Abstract
Mud-bath therapy plays a primary role in the treatment and prevention of osteoarthritis that has been recognised since antiquity. Numerous studies have demonstrated its clinical benefits and its effects on inflammatory mediators (interleukins), the immune system, cenesthesic factors (endorphins), and the diencephalic–pituitary–adrenal axis. This study was conducted to assess the efficacy of mud-bath therapy with mineral water from the Sillene Spring at Italy’s Chianciano Spa in patients with osteoarthritis of the knee. Patients (n = 61) were divided into two groups. Group A underwent three cycles of mud-based spa therapy over a year’s time, whereas group B did not. Clinical conditions, visual analogue scale pain ratings, and Lequesne indexes of the two groups were compared. We also compared these same parameters in the patients of the two groups that were following the therapy with drugs and in the patients of the group A before and after spa treatment. The percentage of patients with no symptoms or mild symptoms was higher in group A than in group B. Within group A, this percentage was higher after treatment than before spa therapy. Even in the comparison between the patients of the two groups that were following the therapy with drug, the results was that in group A the percentage of patients with no symptoms or mild symptoms was higher than in group B. Statistical analyses based on various tests revealed that almost all these differences were highly significant. No adverse effects were observed in any of the patients in group A. In conclusion, the mud-bath therapy performed at Chianciano Spa with Sillene Spring water remarkably improved the clinical conditions of patients with knee arthritis and significantly reduces the frequency and severity of symptoms and the disability they cause.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spa medicine is a branch of medicine that provides natural forms of treatment (baths, mud packs, mineral waters, caves) for a well-defined set of diseases. The therapeutic efficacy of these approaches has been demonstrated in scientific studies. A number of these studies have investigated aspects of mud-based spa therapies (general and local effects, efficacy, mechanisms of action) in patients with osteoarthritis (OA) [1–15]. These treatments have been shown to modify plasma levels of inflammatory and immune mediators, such as IL-1, IL-6, PGE2, LTB4, TNFα, and to activate the diencephalic–pituitary–adrenal axis, causing increased production of ACTH and adrenocortical hormones and endogenous opioids (cortisol, β-endorphin, insulin-like growth factor I). Increases in blood flow induced at the application site by the heat of the mud-pack might promote local clearance of inflammatory mediators and pain-producing substances. These changes explain the analgesic and antiinflammatory effects and the improved mobility observed in patients with arthritis who have had mud-based therapy [16–23]. Mud treatments also increase serum levels of GSH peroxidase, which is the cell’s main defense against free-radical-induced toxicity [24–26]. Some authors have reported that a single cycle of standard mud-based therapy has positive effects at the systemic level, as reflected by chondrocyte markers, and these findings support the hypothesis that mud-based therapy produces protective effects on the articular cartilage [27]. Mud treatments have also been shown to activate osteoblasts without suppressing osteoclast activity, which suggests that this approach can be used (or in any case is not contraindicated) in patients suffering from osteoporosis [28, 29].
At Chianciano Spa in Italy, patients with OA are treated with mud packs prepared with water from the Sillene Spring and baths in the same water. The Sillene Spring is located 505 m above sea level, and its water is characterised by high sulphate, bicarbonate, calcium, and magnesium contents, a source temperature of 38.5°C, and a fixed residue of 2.956 g/L at 180°C. The mud used consisted of a solid argillaceous component, predominantly inorganic, which had “matured” for 6 months in mineral water from the Sillene Spring. The water contains bicarbonate (816 mg/L) and sulphate anions (1.648 g/L) and magnesium (150 mg/L) and calcium cations (680 mg/L). After the 6-month maturation period, the physical and chemical properties of the mud are stable.
Objectives
This study was conducted to evaluate the efficacy of the mud-bath therapy offered at Chianciano Spa in patients with symptomatic OA of one or both knees.
In particular, the objective of the study was to verify the efficacy of mud-bath therapy in reducing the severity of OA symptoms, thereby improving the quality of life, and in preventing progression of the disease and the onset of disability (secondary prevention). We also evaluated the possibility that in patients receiving drug therapy, the addition of mud packs and thermal baths, which are generally not associated with adverse side effects, might produce more favorable results than those achieved with drugs alone.
Methods
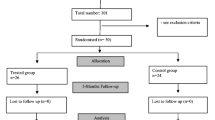
The study population consisted of 61 patients with knee OA, who were divided into two groups. Group A underwent three full cycles of mud-bath therapy at the Chianciano Spa over 1 year’s time, and group B patients did not receive this treatment. Each cycle of therapy included 12 daily treatments. Patients were treated after an overnight fast. A 10-cm thick layer of mud was applied to the knee at a temperature of 47°C and left in place for 20 min, after which the knee was bathed for 15 min at 37°C in Sillene Spring water.
There were not significant differences between the two groups in terms of age or sex distributions or the patients’ clinical characteristics (i.e., severity and extension of OA) when treatment began. In both groups, patients receiving other types of therapy (NSAIDs and/or analgesics) for OA were allowed to continue these treatments for the duration of the study.
The patients who were already being treated with antiinflammatory agents and analgesics were divided into two groups: the first group also underwent spa therapy, and the second did not.
We also conducted a longitudinal observational study on the patients of group A, before and after completion of the treatment protocol, which consisted in three cycles of mud-bath therapy.Footnote 1 The prolonged period of observation (1 year) and the fact that patients underwent three cycles of spa therapy are important factors for an appropriate assessment of the effects of mud-based spa therapy. Enrolment was carried out using the following inclusion criteria: knee pain, age >50 years, stiffness after rest lasting < 30 min, presence of joint crepitus, bony tenderness, bony enlargement, and no palpable warmth [30, 31]. Candidates were excluded if they had any of the following: recent surgery, intra-articular steroid injections within the preceding 3 months, arteriopathy, active thrombophlebitis, severe venous insufficiency, neoplastic disease, febrile diseases, uncontrolled hypertension, uncontrolled diabetes mellitus, other rheumatic diseases, current or past heart failure, ischaemic heart disease.
Each patient enrolled in the study underwent the following assessments:
-
physical examination of the knee joint focusing on the principal symptoms of the disease;
-
visual analogue scale (VAS) assessment of pain;
-
tests comprised the Lequesne Algofunctional index.
The physical examination of each knee included the ascertainment of pain on palpation (presence/absence) and the capacity for flexion/extension, which was rated as complete and pain free, complete but painful, limited, or impossible.
For each of these two clinical variables, as reported in the Tables 2, 3 and 4, the percentage of patients where the pain on palpation was present or absent was calculated and the capacity for flexion/extension was rated as complete and without pain, complete but painful, limited or impossible.
VAS are often used to measure the intensity of pain associated with a given disease. This method involves the assignment of a score ranging from 0 (complete absence of pain) to 10 (very intense/unbearable pain) [32–36].
The Lequesne index was also calculated for each patient. For this purpose, a score was assigned for each of the tests conducted in accordance with indications reported in the literature. An overall score representing the sum of the scores for each test was also calculated [37, 38]. This overall score ranged from 0 (indicating that the patient could carry out all activities without difficulty) to 24 (a situation characterised by maximum-intensity pain, discomfort, and inability to carry out the activities of daily life) (Table 1).
Statistical analyses were based on the use of Pearson’s χ2 test for comparing frequency distributions (number of patients in each group with the clinical conditions considered in the study) and Student’s t test for paired data (comparison of mean severity scores for the clinical conditions of the participants at different times or under different circumstances) or Student’s t test for unpaired data (comparison of mean values calculated for the patients of group A before and after therapy). P < 0.05 was considered statistically significant [39–41].
Results
Part I—comparison of treated and untreated patient groups
Physical examination of the knee joints
As far as pain on palpation was concerned, the vast majority of the right knees in group A were asymptomatic after completion of the mud-bath treatments; similar findings emerged for the left knees in this group. The reverse was true in group B patients, who did not undergo mud-bath therapy: pain on palpation was present in the majority of the right and left knees. The percentage of group A patients with no pain in either knee also exceeded the percentage of those with tenderness in one or both knees; again, the reverse was observed in group B. All of these intergroup differences proved to be highly significant at the χ2 test (Table 2).
The other parameter evaluated in the physical examination was flexion/extension (F/E) of the knee (Table 3). After mud-bath therapy, the vast majority of patients in group A could flex and extend their right knees without pain or limitation, and similar findings emerged for the left knees in this group. The exact opposite was observed in group B. Similar pictures emerged when the two legs were considered together. Frequency distributions in the two groups were significantly different (χ2 test) only for the left knee and for both knees. The difference between findings for the right knee was not significant (Table 3). The latter finding might be related to the number of right knees. In fact, flexion and extension of the right knee was not evaluated in two patients who had prosthetic joints in the right leg.
Statistical analysis was also carried out to evaluate differences in the percentages of knees with both symptoms (pain on palpation + limited and/or painful flexion/extension), one of the two symptoms, or neither of these symptoms at physical examination. Regardless of whether the right and left knees were considered separately or together, the χ2 test revealed significantly higher percentages of patients with neither symptom in group A than in group B (Table 4).
VAS assessments of pain
Patients were asked to rate the intensity of knee pain by means of a VAS in which maximum intensity was rated 10. After treatment, the mean value reported in group A was significantly lower than that reported in group B (3.53 vs. 5.73); P = 0.000 (Student’s t test).
Lequesne Algofunctional index
Total index
The overall Lequesne indexes were markedly different in the two groups of patients. After completion of the mud-bath therapy, the mean index for the patients of group A was 6.82 versus 11.43 for those of group B. Student’s t test revealed that this difference was highly significant (t = 3.30, P = 0.002).
Stratification of participants according to their overall Lequesne index also confirmed the efficacy of the mud-bath therapy. Patients whose indexes were extremely low (<3) represented 35.3% of those in group A, but only 2.3% of those in group B, whereas values >12 were recorded for 23.5% of group A and 43.2% of those in group B. The χ2 test revealed that these intergroup differences were significant.
Scores for individual items in the Lequesne index
Marked intergroup differences also emerged for the single-item scores in the index. For all items, the mean scores in group A after completion of the mud-bath therapy were lower than those of group B patients, who had not undergone this therapy. Student’s t test showed that these differences were significant for all items except those related to increased pain after 30 min of standing and the ability to walk on irregular ground.
The mean scores for each item in groups A and B are shown below with data regarding their statistical significance:
-
pain or discomfort during nocturnal bed rest 0.53–0.91; t = 2.01; P = 0.04
-
morning stiffness 0.41–0.77; t = 2.08; P = 0.04
-
remaining standing for 30 min increases pain 0.53–0.75; t = 1.68; P = n.s.
-
pain on walking 0.65–1.11; t = 2.36; P = 0.02
-
pain or discomfort when rising from a sitting position without using the arms 0.35–0.82; t = 3.87; P < 0.001
-
maximum distance walked 1.47–2.84; t = 2.11; P = 0.04
-
can you go up a standard flight of stairs? 0.56–0.96; t = 2.54; P = 0.01
-
can you go down a standard flight of stairs? 0.79–1.04; t = 2.19; P = 0.03
-
can you squat? 0.82–1.27; t = 2.41; P = 0.02
-
can you walk on irregular ground? 0.79–0.94; t = 0.83; P = n.s.
Part II—patients who continued drug therapy
We also compared the subgroups of patients who continued to take antiinflammatory agents and analgesics during the study (total 40 patients), and the findings that emerged were quite interesting. Analysis of clinical findings showed that the number of patients who were symptom free was higher in group A (those who had undergone spa therapy) than in group B (no spa therapy). Student’s t test for unpaired data also revealed significant differences between groups A and B in terms of mean VAS scores (3.75 and 5.85, respectively; P = 0.004) and mean Lequesne indexes (9.78 and 17.04, respectively; P = 0.005).
Part III—comparison of data collected before and after spa therapy in patients of group A
The clinical conditions of group A patients were compared before they initiated spa therapy (time 0 = T0) and after completion of the treatment (time 3 = T3), which included three cycles of mud-bath therapy distributed over a year’s time (for personal reasons, three of the patients missed the second cycle, which was scheduled 6 months after the first, but all three completed the first and third cycles).
This comparison was based on the same symptoms used for comparison of the two groups of patients. A total score was calculated as the sum of the values reflecting the frequency or severity of each of these symptoms:
-
1.
Physical examination of the knee—values ranging from 0 (no symptoms present) to 4 (all symptoms present at maximum severity).
-
2.
VAS pain rating—scores ranging from 0 (no pain) to 10 (maximum pain, unbearable).
-
3.
Lequesne index—values ranging from 0 (no symptoms present) to 24 (all symptoms present at maximum severity).
For each symptom rating or test result, group mean values were compared, and differences were evaluated for statistical significance with the t test for paired data. Standard error (SE) was calculated for each mean value.
Physical examination of the knee joints
Assessment of the patients’ right knees in terms of the symptoms reported above yielded significantly different results at T0 (before treatment) and T3 (after completion of the therapeutic protocol).
The total scores for the group and the mean scores for the single patient decreased appreciably after treatment for the right knees, the left knees and both knees, and t testing for paired data showed that all of these differences were significant.
Analysis of the scores for each symptom in both knees revealed similar results (Table 5). The mean score for pain on palpation displayed a more substantial decrease after treatment than the score for flexion/extension, but in both cases the change proved to be significant (t test for paired data) (Table 5).
VAS
Patients VAS ratings of pain intensity also decreased appreciably from T0 (before treatment) to T3 (after three cycles of mud-bath therapy). Mean scores (±SE) were T0 = 5.56 ± 0.44 (mean score ± SE) T3 = 3.53 ± 0.60 (mean score ± SE). The difference between the two scores was highly significant (P = 0.007, t test for paired data).
Lequesne index
The Lequesne index is widely used in rheumatology to quantify the severity of symptoms and the degree of disability caused by OA of the knee. In the present study, we calculated the total score and the mean score for each group of symptoms. The analysis of these data with the t test for paired data revealed:
-
mean scores for the first and third groups of symptoms (pain/discomfort and activities of daily life) indicated remarkable decreases in severity from T0 to T3, which were highly significant (t test for paired data);
-
mean scores for the second group of symptoms (maximum distance walked) also decreased appreciably from T0 to T3, but this difference did not reach statistical significance because the data are expressed as the number of meters walked, and this is difficult to estimate at a subjective level without a specific system to measure the distances.
Analysis of the total Lequesne indexes (which reflect the two symptoms and all of the activities) also revealed remarkable decreases from T0 to T3, and this difference was highly significant (P = 0.000 t test for paired data) (Table 6).
Discussion
Osteoarthritis is a chronic degenerative disease with a high incidence and prevalence, and it clearly requires therapeutic interventions and primary and secondary prevention strategies that are multidisciplinary, involving drug therapy, physical therapy, spa therapy and climatotherapy.
Our study was based on the assessment of clinical symptoms by medical specialists and by the patients themselves (e.g., VAS ratings of pain intensity, Lequesne index scores for functional disturbances).
A similar method has been used recently in a study conducted in the Netherlands on patients with non-traumatic knee pain, who were re-examined 1 year after enrolment to determine the prognostic significance of the symptoms observed at baseline. The authors concluded that the symptoms characteristic of this condition (duration and intensity of pain, limitation of daily activities and social interaction) and their persistence after 1 year have an important predictive value. The treatment of knee symptoms required further study to identify the most effective approach for ensuring favourable long-term evolution of these symptoms [42].
We compared clinical parameters in patients who had undergone three cycles of mud-bath therapy over the past year (group A) and controls, who had not undergone this type of therapy (group B). Moreover, this analysis was carried out only on patients of groups A and B who had continued to receive drug therapy during the study. Finally in the patients of group A, the same parameters were also analysed before and after mud-bath therapy. The percentage of patients with no symptoms or mild symptoms was higher in group A than in group B. Within group A, this percentage was higher after treatment that before spa therapy. It is important to note that patients in group A treated with drugs and spa therapy achieved better results than group B patients who used drug therapy alone. Our findings confirm the results of controlled clinical trials, which have documented the positive effects of mud-bath therapy in patients with OA [4, 5, 7]. The therapeutic efficacy of this approach can be attributed to its documented effects on the diencephalic–pituitary–adrenal axis, which result in the release of cortisol and endorphins and inhibition of inflammatory mediators (IL-1, IL-6, PGE2, LTB4, TNFα). The local vasodilatation produced by the mud-pack also favours the removal of proinflammatory and algogenic substances.
It should be stressed that this type of therapy has virtually no known adverse effects and can be combined with other types of therapy and other rehabilitation modalities (i.e. physical therapy etc.) commonly used for the management of osteoarthritis [43].
Notes
For personal reasons, three of the patients in group A were unable to complete the second cycle of treatment scheduled 6 months after the first, but all three completed the third cycle, which began 1 year after the first. .
References
Kovacs I, Bender T (2002) The therapeutic effects of Cserkeszölö thermal water in osteoarthritis of the knee: a double blind, controlled, follow-up study. Rheumatol Int 21(6):218–221
Balint GP, Buchanan WW, Adam A et al (2007) The effect of the thermal mineral water of Nagybaracska on patients with knee joint osteoarthritis—a double blind study. Clin Rheumatol 26(6):890–894
Forestier R, Desfour H, Tessier JM et al (2010) Spa therapy in the treatment of knee osteoarthritis, a large randomised multicentre trial. Ann Rheum Dis 69(4):660–665 [Epub 3 Sep 2009]
Wigler I, Elkaiam O, Paran D et al (1995) Spa therapy for gonarthrosis: a prospective study. Rheumatol Int 15(2):65–68
Elkayam O, Wigler I, Tishler M et al (1991) Effect of spa therapy in Tiberias on patients with rheumatoid arthritis and osteoarthritis. J Rheumatol 18(12):1799–1803
Nguyen M, Revel M, Dougados M (1997) Prolonged effects of 3 week therapy in a spa resort on lumbar spine, knee and hip osteoarthritis follow-up after 6 months a randomized controlled trial. Br J Rheumatol 36(1):77–81
Tishler M, Rosenberg O, Levy O et al (2004) The effect of balneotherapy on osteoarthritis: is an intermittent regimen effective. Eur J Intern Med 15(2):93–96
Karagülle M, Karagülle MZ, Karagülle O et al (2007) A 10-day course of SPA therapy is beneficial for people with severe knee osteoarthritis. A 24-week randomised, controlled pilot study. Clin Rheumatol 26(12):2063–2071 [Epub 13 Apr 2007]
Yurtkuran M, Yurtkuran M, Alp A et al (2006) Balneotherapy and tap water therapy in the treatment of knee osteoarthritis. Rheumatol Int 27(1):19–27
Guillemin F, Virion JM, Escudier P et al (2001) Effect on osteoarthritis of spa therapy at Bourbonne-les Bains. Joint Bone Spine 68:499–503
Evcik D, Kavuncu V, Yeter A et al (2007) The efficacy of balneotherapy and mud-pack therapy in patients with knee osteoarthritis. Joint Bone Spine 74(1):60–65
Cutović M, Jović S, Konstantinović L et al (2006) The effects of balneotherapy on knee osteoarthritis. Med Pregl 59(1):47–50
Bagnato G, De Filippis LG, Morgante S et al (2004) Clinical improvement and serum amino acid levels after mud-bath therapy. Int J Clin Pharmacol Res 24(2–3):39–47
Forestier R (2000) Amplitude et suivi de l’effet de deux cures thermales successives sur la gonarthrose et la coxarthrose. Rev Rheumatol 67:427–436
Bellometti S, Gallotti C, Pacileo G et al (2007) Evaluation of outcomes in SPA-treated osteoarthrosic patients. J Prev Med Hyg 48(1):1–4
Grassi M, Lucchetta MC, Rini GB et al (2003) Mud therapy in chronic degenerative rheumatic disease. Clin Ter 154:45–48
Basili S, Martini F, Ferroni P et al (2001) Effects of mud-pack treatment on plasma cytokine and soluble adhesion molecule levels in healthy volunteers. Clin Chim Acta 314:209–214
Flusser D, Abu-Shakra M, Friger M et al (2002) Therapy with mud compresses for knee osteoarthritis: comparison of natural mud preparations with mineral-depleted mud. J Clin Rheumatol. 8(4):197–203
Pizzoferrato A, Garzia I, Cenni E et al (2000) β-Endorphin and stress hormones in patients affected by osteoarthritis undergoing thermal mud therapy. Minerva Med 91:239–245
Bellometti S, Galzigna L (1998) Serum levels of prostaglandin and leukotriene after thermal mud-pack therapy. J Investig Med 46:140–145
Bellometti S, Galzigna L, Richelmi P et al (2002) Both serum receptors of tumor necrosis factor are influenced by mud pack treatment in osteoarthrotic patients. Int J Tissue React 24(2):57–64
Bellometti S, Giannini S, Sartori L et al (1997) Cytokine levels in osteoarthrosis patients undergoing mud bath therapy. Int J Clin Pharmacol Res 17(4):149–153
Cozzi F, Carrara M, Sfriso P et al (2004) Anti-inflammatory effect of mud-bath applications on adjuvant arthritis in rats. Clin Exp Rheumatol 22(6):763–766
Bellometti S, Cecchettin M, Lalli A et al (1996) Mud-pack treatment increases serum antioxidant defences in osteoarthrosic patients. Biomed Pharmacother 50(1):37
Bellometti S, Poletto M, Gregotti C et al (2000) Mud bath therapy influences nitric oxide, myeloperoxidase and glutathione peroxidase serum levels in arthritic patients. Int J Clin Pharmacol Res 20(3–4):69–80
Bellometti S, Richelmi P, Tassoni T et al (2005) Production of matrix metalloproteinases and their inhibitors in osteoarthritic patients undergoing mud bath therapy. Int J Clin Pharmacol Res 25(2):77–94
Bellometti S, Cecchettin M, Galzigna L (1997) Mud-pack therapy in osteoarthrosis; changes in serum levels of chondrocyte markers. Clin Chim Acta 268:101–106
Fraioli A (2004) La medicina interna e il termalismo. In: Cugini P, Fiorelli G, Guarini G, Lopez M, Violi F, Volpe M (eds) Trattato Italiano di Medicina Interna—Teodori, 7th edn. Società Editrice Universo, Rome, pp 2987–2996
Cecchettin M, Bellometti S, Zennaro RA et al (1993) Effects of treatment with mature thermal mud on postmenopausal osteoporosis: a preliminary evaluation. Curr Ther Res 54(6):758–762
Altman RD, Asch D, Bloch G et al (1986) Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum 29(8):1039–1049
Peat G, Thomas E, Duncan R et al (2006) Clinical classification criteria for knee osteoarthritis: performance in the general population and primary care. Ann Rheum Dis 65(10):1363–1367 [Epub 20 Apr 2006]
Huskinsson EC (1974) Measurement of pain. Lancet 4:1127–1131
Stephenson NL, Herman JA (2000) Pain measurement: a comparison using horizontal and vertical visual analogue scales. Appl Nurs Res 13(3):157–158
Salaffi F, Stancati A, Silvestri CA et al (2004) Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain 8:283–291
Tsai PF, Tak S (2003) Disease-specific pain measures for osteoarthritis of the knee or hip. Geriatr Nurs 24(2):106–109
Cimmino MA, Sarzi-Puttini P, Scarpa R et al (2005) Clinical presentation of osteoarthritis in general practice: determinants of pain in Italian patients in the AMICA study. Semin Arthritis Rheum 35(1 Suppl 1):17–23
Lequesne MG, Mery C, Samson M et al (1987) Indexes of severity for osteoarthritis of the hip and knee. Validation and value in comparison with other assessment tests. Scand J Rheumatol Suppl 65:85–89
Lequesne MG (1997) The algofunctional indices for hip and knee osteoarthritis. J Rheumatol 24(4):779–781
Valsecchi MG, La Vecchia C (1999) Epidemiologia e metodologia epidemiologica clinica. Forum Service Editore, Genova, pp 25–28
Lilienfield AM, Lilienfield DE (1986) Fondamenti di epidemiologia. Piccin, Padova
Di Iorio F (1994) Elementi di metodologia ed epidemiologia clinica. Piccin, Padova, pp 108–109
Belo JN, Berger MY, Koes BW et al (2009) Prognostic factors in adults with knee pain in general practice. Arthritis Rheum 61(2):143–151
Cantarini L, Leo G, Giannitti C et al (2007) Therapeutic effect of spa therapy and short wave therapy in knee osteoarthritis: a randomized, single blind, controlled trial. Rheumatol Int 27(6):523–529 [Epub 15 Nov 2006]
Acknowledgments
This work was supported by the Fondazione Terme Chianciano.
Conflict of interest statement
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fraioli, A., Serio, A., Mennuni, G. et al. A study on the efficacy of treatment with mud packs and baths with Sillene mineral water (Chianciano Spa Italy) in patients suffering from knee osteoarthritis. Rheumatol Int 31, 1333–1340 (2011). https://doi.org/10.1007/s00296-010-1475-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-010-1475-5