Abstract
Background
Recent advances in surgical techniques have led to widespread acceptance of laparoscopic gastrectomy for gastric cancer. We performed distal gastrectomy with regional lymph node dissection in 235 patients with gastric cancer located in the middle and lower third of the stomach.
Methods
In 171 cases, reconstruction was done using the Billroth I method intracorporeally and the aid of laparoscopic linear stapling devices. The Billroth II and Roux-en-Y methods were used in the remaining 56 and eight patients, respectively,
Results
Patients who underwent laparoscopic distal gastrectomy had a more rapid postoperative recovery than those treated via the open approach. Postoperative complications with this technique were within a permissible range. In terms of the survival curve, there was no statistical difference between the laparoscopic group diagonesed as clinical T2N0 (c T2N0) Preoperatively and the open group.
Conclusion
The laparoscopic technique is not only less invasive, but is also similarly safe and curative compared to open gastrectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
As Minimal-access surgical techniques have been refined in recent years, laparoscopic gastrectomy for gastric cancer has become feasible of advances in surgical techniques. Previously, we reported on the technique and results of distal gastrectomy with regional lymph node dissection using hand-assisted laparoscopic surgery (HALS) or totally laparoscopic gastrectomy for gastric cancer [7]. Here we describe the technique of totally laparoscopic gastrectomy with intracorporeal Billroth I reconstruction and discuss the prognosis of advanced cases (cT2N0).
Patients and methods
Patients
Between March 1998 and May 2003, 235 patients with gastric cancer were operated on with this procedure. The average age of the patients was 63.6 years (range, 25–86), and the male-female ratio was 154:81. The inclusion criteria were as follows: the tumors should be located in the middle or lower third of the stomach, confined to the proper muscular layer in terms of depth of tumor invasion, and there should be no evidence of metastases to regional lymph nodes on preoperative examination (not more than cT2N0). The preoperative staging was determined by gastrofiberscopy, upper GI series, CT, and endoscopic ultrasonography. IN principle, we did not do diagnostic laparoscopy or cytologic lavage prior to gastrectomy in this series.
Surgical procedure
In totally laparoscopic gastrectomy, five trocars were used, and a 12-mm paraumbilical port was subsequently extended to 3–4 cm long when pulling out the specimen (Fig. 1). In principle, we performed laparoscopic lymph node dissection in almost the same manner as conventional open gastrectomy. All group 1 and 2 lymph nodes, defined according to the Japanese Classification of Gastric Carcinoma [1], were dissected.
The order of the nine steps in this procedure are shown Fig. 2. The first step is dissection of the left greater omentum and the lymph nodes along the left gastroepiploic vessels (no. 4sb). The second step is dissection of right omentum and the lymph nodes along the right gastroepiploic vessels (no 4d). After dissection of the infrapyloric nodes (no. 6) and the nodes along the superior mesenteric vein (no. 14v) as the third step, transection of duodemun just distal to the pyloric ring is performed as the fourth step. Then we dissect the suprapyloric nodes (no. 5) and the nodes along the proper hepatic artery (no. 12a) as the fifth step. The sixth step is dissection of nodes along the common hepatic artery (no. 8a) and the proximal splenic artery (no. 11p). After dissection of nodes along the left gastric artery (no. 7) and nodes around the celiac artery (no. 9) as the seventh step, skeltonization of the lesser curvature in the remnant stomach, with dissection of the right cardial nodes (no. 1) and the nodes along the lesser curvature (no. 3), is performed as the eighth step. The final step is transection of the stomach on a line defined by inking which is marked during preoperative fibergastroscopy.
In the main, sharp dissection was done using laparoscopic coagulation shears. To reduce the chance of port site metastases periodical suctions of mist in the peritoneal cavity were performed. The laparoscopic image around the celiac and hepatic artery after lymph node dissection is shown in Fig. 3.
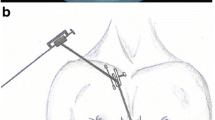
After distal gastrectomy with lymph node dissection was completed, the specimen was pulled out of the peritoneal cavity through the wound which was extended to 3–4 cm long from the 12-mm paraumbilical port. After the proximal and distal margins from the tumor were confirmed to be distant enough, Billroth I reconstruction was used in 171 cases. The Billroth II and Roux-en-Y methods were used in the remaining 56 and eight patients, respectively, because the lesions were located in a relatively proximal portion in the middle third of the stomach and the gastric remnants became small. Billroth I reconstruction was carried by a triangulating stapling technique using a laparoscopic linear stapling device (endo-GIA; US Surgical, Norwalk, CT, USA). Specifically, after the posterior walls of duodenum and remnant stomach were fixed and elevated ventrally by three points of stay sutures, an inverted suture in the posterior wall of gastroduodenostomy a little less than one second in circumference was made by firing the endo-GIA (60–3.5) (Fig. 4). Everted sutures in the anterior wall were carried out in two series using the endo-GIA (Fig. 5). Thus, the gastroduodenostomy was completed using the triangular stapling technique (Fig. 6). After peritoneal irrigation was performed and a drain was inserted around the anastomosis, each wound was closed. The postoperative wound was quite small (Fig. 7).
The statistical analysis was done using the Student t-test or chi-square test. Findings of p < 0.05 were considered significant.
Results
The average operating time for the 235 cases was 236 min (range, 140–380). This time was significantly longer than that for the conventional open procedure (184 min, n = 200), which had been performed in patients of similar staging. The average blood loss was 134 ml (range, 15–900), which was significantly less compared with open gastrectomy (466 ml, n = 200). The average number of harvested lymph nodes per patient was 31 (range, 7–78), which was not significantly different from the number for open gastrectomy (30, n = 200) (Fig. 8).
In the postoperative histopathological examination, the depth of tumor invasion was found to be mucosal in 113 cases, submucosal in 71, proper muscular in 38, subserosal in nine, and serosal in four. There were metastases to the group 1 lymph nodes in 26 cases (11%) and group 2 lymph nodes in 13 cases (6%). The histopathological staging based on the Japanese Classification of Gastric Carcinoma [1], was stage 1A in 169 patients, stage 1B in 34, stage 2 in 23, and stage 3A in nine (Table 1). It was concluded that gastrectomy with regional lymph node dissection was adequate in this series because of the rate of lymph node metastasis. The accuracy rate in preoperative staging (not more than T2N0) was 82 % (193/235). The 42 patients who had exceeded the inclusion criteria for this procedure were all followed up but not given any additional surgical treatments, after informed consent.
Postoperative complications arising from the anastomosis created via the triangulating stapling technique resulted in leakage in two patients, anastomotic bleeding in one, and stenosis in one, respectively. All of them were managed conservatively—that is, with fasting and endoscopic bougie.
In the postoperative course, oral feeding was commenced on the day after flatus, and the day of discharge from hospital was decided after the patients could take over half of their meals. Postoperative times to flatus, oral feeding, and discharge from hospital were 2.6 days (range, 1–4), 3.3 days (range, 3–8), and 12.0 days (range, 7–33) respectively, which were all significantly shorter than those for the patients submitted to open gastrectomy (3.6 days, 6.0 days, 22.6 days, respectively, n = 200) (Fig. 8).
No tumor recurrence has been observed among T1 cases whose tumor depth was confined to mucosa or submucosa, although metastases to group 1 and 2 lymph nodes were seen in 10 and five cases, respectively. Fifty one patients diagnosed as cT2cN0 preoperatively resulted in stage 1B in 24, stage 2 in 18, and stage 3A in nine. Postoperative recurrence was recognized in two of the 51 cases; these patients had been staged as pT2N1 and pT2N2. The median follow-up period in the over-pT2pN0 group (n = 51) was 3 years and 8 months. Their cumulative survival curve was compared with 65 open gastrectomy patients with similar staging. This is not a randomized control study, but the control group includes only stage 1B and stage 2 patients (Tables 2 and 3). There were no significant differences between the laparoscopic group and the open group (Fig. 9).
Discussion
About 10 years have passed since the introduction of laparoscopy assisted distal gastrectomy for early gastric cancer. [3, 4] Recently, laparoscopic distal gastrectomy for advanced gastric cancer (T2 cases) [6, 7, 10] and the laparoscopic management of upper gastric cancer [8, 9] have been attempted in Japan. Laparoscopic gastrectomy has been recognized to be a less invasive operation for early gastric cancer [12]. The fact that the curability in laparoscopic gastrectomy for early gastric cancer located in middle and lower portion is equal to that achieved with open gastrectomy has become a matter of common knowledge. What is now at issue is the curability in laparoscopic gastrectomy for advanced gastric cancer. Our data on the cumulative survival rate in laparoscopically treated cT2N0 cases do not represent a randomized control study, nor do they include long-term survival data. However, the data suggest that laparoscopic gastrectomy for advanced cancer (cT2N0) is similarly curative when compared to open gastrectomy.
Reconstruction after laparoscopy-assisted gastrectomy is commonly performed extracorporeally through an epigastric small incision 4–7 cm long [3, 4]. In this procedure, the operative view of the field of reconstruction is occasionally very poor, and the procedure becomes very difficult in obese patients. We think this might have resulted in complications from anastomosis such as minor leakage due to excessive traction of the organs toward the abdominal wall. Intracorporeal anastomosis after totally laparoscopic gastrectomy has been adopted by a few institutions. [2, 7]. However, end-to-end techniques for anastomosis of the digestive tract using linear stapling devices have been reported in conventional open surgery, and their safety has already been established [5, 11]. This procedure is called “the triangulating stapling technique” because of the triangular shape of the cross section at the anastomotic site. In this technique, anastomotic bleeding and stenosis are rare because of the direct visibility of the suture line and the wide-open anastomotic caliber. The intracorporeal triangulating stapling technique we have described is thought to be a safe and sure method for reconstruction after laparoscopic distal gastrectomy.
Conclusion
In conclusion, laparoscopic distal gastrectomy with regional lymph node dissection is less invasive than its conventional open counterpart. It is not only as safe as open gastrectomy but also curative in patients whose stages are cT2N0 or below. The triangulating stapling technique is a safe and viable procedure for reconstruction after laparoscopic distal gastrectomy.
Reference
Japanese Gastric Cancer Association (1999) Japanese classification of gastric carcinoma. 13th ed. Kanehara, Tokyo
Kanaya S, Gomi T, Momoi H, Tamaki N, Isobe H, Katayama T, Wada Y, et al (2002) Delta-shaped anastomosis in totally laparoscopic Billroth 1 gastrectomy: new technique of intraabdominal gastroduodenostomy. J Am Coll Surg 195: 284–287
Kitano S, Shimoda K, Miyahara M, Shiraishi N, Bandoh T, Yoshida T, Shuto K, et al (1995) Laparoscopic approaches in the management of patients with early gastric carcinomas. Surg Laparosc Endosc 5: 359–362
Nagai Y, Tanimura H, Takifuji K, Kashiwagi H, Yamoto H, Nakatani Y (1995) Laparoscope-assisted Billroth I gastrectomy. Surg Laparosc Endosc 5: 281–287
Ravitch MM, Steichen FM (1972) Technique of staple suturing in the gastrointestinal tract. Ann Surg 175: 815–837
Tanimura S, Higashino M, Fukunaga Y, Osugi H (2001) Hand-assisted laparoscopic distal gastrectomy with regional lymph node dissection for gastric cancer. Surg Laparosc Endosc Percut 11: 155–160
Tanimura S, Higashino M, Fukunaga Y, Osugi H (2003) Laparoscopic distal gastrectomy with regional lymph node dissection for gastric cancer. Surg End. 17: 758–762
Tanimura S, Higashino M, Fukunaga Y, Osugi H (2003) Laparoscopic gastrectomy with regional lymph node dissection for upper gastric cancer. Gastric Cancer 6: 64–68
Uyama I, Sugioka A, Fujita J, Komori Y, Matsui H, Hasumi A (1999) Laparoscopic total gastrectomy with distal pancreatosplenectomy and D2 lymphadenectomy for advanced gastric cancer. Gastric Cancer 2: 230–234
Uyama I, Sugioka A, Matsui H, Fujita J, Komori Y, Hasumi A (2000) Laparoscopic D2 lymph node dissection for advanced gastric cancer lacated in the middle or lower third portion of the stomach. Gastric Cancer 3: 50–55
Venkatesh KS, Morrison N, Larson DM, Ramanujam P (1993) Triangulating stapling technique: an alternative approach to colorectal anastomosis. Dis Colon Rectum 36: 73–76
Yano H, Monden T, Kinuta M, Nakano Y, Tono T, Matsui S, Iwazawa T, et al (2001) The usefulness of laparoscopy-assisted distal gastrectomy in comparison with that of open distal gastrectomy for early gastric cancer. Gastric Cancer 4: 93–97
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tanimura, S., Higashino, M., Fukunaga, Y. et al. Laparoscopic distal gastrectomy with regional lymph node dissection for gastric cancer. Surg Endosc 19, 1177–1181 (2005). https://doi.org/10.1007/s00464-004-8936-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-004-8936-4


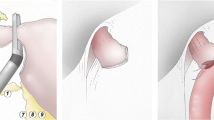



 : Stump of left gastric artery.
: Stump of left gastric artery. : Stump of right gastric artery.
: Stump of right gastric artery.




