the volume of the gastric pouch and bypasses the duodenum, which allows for rapid gastric emptying, thus enhancing GLP-1′s effect. Dramatic increases in the level of GLP-1 immediately after LRYGB and postsurgical increases in postprandial GLP-1 have been observed. Similarly, an increase in fasting and postprandial GLP-1 has been reported following sleeve gastrectomy [33]. Ramon et al. [25] compared the effects of both LSG and LRYGB on glucose metabolism, fasting, and meal-stimulated gut hormone levels and suggested that LSG is more than a restrictive procedure. The postprandial ghrelin, GLP-1, and PYY levels in patients who underwent LSG, at least at 12 months after surgery, are similar to those of patients who had LRYGB. This conclusion supports our result that there was no difference between LSG and LRYGB with respect to remission of T2DM at 12 months.
Hypertension is the most common comorbidity in the obese. Fifty-two percent of obese patients present with hypertension at baseline. The reduction of hypertension, defined as being completely off antihypertensives, with LSG versus LRYGB is 22.5 versus 23.5 % at 30 days, 39.2 versus 40 % at 6 months, and 38.8 versus 52.9 % at 1 year. Both procedures show significant resolution of hypertension. It is also noted that many patients reduce the dose of medicine for hypertension after surgery. Though the exact mechanism of how obesity causes hypertension is unknown, it might be attributed to the neuroendocrine mechanism such as the renin-angiotensin-aldosterone system [34]. Adipose tissue deposition can lead to irregular functioning of the kidney, which can subsequently lead to alteration of blood pressure [35]. Critical weight loss is an effective way to control obesity-related hypertension. Weight loss after LSG and LRYGB will lead to a significant reduction in blood pressure.
Other metabolic outcomes such as resolution of hyperlipidemia and musculoskeletal disease are similar in the LSG group and the LRYGB group. Both hyperlipidemia and musculoskeletal disease are remarkably improved at 1 year after LSG and LRYGB. Sixty-three percent of LSG patients had their hyperlipidemia resolve at 1 year compared to 55.8 % for LRYGB patients. Musculoskeletal disease resolved at 1 year in 66.7 % of LSG patients compared to 79.4 % of LRYGB patients. The result is comparable for both groups.
Overall, both LSG and LRYGB demonstrated a significant weight loss effect at the end of 1 year. Resolution of hyperlipidemia, hypertension, diabetes, and musculoskeletal diseases is comparable for LSG and LRYGB. Although resolution of OSA seems to occur earlier with LRYGB compared to LSG, the results are similar in both groups at 1 year. GERD is the only comorbidity that we analyzed which demonstrated a significant difference between the two groups. Our study demonstrates that LRYGB is more efficacious for the relief of GERD symptoms compared to LSG. LSG may increase the incidence of GERD at 1 year.
The uncontrollable limitation of this study is the selection bias by surgeons or patients in regard to which procedure was performed. However, our data in both groups were similar in regard to age, gender, race, BMI, and most comorbidities except for sleep apnea. Another limitation is that our outcomes are based on short-term follow-up data. Long-term follow-up needs to be conducted to further evaluate the reduction of comorbidities with both types of intervention.
Conclusion
This study demonstrates significant weight loss at 1 year after LSG and LRYGB. Hypertension is the most common comorbidity in obese patients. LRYGB is not superior to LSG in the reduction of sleep apnea, hyperlipidemia, hypertension, diabetes, and musculoskeletal disease at 1 year. However, LSG seems less effective than LRYGB for GERD. In fact, LSG may increase the incidence of GERD at 1 year after surgery.
References
Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK (2008) Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity 16:2323–2330
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292:1724–1737
Hess DS, Hess DW (1998) Biliopancreatic diversion with a duodenal switch. Obes Surg 8:267–282
Cottam D, Qureshi FD, Mattar SG, Sharma S, Holover S, Bonanomi G, Ramanathan R, Schauer P (2006) Laparoscopic sleeve gastrectomy as an initial weight-loss procedure for high risk patients with morbid obesity. Surg Endosc 20:859–863
Regan JP, Inabnet WB, Gagner M, Pomp A (2003) Early experience with two-stage laparoscopic Roux-en-Y gastric bypass as an alternative in the super–super obese patient. Obes Surg 13:861–864
Ren CJ, Patterson E, Gagner M (2000) Early results of laparoscopic biliopancreatic diversion with duodenal switch: a case series of 40 consecutive patients. Obes Surg 10:514–523
Brethauer SA, Hammel JP, Schauer PR (2009) Systematic review of sleeve gastrectomy as staging and primary bariatric procedure. Surg Obes Relat Dis 5:469–475
Nguyen NT, Root J, Zainabadi K, Sabio A, Chalifoux S, Stevens CM, Mavandadi S, Longoria M, Wilson SE (2005) Accelerated growth of bariatric surgery with the introduction of minimally invasive surgery. Arch Surg 140:1198–1202
Boza C, Salinas J, Salgado N, Pérez G, Raddatz A, Funke R, Pimentel F, Ibáñez L (2012) Laparoscopic sleeve gastrectomy as a stand-alone procedure for morbid obesity: report of 1,000 cases and 3-year follow-up. Obes Surg 22(6):866–871
Kehagias I, Karamanakos SN, Argentou M, Kalfarentzos F (2011) Randomized clinical trial of laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy for the management of patients with BMI < 50 kg/m2. Obes Surg 21:1650–1656
Rossi M, Serpa Neto A, Rossi FM, Amarante RD, Alcântara GC Jr, da Silva RB, Regina PF (2009) Percentage of excess BMI lost correlates better with improvement of metabolic syndrome after Roux-en-Y gastric bypass in morbidly obese subjects: anthropometric indexes and gastric bypass. Surg Obes Relat Dis 5:11–18
Suter M, Donadini A, Romy S, Demartines N, Giusti V (2011) Laparoscopic Roux-en-Y gastric bypass: significant long-term weight loss, improvement of obesity-related comorbidities and quality of life. Ann Surg 254:267–273
Keren D, Matter I, Rainis T, Lavy A (2011) Getting the most from the sleeve: the importance of post-operative follow-up. Obes Surg 21:1887–1893
Chopra A, Chao E, Etkin Y, Merklinger L, Lieb J, Delany H (2012) Laparoscopic sleeve gastrectomy for obesity: can it be considered a definitive procedure? Surg Endosc 26:831–837
Srinivasa S, Hill LS, Sammour T, Hill AG, Babor R, Rahman H (2010) Early and mid-term outcomes of single-stage laparoscopic sleeve gastrectomy. Obes Surg 20(11):1484–1490
D’Hondt M, Vanneste S, Pottel H, Devriendt D, Van Rooy F, Vansteenkiste F (2011) Laparoscopic sleeve gastrectomy as a single-stage procedure for the treatment of morbid obesity and the resulting quality of life, resolution of comorbidities, food tolerance, and 6-year weight loss. Surg Endosc 25:2498–2504
Arias E, Martinez PR, Ka Ming Li V, Szomstein S, Rosenthal R (2009) Mid-term follow-up after sleeve gastrectomy as a final approach for morbid obesity. Obes Surg 19:544–548
Hutter MM, Schirmer BD, Jones DB, Ko CY, Cohen ME, Merkow RP, Nguyen NT (2011) First report from the American College of Surgeons Bariatric Surgery Center Network: laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ann Surg 254:410–420
Rosenthal RJ, Diaz AA, Arvidsson D, Baker RS, Basso N, Bellanger D (2012) International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of >12,000 cases. Surg Obes Relat Dis 8:8–19
Akinnusi ME, Saliba R, Porhomayon J, El-Solh AA (2012) Sleep disorders in morbid obesity. Eur J Intern Med 23:219–226
Young T, Peppard PE, Taheri S (2005) Excess weight and sleep-disordered breathing. J Appl Physiol 99:1592–1599
Schafer H, Pauleit D, Sudhop T, Gouni-Berthold I, Ewig S, Berthold HK (2002) Body fat distribution, serum leptin, and cardiovascular risk factors in men with obstructive sleep apnea. Chest 122:829–839
Sutherland K, Lee RW, Phillips CL, Dungan G, Yee BJ, Magnussen JS, Grunstein RR, Cistulli PA (2011) Effect of weight loss on upper airway size and facial fat in men with obstructive sleep apnoea. Thorax 66:797–803
Shuldiner AR, Yang R, Gong DW (2011) Resistin, obesity and insulin resistance—the emerging role of the adipocyte as an endocrine organ. N Engl J Med 345:1345–1346
Ramón JM, Salvans S, Crous X, Puig S, Goday A, Benaiges D, Trillo L, Pera M, Grande L (2012) Effect of Roux-en-Y gastric bypass vs sleeve gastrectomy on glucose and gut hormones: a prospective randomised trial. J Gastrointest Surg 16(6):1116–1122
Lakdawala MA, Bhasker A, Mulchandani D, Goel S, Jain S (2010) Comparison between the results of laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass in the Indian population: a retrospective 1 year study. Obes Surg 20:1–6
Yehoshua R, Eidelman L, Stein M, Fichman S, Mazor A, Chen J, Bernstine H, Singer P, Dickman R, Beglaibter N, Shikora SA, Rosenthal RJ, Rubin M (2008) Laparoscopic sleeve gastrectomy–volume and pressure assessment. Obes Surg 18:1083–1088
Keidar A, Appelbaum L, Schweiger C, Elazary R, Baltasar A (2010) Dilated upper sleeve can be associated with severe postoperative gastroesophageal dysmotility and reflux. Obes Surg 20:140–147
Braghetto I, Lanzarini E, Korn O, Valladares H, Molina JC, Henriquez A (2010) Manometric changes of the lower esophageal sphincter after sleeve gastrectomy in obese patients. Obes Surg 20(3):357–362
Klaus A, Weiss H (2008) Is preoperative manometry in restrictive bariatric procedures necessary? Obes Surg 18:1039–1042
Himpens J, Dapri G, Cadiere GB (2006) A prospective randomized study between laparoscopic gastric banding and laparoscopic isolated sleeve gastrectomy: results after 1 and 3 years. Obes Surg 16:1450–1456
Ochner CN, Gibson C, Shanik M, Goel V, Geliebter A (2011) Changes in neurohormonal gut peptides following bariatric surgery. Int J Obes (Lond) 35:153–166
Scott WR, Batterham RL (2011) Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy: understanding weight loss and improvements in type 2 diabetes after bariatric surgery. Am J Physiol Regul Integr Comp Physiol 301:R15–R27
Sarkhosh K, Birch DW, Shi X, Gill RS, Karmali S (2012) The impact of sleeve gastrectomy on hypertension: a systematic review. Obes Surg 22:832–837
Kotchen TA (2010) Obesity-related hypertension: epidemiology, pathophysiology, and clinical management. Am J Hypertens 23:1170–1178
Acknowledgments
We thank Nancy Nolan, RN, who worked on the data collection system and provided the detailed data for statistical analysis.
Disclosures
Niu Zhang, Anthony Maffei, Thomas Cerabona, Juan Omana, Anil Pahuja and Ashutosh Kaul have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, N., Maffei, A., Cerabona, T. et al. Reduction in obesity-related comorbidities: is gastric bypass better than sleeve gastrectomy?. Surg Endosc 27, 1273–1280 (2013). https://doi.org/10.1007/s00464-012-2595-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2595-7