Abstract
Background
Because only a few studies have been performed to date on the invasiveness of laparoscopy-assisted total gastrectomy (LATG) compared with open total gastrectomy (OTG), the minimal invasiveness of LATG has been unclear.
Methods
The OTG cohort contained 35 cases, which were performed from April 2003 to October 2005. The LATG cohort contained 46 cases, which were performed from November 2005 to November 2008. Postoperative changes over time in various parameters relating to minimal invasiveness were evaluated. We used the Wong-Baker FACES Pain Rating Scale to evaluate pain. Vital signs and a face scale were analyzed using daily maximum values on postoperative days (POD) 1–7. A hematological examination was performed on the preoperative day and POD 1, 4, 7, and 10. The number of days until oxygen saturation level (SaO2) was 95% or more in room air was used to evaluate respiratory function.
Results
Significantly lower pain scores were obtained in the LATG group on POD 1, 4, 5, and 7. There was a significantly lower body temperature in the LATG group on POD 7. A significantly lower white blood cell count was revealed for LATG patients on POD 10, and for C-reactive protein on POD 1. Significantly higher serum total protein values were observed in the LATG group on POD 1, 4, and 7. Significantly lower blood sugar level was found in the LATG group on POD 4 and 7. The number of days until SaO2 was 95% or more in room air was significantly fewer in the LATG group.
Conclusions
LATG seems to be a less invasive procedure than OTG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of laparoscopy-assisted gastrectomy (LAG) has rapidly increased in recent years, and it is now recognized as a less invasive surgery. Because laparoscopy-assisted distal gastrectomy (LADG) accounted for most LAG, almost all studies on the minimal invasiveness of LAG were associated with LADG [1–4]. However, laparoscopy-assisted total gastrectomy (LATG) requires more sophisticated techniques and a longer operative time than LADG; therefore, an independent evaluation of the minimal invasiveness of LATG is necessary [5–7]. Because only a few studies have been performed on the invasiveness of LATG compared with open total gastrectomy (OTG), the minimal invasiveness of LATG is unclear [8–10]. The number of LATG cases is increasing annually, and therefore, we considered that it was time to conduct a detailed examination of the minimal invasiveness of LATG. This study was designed to clarify the minimal invasiveness of LATG by comparing various parameters associated with LATG with those of OTG.
Patients and methods
All patients were preoperatively diagnosed with early gastric cancer in the upper stomach and total gastrectomy was performed without splenectomy with modified D2 lymph node dissection (right and left paracardial lymph nodes, and those along the short gastric vessels, the lesser curvature, left and right gastroepiploic vessels, suprapyloric and infrapyloric lymph nodes, the left gastric, common hepatic, and celiac arteries, the proximal splenic artery, and those along the distal splenic artery) in a single hospital. The OTG cohort contained 35 cases, which underwent the procedure from April 2003 to October 2005, which was before we initiated LATG. The LATG cohort contained 46 cases, which underwent the procedure from November 2005 to November 2008. Postoperative changes in various parameters related to invasiveness were evaluated in 59 cases with no postoperative complications (42 for LATG and 27 for OTG). Moreover, the postoperative changes in blood sugar were evaluated in 33 cases of LATG and 23 of OTG whose preoperative fasting blood sugar level was <110 mg/dl. The postoperative changes in blood pressure were evaluated in 26 cases of LATG and 23 of OTG who did not have preoperative hypertension. Vital signs were analyzed on postoperative days (POD) 1–7 using daily maximum values. A hematological examination was performed on the day before the operation and POD 1, 4, 7, and 10.
Pain scale
We used the Wong-Baker FACES Pain Rating Scale (Fig. 1) to evaluate the differences in pain of patients after LATG and OTG [11]. Each patient was evaluated from POD 1 to 7, and temporal changes in pain were studied comparatively between OTG and LATG. The FACES Pain Rating Scales were recorded three times per day, and the highest score of the day was used for analysis.
Wong-Baker FACES Pain Rating Scale and postoperative changes in face scale. Patients were instructed to choose one of the five faces that best described their level of pain. Face 1 appears to be smiling (no pain), and face 5 indicates crying (unbearable pain). OTG open total gastrectomy; LATG laparoscopy-assisted total gastrectomy [21]
Operating procedure
OTG was performed through an approximately 20-cm-long midline laparotomy incision. LATG was performed using five ports (two 5-mm bilateral costal arch ports, two 12-mm bilateral flank ports, and one 12-mm camera port in the umbilical region). The camera port or left flank port wound was extended to 4 cm for stomach extraction and to perform Y-limb anastomosis. Roux-Y reconstruction was used in all cases. An esophagojejunostomy was performed during OTG using a circular stapler and the Y-limb anastomosis was handsewn. An esophagojejunostomy was achieved laparoscopically during LATG using a linear (side-to-side anastomosis) or circular stapler (DST Series™ EEA™ OrVil™, Covidien Ltd., Hamilton, Bermuda). A linear stapler was used for the Y-limb anastomosis (side-to-side anastomosis). In OTG, lymph node dissection along the distal splenic artery was achieved by mobilizing the spleen and distal pancreas. And in LATG, an original method, “partial mobilizing” (half cranial side of pancreas and spleen after amputation the esophagus), was used.
Clinical pathway
The same postoperative care was provided for both cohorts using the same clinical pathway: walking and drinking water was resumed on POD 1, a water-soluble contrast examination (50 ml of meglumine sodium amidotrizoate) for the esophagojejunostomy on POD 3, meals were resumed on POD 4, and hospital discharge on POD 14. All patients were administered 2000 ml of BFLUID (840 Kcal) (Otsuka Pharmaceutical Co., Ltd., Tokyo, Japan) for 24 h from POD 1 to 4 and 1000 ml of BFLUID (420 Kcal) for 24 h on POD 5 and 6. For patients with a body weight > 60 kg, we added 500 ml of lactate Ringer’s solution from POD 1 to 3. All patients were administered oxygen (2 l/min) in bed until oxygen saturation level (SaO2) was 95% or more in room air. Patients of both cohorts were given continuous epidural anesthesia for 2 days after the operation as well as diclofenac sodium or flurbiprofen axetil if requested.
Statistical analysis
Data obtained were statistically analyzed by the t test and chi-square test using SPSS 16.0 for Windows (SPSS Inc., Chicago, IL). p < 0.05 was considered significant.
Results
Patient background and operative findings
No significant difference was observed in age, sex, American Society of Anesthesiology classification, or body mass index between the LATG and OTG groups. No significant difference was observed in operating time. There was significantly less bleeding associated with LATG (54.9 ± 45.3 ml) than that with OTG (304.3 ± 237.3 ml) (p = 0.000). There was no significant difference in the number of dissected lymph nodes. There were no intraoperative complications in either group, and no case needed to convert to open surgery during LATG (Table 1).
Postoperative course
Postoperative complications
Complications developed in 22.8% of the subjects who received OTG. The complication rate for LATG was lower at 8.7%, but the difference was statistically insignificant. Pneumonia was observed in two cases (4.8%), drug-induced renal dysfunction necessitating diuretics and fluid replacement in one case (2.4%), and anorexia necessitating parenteral fluid in one case (2.4%) of LATG. There was no significant difference in the first flatus day. There was significantly less use of analgesics for patients who received LATG than OTG (p = 0.011). The duration of postoperative hospital stay was significantly shorter for LATG (15.5 ± 3.3) than that for OTG (18.8 ± 6.3) (p = 0.003) patients. There was no operative death or death during hospitalization in either group, and there have been no recurrences to date (Table 2).
Evaluation of invasiveness
Pain scores
Peak pain scores were recorded at POD 3 in both the LATG and OTG groups, and the scores subsequently decreased over time. The LATG group showed lower pain scores on all days and significantly lower scores on POD 1 (p = 0.002), 4 (p = 0.000), 5 (p = 0.025), and 7 (p = 0.023) (Fig. 1).
Vital signs
No significant difference was observed in body temperature immediately after surgery between the two groups. However, a significantly lower temperature was obtained for the LATG group on POD 7 (p = 0.013). Seemingly lower values were obtained for systolic blood pressure in the LATG group; however, no significant differences were observed (Fig. 2).
Hematology
There was no significant difference in white blood cell count (WBC) immediately after surgery; however, significantly lower values were obtained in the LATG group on POD10 (p = 0.005) and for C-reactive protein (CRP) on POD 1 (p = 0.007). Serum total protein levels showed generally higher values in LATG patients after surgery, and a significant difference was observed on POD 1 (p = 0.000), 4 (p = 0.001), and 7 (p = 0.003). There was no significant difference in lymphocyte counts or hemoglobin. Blood sugar showed generally lower values in LATG patients from immediately after surgery, and significant differences were observed on POD 4 (p = 0.001) and 7 (p = 0.000) (Fig. 3).
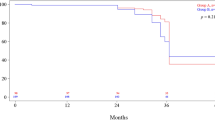
Number of days until SaO2 was obtained 95% or over
The number of days until SaO2 was 95% or more in room air was significantly (p = 0.041) fewer in the LATG group (1.46 ± 0.71) than that in the OTG (2.03 ± 1.54) group (Fig. 4).
Discussion
Presently, it is the end of the second decade since the first LAG for gastric cancer [12]. During this period, LAG has spread rapidly, especially in Asia. According to data from the ninth questionnaire survey conducted by the Japanese Society for Endoscopic Surgery, 21,048 patients underwent LAG in Japan from 1999 to 2007, and 23.4% of gastric cancer operations were performed laparoscopically in 2007 [13]. So far, almost all LAG have been conducted as LADG; however, based on the prevalence of LAG, this laparoscopic technique has progressed and the number of LATG cases is increasing annually. In the questionnaire survey, the rate of LATG compared with LAG was 10.8% (514/4465) in 2007 [13].
LAG is characterized by long operative time, little blood loss and pain, early first flatus, and short postoperative hospital stay [14–16]. In this study, there was no significant difference in defecation because a common clinical pathway was used for both cohorts (diarrhea induced by water-soluble contrast examination on POD 3). However, all other factors were the general characteristics of LAG. In this study, we evaluated the minimal invasiveness of LATG by comparing changes over time in various parameters with those obtained by OTG for making the less invasive characteristics clearer.
A visual analog scale is the most appropriate way to evaluate pain [17]. There are several types of visual analog scales, but the present study used the Wong-Baker FACES Pain Rating Scale, which is commonly used worldwide [11]. Due to the continuous epidural anesthesia given for 2 days immediately after surgery, the pain peaked on POD 3 for patients in both groups and decreased thereafter. The pain scores after LATG were lower than that after OTG on all days and significant differences were obtained on POD 1, 4, 5, and 7, indicating that LATG is a less painful procedure. Blood pressure peaked on POD 3 in both groups and decreased thereafter in agreement with the pattern of the pain face scale. This result suggests that the changes in blood pressure are related to less pain of LATG. There was a significant difference in body temperature between the groups on POD 7, but both groups progressed similarly from POD 1 to 6. Therefore, much difference did not seem to appear in the two procedures concerning body temperature.
WBC and CRP often are used as inflammatory indices. Significantly lower WBC values were observed in the LATG group on POD 10, whereas significantly lower CRP values were seen on POD 1. CRP increased and decreased at different times compared with WBCs. This made it difficult to interpret the data. Only one study has described postoperative changes (POD 0, 1, 3, and 7) in WBC and CRP after LATG. In that study, significant differences in WBC were observed on POD 1, 3, and 7, but there were no significant differences in CRP [8]. Furthermore, there was no significant difference in body temperature as an inflammatory index on POD 1–6, suggesting that the resolution of inflammatory response indices need additional examination. Generally, nutritional parameters, such as serum total protein levels and lymphocyte counts, decrease transiently after surgery. However, only serum protein levels were significantly higher in the LATG group than those in the OTG group. Although there was significantly less bleeding in the LATG group than that in the OTG group, there was no significant difference in postoperative hemoglobin level. Intraoperative blood loss contains not only blood but protein-rich exudates; therefore, this can be regarded as a reason for the hemoglobin and serum protein results. Postoperative blood sugar generally showed lower values with LATG and significant differences were observed on POD 4 and 7, even though the same number of calories was administered, suggesting that LATG also can be regarded as less invasive from the standpoint of dysfunction of glucose tolerance.
We compared the influence of respiratory function between LATG and OTG. The characteristics of lesser pain and destruction of the abdominal wall might result in quicker recovery of respiratory function after the operation; however, pneumoperitoneum could have an adverse effect on respiratory function [18]. In particular, the longer operative time in LATG than LADG could amplify the influence of pneumoperitoneum. In general, respiratory function is examined with a respiratory function test or blood gas analysis; however, a respiratory function test results in severe pain during the early operative period, and long-term detention of an arterial catheter or frequent puncture to the artery should be avoided. On the other hand, SaO2 is regarded as a simple and noninvasive indicator of pulmonary gas exchange and is routinely performed after major operation in all hospitals [19]. Therefore, we considered that SaO2 between LATG and OTG would provide an effective noninvasive evaluation of respiratory function recovery. There were significantly (p = 0.041) fewer days until SaO2 was 95% or more in the LATG (1.46 ± 0.71) than in the OTG (2.03 ± 1.54) group, suggesting that LATG patients recovered their respiratory function earlier than OTG patients.
LAG is reportedly more difficult than open gastrectomy, and furthermore, LATG is more difficult to perform than LADG; therefore, the question is whether complications are more prevalent with LATG than LADG. In our department, the LATG complication rate (8.7%) was lower than that of OTG (22.8%), and all complications were mild. Therefore, LATG can be thought to be safer and not riskier compared with open gastrectomy if performed with adequate skill and experience.
Conclusions
LATG seems to be less invasive than OTG. A phase II study to evaluate feasibility of LADG has just finished and a phase III study is awaited [20]. A phase II study to evaluate feasibility of LATG also should be conducted at the next step.
References
Adachi Y, Shiraishi N, Shiromizu A et al (2000) Laparoscopy-assisted Billroth I gastrectomy compared with conventional open gastrectomy. Arch Surg 135:806–810
Tanimura S, Higashino M, Fukunaga Y et al (2005) Laparoscopic distal gastrectomy with regional lymph node dissection for gastric cancer. Surg Endosc 19:1177–1181
Shiraishi N, Yasuda K, Kitano S (2006) Laparoscopic gastrectomy with lymph node dissection for gastric cancer. Gastric Cancer 9:167–176
Kawamura H, Okada K, Isizu H et al (2008) Laparoscopic gastrectomy for early gastric cancer targeting as a less invasive procedure. Surg Endosc 22:81–85
Tanimura S, Higashino M, Fukunaga Y et al (2007) Laparoscopic gastrectomy with regional lymph node dissection for upper gastric cancer. Br J Surg 94:204–207
Huscher CG, Mingoli A, Sgarzini G et al (2007) Totally laparoscopic total and subtotal gastrectomy with extended lymph node dissection for early and advanced gastric cancer: early and long-term results of a 100-patient series. Am J Surg 194:839–844
Kim JJ, Song KY, Chin HM et al (2008) Totally laparoscopic gastrectomy with various types of intracorporeal anastomosis using laparoscopic linear staplers: preliminary experience. Surg Endosc 22:436–442
Usui S, Yoshida T, Ito K, Hiranuma S, Kudo SE, Iwai T (2005) Laparoscopy-assisted total gastrectomy for early gastric cancer: comparison with conventional open total gastrectomy. Surg Laparosc Endosc Percutan Tech 15:309–314
Topal B, Leys E, Ectors N et al (2008) Determinants of complications and adequacy of surgical resection in laparoscopic versus open total gastrectomy for adenocarcinoma. Surg Endosc 22:980–984
Mochiki E, Toyomasu Y, Ogata K et al (2008) Laparoscopically assisted total gastrectomy with lymph node dissection for upper and middle gastric cancer. Surg Endosc 22:1997–2002
Wong DL, Baker CM (1988) Pain in children: comparison of assessment scales. Pediatric Nursing 14:9–17
Kitano S, Iso Y, Moriyama M, Sugimachi K (1994) Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 4:146–148
Japanese Society for Endoscopic Surgery (2008) The 9th nationwide survey of endoscopic surgery in Japan. J Jpn Soc Endosc Surg 13:499–611
Dulucq JL, Wintringer P, Perissat J et al (2005) Completely laparoscopic total and partial gastrectomy for benign and malignant diseases: a single institute’s prospective analysis. J Am Coll Surg 200:191–197
Pugliese R, Maggioni D, Sansonna F et al (2007) Total and subtotal laparoscopic gastrectomy for adenocarcinoma. Surg Endosc 21:21–27
Memon MA, Khan S, Yunus RM et al (2008) Meta-analysis of laparoscopic and open distal gastrectomy for gastric carcinoma. Surg Endosc 22:1781–1789
Huskisson EC (1974) Measurement of pain. Lancet 2:1127–1131
Tanimura S, Higashino M, Fukunaga Y et al (2006) Respiratory function after laparoscopic distal gastrectomy: an index of minimally invasive surgery. World J Surg 30:1211–1215
Katsuya H, Sakanashi Y (1989) Simple and noninvasive indicator of pulmonary gas exchange using pulse oximetry. J Clin Monit 5:82–86
Kurokawa Y, Katai H, Fukuda H et al (2008) Phase II study of laparoscopy-assisted distal gastrectomy with nodal dissection for clinical stage I gastric cancer: Japan Clinical Oncology Group Study JCOG0703. Jpn J Clin Oncol 38:501–503
Hockenberry MJ, Wilson D, Winkelstein ML (2005) Wong’s essentials of pediatric nursing, 7th edn. Mosby, St. Louis, p 1259
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kawamura, H., Yokota, R., Homma, S. et al. Comparison of Invasiveness Between Laparoscopy-Assisted Total Gastrectomy and Open Total Gastrectomy. World J Surg 33, 2389–2395 (2009). https://doi.org/10.1007/s00268-009-0208-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-009-0208-y