Abstract
The purpose of this study was to investigate the clinical effects of balneotherapy in the treatment of Fibromyalgia Syndrome (FMS) and to determine if balneotherapy influences serum levels of inflammation markers, IL-1, PGE2 and LTB4. 24 primary fibromyalgia female patients diagnosed according to American College of Rheumatology criteria were included to the study. Their ages ranged between 33 and 55 years. FMS patients were randomly assigned in two groups as, group 1 (n = 12) and group 2 (n = 12). Group 1 received 20-min bathing, once in a day for five days per week. Patients participated in the study for 3 weeks (total of 15 sessions) in Denizli. Group 2 did not receive balneotherapy. FMS patients were evaluated by tenderness measurements (tender point count and algometry), Visual Analogue Scale, Beck’s Depression Index, Fibromyalgia Impact Questionnaire. Ten healthy women recruited group three as the controls. Serum PGE2, LTB4 and IL1-α levels were measured in all three groups. The biochemical measurements and clinical assessments were performed before and at the end of general period of therapy. Statistically significant alterations in algometric score, Visual Analogue score, Beck’s Depression Index and PGE2 levels (P < 0.001), numbers of tender points (P < 0.01) and Fibromyalgia Impact Questionnaire score (P < 0.05) were found after the balneotherapy between group 1 and 2. Mean PGE2 level of FMS patients were higher compared to healthy control group (P < 0.0001) and decreased after the treatment period, only in group 1 (P < 0.05). As in the group 2 and 3, detectable IL-1 and LTB4 measurements were insufficient, statistical analysis was performed, only in group 1. After balneotherapy IL-1 and LTB4 significantly decreased in group 1 (P < 0.05). In conclusion, balneotherapy is an effective choice of treatment in patients with FMS relieving the clinical symptoms, and possibly influencing the inflammatory mediators.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fibromyalgia syndrome (FMS) is an idiopathic, common and complex syndrome, defined as long lasting, widespread and symmetrical non-articular musculoskeletal pain with generalized tender points at specific anatomical sites [1]. Fatique, sleep disturbance, anxiety, irritable bowel syndrome, headache, or paresthesia, are the other common symptoms. The pathogenesis and etiology of FMS still remains unclear. The current therapy strategies aimed to reduce the pain and other associated symptoms. Several treatment modalities including pharmacologic therapy (nonsteroidal anti-inflammatory drugs, adjuvant analgesic drugs, tricyclic antidepressants and selective serotonin reuptake inhibitors), psychological interventions, physical therapy, and exercise programs have been used [2]. The application of highly variable types of treatments leads to propose different pathogenesis in FMS. Recent findings suggest that at least a subset of FMS patients (up to 30%) could suffer from an inflammatory process mediated by cytokines, proteases and inflammation mediators [3].
Balneotherapy, also known spa therapy, medical hydrology or thermal therapy is a very popular complementary therapy in many European and Middle East countries used in the treatment of different kinds of rheumatic disorders [4]. Denizli where the study was carried on is one of the thermal spa centers in Turkey. The anti-inflammatory effect of balneotherapy is measurable in terms of biochemical parameters in the serum of treated patients. It was demonstrated that in arthrosis, which is an inflammatory process, mudpack treatment could reduce serum IL-1 levels [5, 6]. It was reported that the reduction in prostaglandin E2 (PGE2) and leukotriene (LTB4) which are potent inflammatory compounds that provoke pain could be achieved by mudpack therapy [7].
Although there are a number of spa studies in FMS [8–12], none of them used biochemical assessment. The aim of this study was to evaluate the clinical effect of balneotherapy and the influence on release of inflammatory mediators IL-1α(IL-1), PGE2 and LTB4 in FMS patients.
Materials and methods
Patients
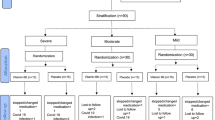
Twenty-four female patients with FMS were recruited from the Outpatient Clinic of Department of Physical Medicine and Rehabilitation, Pamukkale University Hospital, Denizli, Turkey. All the patients were diagnosed on the basis of the 1990 American College of Rheumatology criteria for the classification of FMS [13] and had no other accompanying disease. Patients with contraindication to any form of balneotherapy like peripheral vascular disease, cardiovascular disease or central nervous system disease or who had balneotherapy in the last 12 months were not included to the study. The FMS patients were randomly assigned into two groups as group 1 with balneotherapy and group 2 without balneotherapy before the clinical evaluation was performed. After randomisation, three patients in group 2, were withdrawn from the study because of their social problems and illness during the study. Twenty-one patients completed the study (12 patients with balneotherapy, nine patients without balneotherapy). The patients without balneotherapy were assured that they would have the treatment after completing this study. The control group (group 3) consisted of ten, age-matched healthy women, without symptoms of FMS. Written informed consent was taken from all of the subjects.
Analysis of thermal water
Two bottles of samples were taken from thermal water in Richmond Spa resort and stored in 500 ml polyethylene bottles. One of the bottles was acidified with HCl (pH < 2) for determination of cations and the other was cooled to +4°C or lower and kept unacidified for anion analyses. pH, Eh and temperature values were measured in the field using HACH Sension2 pH meter at the time of sampling. The EC (specific electrical conductivity) was determined in situ, using HACH Sension5 conductivity meter. Alkalinity (HCO3) and free CO2 analyses were performed volumetrically by titration with HCl and NaOH, respectively. Water samples were analyzed with standard methods described by APHA (The American Public Health Association) [14] in 1–7 h, after sampling. Na+, K+, Ca++ and were determined by UNICAM atomic absorption spectrometer. Sulfate, Cl−, F− and dissolved O2 analyses were carried out by HACH DR/4000 VIS Spectrophotometer.
Treatment program
Group 1 (n = 12) received bathing for 20 min a day, for 5 days per week. Patients participated to the balneotherapy program for 3 weeks (for a total of 15 sessions) in the Richmond Pamukkale Thermal and Spa Resort, Denizli. Thermal pool water heat was 36°C. As the therapy center was close to the city centre the patients were transported to thermal resort. The rest of the time, the patients continued their daily activities. The subjects in group 2 (n = 9) were also told to continue their daily activities. Regular exercise or walking programs were not offered to any of the patients. Analgesics, non-steroidal antiinflammatory drugs or additional medication as antidepressive drug usage was not permitted during this period.
Assessment parameters
All the patients were evaluated by visual analogue scale (VAS) and tenderness measurements (tender point count and algometry) for disease severity, Fibromyalgia impact questionnaire (FIQ) for functional capacity, Beck’s depression index (BDI) for depression. Serum PGE2, LTB4 and IL1-α levels were also measured. The biochemical measurements and clinical assesments were performed before and at the end of general period of therapy
Disease severity
*Pain intensity: a 10-cm VAS was used for the evaluation of pain intensity (0 indicates no pain whereas 10 is the worst).
*Tenderness measurements: The number of tender points was obtained by applying 4 kg/cm2 of pressure on 18 different points described in the ACR criteria [15]. The algometer score was then calculated by standard pressure algometer (Algometer Commender TM, Jtech. Med.) as the sum of the minimum pain-generating pressure values was obtained from 18 points [16].
Functional assessment
Functional capacity in daily living activities was evaluated by the Turkish version of FIQ, which is valid and reliable [17]. FIQ is a ten-item, self-administered instrument, measuring physical functioning, work status, depression, anxiety, pain, fatigue, sleep, depression, stiffness, and well-being [18]. Each item is standardized on a scale ranging from 0 to 10, with 10 indicating greater impairment. Higher total value (maximum 100) indicates severe effects on daily activities.
Psychological assessment
BDI used to assess the mood of the subjects with FMS, is a 21-item self-report rating inventory, measuring the symptoms and characteristic attitudes of depression [19]. A higher score indicates more depressed mood.
Biochemical analyses
Full blood count, erythrocyte sedimentation rate (ESR), serum C-reactive protein (CRP), rheumatoid factor (RF), IL-1, LTB4 and PGE2 levels were measured. Blood samples were taken before and at the end of general period of therapy. Venous blood samples were drawn from the participants after a fasting of 12 h. Samples were collected in serum separator tubes, allowed to clot for 30 min, centrifuged at room temperature for 15 min at 2,000 × g. The samples were stored at −70°C until analyzed. The biochemical measurements were done, by using commercial kits. IL1-α, (BioSource International, Inc. Camarillo, CA, USA), LTB4 and PGE2 (Assay Designs Inc., MI, USA) levels were measured by ELISA, according to the manufacturers’ methods with a sensitivity of 1 pg/ml, 5.63 pg/ml and 13.4 pg/ml for IL1-α, LTB4 and PGE2, respectively.
Statistical analysis
SPSS 12.0 was used for statistical analysis. Mann–Whitney U test and Wilcoxon matched paired tests were applied, inter- and intragroup analysis as appropiate, to compare results. Spearman ranked correlation test was used to correlate VAS and serum PGE2 levels. The alterations in the measurements were analyzed by using repeated measures test. Because a large proportion of serum IL-1 ve LTB4 values were undetectable in group 2 and group 3, cytokines were described as either detectable (pg/ml) or undetectable. P value of less than 0.05 was accepted as being statistically significant.
Results
The results of the thermal water field analysis were given in Table 1.
Demographic and clinical characteristics of the patients were given in Table 2. Age, durations of symptoms, baseline VAS scores, and serum PGE2 levels were similar in group 1 and 2 (P > 0.05).
Results obtained from assesment parameters before and after the treatment program were listed in Table 3. The alterations in pain intensity, TP count, algometric score, BDI, FIQ and serum PGE2 levels were significantly different between group 1 and 2 in favor of group 1 at the end of the treatment period (Table 3).
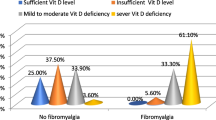
PGE2 levels were detectable in all of the samples. The mean serum PGE2 level of 21 FM patients (86.29 ± 21.68 pg/ml) was significantly higher compared to the healthy control group (42.95 ± 8.81 pg/ml, P < 0.0001). While the mean serum PGE2 level after balneotherapy was significantly lower than the serum PGE2 level before balneotherapy, the same decrease in the second measurement was not observed in group 2 (P < 0.001). In FM patients the change in VAS did not correlate with the change in PGE2 (r = 0.48; P > 0.05).
RF levels were negative in all FMS patients. The ESR in the FMS patients varied between 7 and 30 mm/h. CRP was more than 5 mg/l in two patients with fibromyalgia (10and 15 mg/l, respectively).
In groups 1 and 2, 61.9% of the measurements for both IL-1 and LTB4 were undetectable. In group 1, LTB4 and IL-1 measurements five each, were detectable both before and after balneotherapy, (min–max 1.9–25.9 and 4.7–135 pg/ml, respectively). In group 2, LTB4 and IL-1 measurements, three each, were detectable both before and after balneotherapy (min–max 11.9–25 and 1.3–21 pg/ml, respectively). In healthy control group, IL-1 (n = 3) and LTB4 (n = 2) measurements were 70 and 80% undetectable, respectively, LTB4 was detectable only in two measurements and IL-1 was detectable only in three measurements (min-max 11.3–15 and 1.2–20 pg/ml, respectively ).
As in group 2 and 3, detectable IL-1 and LTB4 measurements were insufficient, statistical analysis was performed only in group 1. In group 1, IL-1 and LTB4, significantly decreased after balneotherapy (P < 0.05) (Table 4).
Discussion
In the historical background of balneotherapy, a great number of patients were treated with thermal therapy and the effects of this treatment in various types of diseases resulted in an increased interest on this topic. Prospective, controlled and randomized studies done in recent years, regarding with the effectiveness of thermal therapy, especially on rheumatic diseases revealed reliable scientific data on this subject [20–22].
FMS has significant impact on a patient’s quality of life and physical functioning. The goals of the treatment in patients with FMS are the relief of pain, which is the main symptom, and increasing the level of functional capabilities. The improvement in clinical symptoms is the expected benefits of spa therapy.
In our study, all clinical parameters were significantly improved in group 1 after balneotherapy. After the treatment period, alterations in pain intensity, TP count, algometric score, BDI, and FIQ were significantly different between group 1 and group 2. Though improvement in BDI, FIQ, pain and number of tender points in FMS patients was detected by various studies, the duration of the balneotherapy benefit differs [8–11]. The clinical findings of our study are consistent with the results of these studies. While the follow-up periods were longer, biochemical evaluation was not included to these studies.
It was suggested that, in up to one third of FMS patients, inflammatory process mediated by cytokines, proteases and inflammatory mediators located in soft body tissues might play role in the pathogenesis of FMS. As a result of this inflammatory process, subcutaneous nociceptors would be stimulated, resulting with the sensation of pain [3]. The detection of IL-1, IL-6, and TNF-α in skin of one-third of FMS patients and measurement of elevated plasma PGE2 levels of fibromyalgia patients supports this hypothesis [23, 24]. The presence of inflammatory foci might be an explanation of the response to nonsteroidal anti-inflammatory drug therapy in a subset of FMS patients [23]. In a study of Kashipaz et al. [25] investigating the production of inflammatory (IL-1α, IL-6, and TNF-α) and anti-inflammatory (IL-10) cytokines in the pathogenesis of chronic fatigue syndrome (CFS) and FMS, it was proposed that dysregulation of cytokine production was not a dominant factor in the pathogenesis of CFS/FMS.
Highly active compounds prostaglandings, produced from arachidonic acid, acts on smooth muscle and can induce inflammatory pain. Hyperalgesia is a prominent feature of the inflammatory response, which is in part mediated by humaral factors such as PGE2 [7]. PGE2 acts by sensitizing afferent nociceptors and inducing release of substance P that influences inflammatory response and long-lasting hyperalgesia [26]. Leukotriens derived from lipooxygenase pathways also participate in inflammatory process [7]. IL-1 is the main mediator of inflammatory process by acting on the nervous system and other various tissues.
Magnusson-Hedenberg et al. [27], demonstrated a relationship among serum PGE2 levels and muscular pain in patients with fibromyalgia. They concluded that, masseter muscle pain seems to be partly of peripheral inflammatory origin in fibromyalgia. In another study of the same authors, it was shown that reduction in masseter PGE2 level after intramuscular glucocorticoid administration was associated with a decrease in resting pain in patients with fibromyalgia [28]. In their study while they did not detect any difference in plasma PGE2 levels before and after the therapy, we demonstrated a significant decrease after balneotherapy. Reduction in serum PGE2 levels could be the reflection of pain relief. Though both pain relief and reduced PGE2 level were detected after the balneotherapy, we couldn’t find any significant correlation among them. We can conclude that, decrease in serum PGE2 levels might be a reflection of anti-inflammatory effect of balneotherapy. It was also suggested that, lower plasma mediator levels compared to the muscle tissue levels might be an indicator of local PGE2 and LTB4 production [28]. This might be one of the possibilities in high rate of undetectable serum measurements in our study. In our study, although there were a few detectable LTB4 measurements before the treatment, LTB4 levels significantly decreased after balneotherapy. In contrast to our findings, in the same study an increased plasma LTB4 levels after glucocorticoid administration was detected [28]. In our study, some patients with pain in combination with undetectable IL-1 and LTB4 levels, suggests the other possible involved mechanism in FMS.
Bellometti et al. [7] showed that mudpack therapy could reduce serum PGE2 and LTB4 levels of patients with osteoarthritis. It was demonstrated that in osteoarthritis mudpack application resulted with a decrease in serum IL-1 levels and they suggested this was related to the presence of an anti-inflammatory mature thermal mud [5, 6]. The strong side of our study compared to these studies, is having a control group. The inhibitory effect of sulfurous thermal water on the production and/or release of cytokines especially IL-1 and gamma-interferon in immune diseases, was also demonstrated in an in vitro study [29]. To our knowledge this is the first results of a spa study investigating the effects of balneotherapy on cytokines in FMS patients.
In conclusion, balneotherapy is an effective choice of treatment in patients with FMS by relieving the clinical symptoms, and possibly influencing the inflammatory mediators. Larger patient groups and longer observation periods are warranted to determine the reproducibility of our results.
References
Inanici F, Yunus MB (2004) History of fibromyalgia: past to present. Curr Pain Headache Rep 8 (5):369–378
Sprott H (2003) What can rehabilitation interventions achieve in patients with primary fibromyalgia? Review. Curr Opin Rheumatol 15(2):145–50
Blanco LE, de Serres FJ, Fernandez-Bustillo E, Kassam DA, Arbesu D, Rodriguez C, Torre JC (2005) alpha1-Antitrypsin and fibromyalgia: new data in favour of the inflammatory hypothesis of fibromyalgia. Med Hypotheses 64(4):759–69
Sukenik S et al (1999) The role of spa therapy in various rheumatic diseases. Rheumatic Diseases Clinics of North America 25 (4):884
Cechettin M, Bellometti S, Lalli A, Galzigna L (1995) Serum interleukin-1 changes in arthrosis patients after mud-pack treatment. Phys Rehab Kur Med 5:92–93
Bellometti S, Giannini S, Sartori L, Crepaldi G (1997) Cytokine levels in osteoarthrosis patients undergoing mud bath therapy. Int J Clin Pharmacol Res 17(4):149–53
Bellometti S., Galzigna L (1998) Serum levels of a prostaglandin and a leukotriene after thermal mud pack therapy. Journal of Investigative Medicine 46:140–145
Altan L, Bingöl Ü, Aykaç M, Koç Z, Yurtkuran M (2003) Investigation of the effects of pool-based exercise on fibromyalgia syndrome. Rheumatol Int 24:272–277
Buskila D, Abu-Shakra M, Neumann L et al (2001) Balneotherapy for fibromyalgia at the Dead Sea. Rheumatol Int 20:105–108
Evcik D, Kizilay B, Gokcen E (2002) The effects of balneotherapy on fibromyalgia patients. Rheumatol Int 22:56–59
Donmez A, Karagulle MZ, Tercan N, Dinler M, Issever H, Karagulle M, Turan M (2005) SPA therapy in fibromyalgia: a randomised controlled clinic study. Rheumatol Int 26(2):168–72
Zijlstra TR, van de Laar MA, Bernelot Moens HJ, Taal E, Zakraoui L, Rasker JJ (2005) Spa treatment for primary fibromyalgia syndrome: a combination of thalassotherapy, exercise and patient education improves symptoms and quality of life. Rheumatology (Oxford) 44(4):539–46
Wolfe F, Smythe HA, Yunus MB et al (1990) The American Collage of Rheumatology 1990 criteria for the classification of fibromyalgia. Arthritis Rheum 33:160–72
APHA (1989) Standard methods for the examination of water and wastewater, 19th edn. American Public Health Association, Washington
Fisher AA (1986) Pressure threshold meter: its use for quantification of tender spots. Arch Phys Med Rehabil 67:836–838
Hewett JE, Buckelew SP, Johnson JC, Shaw SE, Huyser B, Fu YZ (1995) Selection of measures suitable for evaluating change in fibromyalgia clinical trials. J Rheumatol 22:953–958
Sarmer S, Ergin S, Yavuzer G (2000) The validity and reliability of the Turkish version of the Fibromyalgia impact questionnaire. Rheumatol Int 20:9–12
Burckhardt CS, Clark SR, Bennet RM (1991) The Fibromyalgia impact questionnaire: development and validation. J Rheumatol 18:728–733
Beck AT, Rush AJ, Shaw BF, Emergy G (1979) Cognitive therapy of depression. Guildford, New York
Yurtkuran M, Ay A, Karakoc Y (2005)Improvement of the clinical outcome in Ankylosing spondylitis by balneotherapy. Joint Bone Spine. 72(4):303–8
Forestier R (2000) Magnitude and duration of the effects of two spa therapy courses on knee and hip osteoarthritis: an open prospective study in 51 consecutive patients. Joint Bone Spine 67:296–304
Yilmaz B, Goktepe AS, Alaca R, Mohur H, Kayar AH (2004) Comparison of a generic and a disease specific quality of life scale to assess a comprehensive spa therapy program for knee osteoarthritis. Joint Bone Spine 71(6):563–6
Salemi S, Rethage J, Wollina U, Michel BA, Gay RE, Gay S, Sprott H. (2003) Detection of interleukin 1beta (IL-1beta), IL-6, and tumor necrosis factor-alpha in skin of patients with fibromyalgia. J Rheumatol 30(1):146–50
Hamaty D, Valentine JL, Howard R, Howard CW, Wakefield V, Patten MS (1989) The plasma endorphin, prostaglandin and catecholamine profile of patients with fibrositis treated with cyclobenzaprine and placebo: a 5-month study. J Rheumatol Suppl 19:164–8
Amel Kashipaz MR, Swinden D, Todd I, Powell RJ 2003) Normal production of inflammatory cytokines in chronic fatigue and fibromyalgia syndromes determined by intracellular cytokine staining in short-term cultured blood mononuclear cells. Clin Exp Immunol 132(2):360–5
White DM (1996) mechanism of prostaglandin E2-induced substance P release from cultured sensory neurons. Neuroscience 70:561–65
Hedenberg-Magnusson B, Ernberg M, Alstergren P, Kopp S (2001) Pain mediation by prostaglandin E2 and leukotriene B4 in the human masseter muscle. Acta Odontol Scand. 59(6):348–55
Hedenberg-Magnusson B, Ernberg M, Alstergren P, Kopp S. (2002) Effect on prostaglandin E2 and leukotriene B4 levels by local administration of glucocorticoid in human masseter muscle myalgia. Acta Odontol Scand 60(1):29–36
Valitutti S et al (1990) Effects of sulphurus “thermal” water on T lymphocyte proliferative response. Ann Allergy 65:463–468
Acknowledgments
The authors acknowledge the financial support of Pamukkale University Research Fund (Project number: 2002MHF001). We would like to thank the managers of the Richmond SPA Resort.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ardıç, F., Özgen, M., Aybek, H. et al. Effects of balneotherapy on serum IL-1, PGE2 and LTB4 levels in fibromyalgia patients. Rheumatol Int 27, 441–446 (2007). https://doi.org/10.1007/s00296-006-0237-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-006-0237-x