Abstract
Osteoarthritis (OA) continues to be one of the leading causes of ‘years lived with disability’ worldwide. Symptomatic knee OA is highly prevalent among people aged 50 years and over and is destined to become an ever more important healthcare problem. Current management of knee OA includes non-pharmacological and pharmacological treatments. Spa therapy is one of the most commonly used non-pharmacological approaches for OA in many European countries, as well as in Japan and Israel. Despite its long history and popularity, spa treatment is still the subject of debate and its role in modern medicine continues to be unclear. The objective of this review is to summarize the currently available information on clinical effects and mechanisms of action of spa therapy in knee OA. Various randomized controlled clinical trials (RCTs) were conducted to assess the efficacy and tolerability of balneotherapy and mud-pack therapy in patients with knee OA. Data from these clinical trials support a beneficial effect of spa therapy on pain, function and quality of life in knee OA that lasts over time, until 6–9 months after the treatment. The mechanisms by which immersion in mineral or thermal water or the application of mud alleviate suffering in OA are not fully understood. The net benefit is probably the result of a combination of factors, among which the mechanical, thermal and chemical effects are most prominent. In conclusion, spa therapy seems to have a role in the treatment of knee OA. Additional RCTs and further studies of mechanisms of action with high methodological quality are necessary to prove the effects of spa therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) continues to be one of the leading causes of ‘years lived with disability’ worldwide (Woolf and Pfleger 2003). Symptomatic knee OA is highly prevalent among people aged 50 years and over in most parts of the world and is destined to become an ever more important healthcare problem (Busija et al. 2010; Fautrel et al. 2005). Knee OA is associated with symptoms of pain and functional disability that reduce quality of life (QoL) and increase the risk of further morbidity and mortality. Current management of knee OA includes non-pharmacological (for example, education, exercise, lifestyle changes) and pharmacological (for example, paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs), topical drugs) treatments. According to EULAR recommendations, paracetamol is the oral analgesic to try first and, if successful, to prefer for long-term treatment. Other suggested drugs are NSAIDs or selective cyclooxygenase-2 (COX-2) inhibitors (coxibs) (Jordan et al. 2003).
Spa therapy is one of the most commonly used non-pharmacological approaches for OA in many European and Middle Eastern countries, as well as in Japan and Israel, in classical medicine as a cure for various illnesses. However, despite the long history and popularity of spa therapy, its role in modern medicine is still not clear (Verhagen et al. 2007).
Spa therapy comprises a broad spectrum of therapeutic modalities including hydrotherapy, balneotherapy, mud-pack therapy, physiotherapy and exercise (Verhagen et al. 2007). Spa treatment usually consists of a health holiday lasting some 2–3 weeks and creates a special therapeutic ‘atmosphere’ of its own that can lead to the placebo effect. This condition plays an important role in reducing pain and improving the patient’s general well-being (Bender et al. 2005). Balneotherapy uses natural thermal mineral waters, whose definition is based on the sum of the cations Na, K, Ca and Mg and the anions of SO4, Cl and HCO3. It was presumed that most mineral ingredients would be adsorbed through the skin, which is an active immune organ and may play an important role in the mechanism, but to date, this has not been confirmed (Bender et al. 2005). Mud-pack is defined as a natural product that consists of a mixture of mineral or mineral-medicine water (or seawater or salt water from lakes) with organic or inorganic material produced from biological and/or geological processes and used as a therapeutic treatment in the form of a mud wrap applied locally or to the whole body. The main use of the treatment is to relieve rheumatic musculoskeletal pain. Various systematic reviews and meta-analyses on spa therapy for rheumatic diseases have recently been published (Verhagen et al. 2007; Harzy et al. 2009). The Authors conclude that there is encouraging evidence to suggest that spa therapy is effective and safe for the treatment of patients with knee OA, although the results of the existing studies are not strong enough to draw firm conclusions. In an era of evidence-based medicine, it is necessary to ask what real medical and scientific value these therapies have.
The objective of this review is to summarize the currently available information on clinical effects and briefly discuss the possible mechanisms of action of spa therapy in knee OA. We also provide some suggestions for further development in this area.
Methods
We conducted a search of the literature concerning clinical studies about spa therapy in knee OA in October 2013 and in particular, we examined the period between October 2003 and September 2013. First of all, the strategy to select the clinical studies consisted in a detailed search in scientific databases Pubmed, Scopus, Cochrane Library and EMBASE. The keywords were ‘spa therapy’, ‘mud’, ‘mud-bath’, ‘balneotherapy’ in combination with ‘osteoarthritis’, ‘gonarthrosis’, ‘arthrosis’ and ‘knee osteoarthritis’. Studies were considered eligible if they met the following criteria: (i) patients had a diagnosis of knee OA, who fulfilled the ACR criteria (Altman et al. 1986); (ii) randomized clinical trial (RCT) design; (iii) original articles whose main objectives were to analyse the effect of spa therapy. No limitation was placed on the possible association of spa therapy with exercise intervention; (iv) studies published from 2003 to the present totally written in English language. The studies that were excluded from the review were the following: (i) those that analysed the effects of spa therapy in different joints other than the knee; (ii) reviews; (iii) an overall follow-up duration less than 8 weeks.
Results
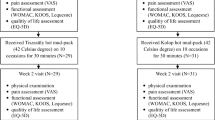
In total, 176 potential studies were found; no additional papers were found by hand searching of references. Of these, 56 studies were excluded because they were written in a language other than English. Based on the title and the abstract content, 66 of these articles were not included in our review. The full texts of the remaining 54 studies were read, and a further 39 studies were excluded, because of the lack of an RCT design (Fig. 1). We identified 14 assessable articles reporting RCTs on spa therapy in knee OA, including a total number of patients of 1198 (Tables 1, 2 and 3). Over 90 % of the participants in the studies were women. Six studies were blind with an ‘assessor’ blind to the type of treatment. In five studies, mineral baths were used; in two studies, bathing was combined with exercise treatment; six studies evaluated the effect of spa therapy, and three studies evaluated the effect of mud-pack treatment. Furthermore, we analysed the results of a study that compared the efficacy of balneotherapy and mud-pack therapy.
Studies that analyse the effects of balneotherapy in knee OA
Five studies that analysed the effect of balneotherapy in patients with knee OA were found (Table 1). Tishler et al. (2004) investigated the effect of balneotherapy in 72 patients in a double-blind RCT. Group A (48 patients) received balneotherapy, consisting in bathing in mineral water pools at 37 °C for 30 min once weekly for 6 consecutive weeks. Group B (24 patients) served as a control group who continued their daily activities and medications. Each patient was assessed 1 week before the treatment, at weeks 4, 6 and 10. Assessment included patient’s global pain through Visual Analogue Scale (VAS), the Western Ontario and Mc Master Universities OA index (WOMAC) (Bellamy et al. 1991; Salaffi et al. 2003), Lequesne’s functional index (Lequesne et al. 1987) and patient’s and physician’s assessment of change of disease severity. Every tested parameters resulted statistically significant improved in group A at weeks 4 and 6, and this variation was sustained at week 10, while no significant changes were found in group B. These results were confirmed, some years later, by Sherman et al. (2009) who evaluated the effect of balneotherapy at the Dead Sea area for patients suffering from knee OA. The Authors chose a study protocol very similar to that followed by Tishler et al. and observed a statistically significant improvement in every clinically analysed parameters, lasting up to 6 months, in the treated group (Table 1).
Subsequently, the efficacy of balneotherapy versus tap water treatment, in knee OA patients, was investigated by Yurtkuran et al. (2006) and Balint et al. (2007) in two different studies. The first author (Yurtkuran et al. 2006) enrolled 52 patients, randomly assigned to group I (treatment in the pool full of mineral water at 37 °C for 20 min a day, 5 days a week, for 2 weeks) and group II (treatment with tap water following the same protocol of group I). VAS, tenderness score (TS), 50-ft walking duration, quadriceps muscle strength (QMS), active flexion degree (AFD), WOMAC index and Nottingham Health Profile (NHP) (McDowell et al. 1978; Kücükdeveci et al. 2000) were evaluated before and after the treatment and 12 weeks later. Comparison of the groups showed that VAS, NHP pain score and TS differed significantly in favour of group I at the 2nd and 12th week. Bálint et al. (2007), in a consecutive study with similar protocol (one group received 30 min sessions of bathing, 5 days a week for 4 consecutive weeks and the other one performed tap water therapy with the same modalities), demonstrated a significant improvement of WOMAC score at the end of bathing sessions that persisted for 3 months follow-up in treated group.
Another study demonstrating the lasting over time of balneotherapy in knee OA patients was conducted by Fioravanti et al. (2012) in 2012. Sixty outpatients were included in the study and randomized into two groups: group I was treated with daily sulphate-bicarbonate-calcium mineral water at 38 °C for 20 min in a bathtub for a total of 12 applications carried out over a period of 2 weeks; group II, the control group, continued their regular outpatient care routine. At baseline, after 15 days and after 12 weeks, patients were evaluated by VAS, Lequesne index, WOMAC, short form (SF)-36 (Ware and Sherbourne 1992; Apolone and Mosconi 1998), Arthritis Impact Measurement Scale (AIMS) (Meenan et al. 1980; Salaffi et al. 1991) and symptomatic drugs consumption. A significant improvement of all parameters at the end of the treatment which persisted throughout the follow-up period was observed in group I, while no significant differences were noted in group II.
Studies that analyse the effects of spa therapy in knee OA
There are six studies that analysed the effects of spa therapy, in a broad sense, in patients with knee OA (Table 2). In 2007, Karagülle et al. (2007) performed the first study to evaluate the medium-term (up to 24 weeks) efficacy of spa therapy in radiologically and clinically severe knee OA. Twenty patients were randomly allocated into two groups. Spa group spent 10 days at spa centre, following a traditional regimen consisting of two thermal water baths at 38 °C for 30 min everyday; furthermore, they also could take part in the other spa activities (therapeutic massage, exercise, outdoor activities). Drug therapy group stayed at home and followed their individually prescribed drug therapy. Patients were assessed at baseline, after spa therapy (at week 2) and during the follow-up period at 12 and 24 weeks with Lequesne index, VAS, ten-stairs stepping up and down time, 15-m walking time and three times squatting up and down time. In the treated group, the improvement of all studied parameters, observed at the end of the therapy, lasted up to 24 weeks. More recently, the short- and long-term efficacy (up to 9 months) of spa therapy in knee OA was demonstrated by Fioravanti et al. (2010). Eighty patients were enrolled and divided in group I (40 patients treated daily with combination of mud-packs for 20 min at 45 °C and with bicarbonate-sulphate mineral bath water at 38 °C for 15 min, for a total of 12 applications in a period of 2 weeks) and group II (control group that continued their regular care). Patients were assessed at baseline, after 2 weeks and after 3, 6 and 9 months for VAS, Lequesne index, WOMAC, AIMS-1 and symptomatic drug consumption. The study pointed out not only a significant improvement of all evaluated parameters at the end of the cycle of spa therapy but also of this long lasting effect throughout the whole follow-up period. These promising results were already presented by the same authors in a previous study that considered a shorter follow-up period (12 weeks) (Cantarini et al. 2007).
However, nowadays, the longest follow-up period performed in knee OA patients who underwent spa therapy was observed by Fraioli et al. (2011). The authors found a significant improvement of clinical parameters after 3 cycles of mud-bath therapy over 1 year’s time (each cycle included 12 daily treatments consisting of mud applications to the knee and consecutive bath in mineral water). The larger multicentre trial that assessed the effect of spa therapy in knee OA remains that conducted by Forestier et al. in (2010). Four hundred fifty-one patients were enrolled and subdivided into two groups: spa group received 18 days of therapy over 3 weeks consisting in mineral hydrojet sessions, manual massages of the knee, applications of mud and general mobilization in a collective mineral water pool; control group did not receive spa therapy. Both groups continued usual treatments and performed daily standardized home exercises. This trial demonstrated that an intensive course of spa therapy with home exercise programme and usual treatment provided medium-term benefit over a home exercise programme and usual treatment alone in the management of knee OA.
The efficacy of different modalities which belong to the wider group of spa therapy were compared by Evcik et al. (2007). Eighty patients with knee OA were included and separated into three groups. Group I received balneotherapy, group II mud-pack therapy and group III hot-pack therapy. All treatments were administered once a day for 20 min, 5 days a week, for 2 weeks. Some assessed parameters (VAS, WOMAC and physician’s global assessment) were statistically significant improved in all groups at the end of therapy and after 3 months versus baseline. Instead, other outcome measures (QoL and the maximum distance that patient can walk without pain) improved only in group I and II at the end of the study and after 3 months.
Studies that analyse the effects of mud therapy in knee OA
Despite the common use, there are only few articles that evaluate the effect of mud-pack therapy alone in patients with knee OA (Espejo-Antúnez et al. 2013) (Table 3). The efficacy of mud-pack therapy on 60 knee OA patients was investigated by Odabasi et al. (2008) in a trial that consisted of two groups: study group received 15 mud applications directly to skin for 30 min daily for 3 weeks; control group was treated with mud applied to both knees over impermeable nylon film with the same frequency of the previous group. Mud-pack treatment resulted effective in improving the pain and the functional status of patients, but the direct application was found to be superior than indirect application. Also, Sarsan et al. (2012) demonstrated that mud-pack therapy is a favourable option compared with hot-pack treatment for pain relief and for the improvement of functional conditions in treating patients with knee OA.
The most recent study in this field was conducted by Tefner et al. (2013) in 2013. Fifty-three patients with knee OA were randomly allocated into two groups: one group received mud-pack therapy, and the other one received control hot-pack therapy in a total of 10 occasions, for 30 min, 5 days a week for 2 weeks. WOMAC, EuroQol-5D QoL (EuroQol Group 1990) measure and consumption of drugs were recorded before the treatment, at the end (week 2), and at week 6 and 12. The WOMAC and the EQ5D QoL scores improved from the baseline to the end of treatment in both groups, and further improvement was observed during the follow-up period. The drug consumption reduced in both groups, and these changes were significant only in the mud-treated group compared to baseline.
Possible mechanisms of action of spa therapy in OA
The mechanisms by which immersion in mineral or thermal water or the application of mud alleviate the main symptoms of OA and of other rheumatic diseases are not fully understood. The efficacy is probably the result of a combination of factors, among which mechanical, thermal and chemical effects are most prominent (Sukenik et al. 1999; Fioravanti et al. 2011a, b). A distinction can be made between the non-specific and the specific mechanisms of action. The former (hydrotherapeutic in a broad sense) consisting in simple bathing in hot tap water are well known, while the latter (hydromineral and crenotherapeutic) depending on the chemical and physical properties of the water used are difficult to identify and assess. Buoyancy, immersion, resistance and temperature all play important roles. Hot stimuli produce analgesia on nerve endings by increasing the pain threshold. It causes relief of muscle spasms through the gamma fibres of muscle spindles and activates the descending pain inhibitory system. According to the ‘gate theory’, pain relief may be due to the temperature and hydrostatic pressure of water on the skin (Melzack and Wall 1965; Guidelli et al. 2012).
Spa therapy provokes a series of neuroendocrine reactions, in particular release of adrenocorticotropic hormone (ACTH), cortisol, prolactin and growth hormone (GH), although it does not alter the circadian rhythm of these hormones. The effect of thermal stress on the hypothalamus-pituitary-adrenal axis seems to be particularly important for the anti-edemigenous and anti-inflammatory effects of corticosteroids (Kuczera and Kokot 1996). Furthermore, various spa therapy techniques have been demonstrated to increase plasma levels of beta-endorphin (Kubota et al. 1992). Interestingly, it has been found that application of mature thermal mud in healthy individuals brings about a rapid increase in plasma beta-endorphin, which returns to pretreatment levels within the period of the so-called thermal reaction (Cozzi et al. 1995).
This increase in beta-endorphin is probably the key factor in the mechanism of individual tolerance to thermal mud-baths.
Recent studies have shown a reduction in circulating levels of prostaglandin E2 (PGE2) and leukotriene B4 (LTB4), important mediators of inflammation and pain, in patients with knee OA undergoing a cycle of balneotherapy or mud-pack therapy (Bellometti and Galzigna 1998; Ardiç et al. 2007). Crenotherapy also affects the synthesis of various cytokines involved in the ongoing chondrolysis and inflammation in OA; in fact, a reduction in the cytokines interleukin (IL)-1β and tumour necrosis factor (TNF)-α and the soluble receptors of the latter has been demonstrated following a cycle of mud-baths therapy (temperature > 41 C°) in patients with knee OA (Cecchettin et al. 1995; Bellometti et al. 2002) (Table 4).
Several studies pointed out a significant role of matrix metalloproteinases (MMPs), particularly MMP-3 or stromelysin-1, produced by activated chondrocytes and other cell types in the cartilage degradation in joint diseases (Malemud et al. 2003). A recent study of Bellometti et al. (2005) showed that MMP-3 serum levels were significantly reduced by mud-bath therapy in patient with OA.
Cycles of mud applications and balneotherapy also cause an increase in some growth factors, such as insulin-like growth factor 1 (IGF1) (Bellometti et al. 1997) which stimulates cartilage anabolism (Trippel 1995). Spa therapy has also been shown to exert positive effects on the oxidant/antioxidant system, resulting in a reduced release of reactive oxygen species (ROS) and nitrogen (RNS) (Braga et al. 2008; Grabski et al. 2004; Eckmekcioglu et al. 2002; Bender et al. 2007).
In a recent study, Fioravanti et al. (2011a, b) assessed the possible modifications of plasma levels of leptin and adiponectin in patients with knee OA treated with a cycle of spa therapy. The data showed, at the end of mud-bath therapy cycle, a slight but not significant increase of plasma leptin concentrations and a significant decrease in serum adiponectin levels. These adipocytokines play an important role in the pathophysiology of OA (Lago et al. 2008). In particular, there is evidence that adiponectin in skeletal joints may have proinflammatory effects and may be involved in cartilage degradation (Gomez et al. 2009). In view of these recent findings, the decrease of adiponectin after spa therapy demonstrated in this study may play a protective role in OA. On the other side, partial contradictory data were observed in a recent pilot study conducted by Shimodozono et al. (2012). The authors reported a significant increase of serum levels of leptin in seven healthy men after a single 10-min warm-water bath (WWB) at 41 °C with tap water or WWB with inorganic salts and carbon dioxide (ISCO2) and remained significantly higher than those at baseline even 30 min after WWB with tap water; serum levels of adiponectin showed a slight, but not significant, increase immediately and 30 min after a single WWB under both conditions. These differences might be due to the heterogeneity of subjects (relatively healthy, young, lean and male in this last study) and to bathing modalities (duration of thermal stimulation and the substances used in the mineral water).
Experimental studies in animal models of arthritis corroborate the evidence of beneficial effects of mud-bath therapy on inflammatory and degenerative joint diseases. Cozzi et al. (2004) have recently demonstrated an anti-inflammatory effect of mud-bath applications in Freund’s adjuvant-induced arthritis in rats. Following the application of crenotherapy, a reduction of oedema in the rat paws (measured by plethysmometry) was accompanied by a significant reduction in the levels of circulating TNF-α and IL-1β. In 2007, Britschka et al. (2007) confirmed the anti-inflammatory and chondroprotective effects of the application of mud in zymosan-induced arthritis in rats, by performing histological analysis on synovial tissues and cartilage taken from the sacrificed animals on day 21 of treatment. In the synovial tissue resulted a reduction of the hyperplasia of the lining, vascularization and cellular infiltration in the group of rats treated with mud applications, in contrast to the group of rats treated with simple heated tap water and the untreated (control) group of rats. At cartilage level, there was a macroscopically visible reduction of the erosive lesions, as well as an increase in chondrocyte density and collagen and proteoglycan content only in the mud-treated animals.
A possible chondroprotective role of mineral water or mineral components was demonstrated by some pilot studies in chondrocyte cultures. Burguera et al. (Burguera et al. 2012) studied the possible activity of hydrogen sulphide (H2S) in human OA chondrocytes stimulated with IL-1β. They analysed the effects of different concentrations of a fast (NaHS) or a slow (GYY4137) release H2S donor on three key aspects of the inflammatory and degenerative process in OA. After incubation with H2S donors, the authors demonstrated a significant reduction of nitric oxide (NO), PGE-2, and ROS levels in culture medium and of inducible nitric oxide synthase (iNOS) gene expression, induced by IL-1β. These data were confirmed by Li et al. (2013) in normal human chondrocytes stimulated by lipopolysaccharide (LPS). GYY4137 decreased LPS-induced production of NO, PGE2, TNF-α and IL-6, reduced the levels and catalytic activity of iNOS and of COX-2 and nuclear factor (NF)-kB activation. Furthermore, GYY4137, in a previous study, showed a potent inhibition on oxidative stress-induced cell death (Fox et al. 2012).
The incubation of human chondrocytes cell line C-28/I2 with another H2S donor, Natrium hydrogen sulphide (NaHS), provided prove that constitutive as well as IL-1 β-induced IL-6 and IL-8 expression was partially and transiently blocked by the NaHS (Kloesch et al. 2012).
Fioravanti et al. (2013) studied the possible chondroprotective role of highly mineralized water, strongly acidic sulphate, rich in calcium, magnesium and iron (Vetriolo’s thermal water (VW)) in human OA chondrocytes cultivated with a with or without IL-1β. For this purpose, OA chondrocytes were cultivated in deionized water (DW) (DW-DMEM, controls), or in one of three different VW-DMEM media, in which DW had been totally (100 %) or in part (50 or 25 %) substituted with VW. The results showed that VW alone at 25 or 50 % concentration did not affect the viability of cultured OA chondrocytes and determined a significant survival recovery rate in cultures stimulated with IL-1β. NO levels were low both in DW-DMEM cultures and in those reconstituted with 25 or 50 % of VW and were significantly increased by IL-1β. VW at 25 or 50 % concentration significantly (P < 0.001) reduced the NO production induced by IL-1β. The data of the NO levels were confirmed by the immunocytochemistry assay for iNOS. Furthermore, the authors confirmed the pro-apoptotic effect of IL-1β and demonstrated a protective effect of VW at 25 or 50 % concentration.
Finally, other factors may contribute positively to the beneficial effects of spa therapy in OA, such as change of environment, the ‘spa-scenery’, the absence of (house) work duties, physical and mental relaxation, the non-competitive atmosphere with similarly suffering companions and physical therapy. As such, spa benefits could perhaps be attributed also to the effects of factors unrelated to the water therapy per se. These spa benefits are especially important in studies evaluating the effects of mud and balneotherapy compared with no treatment or another treatment (Bender et al. 2005; Fioravanti et al. 2011a, b).
Discussion
The aim of this review was to summarize the currently available information on clinical effects and mechanisms of action of spa therapy in the management of knee OA. Although the magnitude of the treatment effect varied across studies, most trials documented improvements after the treatment and in the long term. This consistency supports a therapeutic effect of spa therapy in patients with knee OA. For what concern the different modalities of spa therapy (spa therapy in a broad sense, balneotherapy and mud-pack therapy), we can’t state the superiority of one of these techniques over another one, because there is a lack of studies that compare these different spa approaches.
The results of the RCTs, using various spa modalities for gonarthrosis, suggest a positive effect on pain, functional capacity and QoL (when investigated). The studies aimed to assess the medium- long-term effect found that the clinical efficacy of spa therapy lasts over time, until 6–9 months after the treatment (Fioravanti et al. 2010; Fraioli et al. 2011; Forestier et al. 2010). Spa therapy resulted to be well tolerated and have a lower percentage of side effects, which also are less severe, than those associated with pharmacological treatments.
Some aspects of the studies on spa therapy for knee OA are disputable and could be a source of bias. Comparisons between the various studies are difficult as the baseline characteristics of the patients are heterogeneous, the interventions differ in type, intensity and in length, and in certain studies, the treatment protocol consists in a combination of more modalities (for example spa therapy and exercise). Patients have been assessed at different time points after spa therapy, and the methods used for the assessment of efficacy vary, although the most used are VAS, WOMAC and Lequesne index. It is noteworthy that these criteria, as well as QoL indices, could not correspond to reality, because they rely on a subjective evaluation by the patients, which may be markedly influenced by a placebo effect (Forestier and Françon 2008).
Furthermore, another possible source of bias is the few number of double-blind experimental designs because of the difficulty to create a satisfactory control group. In most studies, the effects of spa therapy are assessed comparatively to findings in patients that stay at home and follow their routine medical care.
Finally, we noted poor studies on cost-effectiveness. At this regard, the data derived from the Italian project ‘Naiade’ are particularly interesting (Fioravanti et al. 2003). This study demonstrated a reduction of the consumption of drugs (NSAIDs and analgesics) and of the number and duration of hospitalization and missed working days for OA, after spa therapy. These results were particularly important, considering the adverse effects frequently induced by NSAIDs and the costs relative to their use associated with a support therapies (such as gastro-protective drugs). Furthermore, the significant reduction of the hospitalization and average hospitalization days could minimize National Health Service costs.
Then, although the data from recent studies are stimulating, it is impossible to ignore the existence of a complex series of problems and uncertainties that prevent spa therapies from gaining the full consensus of the scientific community. One of the critical points is the controversial problem of the absorption of the minerals dissolved in thermal waters, for example, the demonstration of specific effects other than those linked to the simple action of heat. Unfortunately, few studies have been conducted on this topic and little is known about the specific effects of various mineral waters. It is still not clear which elements are essential and what is the ideal concentration of each element in order to attain an optimal response to treatment. It remains to be clarified which mineral waters are most suitable for various diseases and whether the different components exert specific actions.
In conclusion, spa therapy seems to have a role in the treatment of knee OA. It cannot substitute for conventional therapy but can complement to it. The improvement reported in some clinical studies lasts over time. Actually, spa therapy can represent a useful backup to pharmacologic treatment of OA or a valid alternative for patients who do not tolerate pharmacologic treatments. Future researches to clarify the mechanisms of action and the effects deriving from the application of thermal treatments are imperative. Additional RCTs with high methodological quality concerning the effectiveness of spa therapy in knee OA are necessary in order to obtain strong evidence on the effects of spa therapy.
References
Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, Christy W, Cooke TD, Greenwald R, Hochberg M et al (1986) Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum 29:1039–1049
Apolone G, Mosconi P (1998) The Italian SF-36 health survey: translation, validation and norming. J Clin Epidemiol 51:1025–1036
Ardiç F, Ozgen M, Aybek H, Rota S, Cubukçu D, Gökgöz A (2007) Effects of balneotherapy on serum IL-1, PGE2 and LTB4 levels in fibromyalgia patients. Rheumatol Int 27:441–446
Bálint GP, Buchanan WW, Adám A, Ratkó I, Poór L, Bálint PV, Somos E, Tefner I, Bender T (2007) The effect of the thermal mineral water of Nagybaracska on patients with knee joint osteoarthritis—a double blind study. Clin Rheumatol 26:890–894
Bellamy N, Goldsmith CH, Buchanan WW, Campbell J, Duku E (1991) Prior score availability: observations using the WOMAC osteoarthritis index. Br J Rheumatol 30:150–151
Bellometti S, Galzigna L (1998) Serum levels of a prostaglandin and a leukotriene after thermal mud pack therapy. J Investig Med 46:140–145
Bellometti S, Cecchettin M, Galzigna L (1997) Mud pack therapy in osteoarthrosis. Changes in serum levels of chondrocyte markers. Clin Chim Acta 268:101–106
Bellometti S, Galzigna L, Richelmi P, Gregotti C, Bertè F (2002) Both serum receptors of tumor necrosis factor are influenced by mud pack treatment in osteoarthrotic patients. Int J Tissue React 24:57–64
Bellometti S, Richelmi P, Tassoni T, Bertè F (2005) Production of matrix metalloproteinases and their inhibitors in osteoarthritic patients undergoing mud bath therapy. Int J Clin Pharmacol Res 25:77–94
Bender T, Karagülle Z, Bálint GP, Gutenbrunner C, Bálint PV, Sukenik S (2005) Hydrotherapy, balneotherapy, and spa treatment in pain management. Rheumatol Int 25:220–224
Bender T, Bariska J, Vàghy R, Gomez R, Kovàcs I (2007) Effect of balneotherapy on the antioxidant system—a controlled pilot study. Arch Med Res 38:86–89
Braga PC, Sambataro G, Dal Sasso M, Culici M, Alfieri M, Nappi G (2008) Antioxidant effect of sulphurous thermal water on human neutrophil bursts: chemiluminescence evaluation. Respiration 75:193–201
Britschka ZMN, Teodoro WR, Velosa APP, de Mello SB (2007) The effect of Brazilian black mud treatment in chronic experimental arthritis. Rheumatol Int 28:39–45
Burguera EF, Anero AV, Falide RM, Blanco FJ (2012) The effect of hydrogen sulfide donors on inflammatory mediators in human articular osteoarthritic chondrocytes. Arthritis Rheum 64(Suppl 10):S6
Busija L, Bridgett L, Williams SR, Osborne RH, Buchbinder R, March L, Fransen M (2010) Osteoarthritis. Best Pract Res Clin Rheumatol 24:757–768. doi:10.1016/j.berh.2010.11.001
Cantarini L, Leo G, Giannitti C, Cevenini G, Barberini P, Fioravanti A (2007) Therapeutic effect of spa therapy and short wave therapy in knee osteoarthritis: a randomized, single blind, controlled trial. Rheumatol Int 27:523–529
Cecchettin M, Bellometti S, Lalli A, Galzigna L (1995) Serum interleukin 1 changes in arthrosic patients after mud-packs treatment. Phys Rheab Kur Med 5:92–93
Cozzi F, Lazzarin P, Todesco S, Cima L (1995) Hypothalamic-pituitary-adrenal axis dysregulation in healthy subjects undergoing mud-bath applications. Arthritis Rheum 38:724–726
Cozzi F, Carrara M, Sfriso P, Todesco S, Cima L (2004) Anti-inflammatory effect of mud-bath applications on adjuvant arthritis in rats. Clin Exp Rheumatol 22:763–766
Eckmekcioglu C, Strauss-Blasche G, Holzer F, Marktl W (2002) Effect of sulfur baths on antioxidative defense systems, peroxide concentrations and lipid levels in patients with degenerative osteoarthritis. Forsch Komplementarmed Klass Naturheilkd 9:216–220
Espejo-Antúnez L, Cardero-Durán MA, Garrido-Ardila EM, Torres-Piles S, Caro-Puértolas B (2013) Clinical effectiveness of mud pack therapy in knee osteoarthritis. Rheumatology (Oxford) 52:659–668. doi:10.1093/rheumatology/kes322
EuroQol Group (1990) EuroQol—a new facility for the measurement of health-related quality of life. Health Policy 16:199–208
Evcik D, Kavuncu V, Yeter A, Yigit I (2007) The efficacy of balneotherapy and mud-pack therapy in patients with knee osteoarthritis. Joint Bone Spine 74:60–65
Fautrel B, Hilliquin P, Rozenberg S, Allaert FA, Coste P, Leclerc A, Rossignol M (2005) Impact of osteoarthritis: results of a nationwide survey of 10,000 patients consulting for OA. Joint Bone Spine 72:235–240
Fioravanti A, Valenti M, Altobelli E, Di Orio F, Nappi G, Crisanti A, Cantarini L, Marcolongo R (2003) Clinical efficacy and cost-effectiveness evidence of spa therapy in osteoarthritis. The results of “Naiade” Italian Project. Panminerva Med 45:211–217
Fioravanti A, Iacoponi F, Bellisai B, Cantarini L, Galeazzi M (2010) Short- and long-term effects of spa therapy in knee osteoarthritis. Am J Phys Med Rehabil 89:125–132. doi:10.1097/PHM.0b013e3181c1eb81
Fioravanti A, Cantarini L, Bacarelli MR, de Lalla A, Ceccatelli L, Blardi P (2011a) Effects of spa therapy on serum leptin and adiponectin levels in patients with knee osteoarthritis. Rheumatol Int 31:879–882. doi:10.1007/s00296-010-1401-x
Fioravanti A, Cantarini L, Guidelli GM, Galeazzi M (2011b) Mechanisms of action of spa therapies in rheumatic diseases: what scientific evidence is there? Rheumatol Int 31:1–8. doi:10.1007/s00296-010-1628-6
Fioravanti A, Giannitti C, Bellisai B, Iacoponi F, Galeazzi M (2012) Efficacy of balneotherapy on pain, function and quality of life in patients with osteoarthritis of the knee. Int J Biometeorol 56:583–590. doi:10.1007/s00484-011-0447-0
Fioravanti A, Lamboglia A, Pascarelli NA, Cheleschi S, Manica P, Galeazzi M, Collodel G (2013) Thermal water of Vetriolo, Trentino, inhibits the negative effect of interleukin 1β on nitric oxide production and apoptosis in human osteoarthritic chondrocytes. J Biol Regul Homeost Agents 27:891–902
Forestier R, Françon A (2008) Crenobalneotherapy for limb osteoarthritis: systematic literature review and methodological analysis. Joint Bone Spine 75:138–148. doi:10.1016/j.jbspin.2007.06.009]
Forestier R, Desfour H, Tessier JM, Françon A, Foote AM, Genty C, Rolland C, Roques CF, Bosson JL (2010) Spa therapy in the treatment of knee osteoarthritis: a large randomised multicentre trial. Ann Rheum Dis 69:660–665. doi:10.1136/ard.2009.113209
Fox B, Schantz JT, Haigh R, Wood ME, Moore PK, Viner N, Spencer JP, Winyard PG, Whiteman M (2012) Inducible hydrogen sulfide synthesis in chondrocytes and mesenchymal progenitor cells: is H2S a novel cytoprotective mediator in the inflamed joint? J Cell Mol Med 16:896–910. doi:10.1111/j.1582-4934.2011.01357.x
Fraioli A, Serio A, Mennuni G, Ceccarelli F, Petraccia L, Fontana M, Grassi M, Valesini G (2011) A study on the efficacy of treatment with mud packs and baths with Sillene mineral water (Chianciano Spa Italy) in patients suffering from knee osteoarthritis. Rheumatol Int 31:1333–1340. doi:10.1007/s00296-010-1475-5
Gomez R, Lago F, Gomez-Reino J, Dieguez C, Gualillo O (2009) Adipokines in the skeleton: influence on cartilage function and joint degenerative diseases. J Mol Endocrinol 43:11–18. doi:10.1677/JME-08-0131
Grabski M, Wozakowska-Kaplon B, Kedziora J (2004) Hydrogen sulphide water balneum effect on erythrocyte superoxide dismutase activity in patients with rheumatoid arthritis-in vitro study. Przegl Lek 61:1405–1409
Guidelli GM, Tenti S, De Nobili E, Fioravanti A (2012) Fibromyalgia syndrome and spa therapy: myth or reality? Clin Med Insights Arthritis Musculoskelet Disord 5:19–26. doi:10.4137/CMAMD.S8797
Harzy T, Ghani N, Akasbi N, Bono W, Nejjari C (2009) Short- and long-term therapeutic effects of thermal mineral waters in knee osteoarthritis: a systematic review of randomized controlled trials. Clin Rheumatol 28:501–507. doi:10.1007/s10067-009-1114-2
Jordan KM, Arden NK, Doherty M, Bannwarth B, Bijlsma JW, Dieppe P, Gunther K, Hauselmann H, Herrero-Beaumont G, Kaklamanis P, Lohmander S, Leeb B, Lequesne M, Mazieres B, Martin-Mola E, Pavelka K, Pendleton A, Punzi L, Serni U, Swoboda B, Verbruggen G, Zimmerman-Gorska I, Dougados M (2003) Standing Committee for International Clinical Studies Including Therapeutic Trials ESCISIT. EULAR Recommendations 2003: an evidence based approach to the management of knee osteoarthritis: Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis 62:1145–1155
Karagülle M, Karagülle MZ, Karagülle O, Dönmez A, Turan M (2007) A 10-day course of SPA therapy is beneficial for people with severe knee osteoarthritis. A 24-week randomised, controlled pilot study. Clin Rheumatol 26:2063–2071
Kloesch B, Liszt M, Steiner G, Brӧll J (2012) Inhibitors of p38 and ERK1/2 MAPkinase and hydrogen sulphide block constitutive and IL-1β-induced IL-6 amd IL-8 expression in the human chondrocyte cell line C-28/I2. Rheumatol Int 32:729–736. doi:10.1007/s00296-010-1682-0
Kubota K, Kurabayashi H, Tamura K, Kawada E, Tamura J, Shirakura T (1992) A transient rise in plasma beta-endorphin after a traditional 47 degrees C hot-spring bath in Kusatsu-spa, Japan. Life Sci 51:1877–1880
Kücükdeveci AA, McKenna SP, Kutlay S, Gürsel Y, Whalley D, Arasil T (2000) The development and psychometric assessment of the Turkish version of the Nottingham Health Profile. Int J Rehabil Res 23:31–38
Kuczera M, Kokot F (1996) Effect of spa therapy on the endocrine system. I. Stress reaction hormones. Pol Arch Med Wewn 95:11–20
Lago R, Gomez R, Otero M, Lago F, Gallego R, Dieguez C, Gomez-Reino JJ, Gualillo O (2008) A new player in cartilage homeostasis: adiponectin induces nitric oxide synthase type II and pro-inflammatory cytokines in chondrocytes. Osteoarthritis Cartil 16:1101–1109. doi:10.1016/j.joca.2007.12.008
Lequesne MG, Mery C, Samson M, Gerard P (1987) Indexes of severity for osteoarthritis of the hip and knee. Validation—value in comparison with other assessment tests. Scand J Rheumatol Suppl 65:85–89
Li L, Fox B, Keeble J, Salto-Tellez M, Winyard PG, Wood ME, Moore PK, Whiteman M (2013) The complex effects of the slow-releasing hydrogen sulfide donor GYY4137 in a model of acute joint inflammation and in human cartilage cells. J Cell Mol Med 17:365–376. doi:10.1111/jcmm.12016
Malemud CJ, Islam N, Haqqi TM (2003) Pathophysiological mechanisms in osteoarthritis lead to novel therapeutic strategies. Cells Tissues Organs 174:34–48
McDowell IW, Martini CJ, Waugh W (1978) A method for self-assessment of disability before and after hip replacement operation. Br Med J 2:857–859
Meenan RF, Gertman PM, Mason JH (1980) Measuring health status in arthritis. The arthritis impact measurement scales. Arthritis Rheum 23:146–152
Melzack R, Wall PD (1965) Pain mechanisms: a new theory. Science 150:971–979
Odabasi E, Turan M, Erdem H, Tekbas F (2008) Does mud pack treatment have any chemical effect? A randomized controlled clinical study. J Altern Complement Med 14:559–565. doi:10.1089/acm.2008.0003
Salaffi F, Cavalieri F, Nolli M, Ferraccioli G (1991) Analysis of disability in knee osteoarthritis. Relationship with age and psychological variables but not with radiographic score. J Rheumatol 18:1581–1586
Salaffi F, Leardini G, Canesi B, Mannoni A, Fioravanti A, Caporali R, Lapadula G, Punzi L (2003) GOnorthrosis and Quality Of Life Assessment (GOQOLA). Reliability and validity of the Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index in Italian patients with osteoarthritis of the knee. Osteoarthritis Cartilage 11:551–560
Sarsan A, Akkaya N, Ozgen M, Yildiz N, Atalay NS, Ardic F (2012) Comparing the efficacy of mature mud pack and hot pack treatments for knee osteoarthritis. J Back Musculoskelet Rehabil 25:193–199. doi:10.3233/BMR-2012-0327
Sherman G, Zeller L, Avriel A, Friger M, Harari M, Sukenik S (2009) Intermittent balneotherapy at the Dead Sea area for patients with knee osteoarthritis. Isr Med Assoc J 11:88–93
Shimodozono M, Matsumoto S, Ninomiya K, Miyata R, Ogata A, Etoh S, Watanabe S, Kawahira K (2012) Acute effects of a single warm-water bath on serum adiponectin and leptin levels in healthy men: a pilot study. Int J Biometeorol 56:933–939. doi:10.1007/s00484-011-0502-x
Sukenik S, Flusser D, Abu-Shakra M (1999) The role of spa therapy in various rheumatic diseases. Rheum Dis Clin N Am 25:883–897
Tefner IK, Gaál R, Koroknai A, Ráthonyi A, Gáti T, Monduk P, Kiss E, Kovács C, Bálint G, Bender T (2013) The effect of Neydharting mud-pack therapy on knee osteoarthritis: a randomized, controlled, double-blind follow-up pilot study. Rheumatol Int 33:2569–2576. doi:10.1007/s00296-013-2776-2
Tishler M, Rosenberg O, Levy O, Elias I, Amit-Vazina M (2004) The effect of balneotherapy on osteoarthritis. Is an intermittent regimen effective? Eur J Intern Med 15:93–96
Trippel SB (1995) Growth factor actions on articular cartilage. J Rheumatol Suppl 43:129–132
Verhagen AP, Bierma-Zeinstra SM, Boers M, Cardoso JR, Lambeck J, de Bie RA, de Vet HC (2007) Balneotherapy for osteoarthritis. Cochrane Database Syst Rev 4, CD006864
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Woolf AD, Pfleger B (2003) Burden of major musculoskeletal conditions. Bull World Health Organ 81:646–656
Yurtkuran M, Yurtkuran M, Alp A, Nasircilar A, Bingöl U, Altan L, Sarpdere G (2006) Balneotherapy and tap water therapy in the treatment of knee osteoarthritis. Rheumatol Int 27:19–27
Acknowledgments
The authors affirm that there are no undeclared contributors, funding sources or study sponsors.
Conflict of interest
All authors declare that there is no conflict of interests regarding the publication of this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tenti, S., Cheleschi, S., Galeazzi, M. et al. Spa therapy: can be a valid option for treating knee osteoarthritis?. Int J Biometeorol 59, 1133–1143 (2015). https://doi.org/10.1007/s00484-014-0913-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-014-0913-6